Abstract
Hereditary spastic paraplegias (HSP) are the second most common type of motor neuron disease recognized worldwide. We investigated a total of 25 consanguineous families from Sudan. We used next-generation sequencing to screen 74 HSP-related genes in 23 families. Linkage analysis and candidate gene sequencing was performed in two other families. We established a genetic diagnosis in six families with autosomal recessive HSP (SPG11 in three families and TFG/SPG57, SACS and ALS2 in one family each). A heterozygous mutation in a gene involved in an autosomal dominant HSP (ATL1/SPG3A) was also identified in one additional family. Six out of seven identified variants were novel. The c.64C>T (p.(Arg22Trp)) TFG/SPG57 variant (PB1 domain) is the second identified that underlies HSP, and we demonstrated its impact on TFG oligomerization in vitro. Patients did not present with visual impairment as observed in a previously reported SPG57 family (c.316C>T (p.(Arg106Cys)) in coiled-coil domain), suggesting unique contributions of the PB1 and coiled-coil domains in TFG complex formation/function and a possible phenotype correlation to variant location. Some families manifested marked phenotypic variations implying the possibility of modifier factors complicated by high inbreeding. Finally, additional genetic heterogeneity is expected in HSP Sudanese families. The remaining families might unravel new genes or uncommon modes of inheritance.
Introduction
Hereditary spastic paraplegias (HSP) and hereditary ataxias (HA) represent the extremes on the spectrum of spinocerebellar neurodegenerative disorders. They are often correlated and impose diagnostic difficulty, especially with other overlapping neurodegenerative disorders.1 They can be transmitted by all modes of inheritance.1, 2, 3, 4, 5 The core defining clinical features of HSP are insidiously progressive weakness and spasticity of the lower extremities. HSP has a prevalence of 3–10 per 100 000 in most populations.6 Prevalence of autosomal dominant (AD) HSP ranges between 0.5 and 5.5 per 100 000 individuals and that of autosomal recessive (AR) HSP between 0.3 and 5.3 per 100 000 individuals.7 HSP can be pure (uncomplicated) or complex according to the absence or presence of additional neurological and non-neurological manifestations. There are >67 known HSP genes.1 AD HSP forms are the most frequent in western populations. SPG4, SPG3A, SPG10 and SPG31 account for up to 50% of AD HSP. SPG3A (ATL1) alone accounts for ~10% of AD HSP.8 On the contrary, AR HSP predominates in highly consanguineous communities.7, 9, 10 Thin corpus callosum-associated HSP (TCC-HSP) represents a distinct subgroup accounting for approximately one-third of all AR HSP.11 At least nine genes have been identified to be responsible for TCC-HSP. They include SPG1, SPG11, SPG15, SPG18, SPG21, SPG32, SPG46 and SPG49/56 and in rare cases, SPG7. Disease causing variants in SPG11 (KIAA1840) (OMIM phenotype #604360) constitute the most frequent cause of TCC-associated HSP (41–77%) and up to for 10–20% of all AR HSP, particularly in the Mediterranean basin.6, 10, 12, 13, 14, 15, 16 Next-generation sequencing aided in the identification of many rare HSP genes.1, 17 TFG/SPG57 stands as an example of this genetic surge. TFG is a highly conserved regulator of protein secretion and functions at the interface between the endoplasmic reticulum (ER) and ER–golgi intermediate compartments. Variants in TFG were implicated in SPOAN-like HSP (spastic paraplegia, optic atrophy, neuropathy)18 and hereditary sensory motor neuropathy with proximal predominant involvement (HSMN-P).19 Spastic ataxias now stand as a distinct disease category. Autosomal Recessive Spastic Ataxia of Charlevoix Saguenay (ARSACS) (OMIM phenotype #270550) shows a challenging phenotypic overlap with HSP and HA, with a remarkable clinical diversity.20, 21, 22 ALS2 (Alsin) (OMIM gene *606352) is another prominent example of a gene implicated in pyramidal syndromes, with overlapping roles in other neurodegenerative conditions including amyotrophic lateral sclerosis.23
Relatively little is known about the genetics of spinocerebellar degenerations in the Sudanese population.24 In this article, we studied 25 families with progressive spastic neurodegenerative disorders in an effort to determine the genes underlying the disease. We report the first seven Sudanese families carrying novel and rare variants in KIAA1840 (SPG11), TFG/SPG57, ATL1 (SPG3A), ALS2 and SACS. Using in vitro biochemical experiments, we demonstrate the pathological effect of a novel TFG variant. Further genetic heterogeneity of HSP is also highlighted.
Materials and methods
Ethical approval
This study was prospectively reviewed and approved by the Paris Necker Ethics Committee (France) and the Ethical Committee of the University of Khartoum Medical Campus (Sudan). It was conducted in accordance with the recommendation of the Declaration of Helsinki. A written informed consent was obtained from all participants.
Subjects recruitment
We investigated 25 consanguineous Sudanese families (of various ethnic backgrounds and with multiple consanguinity loops). The total number of patients sampled in these families was 65 patients. In each family, we recruited the proband along with all accessible diseased family members and available unaffected first-, second- and third-degree relatives when possible. Inclusion criteria for patients were clinical presentation suggestive of spastic neurodegeneration plus familial consanguinity and/or positive family history of neurodegenerative disorders. Alternative diagnoses were excluded.
Clinical phenotyping
Patients were examined and diagnosed by the referring consultant neurologists/neuro-pediatricians, followed by a second standardized phenotyping by the research team. Healthy related controls were examined to exclude subtle disorders. Patients were assessed for motor disability using a Seven-Stage Disability Score (Supplementary Tables 1 and 2). Magnetic resonance imaging (MRI) of the brain was performed for at least one patient per family in most cases.
Sampling and DNA purification
Two milliliters of saliva were collected using Oragene.Discover DNA collection kits (DNA Genotek Inc., Ottawa, ON, Canada). DNA purification was done according to the prepIT.L2P manual protocol provided by the manufacturer. DNA quality and quantity control were performed using standard Agarose gel electrophoresis, NanoDrop spectrophotometer (Thermo Scientific, Wilmington, DE, USA) and Qubit fluorometer (Promega, Madison, WI, USA).
Genetic linkage analysis
We performed linkage analysis to screen two families (10 patients and 31 healthy relatives) for candidate loci based on patients’ clinical presentation, brain imaging and previously known relative frequencies of HSP genetic mutations. We used microsatellite markers (list available upon request) flanking the CYP7B1 (SPG5), KIAA1840 (SPG11), ZFYVE26 (SPG15), GBA2 (SPG46), CYP2U1 (SPG49/SPG56) and SACS genes. Classical procedures were used for their PCR amplification and allelic resolution in an ABI3730 sequencer (Applied Biosystems, Foster City, CA, USA). Peak Scanner software (Applied Biosystems) was utilized for analysis of product length. Haplotypes were then manually reconstructed for each locus and pedigree in order to obtain the minimum number of recombination events.
Targeted next-generation sequencing screening panel
We used a multi-gene targeted next-generation exome-sequencing panel to screen the remaining 23 (out of 25) HSP families. The total number of patients in these families was 55 patients. However, an index patient(s) in each family underwent exome panel screening, whereas samples from the remaining patients were used to test the segregation of candidate variants. The panel (Supplementary 3) covered a total of 74 genes including 68 genes previously implicated in a variety of spastic disorders1 and six unpublished candidate genes. In total, 1042 exonic regions with total length of 220 095 bp were targeted. Twenty base pairs of flanking intronic sequences were included, whereas promotors and UTRs were excluded. NimbleGen/SeqCap Ez enrichment system was used (Roche, Madison, WI, USA). Sequencing was performed using MiSeq platform (Illumina, San Diego, CA, USA) on 250 bp paired-end reads. Variant calling and quality control were performed using Genomics Workbench (CLC Bio, Aarhus, Denmark). Short variations (SNVs and Indels) were detected using probability-based and quality-based algorithms. Large variations (duplications and large deletions) and zero-coverage exons were examined as well through the analysis of the coverage results. For gene/variant prioritization, nonsense, frameshift, splice site and missense variants with a minimum depth of 30 × were selected. Minor allele frequency cutoff of 1.5% was used first then decreased to 0.1% for more stringency. Five pathogenicity prediction algorithms were used to predict the effect of missense variants (SIFT, Polyphen-2, Mutation Taster, Align GVGD, KD4v). PhastCons and PhyloP conservation scores were used to indicate conservation. For splicing sites prioritization, five tools (Human Splicing Finder, SpliceSiteFinder–Like, Gene Splicer, NNSPLICE, MaxEntScan) were used. All tools were collectively provided by AlamutVisual software (Interactive Biosoftware, Rouen, France). Using these criteria, heterozygous variants in AD families and homozygous variants in families with AR inheritance were considered as candidate variants. Heterozygous variants in AR pedigrees were examined to exclude the presence of compound heterozygous inheritance. Exons with one (or more) base pair(s) with less 30 × coverage were sequenced (Sanger sequencing) in all genes in which a single heterozygous variant was found to exclude missing variants due to low coverage.
Sanger sequencing
We performed Sanger sequencing using the BIGDYE chemistry on an ABI3730 sequencer (Applied Biosystems) to validate candidate variants in index patients and to confirm their co-segregation with the disease distribution within each family. Bioinformatic sequence analysis was performed using Seqscape (Applied Biosystems) and Chromas lite software (Technelysium, South Brisbane, QLD, Australia).
Submission to locus specific databases
Variants were submitted to Leiden Open Variation Database available at: http://databases.lovd.nl/shared/variants/ with the following variant IDs: 0000090056 (SPG11, c.6709del), 0000090058 (SPG11, c.3568A>T), 0000090050 (SPG11, c.6349G>T), 0000090062 (TFG, c.64C>T), 0000090063 (SACS, c.7739G>A), 0000090069 (ALS2, c.368G>A), 0000090064 (ATL1, c.452T>C).
Biochemistry
We conducted a series of size-exclusion chromatography studies, coupled to multi-angle light scattering (to accurately determine absolute protein molecular mass) to determine whether the novel TFG c.64C>T variant impacts the homo-oligomeric properties of the TFG PB1 domain. Recombinant TFG proteins (amino acids 1–96) were expressed as fusions to glutathione-S-transferase (GST) using Escherichia coli BL21 (DE3). Purifications were conducted using glutathione agarose beads. Proteins were cleaved from resin with GST-HRV3C protease overnight at 4 °C and purified further using ion exchange chromatography. Light-scattering data were collected as described previously.18 In brief, purified proteins were applied onto a high-resolution size-exclusion chromatography column (WTC-030S5, Wyatt Technology, Santa Barbara, CA, USA), which was coupled to a three-angle light-scattering detector (miniDAWN TREOS, Wyatt Technology). Data were collected at a flow rate of 0.5 ml/min and analyzed (ASTRA software, Wyatt Technology) to determine the molecular mass of TFG proteins.
Results
Description of the cohort
All investigated 25 families were consanguineous. The majority of these showed a probable AR inheritance with multiple affected individuals (15 families; 60%), whereas some pedigrees featured only one patient despite the consanguinity (seven families; 28%). Few were consistent with a dominant inheritance pattern, although pseudo-dominant autosomal inheritance cannot be excluded (three families; 12%). In these 25 families, a complex phenotype was predominant (21/25 families; 84%).
In total, genetic diagnosis was established in seven families (28%). The genetics and phenotype–genotype correlations of these families with a genetic diagnosis are presented in the following sections. In the remaining 18 families yet to have a confirmed genetic diagnosis, two families presented with pure HSP, six families showed complex HSP, whereas 10 families presented with spastic ataxia. HSP cases were complicated by stereotypic movement (2/18), bulbar signs and sensory motor polyneuropathy (1/18), cognitive decline (1/18), dystonia (1/18) or severe cortical atrophy (1/18). Spastic ataxia was complicated with dysmorphic features (2/18), chorea (1/18) and visual impairment (3/18).
Genetic results
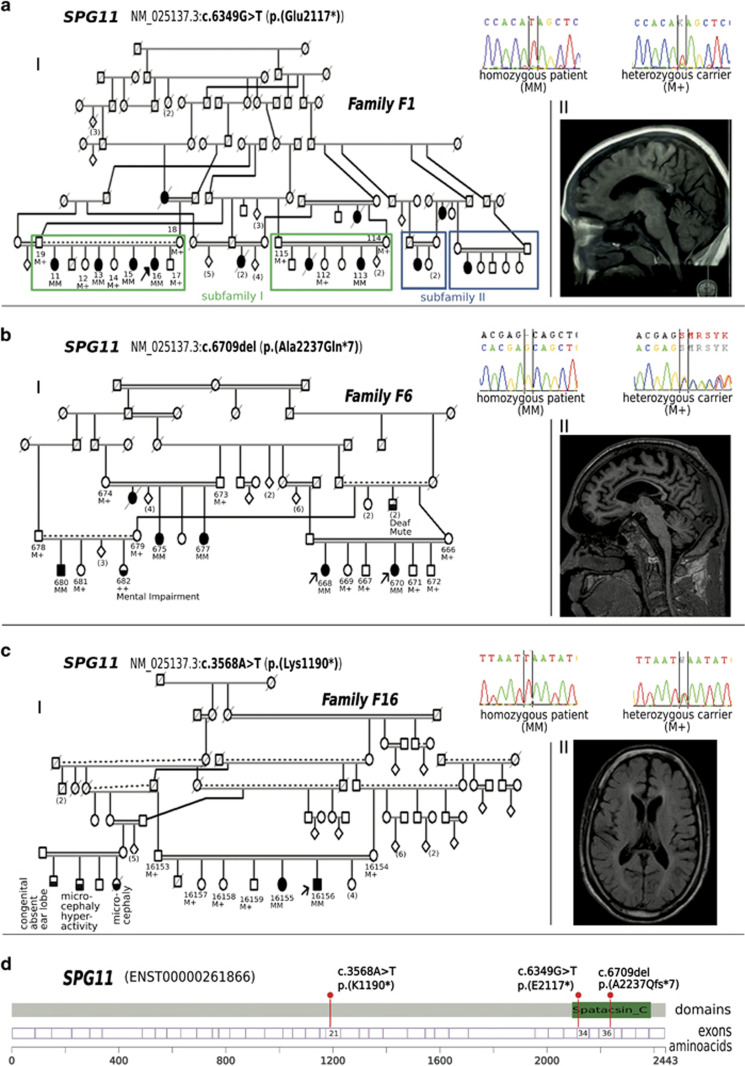
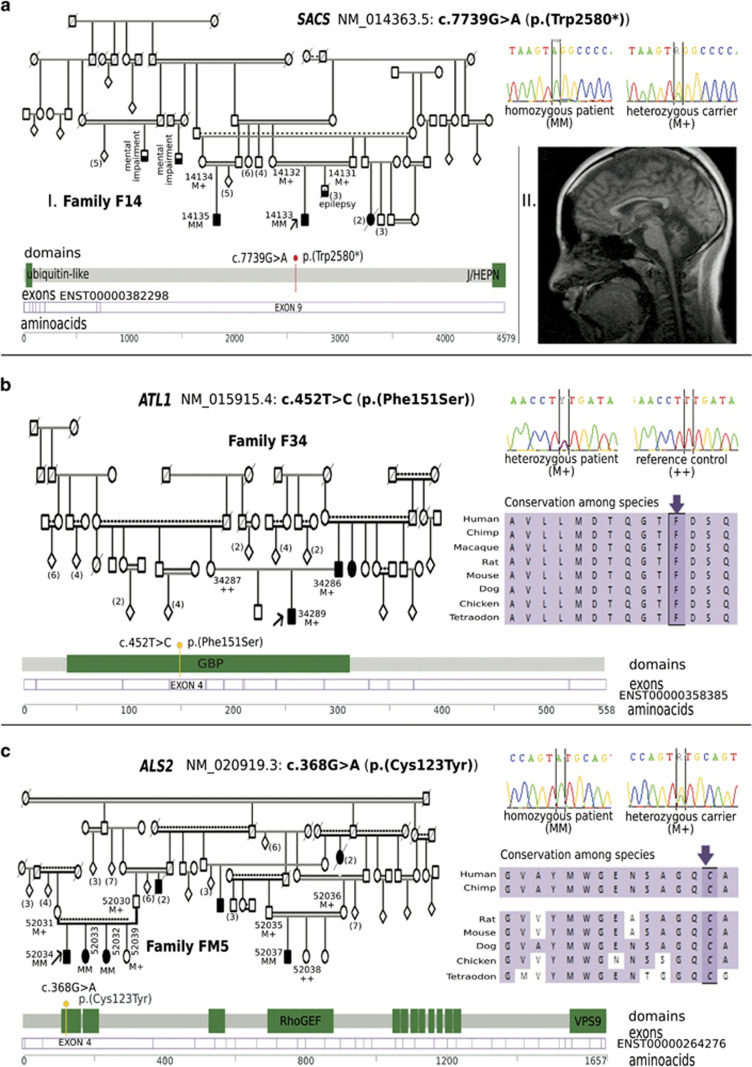
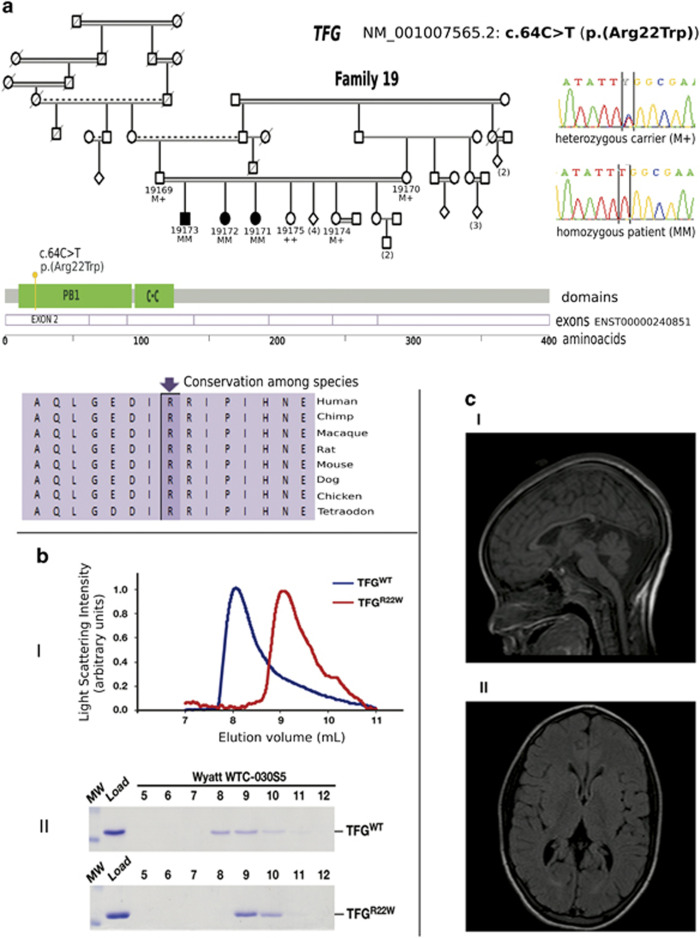
In two families, homozygous microsatellite haplotypes surrounding the SPG11 locus segregated with the disease (data not shown). Sanger sequencing confirmed the segregation of two homozygous SPG11 variants, one in each family: c.6349G>T and c.6709del (Figure 1). Using a multi-gene NGS panel, causative variants were identified in other five families: SPG11 c.3568A>T, TFG/SPG57 c.64C>T, ATL1 c.452T>C, ALS2 c.368G>A and SACS c.7739G>A (Figures 1–3). Table 1 shows the details of these variants. All variants were novel except the SPG11 c.6709del variant, which was reported previously in a Somalian patient.25 All variants co-segregated with the disease in the families and were absent from large sets of databases including 1000 Genomes, EVS, Broad institute ExAC and our local institutional databases. Missense variants were predicted to be deleterious by at least three pathogenicity prediction algorithms and affected highly conserved amino acids (Table 1). No pathological variant in an unexpected zygosity, zero-coverage exons or large rearrangements (for example, deletions/duplications) were identified. We found rare deleterious heterozygous variants in our cases that did not conform to the mode of inheritance in the families and were not considered as causative mutations (Supplementary Table 4).
Figure 1.
Families F1, F6 and F16 with autosomal recessive hereditary spastic paraplegia with thin corpus callosum (TCC) caused by SPG11 variants. (a (I)) Pedigree of family F1 in which a nonsense variant segregates with the disease in subfamily I. Electrophoregrams show the variant in a homozygous patient and a heterozygous carrier. Subfamily II showed dissimilarities in HSP phenotypes. (a (II)) Brain MRI (sagittal T1W section) of an SPG11 patient showing severe TCC. (b (I)) Pedigree of family F6 showing the segregation of a frameshift variant. Electropherograms show the variant in a patient (homozygous) and in a heterozygous carrier. (b (II)) Brain MRI (sagittal T1W section) of the index patient showing severe TCC and cortical atrophy. (c (I)) Pedigree of family F16 showing the segregation of a nonsense variant. Electropherograms show the variant in a patient (homozygous mutant) and in a heterozygous carrier. (c (II)) Brain MRI (axial T2 FLAIR) of the index patient showing TCC and periventricular hyperintensities. (d) SPG11 gene model showing the position of detected variants as red lollipops. Pedigree symbols: full shading indicates affected individuals, half horizontal shading indicates other diseases, numbers between brackets are multiple siblings, diamonds indicate multiple siblings of different sex. Individual ID numbers and genotypes are indicated. Genotypes: ++ homozygous reference; M+ heterozygous; MM homozygous mutant. Others are standard medical pedigree symbols.
Figure 3.
Families F14, F34 and FM5 with spastic ataxia and hereditary spastic paraplegia caused by SACS, SPG3A and ALS2 variants. (a (I)) Pedigree of family F14 with recessive spastic ataxia of Charlevoix Saguenay (ARSACS) caused by a nonsense variant in SACS. Other diseases are seen in the family. Electropherograms show the variant in a patient (homozygous mutant) and a heterozygous carrier. (a (II)) Brain MRI (Sagittal section T1W) of individual 14133 showing thinning of the posterior half of the body of corpus callosum and moderate thinning of cerebellum. (b) Pedigree of Family F34 with autosomal dominant HSP caused by a missense variant in ATL1. Electropherograms show the variant in a patient (heterozygous) and a control (reference alleles). (c) Pedigree of family FM5 with autosomal recessive HSP caused by missense variant in ALS2. Electropherograms are shown for a patient (homozygous mutant) and a heterozygous carrier. Pedigree symbols: shading indicates affected individuals, numbers between brackets are multiple siblings, diamonds indicate multiple siblings of different sex. Individual ID numbers and genotypes are indicated. Gene models show the position of detected variant in each gene. For missense variants (b and c) conservation of the (predicted) affected amino-acid is shown.
Table 1. Hereditary spastic paraplegia variants identified in seven studied families.
| Conservation | Predicted pathogenicity | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Family code | No. of patients | Gene | Transcript | Ensembl transcript | cDNA change | Exon | Protein change | Consequence | Zygosity | PhastCons | PhyloP | SIFT | Polyphen-2 | Mutation taster | Align GVGD | First report |
| F1 | 5 | SPG11 | NM_025137.3 | ENST00000261866 | c.6349G>T | 34 | p.(Glu2117*) | NS | Hom | 1.0 | 6.02 | NA | NA | NA | NA | This article |
| F6 | 5 | SPG11 | NM_025137.3 | ENST00000261866 | c.6709del | 36 | p.(Ala2237Glnfs*7) | FS | Hom | 1.0 | 6.02 | NA | NA | NA | NA | DeBot et al.23 |
| F16 | 2 | SPG11 | NM_025137.3 | ENST00000261866 | c.3568A>T | 21 | p.(Lys1190*) | NS | Hom | 1.0 | 4.0 | NA | NA | NA | NA | This article |
| F14 | 3 | SACS | NM_014363.5 | ENST00000382298 | c.7739G>A | 10 | p.(Trp2580*) | NS | Hom | 1.0 | 6.10 | NA | NA | NA | NA | This article |
| F19 | 2 | SPG57 (TFG) | NM_001007565.2 | ENST00000490574 | c.64C>T | 2 | p.(Arg22Trp) | MS | Hom | 1.0 | 0.85 | Deleter. | Prob. damag. | Disease causing | Deleter. | This article |
| F34 | 2 | ATL1 | NM_015915.4 | ENST00000358385 | c.452T>C | 5 | p.(Phe151Ser) | MS | Het | 1.0 | 4.81 | Deleter | Prob. damag. | Disease causing | Deleter. | This article |
| FM5 | 4 | ALS2 | NM_020919.3 | ENST00000264276 | c.368G>A | 4 | p.(Cys123Tyr) | MS | Hom | 1.0 | 6.02 | Deleter. | Prob. damag. | Disease causing | Benign | This article |
Abbreviations: NS, nonsense; Deleter., deleterious; Het, heterozygous; Hom, homozygous; NA, not applicable; Prob. damag., probably damaging; MS, missense. Allele frequencies were zero in four databases (dbSNP, 1000Genome, EVS, ExAC). PhastCons score ranges from zero (low conservation) to 1 (high conservation), Phylop score from −14.1 (low conservation) to 6.4 (high conservation). No. of patients: the number of patients who were genetically investigated and showed the designated variants.
Phenotype–genotype correlations
Clinical data from seven families (23 patients) with established genetic diagnosis is presented (Tables 2 and 3). A summary of the MRI and electrophysiological investigations is also provided (Table 4).
Table 2. Clinical data of 12 patients from three families with SPG11 genetic diagnosis.
| Family code | F1 A | F1 A | F1 A | F1 A | F1 B | F6 A | F6 A | F6 B | F6 B | F6 C | F16 | F16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mutated gene | SPG11/KIAA1840 | SPG11/KIAA1840 | SPG11/KIAA1840 | |||||||||
| Individual code | 11 | 13 | 15 | 16 | 113 | 668 | 670 | 675 | 677 | 680 | 16155 | 16156 |
| Gender | F | F | F | F | F | F | F | F | F | M | F | M |
| Clinical diagnosis | Complex spastic ataxia | Complex spastic ataxia | Complex spastic ataxia | |||||||||
| Origin | Gezira, Central Sudan | Halfa, North Sudan | Gezira, Central Sudan | |||||||||
| Age at onset of motor symptoms | 20 Yrs | 20 Yrs | 19 Yrs | 24 Yrs | 13 Yrs | 17 Yrs | 15 Yrs | 12 Yrs | 15 Yrs | 10 Yrs | 16 Yrs | 13 Yrs |
| Age at initial examination | 49 Yrs | 43 Yrs | 36 Yrs | 29 Yrs | 47 Yrs | 29 Yrs | 26 Yrs | 39 Yrs | 32 Yrs | 30 Yrs | 19 Yrs | 23 Yrs |
| Spasticity UL/LL | +++/+++ | ++/+++ | ++/+++ | ++/++ | +++/+++ | ++/+++ | +/+++ | +/+++ | +/+ | +/+ | −/++ | −/++ |
| Motor deficit PUL/DUL | ++/+++ | ++/+++ | ++/+++ | −/++ | +++/+++ | +/+ | +/+ | +/+ | −/+ | −/+ | −/− | −/− |
| Motor deficit PLL/DLL | +++/+++ | +++/+++ | +++/+++ | +/++ | +++/+++ | ++/++ | +++/+++ | +++/+++ | +/+ | +++/+++ | ++/+ | ++/++ |
| Reflexes: UL/LL patellar | ↑/↑ | ↑/↑ | ↑/↑ | N/↑ | ↑/↑ | ↑/↑ | ↑/↑ | ↑/↑ | N/N | ↑/↑ | ↑/↑ | N/N |
| Reflexes: ankle/planter | ↓/↑↑ | ↑/↑↑ | ↑/↑↑ | ↑/↑↑ | ↑/↔ | ↑/↑↑ | ↑/↑↑ | ↑/↑↑ | ↑/↔ | ↑/↑↑ | ↑/↑↑ | ↑/↔ |
| Ataxia: Eye | − | − | + | + | − | − | − | − | − | − | − | − |
| Ataxia UL/LL | ++/NA | ++/NA | +++/NA | ++/++ | NA/NA | +/NA | +/NA | ++/NA | +/+ | −/NA | −/− | +++/NA |
| Gait ataxia | NA | NA | NA | ++ | NA | + | − | NA | ++ | NA | ++ | +++ |
| Dysarthria spastic/cereb. | ++/+ | ++ | ++ | ++ | +++/NA | +/+ | ++/++ | +++/+++ | −/++ | ++/− | −/− | −/++ |
| Muscle atrophy DUL/DLL | ++/++ | ++/++ | +++/+++ | +/+ | +++/+++ | −/− | −/− | −/− | −/− | −/+++ | −/− | ++/++ |
| Facial atrophy | − | − | + | − | + | − | − | − | − | − | − | + |
| Cog/Psych signs | +/+ | +/+ | +/+ | −/− | +/+ | −/− | −/− | +/+ | +/− | +/− | +/+ | +/+ |
| Optic atrophy | − | − | − | − | + | − | − | NA | − | − | − | − |
| Extrapyramidal signs | − | − | Resting tremor, rigidity | − | − | − | − | − | − | Hypokinesia | − | Hypokinesia, rigidity |
| Sensory loss | − | − | − | − | NA | − | − | − | − | − | − | − |
| Other signs | Dysphagia, urgency | Dysphagia, urgency | Dysphagia, urgency | Urgency | Dysphagia, urgency, died at 47.5 Yrs | Irreg. menses, urgency | Urgency | Incontinence | Urgency | Incontinence | − | − |
Abbreviations: Cereb, cerebellar; Cog, cognitive; DUL/DLL, distal upper/lower limbs; LL, lower limbs; N: normal; NA, not applicable due to patients’ condition; PBP, pseudobulbar palsy; Psych, psychological; PUL/PLL, proximal upper/lower limbs; UL, upper limbs. Clinical signs severity: – absent, + mild, ++ moderate, +++ severe. Tendon reflexes: ↑ Increased tendon reflex. ↓ Diminished reflex. Extensor Planter response: ↑ unilateral, ↑↑ bilateral, ↔ mute, ↓ flexor. The resulting disability stage is given in Supplementary Table 2.
Table 3. Clinical data of 11 patients from four families with SPG57, ATL1, ALS2 and SACS genetic diagnosis.
| Family code | F19 | F19 | F19 | F34 | F34 | FM5 | FM5 | FM5 | FM5 | F14 A | F14 B |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mutated gene | TFG/SPG57 | ATL1 | ALS2 | SACS | |||||||
| Individual code | 19171 | 19172 | 19173 | 34286 | 34289 | 52032 | 52033 | 52034 | 52037 | 14133 | 14135 |
| Gender | F | F | M | M | M | F | F | M | M | M | M |
| Clinical diagnosis | Complex HSP | Pure HSP | Complex spasticity, PBP | Complex spastic ataxia | |||||||
| Origin | Sinnar, Eastern Sudan | Dongola, North Sudan | Soba, Central Sudan | White Nile, Central Sudan | |||||||
| Age at onset of motor symptoms | 1 Yrs | 10 Months | 14 Months | 7 Yrs | 19 Months | 3 Months | 4 Months | 12 Months | 18 Months | 11 Yrs | 10 Yrs |
| Age at initial examination | 15 Yrs | 8 Yrs | 4 Yrs | 38 Yrs | 5.5 yrs | 18 Yrs | 13 Yrs | 11 Yrs | 11 Yrs | 38 Yrs | 24 Yrs |
| Spasticity UL/LL | ++/+++ | +/++ | ++/++ | −/++ | −/+ | ++/+++ | ++/+++ | ++/+++ | ++/+++ | −/+ | −/+ |
| Motor deficit PUL/DUL | +/+ | −/− | +/+ | −/− | −/− | +/++ | +/+ | −/− | +/+ | −/− | -/++ |
| Motor deficit PLL/DLL | ++/+++ | ++/+++ | ++/++ | +/− | ++/− | +++/+++ | ++/− | −/− | +++/+++ | +/− | +/+ |
| Tendon reflexes UL/LL patellar | ↑/↑ | ↑/↑ | ↑/↑ | N/↑ | N/↑ | ↑/↑ | ↑/↑ | ↑/↑ | ↑/↑ | N/↓ | ↑/↑ |
| Ankle reflex/planter response | ↑/↑↑ | ↑/↑↑ | N/↑↑ | ↑/↑↑ | ↑/↑ | ↑/↑ | ↑/↔ | ↑/↓ | ↑/↑↑ | ↓/↑ | ↑/↑ |
| Ataxia eye/UL/LL/gait | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | −/−/−/− | +/++/+++/+++ | +/−/+/+ |
| Dysarthria spastic/cerebellar | −/− | −/− | −/− | −/− | −/− | Anarthric | +++/− | +++/− | +++/− | −/+ | −/− |
| Muscle atrophy DUL/DLL | −/− | −/− | −/− | −/++ | −/− | +++/+++ | −/+ | −/− | −/− | +/+ | ++/++ |
| Facial atrophy | − | − | − | − | − | − | − | − | − | − | − |
| Cog/psych | +/− | +/− | +/− | −/− | −/− | −/− | −/− | −/− | −/− | +/+ | +/+ |
| Optic atrophy | − | − | − | − | − | − | − | − | − | − | − |
| Extrapyramidal Signs | − | − | − | − | − | − | − | − | − | −/− | −/− |
| Sensation | Intact | Intact | Intact | Intact | Intact | Intact | Intact | Intact | Intact | Vibration sense lost | Intact |
| Other signs | Microcephaly | − | Microcephaly | − | − | Dysphagia, Involuntary laughter | Involuntary laughter | Involuntary laughter | − | Absent morning erection | Absent morning erection, urgency, epilepsy |
Abbreviations: Cog, cognitive; DUL/DLL, distal upper/lower limbs; LL, lower limbs; N: normal; NA, not applicable due to patients’ condition; PBP, pseudobulbar palsy; Psych, psychological; PUL/PLL, proximal upper/lower limbs; UL, upper limbs. Clinical signs severity: – absent, + mild, ++ moderate, +++ severe. Tendon reflexes: ↑ Increased tendon reflex. ↓ Diminished reflex. Extensor Planter response: ↑ unilateral, ↑↑ bilateral, ↔ mute, ↓ flexor. The resulting disability stage is given in Supplementary Table 2.
Table 4. Available radiological (MRI brain) and electrophysiological (NCS) data of 11 patients (from five of the seven families with genetic diagnoses).
| Family code | Individual code | Gene affected | Magnetic resonance imaging of the brain (MRI) | Electrophysiological studies (NCS) |
|---|---|---|---|---|
| F1 | 16 | SPG11 | Severe generalized TCC | UL and LL motor demyelination. UL motor and sensory axonal degeneration. Normal sensory response in LL |
| F6 | 668 | SPG11 | Generalized TCC (anterior more marked). Cortical atrophy, PVWMHS | NA |
| F6 | 670 | SPG11 | Generalized TCC (anterior more marked), Cortical atrophy, PVWMHS | NA |
| F6 | 680 | SPG11 | Severe TCC (genu, body and to a lesser extent the splenium). PVWMHS (frontal horns). Generalized cerebral atrophy. Mild cerebellar atrophy | Severe signs of motor demyelination and axonal degeneration (CPN, Rt TN) Normal sensory response (SN) |
| F16 | 16155 | SPG11 | Generalized TCC. Mild cortical atrophy. PVWMHS | Motor demyelination changes (TN, CPN). Normal sensory response (SN) |
| F16 | 16156 | SPG11 | Mild generalized TCC. Mild cerebral atrophy. PVWMHS. Moderate cerebellar atrophy | Remarkable motor demyelination changes (TN, CPN). Adequate sensory response (SN) |
| F19 | 19171 | TFG/SPG57 | Focal TCC (body). Mild degree of cerebellar atrophy | Signs of motor demyelination (TN, CPN). Motor axonal degeneration (CPN) |
| F19 | 19172 | TFG/SPG57 | Mild thinning of the body of CC. Mild cerebellar atrophy. Very mild PVWMHS at the occipital horns | Signs of motor demyelination (Lt TN, Both CPN) |
| F19 | 19173 | TFG/SPG57 | Mild degree of cerebellar atrophy | Mild demyelination of both Rt and Lt TN (Motor) |
| F14 | 14133 | SACS | TCC (posterior half of the body). Moderate cerebellar atrophy | Very severe sensory (SN) and motor axonal degeneration (Lt TN, Both CPN) |
| F14 | 14135 | SACS | Focal TCC (posterior half of the body). Mild cerebral atrophy (frontal lobes mainly). Mild cerebellar atrophy | Severe distal motor axonal degeneration (Rt TN and Rt CPN). Absent sensory response (SN) |
Abbreviations: CPN, common peroneal nerve; LL, lower limb; Lt, left; MRI, magnetic resonance imaging; NA, not available; NCS, nerve conduction studies; PVWMHS, periventricular white matter hyperintense signal; RT, right; SN, sural nerve; TCC, thin corpus callosum; TN, tibial nerve; UL, upper limb.
Patients from three families with variants in SPG11 presented with a complex HSP associated frequently with cognitive deficit. MRI and electrophysiological findings matched previous reports.26, 27 MRI of the brain showed atrophy of the corpus callosum in six tested cases, often associated with periventricular white matter abnormalities (Figure 1). Signs of motor demyelination frequently mixed with axonal degeneration were found in electrophysiological examination.
In family F14, the phenotypic presentation varied between patients from different branches. The two affected individuals in this family (cousins) had the same variant (SACS c.7739G>A) but showed interesting clinical differences. Both had spastic ataxia but one showed predominant ataxia and peripheral neuropathy whereas the other had predominant spastic paraparesis. Age at onset was late childhood in agreement with Baets et al.28 and higher than what was reported in Tunisian patients.29 Both patients had absent fundal striations in accordance with previous reports of Italian patients30, 31 and Japanese sibship.32 The family history revealed three brothers who were clinically diagnosed with Laurence Moon Biedl syndrome and died from renal failure years ago (suggesting a second segregating disease gene within the same family, although this was not genetically analyzed).
In three families with variants in ATL1, ALS2 and TFG (F34, FM5 and F19, respectively), we observed homogeneous clinical patterns in all patients within each family. Family F34 had rather unusual characteristics in our cohort with pure HSP and dominant inheritance (heterozygous variant) despite the high consanguinity in this family. The presentation (Table 3) matched the classical clinical pattern and the early age of onset associated with SPG3A.33 In family FM5, four patients from two branches presented with infantile onset progressive pyramidal syndrome with pseudobulbar palsy. This is in conformity with what was reported in Infantile Onset Ascending Spastic Paralysis associated with Alsin variants (OMIM #607225) (Table 3).34, 35, 36
Interestingly, disease phenotypes in family F19 extended the clinical spectrum associated with TFG/SPG57 variants. As in first SPG57 family (c.316C>T), the mean age at onset in the three affected sibs was around 1 year. They presented with signs of progressive pyramidal tract involvement. In contrast to the SPOAN-like HSP reported by Beetz et al.,18 patients in this family with a second novel variant (c.64C>T) had intact optic nerve and normal fundi. The electrophysiological studies confirmed variable degrees of motor neuronal demyelination in addition to motor axonal degeneration matching the previous report. Although brain MRI revealed no significant abnormalities in the first family, we report thinning of the corpus callosum, variable degrees of cerebellar atrophy and mild white matter hyperintensities, as part of the SPG57 clinical spectrum.
Biochemical impact of the novel TFG c.64C>T variant
This variant is the second TFG/SPG57 to be reported in HSP families and is predicted to result in a missense change c.64C>T (p.(Arg22Trp)) that lies within the Phox and Bem1p (PB1) domain of the TFG protein. The PB1 domain has been shown previously to self-associate (forming homo-oligomers) in yeast two-hybrid studies.37 Consistent with a previous structural characterization of TFG,38 we found that the wild-type PB1 domain, at concentrations ranging from 18–45 μM, formed octamers in solution (~92 kD). In contrast, the c.64C>T (p.(Arg22Trp)) mutant of the PB1 domain exhibited a significantly reduced molecular mass of ~24 kD (around one-fourth of the wild-type protein mass) throughout the same range of protein concentrations, indicating it was only capable of forming dimers rather than octamers. In addition, its elution time was extended relative to the wild-type protein, consistent with the idea that the mutant failed to self-assemble properly (Figure 2). Together, these studies demonstrate that the c.64C>T (p.(Arg22Trp)) missense variant disrupts the ability of the PB1 domain to oligomerize in octamers thus extending what was previously reported38 about the effect of c.316C>T (p.(Arg106Cys)) variant (located in the coiled-coil domain) on TFG self-assembly.
Figure 2.
Family F19 with autosomal recessive hereditary spastic paraplegia caused by TFG/SPG57. (a) Pedigree of family F19 in which a missense variant segregates with the disease. Electropherograms show homozygous and heterozygous genotypes. Conservation of the amino-acid sequence is shown as well as a gene model showing the position of detected variant. (b) Purified, untagged forms of TFG (amino acids 1–96; wild-type or mutated to include the c.64C>T (p.(Arg22Trp)) substitution), were separated over a gel filtration column (Wyatt TWC-030S5) that was coupled to a multi-angle light-scattering device. Representative light-scattering profiles (wild-type TFG, blue; TFG c.64C>T (p.(Arg22Trp)), red) are plotted (b (I)). Eluted fractions were separated by SDS-PAGE and stained using Coomassie to highlight the elution profiles of the both forms of TFG (b (II)). Based on three independent experiments for each protein, wild-type TFG (amino acids 1–96) exhibited a molecular mass of 92.4 kD ± 3.7 kD, and c.64C>T (p.(Arg22Trp)) TFG (amino acids 1–96) exhibited a molecular mass of 24.4 kD ± 1.0 kD. (c) Brain MRIs of individuals 19172 (sagittal T1W section) and 19171 (T2 FLAIR axial section) showing thinning of the body of the corpus callosum (c (I)) and TCC with mild periventricular signal hyperintensity lesions at the occipital pole (c (II)). Pedigree symbols: full shading indicates affected individuals, half horizontal shading indicates other diseases, numbers between brackets are multiple siblings, diamonds indicate multiple siblings of different sex. Individual ID numbers and genotypes are indicated. Genotypes: ++ homozygous reference; M+ heterozygous; MM homozygous mutant. Others are standard medical pedigree symbols.
Discussion
Similar to other communities with high consanguinity,9, 10 we found that AR HSP inheritance is predominant in Sudan. However, in our series, the complex phenotype is predominant (84%), which is in disagreement with Coutinho et al.9 who elicited a predominant pure phenotype, but in agreement with a study in South Tunisia10 that reported 69% of complex cases. Sudanese families with AR HSP showed a high frequency of SPG11 variants (~13%) in conformity with other populations.15 Other genes were identified in single families. Of note, SPG7 and SPG4 were not identified in this report. Commonly, phenotypes were relatively heterogeneous within families and between different families. These differences ranged between subtle and overt, including onset, progression, and motor and cognitive aspects. This represented a diagnostic challenge especially when symptoms overlapped with other diseases. The use of a targeted NGS exome panel provided an efficient and reliable screening method to test HSP and HSP-related genes. Here, it was possible to identify causative variants in 28% of screened families, a success rate similar to other reports using candidate gene or exome sequencing in heterogeneous diseases.27
In the remaining families with yet unidentified causative variants, no pathological short variants (homozygous/compound heterozygous) or deletions/duplications in known HSP genes were identified. The complex heterogeneous phenotypes seen in these undiagnosed families imply a high possibility to expand the molecular basis of HSP and carry a prospect of unraveling new candidate genes with monogenic or digenic/oligogenic inheritance, non-coding variations, undetected large deletions/rearrangements or epigenetic modifications.
Correlations between HSP phenotypes and variants' positions (in the same gene) are rarely noted, reported previously only in PNPLA6 by Schabhüttl et al.39 In TFG/SPG57, variants in the proline and glutamine-rich domain (carboxyl terminus) of TFG/SPG57 result in AD hereditary sensory motor neuropathy with proximal predominant involvement.19 On the contrary, variants in the amino terminus result in AR HSP.18 In this study, an amino terminus variant resulted in AR HSP as well. Significant clinical differences were observed between the first reported SPG57 c.316C>T variant (p.(Arg106Cys)) and the variant c.64C>T (p.(Arg22Trp)) reported here. SPG57 may thus represent another exception regarding phenotype vs variant position correlations, although other variants are required to study this phenomenon with accuracy. These observed differences might be attributed to the different domains affected in the two families (coiled-coil and PB1 domains) and the functional impact of each. Although both variants resulted in perturbed oligomerization of the protein, the mechanism and consequent functional effect are likely to be distinct based on our biochemical analysis. Structural studies indicate that full length TFG self-assembles into octameric ring-like complexes in solution.18 Our analysis of the PB1 domain indicates that it is likely to be responsible for the octameric self-assembly, as it exhibits a similar propensity to form octamers. Thus, the coiled-coil domain may play another distinct role in promoting TFG complex assembly, potentially facilitating its ring-like conformation, which is likely under considerable strain.
Conclusions
We identified the first Sudanese families carrying novel variants in SPG11, ATL1, ALS2, SACS and TFG/SPG57. A novel TFG variant c.64C>T (p.(Arg22Trp)) – the second SPG57 variant to be reported – was found to disrupt TFG protein oligomerization. The difficulty to reach a genetic diagnosis in the majority of studied families suggests the possibility of new genes, unusual models of inheritance or non-coding variations underlying spinocerebellar degeneration. Adoption of novel diagnostic approaches like whole-exome or -genome sequencing is therefore highly recommended to explore these families.
Acknowledgments
We thank the members of the DNA and cell bank of the ICM, Federica Barreca, Emeline Mundwiller, Khalid El Hachimi and Delphine Bouteiller for their valuable contribution. This study was supported financially by the Agence Nationale de la Recherche (SPATAX-QUEST project, to Giovanni Stevanin), the Verum Foundation and Roger de Spoelberg Foundation (to Alexis Brice), the European Union (Neuromics projects, OMICS call, to Alexis Brice, Alexandra Durr and Giovanni Stevanin) and the National Institutes of Health (GM110567 to Anjon Audhya) and benefited from the Programme d’Investissement d’Avenir IHU-A-ICM. Liena Elsayed was the recipient of a Campus France and University of Khartoum fellowships.
Footnotes
Supplementary Information accompanies this paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
The authors declare no conflict of interest.
Supplementary Material
References
- Tesson C, Koht J, Stevanin G: Delving into the complexity of hereditary spastic paraplegias: how unexpected phenotypes and inheritance modes are revolutionizing their nosology. Hum Genet 2015; 134: 511–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink J: Hereditary spastic paraplegia overview. In: Pagon R, Adam M, Ardinger H et al: (eds): GeneReviews. University of Washington: Seattle (WA), USA, 1993. Available at: http://www.ncbi.nlm.nih.gov/books/NBK1509/. [PubMed] [Google Scholar]
- Schmitz-Hübsch T, Klockgether T: An update on inherited ataxias. Curr Neurol Neurosci Rep 2008; 8: 310–319. [DOI] [PubMed] [Google Scholar]
- Finsterer J: Ataxias with autosomal, X-chromosomal or maternal inheritance. Can J Neurol Sci 2009; 36: 409–428. [DOI] [PubMed] [Google Scholar]
- Coutelier M, Stevanin G, Brice A: Genetic landscape remodelling in spinocerebellar ataxias: the influence of next-generation sequencing. J Neurol 2015; 262: 2382–2395. [DOI] [PubMed] [Google Scholar]
- Noreau A, Dion P, Rouleau G: Molecular aspects of hereditary spastic paraplegia. Exp Cell Res 2014; 325: 18–26. [DOI] [PubMed] [Google Scholar]
- Ruano L, Melo C, Silva M, Coutinho P: The global epidemiology of hereditary ataxia and spastic paraplegia: a systematic review of prevalence studies. Neuroepidemiology 2014; 42: 174–183. [DOI] [PubMed] [Google Scholar]
- Finsterer J, Löscher W, Quasthoff S, Wanschitz J, Auer-Grumbach M, Stevanin G: Hereditary spastic paraplegias with autosomal dominant, recessive, x-linked, or maternal trait of inheritance. J Neurol Sci 2012; 318: 1–18. [DOI] [PubMed] [Google Scholar]
- Coutinho P, Barros J, Zemmouri R et al: Clinical heterogeneity of autosomal recessive spastic paraplegias: analysis of 106 patients in 46 families. Arch Neurol 1999; 56: 943–949. [DOI] [PubMed] [Google Scholar]
- Boukhris A, Stevanin G, Feki I et al: Hereditary spastic paraplegia with mental impairment and thin corpus callosum in tunisia: SPG11, SPG15, and further genetic heterogeneity. Arch Neurol 2008; 65: 393–402. [DOI] [PubMed] [Google Scholar]
- França M, D’Abreu A, Maurer-Morelli C et al: Prospective neuroimaging study in hereditary spastic paraplegia with thin corpus callosum. Mov Disord 2007; 22: 1556–1562. [DOI] [PubMed] [Google Scholar]
- Stevanin G, Santorelli F, Azzedine H et al: Mutations in SPG11, encoding spatacsin, are a major cause of spastic paraplegia with thin corpus callosum. Nat Genet 2007; 39: 366–372. [DOI] [PubMed] [Google Scholar]
- Shibasaki Y, Tanaka H, Iwabuchi K et al: Linkage of autosomal recessive hereditary spastic paraplegia with mental impairment and thin corpus callosum to chromosome 15A13-15. Ann Neurol 2000; 48: 108–112. [PubMed] [Google Scholar]
- Casali C, Valente E, Bertini E et al: Clinical and genetic studies in hereditary spastic paraplegia with thin corpus callosum. Neurology 2004; 62: 262–268. [DOI] [PubMed] [Google Scholar]
- Stevanin G, Montagna G, Azzedine H et al: Spastic paraplegia with thin corpus callosum: description of 20 new families, refinement of the SPG11 locus, candidate gene analysis and evidence of genetic heterogeneity. Neurogenetics 2006; 7: 149–156. [DOI] [PubMed] [Google Scholar]
- Schüle R, Schlipf N, Synofzik M et al: Frequency and phenotype of SPG11 and SPG15 in complicated hereditary spastic paraplegia. J Neurol Neurosurg Psychiatry 2009; 80: 1402–1404. [DOI] [PubMed] [Google Scholar]
- Novarino G, Fenstermaker A, Zaki M et al: Exome sequencing links corticospinal motor neuron disease to common neurodegenerative disorders. Science 2014; 343: 506–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beetz C, Johnson A, Schuh A et al: Inhibition of TFG function causes hereditary axon degeneration by impairing endoplasmic reticulum structure. Proc Natl Acad Sci USA 2013; 110: 5091–5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishiura H, Sako W, Yoshida M et al: The TRK-fused gene is mutated in hereditary motor and sensory neuropathy with proximal dominant involvement. Am J Hum Genet 2012; 91: 320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takiyama Y: Sacsinopathies: sacsin-related ataxia. Cerebellum 2007; 6: 353–359. [DOI] [PubMed] [Google Scholar]
- Gregianin E, Vazza G, Scaramel E et al: A novel SACS mutation results in non-ataxic spastic paraplegia and peripheral neuropathy. Eur J Neurol 2013; 20: 1486–1491. [DOI] [PubMed] [Google Scholar]
- Synofzik M, Soehn A, Gburek-Augustat J et al: Autosomal recessive spastic ataxia of charlevoix saguenay (ARSACS): expanding the genetic, clinical and imaging spectrum. Orphanet J Rare Dis 2013; 8: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Hentati A, Deng H: The gene encoding Alsin, a protein with three guanine-nucleotide exchange factor domains, is mutated in a form of recessive amyotrophic lateral sclerosis. Nat Genet 2001; 29: 160–165. [DOI] [PubMed] [Google Scholar]
- Salih M: Genetic disorders in Sudan. In: Teebi AS (eds): Genetic Disorders Among Arab Populations, 2nd edn. Springer Science & Business Media, Springer-Verlag Berlin Heidelberg: Germany, 2010, pp 575–612. [Google Scholar]
- de Bot S, Burggraaff R, Herkert J et al: Rapidly deteriorating course in Dutch hereditary spastic paraplegia type 11 patients. EJHG 2013; 21: 1312–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denora P, Muglia M, Casali C et al: Spastic paraplegia with thinning of the corpus callosum and white matter abnormalities: further mutations and relative frequency in ZFYVE26/SPG15 in the Italian population. J Neurol Sci 2009; 277: 22–25. [DOI] [PubMed] [Google Scholar]
- Abdel-Aleem A, Abu-Shahba N, Swistun D et al: Expanding the clinical spectrum of SPG11 gene mutations in recessive hereditary spastic paraplegia with thin corpus callosum. Eur J Med Genet 2011; 54: 82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baets J, Deconinck T, Smets K: Mutations in SACS cause atypical and late-onset forms of ARSACS. Neurology 2010; 75: 1181–1188. [DOI] [PubMed] [Google Scholar]
- El Euch-Fayache G, Lalani I, Amouri R et al: Phenotypic features and genetic findings in sacsin-related autosomal recessive ataxia in Tunisia. Arch Neurol 2003; 60: 982–988. [DOI] [PubMed] [Google Scholar]
- Criscuolo C, Banfi S, Orio M et al: A novel mutation in SACS gene in a family from Southern Italy. Neurology 2004; 62: 100–102. [DOI] [PubMed] [Google Scholar]
- Grieco G, Malandrini A, Comanducci G et al: Novel SACS mutations in autosomal recessive spastic ataxia of charlevoix-saguenay type. Neurology 2004; 62: 103–106. [DOI] [PubMed] [Google Scholar]
- Ogawa T, Takiyama Y, Sakoe K et al: Identification of a SACS gene missense mutation in ARSACS. Neurology 2014; 62: 107–109. [DOI] [PubMed] [Google Scholar]
- Hedera P: Spastic paraplegia 3A. In: Pagon R, Adam M, Ardinger H et al: (eds): GeneReviews. University of Washington: Seattle (WA), USA, 1993. Available at: http://www.ncbi.nlm.nih.gov/books/NBK45978/. [PubMed] [Google Scholar]
- Eymard-Pierre E, Lesca G, Dollet S et al: Infantile-onset ascending hereditary spastic paralysis is associated with mutations in the Alsin gene. Am J Hum Genet 2002; 71: 518–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devon R, Helm J, Rouleau G et al: The first nonsense mutation in Alsin results in a homogeneous phenotype of infantile-onset ascending spastic paralysis with bulbar involvement in two siblings: first nonsense mutation in Alsin. Clin Genet 2003; 64: 210–215. [DOI] [PubMed] [Google Scholar]
- Wakil S, Ramzan K, Abuthuraya R et al: Infantile-onset ascending hereditary spastic paraplegia with bulbar involvement due to the novel ALS2 mutation c.2761C>T. Gene 2014; 536: 217–220. [DOI] [PubMed] [Google Scholar]
- Lamark T, Perander M, Outzen H et al: Interaction codes within the family of mammalian Phox and Bem1p domain-containing proteins. J Biol Chem 2003; 278: 34568–34581. [DOI] [PubMed] [Google Scholar]
- Johnson A, Bhattacharya N, Hanna M et al: TFG clusters COPII-coated transport carriers and promotes early secretory pathway organization. EMBO J 2015; 34: 811–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schabhüttl M, Wieland T, Senderek J et al: Whole-exome sequencing in patients with inherited neuropathies: outcome and challenges. J Neurol 2014; 261: 970–982. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.