Abstract
Background and Purpose
As a result of the anatomical proximity of the thoracic spine to the cervical, lumbar, and shoulder regions, dysfunction in the thoracic spine can influence pain, mobility, and stability across these areas. Currently, a paucity of evidence exists addressing treatment of individuals with primary thoracic pain, especially in young, athletic patients. Furthermore, current research discussing clinical reasoning frameworks focus on the differential diagnostic process. The purpose of this case report was to present a framework that describes the clinical reasoning process for the implementation and sequencing of procedural interventions for the management of a dancer with thoracic pain.
Case Description
A 21-year-old female dancer presented to physical therapy with a medical diagnosis of thoracic pain. The patient reported exacerbation of left thoracic pain with prolonged sitting, twisting/arching her back during dance, and lifting >15 lbs overhead. Examination revealed hypomobility with positive pain provocation during mobility testing of T1-T3 and the sternocostal junction of ribs 2-4, with associated muscle guarding palpated in the left iliocostalis thoracis and levator scapulae.
Outcomes
Following 10 visits, the patient had no pain, no functional deficits, and a Global Rating of Change (GROC) of + 6. She returned to full competition, and a 3-month follow-up revealed continued success with dancing and a GROC of +7.
Discussion
This case report described the successful management of a dancer with primary thoracic pain using a clinical reasoning framework for the sequencing of procedural interventions, while incorporating Olson's impairment-based classification system. A combination of manual therapy techniques and neuromuscular control exercises were incorporated to address mobility, stability, mobility on stability, and skill level impairments, which allowed the patient to return to dance activities safely. Future studies should consider the development of further treatment-based clinical reasoning frameworks that illustrate the importance of the sequencing within a session and across the episode of care.
Level of Evidence
4
Keywords: clinical reasoning, impairment-based classification, manual therapy, neuromuscular re-education, thoracic pain
BACKGROUND
While primary thoracic pain has been cited as occurring less frequently than neck or low back pain,1 it can be equally disabling.2,3 The point prevalence for thoracic spine pain in the adult working population ranges from 3% to 70% with 10% to 38% for one-month prevalence, 13% to 39% for three-month prevalence, and 25% to 55% for one-year prevalence.4 As a result of the anatomical proximity of the thoracic spine to the cervical, lumbar, and shoulder regions, dysfunction in the thoracic spine and/or rib cage can influence pain, mobility, and stability in these areas.5 While specific mechanisms for the benefits of manual therapy remain unclear, substantial evidence suggests that manual therapy interventions directed at the thoracic spine can lead to a decrease in pain and improvement in function in the thoracic spine and adjacent regions.6-16 Previous authors of low-level evidence have suggested a combination of manual therapy and exercise in the treatment of individuals with thoracic spine pain.17-21 However, optimal interventions for the management of primary thoracic pain have yet to be determined.
Similar to the cervical and lumbar spine, it often is not feasible to identify pathoanatomical diagnoses as a specific cause of pain in the thoracic spine. Moreover, pathoanatomical diagnoses do not necessarily provide clinicians with relevant information in the clinical decision making process for treatment planning. An alternative method for diagnosis is through the implementation of Olson's impairment-based classification system,22 which breaks down thoracic disorders into several categories based on examination findings and provides suggestions for treatment interventions (Table 1).22 However, while this impairment-based classification system is a good first step in the clinical management of individuals with primary complaints of thoracic pain, it does not provide the clinician with a comprehensive plan of care. A thorough treatment plan must be based on a sound clinical reasoning framework that goes beyond mobility issues to address all aspects of the movement system.
Table 1.
Impairment-based classification system for the thoracic spine. Adapted from Olson, Manual Physical Therapy of the Spine.22
| Classification | Examination Findings | Proposed Interventions |
|---|---|---|
| Thoracic hypomobility |
|
|
| Thoracic hypomobility with upper extremity referred pain |
|
|
| Thoracic hypomobility with neck pain |
|
|
| Thoracic hypomobility with shoulder impairments |
|
|
| Thoracic hypomobility with low back pain |
|
|
| Thoracic clinical instability |
|
|
Abbreviations: AROM, active range of motion; PIVM, passive intervertebral motion; ULND, upper limb neurodynamic.
Clinical reasoning has most recently been defined as “a reflective process of inquiry and analysis carried out by a health professional in collaboration with a patient with the aim of understanding the patient, their context, and their clinical problem in order to guide evidence-based practice.”23 Several clinical reasoning approaches—including the most frequently considered models: deductive reasoning (hypothetico-deductive model) and inductive reasoning (pattern recognition)24—have been thoroughly discussed in the literature and are commonly implemented in clinic practice. However, the majority, if not all identified clinical reasoning approaches are strongly concentrated on the examination and differential diagnosis process.24 An assumed understanding among clinicians that interventions progress from manual therapy, to neuromuscular re-education, to therapeutic exercise fails to take into account the complex procedural reasoning strategies necessary for the development of an appropriate treatment plan. In order for clinicians to provide effective management strategies throughout the episode of care, the clinical reasoning paradigm must shift its focus from differential diagnosis to treatment planning.
The American Physical Therapy Association (APTA) has recently proposed a new mission statement centered around the human movement system,25,26 that facilitates the expansion of an approach that guides the sequencing of interventions during patient management. It encourages physical therapists, as experts of the movement system, to design treatment plans that ultimately assist patients in returning to their desired level of pain-free function and skill. One approach to developing a physical therapy treatment plan is to incorporate our understanding of motor task requirements of functional movement into the clinical reasoning process for treatment planning. As physical therapists we understand that mobility, stability, mobility on stability, and skill are motor task requirements of all functional movements.27,28 This suggests a natural sequencing for the progression of treatment interventions throughout the episode of care. Therefore, the purpose of this case report was to present the clinical reasoning process associated with the development and implementation of a treatment plan for the management of a dancer with thoracic pain across the episode of care.
CASE DESCRIPTION
Patient Characteristics
The patient was a 21-year-old female dancer who presented to physical therapy with a medical diagnosis of thoracic pain (ICD 10: M54.6). The patient intake form showed no significant past medical or surgical history. Current medications included birth control and Motrin for pain as needed. The patient was educated not to change her medication for the duration of the episode of care. The patient reported an insidious onset of left thoracic pain beginning eight months prior to the initial visit. The patient reported that at that time she was dancing seven hours per week and performing contemporary dance routines. Three months following the onset of pain, the patient increased her dancing to 30 hours per week. This intensity was maintained for three months, during which time her thoracic pain increased from 3-4/10 to 7/10 on the Numeric Pain Rating Scale (NPRS). Upon conclusion of competition, the patient was not scheduled to dance for the following two months. When the pain did not subside after one month of rest, the patient sought medical care from her primary care physician and was referred to physical therapy.
History
At the initial examination, the patient reported that she had returned to dancing three weeks earlier and was performing ballet, hip hop, and jazz approximately 25-30 hours per week. The patient reported constant achy/sharp pain localized to the left side of the upper and middle thoracic spine (T3-T5) with no reports of radicular symptoms. She was unable to identify any position that made the pain better, but stated that the pain subsided an hour into dancing and did not affect her ability to sleep. Throughout the day, her thoracic pain varied between 4/10 and 7/10, with an average pain intensity of 6/10. Aggravating factors, as indicated on the Patient Specific Functional Scale (PSFS), included sitting in one place for more than 30 minutes, twisting/arching her back during dance movements, and lifting more than 15 lbs overhead. The baseline Neck Disability Index (NDI) and PSFS Scale were 32% and 4/10, respectively (Table 2). The patient's goals for physical therapy included returning to pain-free dancing, being able to sit for at least 4-5 hours without pain, and resuming all overhead activities without pain.
Table 2.
Pertinent Examination Findings and Outcome Measures
| Outcome Measure | IE |
Visit 6 Week 5 |
Visit 10 Week 10 |
3 month follow up |
|---|---|---|---|---|
| NPRS* | 6/10 | 3/10† | 0/10† | 0/10 |
| NDI (%) | 32 | 20 | 6† | 0% |
| GROC | +5† | +6† | +7 | |
| PSFS | 4/10 | 6/10† | 8/10† | 10/10 |
| C/S flexion* | 55 ° NPRS 5/10 | 60 ° NPRS 2/10 | 60 | |
| C/S LSB* | 40 ° NPRS 3/10 | 40 ° NPRS 0/10 | 40 | |
| C/S LR* | 55 ° NPRS 4/10 | 75 ° NPRS 0/10 | 75 | |
| Left MT | 3+/5 | 4+/5 | 5/5 | |
| Left LT | 3+/5 | 4+/5 | 5/5 | |
| DNF endurance | 10 sec | 35 sec | 40 sec |
Abbreviations: C/S = cervical spine; DNF = deep neck flexor; GROC = Global Rating of Change Score; IE = initial examination; LR = left rotation; LSB = left side bending; LUE = left upper extremity; LT = lower trapezius; MCID = minimal clinically important difference; MT = middle trapezius; NDI = Neck Disability Index; NPRS = Numeric Pain Rating Scale; PSFS = Patient-Specific Functional Scale; lbs = pounds; RUE = right upper extremity; sec = seconds
= Pain reproduced on left side of mid thoracic spine.
= Met MCID
CLINICAL IMPRESSION #1
In the absence of significant past medical history, past surgical history, and red flags, the patient's overall history and subjective findings were consistent with a musculoskeletal spine dysfunction. In addition, the ability of the patient to identify exacerbating and relieving factors, along with uninterrupted sleep made the likelihood of sinister pathology extremely low. Pattern recognition was utilized at this point in the reasoning process to arrive at the initial diagnostic hypothesis. A thorough physical examination assessing range of motion (ROM), muscle strength, joint mobility, and palpation was indicated to confirm the hypothesis of mechanical thoracic spine pain generated from the subjective portion of the initial examination and to definitively rule out serious medical pathology such as cancer, thoracic aortic aneurysm, myocardial ischemia, cholecystitis, etc.
EXAMINATION
A complete neuromusculoskeletal examination was performed, assessing for potential red flags to treatment interventions. A static structural inspection revealed right side bending at the upper cervical spine, a slight forward head posture, and a flat thoracic spine. Reflexes, dermatomes, and myotomes were all intact and symmetrical bilaterally. Joint mobility assessment revealed hypomobility with positive pain provocation during posterior-to-anterior mobilization of T1-T3 and anterior-to-posterior rib mobilization at the sternocostal junction of ribs 2-4 on the left side. During mobility assessment, rib 4 on the left was anteriorly displaced with associated tenderness to palpation (TTP). In addition, TTP with associated muscle guarding was elicited in the left iliocostalis thoracis and left levator scapulae. A breathing assessment revealed limited diaphragmatic action on the left side, with excessive left upper chest excursion. For additional key examination findings see Table 2.
CLINICAL IMPRESSION #2
The addition of the clinical examination findings confirmed the initial hypothesis of mechanical thoracic pain (ICD 10: M54.6). The primary complaint of thoracic pain, muscle imbalances, and segmental hypomobility in the thoracic spine and rib cage led to categorization of the patient into the thoracic hypomobility subgroup of Olson's22 impairment-based classification system (Table 1). The reproduction of thoracic symptoms and the absence of neck pain associated with cervical AROM further supported the patient's classification into this subgroup (Table 2). Clinicians are strongly encouraged to implement multiple forms of clinical reasoning during the differential diagnostic process to minimize errors, such as confirmation bias.29 Both pattern recognition and the hypothetico-deductive reasoning processes were implemented to reach a final diagnostic hypothesis. Physical therapy was recommended for a total of 10 visits over a 10-week period, with re-assessment at five weeks, 10 weeks, and a three month follow-up. It was hypothesized that the patient should respond well to a combination of mobility, stability, and controlled mobility interventions that would address both her impairment level dysfunction, the standardized objective functional outcome measures, and the patient's goals.
INTERVENTIONS
Manual therapy techniques, neuromuscular re-education, and therapeutic exercises were incorporated throughout the episode of care as indicated based on the patient's presentation at each treatment session. While previous research on pattern recognition and the deductive reasoning process support the reasoning approach used for the development of a diagnostic hypothesis, no standardized clinical reasoning framework exists for the development and progression of procedural interventions.24 This case report aims to present a clinical reasoning framework based on motor development in order to guide the plan of care. For a complete description of all the interventions utilized in this case report, please see Table 3 and the Appendix.
Table 3.
Interventions
| Intervention | IE | Visit 2 | Visit 3 | Visit 4 | Visit 5 | Visit 6 | Visit 7 | Visit 8 | Visit 9 | Visit 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Manual Therapy | ||||||||||
| STM to left ICT | X | X | X | |||||||
| STM to left levator scapula | X | X | X | X | X | |||||
| STM to left pectoralis minor | X | X | X | X | X | |||||
| Manipulation CTJ (T3-T5) | X | X | X | |||||||
| AP Ribs 3-4 mobilization | Grade 3 5 x 30s |
Grade 3 5 x 30s |
Grade 4 5 x 30s |
Grade 4 5 x 30s |
||||||
| Cervical spine PA mobilization (C6-C7) | Grade 4 5 x 30s |
Grade 4 5 x 30s |
||||||||
| MET to serratus anterior | 3 x 8s | 3 x 8s | ||||||||
| Neuromuscular Re-education | ||||||||||
| Conc/ecc contractions of left LT/MT | RSL 20reps | RSL 30reps | ||||||||
| Craniocervical flexion (start BP cuff at 20) | 10s hold at 22, 24 | 10s hold at 22, 24, 26 | 10s hold at 22, 24, 26, 28, 30 | |||||||
| Left LT/MT re-education on physioball | Prone 3 x 15 with TC | Prone 3 x 25 with TC | ||||||||
| Left ER re-education | Prone 3 x 15 with TC | Prone 3 x 15 with TC | ||||||||
| Therapeutic Exercise | ||||||||||
| Bridging (foam roll MTS) | 3 x 30s | 3 x 30s | ||||||||
| Standing scapular retraction in squat | Red thera-band 2 x 25 | Blue thera-band 2 x 25 | Grey thera-band 2 x 25 | 25lbs 3 x 25 | 35lbs 3 x 25 | 50lbs 3 x 25 | 60lbs 3 x 25 | |||
| Left LT/MT strengthening on physioball | Prone 3 x 25 | Prone 3 x 25 2lbs | Prone 3 x 25 3lbs | Prone 3 x 25 3lbs | Prone 4 x 25 3lbs | |||||
| Left ER 90 °/90 ° strengthening on physioball | Prone 3 x 25 | Prone 3 x 25 2lbs | Prone 3 x 25 3lbs | Prone 3 x 25 3lbs | Prone 4 x 25 3lbs | |||||
| Left/right HAB with trunk rotation in quadruped | 3 x 25 2lbs | 3 x 25 4lbs | 3 x 25 5lbs | |||||||
Abbreviations: AB, abduction; AP, anterior to posterior; BP, blood pressure; conc, concentric; CTJ, costotransverse joint; ecc, eccentric; ER, external rotators; HAB, horizontal abduction; ICS, iliocostalis thoracic; IE, initial examination; lbs, pounds; LT, lower trapezius; MTS, middle thoracic spine; MT, middle trapezius; MET, muscle energy technique; PA, posterior to anterior; reps, repetitions; RSL, right side lying; s, seconds; STM, soft tissue mobilization; TB, theraband; TC, tactile cues
Clinical Reasoning for the Plan of Care
During initial treatment sessions, the proposed interventions associated with the thoracic hypomobility classification were utilized to guide clinical decision making. Thrust and non-thrust manipulation of the thoracic spine and rib cage, respectively, were performed, followed by postural exercises (Table 1). While the impairment-based classification system provides clinicians with guidelines for the early management of spinal mobility and postural stability impairments in patients with thoracic pain, it does not address the remainder of the rehabilitation process for full return to pain-free movement and functional skills. The neuromuscular re-education of proper dynamic stability and controlled mobility (or mobility on stability) within each involved body segment and across segments is crucial to long-term pain-free functional skill. The authors suggest that when combined, Olson's22 impairment-based classification system and our understanding of motor task requirements of functional movement27 provide a sound clinical reasoning process to guide the plan of care in the absence of strong scientific evidence.
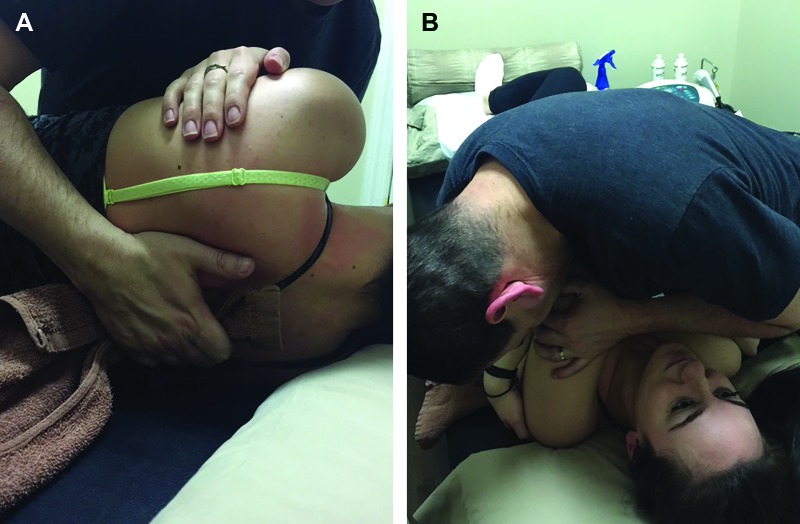
Session one: day of initial examination
Treatment began with manual therapy techniques to address the mobility impairments of the mid thoracic spine, which are the key treatment interventions of Olson's22 impairment-based classification system and the most fundamental motor task requirement for pain-free functional movement. These included soft tissue mobilization to the iliocostalis thoracis and levator scapulae muscle immediately followed by a single thrust manipulation to the costotransverse joints of T3-T5 (Figure 1). At the conclusion of session one, the patient was educated to avoid static sitting positions for more than one hour, to perform 50 cervical retraction exercises throughout the day (5 sets of 10), and to refrain from dancing until further notice. Performing cervical retraction exercises multiple times a day is intended to facilitate long-term postural changes.
Figure 1.
(A) Hand placement of costotransverse joint thrust manipulation. (B) Costotransverse joint thrust manipulation.
Sessions 2-7
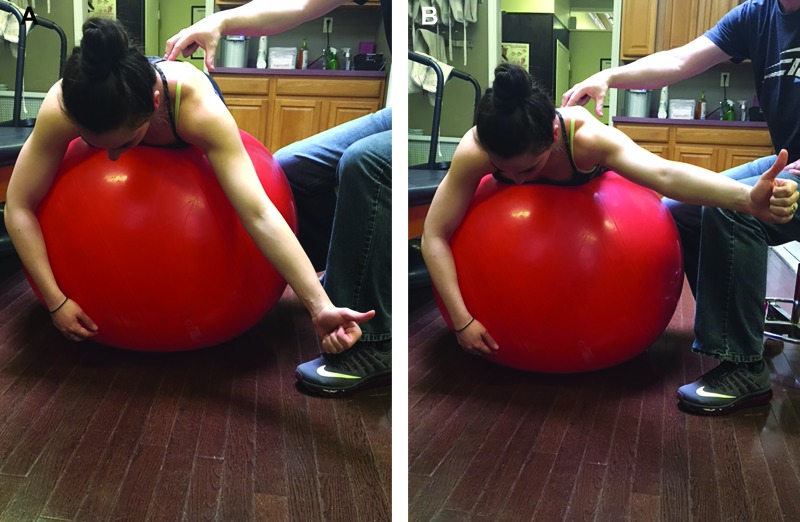
The focus of the next six sessions was to continue to restore mobility throughout the joints and soft tissues of the thoracic spine and rib cage to promote balance across all segments of the spine for the facilitation of controlled mobility during functional activities. On the second session, anterior to posterior grade III non-thrust manipulations to the third and fourth ribs were performed to address the anteriorly displaced fourth rib, which had not been resolved by the previous thrust manipulation (Table 3, Appendix). In addition, on sessions four and five, a muscle energy technique directed at the serratus anterior was applied to further address the anteriorly displaced fourth rib (Table 3, Appendix). During these sessions, neuromuscular re-education focused on stability and controlled mobility following manual therapy interventions (Table 3). This was deemed necessary to develop strength and to teach the patient new movement patterns with proper motor control in the areas of newly gained mobility. Stability of the craniocervical region and upper thoracic spine was attained by using the craniocervical flexion test as a treatment intervention (Figure 2, Appendix). Neuromuscular re-education for the middle and lower trapezius muscle was among a number of controlled mobility exercises during this period of care (Figure 3, Appendix).
Figure 3.
(A) Left lower trapezius strengthening start position. (B) Left lower trapezius strengthening end position.
Figure 2.
(A) Craniocervical flexion test start position. (B) Craniocervical flexion test end position (chin tuck).
During session five, the patient subjectively reported an onset of new central cervical spine pain that may have been brought on by increased time studying and reading in poor postures. A re-assessment revealed hypomobility on posterior to anterior spring testing of C6-C7. The treatment plan was modified (Table 1) based on the new cervical impairments and non-thrust, grade IV posterior to anterior mobilizations to the spinous processes of C6-C7 (Table 3). The patient reported absence of cervical pain on session six, with return of pain on session seven. During this session, manual therapy to the cervical spine was performed as described above, resulting in resolution of pain. Although the lead author considered the use of thrust manipulation, previous research comparing the effects of thrust and non-thrust manipulation of the cervical spine has not demonstrated any significant differences in outcomes.30-32 Furthermore, while the risks of vertebral artery dissection appear low in this particular patient, it is impossible to predict who may sustain an adverse reaction following cervical spine thrust manipulation; therefore, non-thrust manipulation was chosen. All sessions were followed by a home exercise program aimed at reinforcing the neuromuscular re-education introduced during that particular treatment session, in order to integrate the new, more efficient movement pattern into the patient's daily life.
Sessions 8-10
Interventions during the final three treatment sessions focused on the acquisition of motor control in specific functional movements and skill level activities required for this patient to return to dancing. These included quadruped rotational drills that closely resembled certain dance positions and movements (Table 3, Appendix). Additionally, the patient was educated on how to gradually resume dance practice with limitations in previously pain provoking postures until she was cleared for full return to activity.
OUTCOMES
As healthcare providers are increasingly reimbursed based on the value of care delivered to patients, physical therapists will need to continue to implement evidence-based interventions that lead to measureable improvement in outcomes. Based on current evidence and clinical judgment, the primary author chose a combination of outcome measures for this case including an assessment of pain (NPRS), disability (NDI), functional skills (PSFS), and perceived improvement (Global Rating of Change - GROC). These measures encompass all aspects of the movement system and provide objective data that is meaningful to the management of the patient. The outcome measures and their associated scoring metrics have been previously described in detail in several other peer-reviewed articles.8,10,14,33-38 Table 2 summarizes the changes observed in the various examination findings and outcome measures throughout the episode of care and at a 3-month follow-up. Previous research has documented the reliability, validity, and minimal clinically important difference (MCID) of the NPRS (2 points), NDI (14%), PSFS (2 points), and GROC (+3).33,35-39 At the time of discharge, MCID values were met for all of the included outcome measures. In addition, the patient reported improvement in all items listed on the PSFS: sitting in one place for more than 30 minutes, twisting/arching her back during dance movements, and lifting more than 15 lbs overhead.
DISCUSSION
Physical therapists are equipped with a distinct body of knowledge and skills to guide the examination and management of neuromusculoskeletal disorders. Using these tools, the ultimate goal should be the restoration of efficient, pain-free movement for all individuals seeking treatment. This case report demonstrated the successful achievement of this goal for a dancer with primary thoracic pain through the implementation of a clinical reasoning approach that combined Olson's22 impairment-based classification system and an understanding of the requirements of the movement system.27 Although the interventions described in this case are not novel, the authors suggest that implementing a clinical reasoning framework for the development and sequencing of a treatment plan led to a successful outcome of this patient.
Previous research has demonstrated the positive effects of thoracic spine thrust manipulation in the management of individuals with cervical, thoracic, and/or shoulder pain.6-9,11,12,14,15,40 Based on the examination findings in this case, the lead author first chose to perform a thrust manipulation to the costotransverse joints of T3-T5 (Table 2, Appendix). This particular technique may have alleviated the associated muscle guarding of the iliocostalis thoracis muscle and provided neurophysiological input that may have improved the motor recruitment of the deep neck flexors and scapulothoracic muscles.40,41 Olson's22 impairment-based classification system supported this initial choice of manual therapy, which improved the mobility throughout the soft tissues and joints of the thoracic spine, potentially providing a window of opportunity for improving stability of the deep neck flexors and controlled mobility of the scapulothoracic muscles over the next several sessions.
The authors emphasize the importance of manual therapy in the initial management of individuals with cervical/thoracic spine dysfunction. Its primary goal is to provide input to the nervous system that can lead to improvements in mobility, pain, and motor recruitment.41 However, manual therapy in isolation will not restore stability, controlled mobility, or skill. While therapeutic exercise and neuromuscular re-education are commonly implemented in clinical practice, delineation of specific interventions, and their progression, to address these aspects of the movement system is often vague. As the profession of physical therapy evolves, current research calls for the justification of therapists’ selection of manual therapy approaches to treatment. Recently, two different approaches have been widely discussed in the literature. The first, which has been implemented in several randomized clinical trials,7,8,10-12,14 incorporates a prescriptive treatment paradigm to maximize internal validity and minimize the potential for cofounding variables. Conversely, other trials30-32 have implemented a more pragmatic approach to manual therapy, in which the clinicians choose the dosage and type of technique based on the results of the clinical examination. Although this second approach potentially creates additional confounding factors to control for and may challenge the internal validity of the study, it also enhances the external validity and generalizability of the study findings. Regardless of the approach selected, manual therapy remains a passive intervention provided by the therapist, which alone does not allow for the patient's acquisition of motor skill. Therefore, manual therapy must be combined with neuromuscular re-education of functional movement patterns in order to restore efficient, pain-free movement.
Previous research has documented the variety of clinical reasoning strategies used during the differential diagnostic process.24 The importance of ‘reasoning about procedures’ has also been presented.24 However, a clinical reasoning framework designed to systematically progress a patient through an episode of care has yet to be widely accepted in the scientific and clinical communities and may potentially lead to a wide variation in clinical practice. The authors postulate that a combination of an impairment-based classification system22 and the application of motor tasks requirements of functional movement27,42 is one treatment-based reasoning approach that may lead to optimal patient progression. This particular approach may also help clinicians engage in the process of meta-cognition, so that both reflection-in-action and reflection-on-action strategies can be implemented to provide a comprehensive and organized clinical reasoning framework that may assist the clinician's clinical decision making throughout the various phases of rehabilitation.
Similar to the treatment-based classification systems for the cervical and lumbar spine, Olson's impairment-based classification system22 enables the therapist to assign the patient to a specific subgroup from which targeted interventions can be selected. This could potentially reduce variability in practice and facilitate the streamline of initial interventions that have been supported by strong scientific evidence.7,8,10-12,14 An understanding of the motor tasks requirements of functional movement subsequently provides therapists with an organized method to specifically address neuromuscular control and functional skill for each individual patient. While there are no current studies that have explored this model, the authors argue that it speaks to the art of fostering pain-free functional movement patterns. Combined, these approaches support the recently adopted mission statement of the APTA that focuses on the human movement system,25,26 enabling the attainment of the APTA's new vision: to transform society and optimize the human experience.25
Although this case demonstrated a successful outcome, several limitations exist. First, case reports do not provide cause and effect relationships. It is possible, although unlikely, given the duration of the patient's symptoms that spontaneous recovery would have occurred in the absence of treatment. Second, it is difficult to identify which intervention provided the single greatest benefit. In this case, after receiving thrust manipulation and other manual therapy interventions during the first three sessions (Table 3), the patient was able to sit comfortably for four hours without an increase in pain and presented with a NPRS of 3/10, a NDI of 20%, and a GROC of +4 at the beginning of the fourth session. Although some of these measurements did not meet published MCID values,34,35 the authors suggest that the thrust manipulation was the impetus for improvement demonstrated from the initial examination. This is supported by previous research, which has demonstrated dramatic, short-term beneficial effects following thrust manipulation.7,8,10-12,14,43 Finally, and perhaps most importantly, the authors realize that this is not the only reasoning framework that can be utilized to successfully treat individuals with thoracic pain. However, we suggest that focusing the sequence of treatment on motor task requirements of functional movement may provide more specific guidelines for the various phases of rehabilitation. Other manual therapy and neuromuscular rehabilitation approaches may have potentially resulted in similar patient outcomes. Independent of which approach one chooses to follow, the use of a sound reasoning paradigm for the development of the plan of care can provide physical therapists with the opportunity to deliver effective clinical care while meeting the demands of an ever changing healthcare system. Future studies should consider comparing different manual therapy and reasoning approaches in the management of younger individuals with primary complaints of thoracic pain in larger pilot or randomized clinical trials.
CONCLUSION
This case report described the successful management of an individual with thoracic spine pain using a clinical reasoning framework that encouraged the combination of manual therapy, neuromuscular re-education, and therapeutic exercises. While none of the interventions described are unique, this case report incorporated rationale for sequencing and selective implementation of common interventions across the episode of care that resulted in a return to pain-free functional movement.
APPENDIX.
Description of Select Interventions
| Manual Therapy | |
Soft Tissue Mobilization to Iliocostalis Thoracis (Mobility)
|
Patient position: prone, with head and neck in neutral. Therapist position: standing, at the side of the table, facing the patient. Instructions
|
Anterior to Posterior Rib 3-4 Mobilization (Mobility)
|
Patient position: supine, with head and neck in neutral. Therapist position: standing, at the side of the table, facing the patient. Instructions
|
Manipulation CTJ (Mobility)
|
Patient position: supine, with the head and neck in neutral Therapist position: standing, next to the patient Instructions
|
MET to Serratus Anterior (Mobility)
|
Patient position: sitting Therapist position: standing, behind the patient Instructions
|
| Neuromuscular Re-education | |
Concentric / Eccentric Contraction of Lower Trapezius (Stability)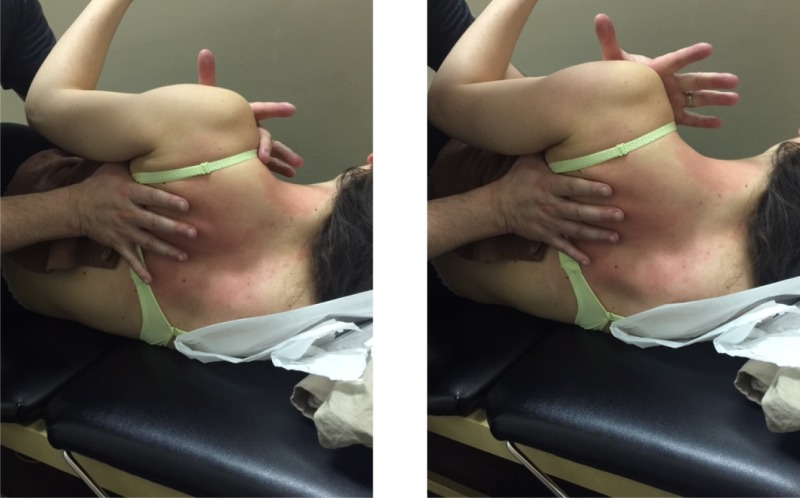
|
Patient position: right side lying, with the head and neck in neutral Therapist position: standing, next to the patient Instructions
|
Craniocervical Flexion (Stability)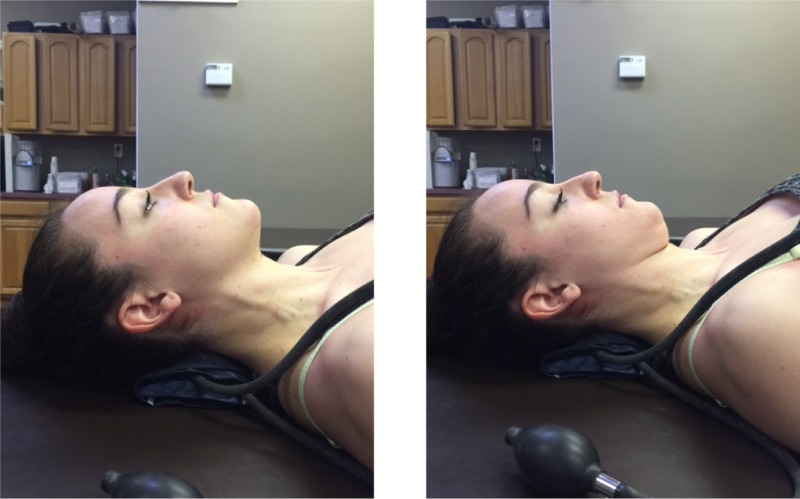
|
Patient position: supine, with the head resting on the table Instructions
|
| Therapeutic Exercise | |
Standing Scapular Retraction in Squat (Controlled Mobility)
|
Patient position: standing, in a slight squat Instructions
|
Left Lower Trapezius Strengthening (Controlled Mobility)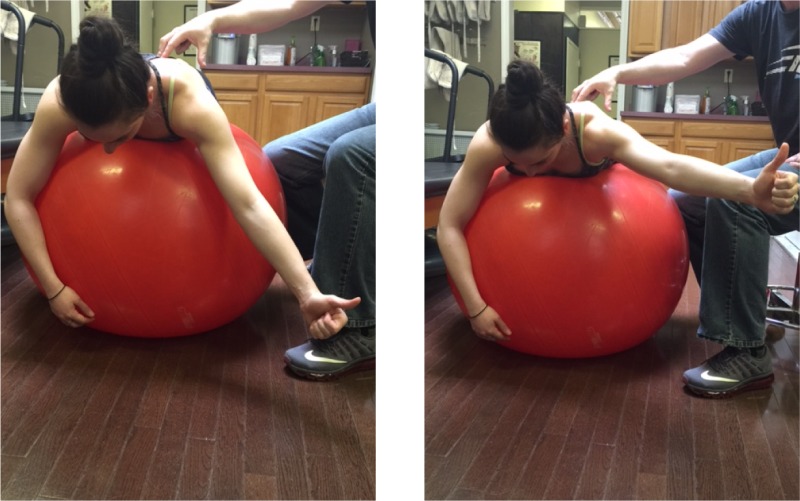
|
Patient position: prone, on a physioball Instructions
|
Left Middle Trapezius Strengthening (Controlled Mobility)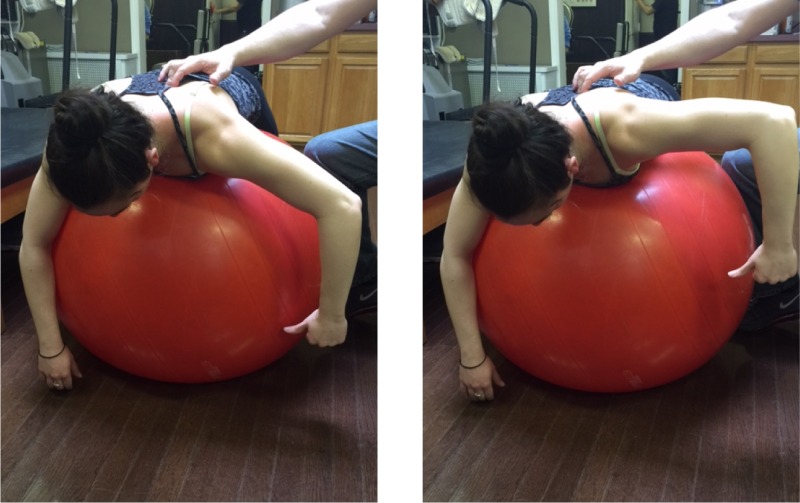
|
Patient position: prone, on a physioball Instructions
|
Left External Rotator Strengthening (Controlled Mobility)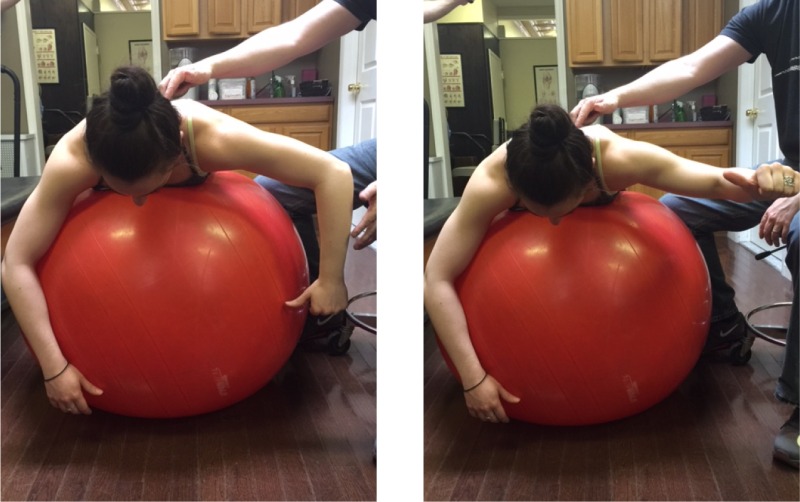
|
Patient position: prone, on a physioball Instructions
|
REFERENCES
- 1.Linton SJ, Hellsing AL, Hallden K. A population-based study of spinal pain among 35-45-year-old individuals. Prevalence, sick leave, and health care use. Spine (Phila Pa 1976). 1998;23:1457-1463. [DOI] [PubMed] [Google Scholar]
- 2.Dreyfuss P, Tibiletti C, Dreyer SJ. Thoracic zygapophyseal joint pain patterns. A study in normal volunteers. Spine (Phila Pa 1976). 1994;19:807-811. [DOI] [PubMed] [Google Scholar]
- 3.Fukui S, Ohseto K, Shiotani M. Patterns of pain induced by distending the thoracic zygapophyseal joints. Reg Anesth. 1997;22:332-336. [DOI] [PubMed] [Google Scholar]
- 4.Briggs AM, Bragge P, Smith AJ, Govil D, Straker LM. Prevalence and associated factors for thoracic spine pain in the adult working population: a literature review. J Occup Health. 2009;51:177-192. [DOI] [PubMed] [Google Scholar]
- 5.Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: A musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37:658-660. [DOI] [PubMed] [Google Scholar]
- 6.Childs JD, Cleland JA, Elliott JM, et al. Neck pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1-A34. [DOI] [PubMed] [Google Scholar]
- 7.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: Use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9-23. [DOI] [PubMed] [Google Scholar]
- 8.Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10:127-135. [DOI] [PubMed] [Google Scholar]
- 9.Cleland JA, Flynn TW, Childs JD, Eberhart S. The audible pop from thoracic spine thrust manipulation and its relation to short-term outcomes in patients with neck pain. J Man Manip Ther. 2007;15:143-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Phys Ther. 2007;87:431-440. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Iglesias J, Fernandez-de-las-Penas C, Cleland JA, Alburquerque-Sendin F, Palomeque-del-Cerro L, Mendez-Sanchez R. Inclusion of thoracic spine thrust manipulation into an electro-therapy/thermal program for the management of patients with acute mechanical neck pain: A randomized clinical trial. Man Ther. 2009;14:306-313. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez-Iglesias J, Fernandez-de-las-Penas C, Cleland JA, Gutierrez-Vega Mdel R. Thoracic spine manipulation for the management of patients with neck pain: A randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:20-27. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez-Iglesias J, Fernandez-de-Las-Penas C, Cleland JA, Huijbregts P, Del Rosario Gutierrez-Vega M. Short-term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: A randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515-521. [DOI] [PubMed] [Google Scholar]
- 14.Masaracchio M, Cleland JA, Hellman M, Hagins M. Short-term combined effects of thoracic spine thrust manipulation and cervical spine nonthrust manipulation in individuals with mechanical neck pain: A randomized clinical trial. J Orthop Sports Phys Ther. 2013;43:118-127. [DOI] [PubMed] [Google Scholar]
- 15.Mintken PE, Cleland JA, Carpenter KJ, Bieniek ML, Keirns M, Whitman JM. Some factors predict successful short-term outcomes in individuals with shoulder pain receiving cervicothoracic manipulation: a single-arm trial. Phys Ther. 2010;90:26-42. [DOI] [PubMed] [Google Scholar]
- 16.Strunce JB, Walker MJ, Boyles RE, Young BA. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17:230-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aiken DL, Vaughn D. The use of functional and traditional mobilization interventions in a patient with chronic thoracic pain: A case report. J Man Manip Ther. 2013;21:134-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chok B, Wong WP. Treatment of unilateral upper thoracic vertebral pain using an eclectic approach. Physiother Res Int. 2000;5:129-133. [DOI] [PubMed] [Google Scholar]
- 19.Fruth SJ. Differential diagnosis and treatment in a patient with posterior upper thoracic pain. Phys Ther. 2006;86:254-268. [PubMed] [Google Scholar]
- 20.Kelley JL, Whitney SL. The use of nonthrust manipulation in an adolescent for the treatment of thoracic pain and rib dysfunction: A case report. J Orthop Sports Phys Ther. 2006;36:887-892. [DOI] [PubMed] [Google Scholar]
- 21.Schiller L. Effectiveness of spinal manipulative therapy in the treatment of mechanical thoracic spine pain: A pilot randomized clinical trial. J Manipulative Physiol Ther. 2001;24:394-401. [DOI] [PubMed] [Google Scholar]
- 22.Olson KA. Manual Physical Therapy of the Spine. St. Louis, MI: Elsevier; 2009. [Google Scholar]
- 23.Brooker C. Mosby's 2013 Dictionary of Medicine, Nursing, and Health Professions. 9th ed. Edinburgh, Scotland: Elsevier; 2013. [Google Scholar]
- 24.Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. Clinical reasoning strategies in physical therapy. Phys Ther. 2004;84:312-330; discussion 331-315. [PubMed] [Google Scholar]
- 25.American Physical Therapy Association. Physical therapist practice and the human movement system. 2015; http://www.apta.org/MovementSystem/. Accessed April 27, 2016.
- 26.Delitto A. American Physical Therapy Association. Rothstein roundtable debates implementation of human movement system. Next Conference and Exposition; 2015.
- 27.O'Sullivan S, Portney L. Examination of motor function: Motor control and motor learning. In: O'Sullivan S Schmitz T, eds. Physical Rehabilitation. 5th ed. Philadelphia, PA: FA Davis; 2007. [Google Scholar]
- 28.Bertoti D. Functional Neurorehabilitation through the Lifespan. Philadelphia, PA: FA Davis; 2003. [Google Scholar]
- 29.Klein JG. Five pitfalls in decisions about diagnosis and prescribing. BMJ. 2005;330:781-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Griswold D, Learman K, O'Halloran B, Cleland J. A preliminary study comparing the use of cervical/upper thoracic mobilization and manipulation for individuals with mechanical neck pain. J Man Manip Ther. 2015;23:75-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: Clinical outcomes from the UCLA neck-pain study. Am J Public Health. 2002;92:1634-1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leaver AM, Maher CG, Herbert RD, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Arch Phys Med Rehabil. 2010;91:1313-1318. [DOI] [PubMed] [Google Scholar]
- 33.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005;30:1331-1334. [DOI] [PubMed] [Google Scholar]
- 34.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69-74. [DOI] [PubMed] [Google Scholar]
- 35.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Controlled Clinical Trials. 1989;10:407-415. [DOI] [PubMed] [Google Scholar]
- 36.MacDermid JC, Walton DM, Avery S, et al. Measurement properties of the neck disability index: A systematic review. J Orthop Sports Phys Ther. 2009;39:400-417. [DOI] [PubMed] [Google Scholar]
- 37.Vernon H, Mior S. The Neck Disability Index: A study of reliability and validity J Manipulative Physiol Ther. 1989;47:409-415. [PubMed] [Google Scholar]
- 38.Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: validation of its use in persons with neck dysfunction. J Orthop Sports Phys Ther. 1998;27:331-338. [DOI] [PubMed] [Google Scholar]
- 39.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31:598-602. [DOI] [PubMed] [Google Scholar]
- 40.Cleland JA, Selleck B, Stowell T, Browne L, St. Cyr H, Caron T. Short-term effects of thoracic manipulation on lower trapezius muscle strength. J Man Manip Ther. 2004;12:82-90. [Google Scholar]
- 41.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Sullivan S. Strategies to improve motor function. In: Schmitz T O'Sullivan S Fulk G, eds. Physical Rehabilitation. 6th ed. Philadelphia, PA.: F.A. Davis; 2014. [Google Scholar]
- 43.Boyles RE, Ritland BM, Miracle BM, et al. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther. 2009;14:375-380. [DOI] [PubMed] [Google Scholar]