SUMMARY
Objectives
The aim of the present study was to describe a proof of concept digital workflow for the implant-prosthetic treatment in partially edentate patients and evaluate its clinical performance.
Methods
A 55-year-old woman with a Kennedy class III bilateral edentulism in the mandible has been selected for a computer guided implantology according with the Smart Fusion® protocol (NobelBiocare, Kloten, Switzerland). After the template-guided implant placement, an immediate loading of the implants has been performed. QuickTemp conical temporary abutments were selected to deliver immediately prefabricated cement-retained provisionals. Two months after an impression was taken with an intraoral digital scanner (3Shape Trios3, Copenhagen, Denmark). The provisional restoration optical scanning was used to transfer the functionalized prosthetic contour to be duplicated into the definitive porcelain fused to zirconia restoration cemented on customized titanium abutments.
Results
A satisfying esthetic and functional result has been achieved. No biological and mechanical complications were recorded.
Conclusions
The investigated fully digital implant-prosthetic protocol provided a smooth, complication free and time effective treatment alternative to the conventional workflow.
Besides the fully digital workflow allowed the surgical and prosthetic decision making and the communication within the dental team and with the patient. Further improvements heading to a direct match between the intraoral scan and the CBCT are strongly advised in order to create the so-called virtual patient.
Keywords: computer-guided implant surgery, smart fusion, dental implant, digital impression, intraoral scanner
Introduction
Nowadays the use of digital technologies into the daily practice is growing rapidly despite poor scientific and clinical evidence. The introduction of low dose 3D imaging systems such as the CBCT (Cone Beam Computed Tomography), 3D implant planning software, and CAD/CAM (computer-aided design/computed-assisted manufacturing) technology have undoubtedly been important achievements in the field of dental implantology (1).
Efforts to incorporate innovative technological advances into daily clinical practice are resulting in optimized and personalized oral health care delivery (2, 3).
Computer guided surgery has been validated since its introduction in the early 2000s as an efficient and reliable procedure for obtaining functional and aesthetic outcome (4–8).
With increasing availability, reduced radiation and lower costs of three-dimensional imaging because of cone beam computer tomography, pre-operative three-dimensional implant planning is becoming more popular in dentistry and cranio-maxillofacial surgery (7–14). Navigated implant surgery provides for improved implant positioning at anatomically sensitive structures such as the maxillary sinus, the mandibular canal, and the mental foramen. Besides, modern template-guided systems make use of the advantage of the minimally invasive access (15–17). Correct implant positioning has a number of advantages such as a favorable esthetic and prosthetic outcome and the potential to ensure optimal occlusion and implant loading (18–22). Recently a radiological template-free implant guided surgery workflow has been introduced for partially edentate patients. Sophisticated algorithms allow the fusion between STL file belonging from the 3D optical scan of the master models and wax up, with those gathered from the CBCT scan of the patient. The dental team is then driven through the proper surgical and prosthetic decision making and delivery the implant treatment accordingly. A relatively new approach employs Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM) technology to take a digital impression intraorally, fabricate the master model, and design as well as produce the final restoration (23). This method aims to overcome certain physical limitations of conventional means, such as the dimensional changes of impression materials, the expansion of dental stone, and human errors associated with final restoration fabrication, thus reducing processing time as well as cost (24–26). The application of intraoral digital scanner and CAD/CAM technologies has to be considered a valid alternative to conventional impression and prostheses fabrication procedures. Even if it still has some difficulties in detecting the finishing line of tooth preparations, digital impression has shown a great precision and ease of application in detecting the implant position. That is due to the use of dedicated impression transfers called scan bodies, whose surfaces are universally known and saved in digital libraries (27). The objective of the present case report was to describe a proof of concept digital workflow for the implant-prosthetic treatment in partially edentate patients and evaluate its clinical performance.
Methods
A 55-year-old woman with a Kennedy class III bilateral edentulism (Figure 1) in the mandible has been selected for a computer guided implantology according with the Smart Fusion® protocol (NobelBiocare, Kloten, Switzerland).
Figure 1.
Preoperative CBCT panorex slice.
The patient underwent a CBCT scan (Planmeca ProMax 3D, Helsinki, Finland) with a 0,2 mm slice increment and keeping the two arches separated with a byte index. Alginate impressions of both dental arches were taken and the master cast poured.
A first digital implant planning has been carried out, through the NobelClinician software, taking into account just the anatomical information derived by the CBCT. The alveolar nerves have been highlighted and the implants were digitally positioned. The planning has been shared with the technician through NobelConnect and a wax-up request has been performed.
The technician has accomplished the wax-up on the basis of the first approximate digital implant planning.
The Nobel Procera 2G optical scanner (Nobel-Biocare, Kloten, Switzerland) was then used to record the 3D scans of the master casts with the wax up, and the STL files obtained were then sent to the clinician always through NobelConnect. The smart fusion process allowed the superimposition of the DICOM data with the STL data, through an automatic process executed by a proprietary algorithm (Figure 2). The smart fusion superimposition was verified with a careful visualization of the overlapped patient anatomy and master casts. Considering both the anatomical and prosthetic data, the clinician has modified the implant positions in order to obtain an ideal aesthetic and functional compromise (Figures 3, 4).
Figure 2.
Smart fusion steps, digital planning and surgical template.
Figure 3.
Implant divergence tool.
Figure 4.
Digital implant planning axial slice.
A Ø 4,3 × 8,5 mm NobelActive RP and a Ø 5,0 × 8,5 mm NobelActive RP implants have been planned in position 3.5–3.6.
A 4.4–4.6 bridge has been planned over a Ø 5,0 × 8,5 mm NobelActive RP and a Ø 5,5 × 8,5 mm NobelActive WP implants respectively in 4.4 and 4.6 position (Figure 5).
Figure 5.
Digital implant planning panorex slice.
On the basis of the digital implant planning a CAD-CAM surgical template was fabricated and used to place the implants with a fully guided surgical protocol.
The teeth-supported surgical template has been first reinforced with a resin-metal armor in order to reduce the risk of fracture during the surgical phase and a fitting check has been accomplished on the plaster cast.
During the day of surgery, a single dose of antibiotic (2 g of amoxicillin and clavulanic acid) was administered prophylactically 1 h prior to surgery. This treatment continued for 7 days (1 g amoxicillin and clavulanic acid twice a day) after surgery. Prior to the start of surgery, the patient rinsed with 0.2% chlorhexidine for 1 min. Local anesthesia was induced by using a 4% articaine solution with epinephrine 1:100.000 (Ubistesin; 3M Italia, Milan, Italy).
The surgical template has been relined with low-percentage contraction acrylic resin (Pattern Resin GC, Tokyo, Japan) to increase its stability and its position has been checked through the inspection windows.
The implant company guidelines have been followed concerning the guided drilling sequence.
Following the guided implants insertion, a percussion stability test has been executed and an immediate loading protocol has been carried out. QuickTemp conical temporary abutments were selected to deliver immediately metal-reinforced cement-retained provisionals.
Two months after, an impression was taken with an intraoral digital scanner (Trios3, 3Shape, Copenhagen, Denmark) (Figure 6). Five scans have been performed. The first one including the lower arch with the temporary restorations still in situ. The second one of the opposite arch. The third one of the left and right bites, so that the upper and lower arches could be correctly matched. The fourth scan was performed after the removal of temporary restorations and temporary abutments, detecting the transmucosal path created during the two-month healing period. The last scan was performed to record implants position, screwing dedicated scan bodies (LaStruttura, Varese, Italy) to the implants. A color matching digital tool was used to detect the tooth color.
Figure 6.
Provisional digital impression. Scan bodies digital impression. Color matching tool. Cad/Cam definitive restorations on 3D printed models.
The STL file belonging from the scan were automatically forwarded to a centralized CAD-CAM facility (GF AgieCharmilles, Schaffhausen, Switzerland) to carry-on the prosthetic workflow of the treatment.
The provisional restoration optical scanning was used to transfer the functionalized prosthetic contour to be duplicated into the definitive porcelain fused to zirconia restoration cemented on customized titanium abutments (Figures 7, 8).
Figure 7.
Intrabuccal X-rays.
Figure 8.
Definitive restorations.
Results
A satisfying aesthetic and functional result has been achieved. No need of occlusal adjustments during the day of the definitive restoration delivery. No biological and mechanical complications were recorded.
Discussion
This Case Report study was conducted with the aim to describe a proof of concept digital workflow for the implant-prosthetic treatment in partially edentate patients and evaluate its clinical performance (Figure 9).
Figure 9.
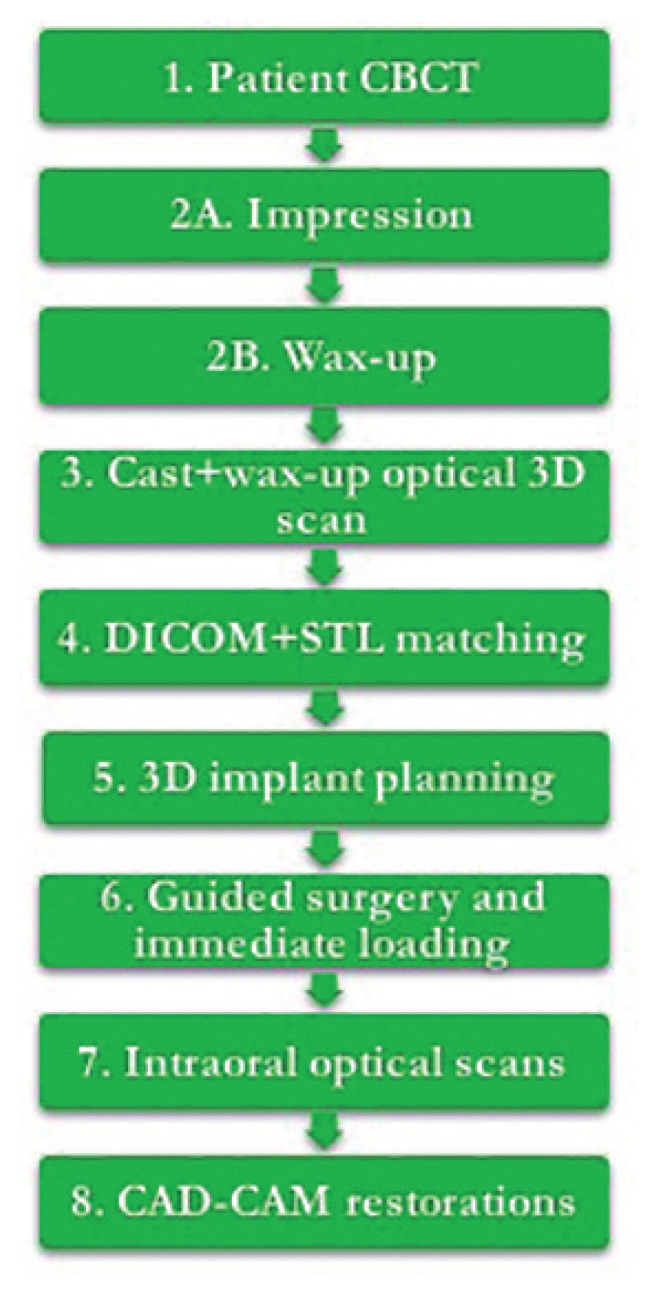
Implant-prosthetic digital workflow.
Computer guided implantology, flapless surgery, immediate loading, digital impression and CAD/CAM technologies have been adopted to solve a Kennedy class III bilateral edentulism in the mandible.
The interest of clinicians has turned, in recent years, towards research into safe protocols, implying the use of procedures to verify the compatibility of the proposed surgical and prosthetic planning before surgery to reduce excessive surgical trauma and achieve an excellent aesthetic result (28). The introduction of digital implant planning software allowed clinicians to ideally select number, type, length, width and 3D position of the implants, considering both the anatomical features of the patient and the prosthetic project (29). In that way the clinician has the possibility to first analyze all the limits and opportunities of the implant-prosthetic case, and so there is the possibility to select the best compromise between function, aesthetic and anatomical characteristics. Furthermore, the final implant-prosthetic result should be clear and already visible before the surgery. That is a great advantage for the clinician in reducing different types of complications and at the same time it enhances the communication with the patient. Being guided surgery performed quite always flapless, reduced postoperative pain and swelling, reduced intraoperative bleeding, preservation of soft and hard tissue and maintenance of periosteal blood supply are to be expected (30). Anyway a learning curve is necessary to use this software in order to avoid undesired complications. A mistake during the virtual planning step would be subsequently integrated into the surgical template, leading the clinician to an implant position error or even to severe anatomical complications, damaging nerves and/or vessels. In fact, during the static guided surgery there is no possibility to change the implant planning and the drilling sequence occurs without a clear vision of the underlying anatomy. Recent improvements of dental digital technologies are now enabling clinicians to take the digital impressions of the dental arches, avoiding the use of conventional impression materials (31). Studies demonstrated that the digital technique was more efficient and convenient than the conventional impression technique and that patients often prefer intraoral scan approach compared to the traditional impression (32, 33). While there are still some difficulties in detecting the tooth finishing line of subgingival preparations, a good feedback has been noticed for the use of IOS to detect the implant position. The IOS implant impression results easier because the transfer surface to scan is a known surface, contained in digital libraries. Attention has to be paid just to the correct scan body sitting. For these reasons, the combination of computer guided implantology and IOS has resulted as a fast and predictable protocol. A greater time had to be spent in the preoperative virtual planning, but a noticeable operative time reduction was recorded. Learning curve was necessary to have a good command of both software and traditional surgical and prosthetic concepts were still absolutely necessary to make a good virtual planning.
Conclusions
Within the limitations of the present study the investigated fully digital implant-prosthetic protocol provided a smooth, complication free and time effective treatment alternative to the conventional workflow. Besides, the fully digital workflow allowed the surgical and prosthetic decision making and the communication within the dental team and with the patient. Further improvements heading to a direct match between the intraoral scan and the CBCT are strongly advised in order to create the so-called virtual patient.
References
- 1.Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CHF, et al. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2009;24(Suppl):92–109. [PubMed] [Google Scholar]
- 2.Lanis A, Álvarez del Canto O. The Combination of Digital Surface Scanners and Cone Beam Computed Tomography Technology for Guided Implant Surgery Using 3Shape Implant Studio Software: A Case History Report. Int J Prosthodont. 2015;28(2):169–178. doi: 10.11607/ijp.4148. [DOI] [PubMed] [Google Scholar]
- 3.Tatullo M, Marrelli M, Falisi G, Rastelli C, Palmieri F, Gargari M, Zavan B, Paduano F, Benagiano V. Mechanical influence of tissue culture plates and extracellular matrix on mesenchymal stem cell behavior: A topical review. International Journal of Immunopathology and Pharmacology. 2016;29(1):3–8. doi: 10.1177/0394632015617951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verstreken K, Van Cleynenbreugel J, Marchal G, Naert I, Suetens P, van Steenberghe D. Computer-assisted planning of oral implant surgery: a three-dimensional approach. Int J Oral Maxillofac Implants. 1996;11(6):806–10. [PubMed] [Google Scholar]
- 5.Vercruyssen M, Laleman I, Jacobs R, Quirynen M. Computer-supported implant planning and guided surgery: a narrative review. Clin Oral Implants Res. 2015;26(Suppl 11):69–76. doi: 10.1111/clr.12638. [DOI] [PubMed] [Google Scholar]
- 6.De Vico G, Spinelli D, Bonino M, Schiavetti R, Pozzi A, Ottria L. Computer-assisted virtual treatment planning combined with flapless surgery and immediate loading in the rehabilitation of partial edentulies. Oral Implantol (Rome) 2012 Jan;5(1):3–10. [PMC free article] [PubMed] [Google Scholar]
- 7.Pozzi A, Gargari M, Barlattani A. CAD/CAM technologies in the surgical and prosthetic treatment of the edentulous patient with biomymetic individualized approach. Oral Implantol (Rome) 2008 Apr;1(1):2–14. [PMC free article] [PubMed] [Google Scholar]
- 8.Ottria L, Zavattini A, Ceruso FM, Gargari M. Maxillofacial prosthesis (P.M.F): In a case of oral-nasal communication post-surgery and post-radiotherapy. ORAL and Implantology. 2014;7(2):46–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofacial Radiology. 2004;33(2):83–6. doi: 10.1259/dmfr/28403350. [DOI] [PubMed] [Google Scholar]
- 10.Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Invest. 2006;10(1):1–7. doi: 10.1007/s00784-005-0031-2. [DOI] [PubMed] [Google Scholar]
- 11.Schneider D, Marquardt P, Zwahlen M, Jung RE. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res. 2009;20:73–86. doi: 10.1111/j.1600-0501.2009.01788.x. [DOI] [PubMed] [Google Scholar]
- 12.Gargari M, Prete V, Pujia M, Ceruso FM. Development of patient-based questionnaire about aesthetic and functional differences between overdentures implant-supported and overdentures tooth-supported. Study of 43 patients with a follow up of 1 year. ORAL and Implantology. 2012;5(4):86–91. [PMC free article] [PubMed] [Google Scholar]
- 13.Gargari M, Prete V, Pujia A, Ceruso FM. Full-arch maxillary rehabilitation fixed on 6 implants. ORAL and Implantology. 2013;6(1):1–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Clementini M, Ottria L, Pandolfi C, Bollero P. A Novel Technique to Close Large Perforation of Sinus Membrane. ORAL and Implantology. 2013;6(1):11–14. [PMC free article] [PubMed] [Google Scholar]
- 15.Vasak C, Strbac GD, Huber CD, Lettner S, Gahleitner A, Zechner W. Evaluation of three different validation procedures regarding the accuracy of template-guided implant placement: an in vitro study. Clinical Implant Dentistry and Related Research. 2015;17(1):142–9. doi: 10.1111/cid.12085. [DOI] [PubMed] [Google Scholar]
- 16.BouSerhal C, Jacobs R, Quirynen M, van Steenberghe D. Imaging technique selection for the preoperative planning of oral implants: a review of the literature. Clinical Implant Dentistry and Related Research. 2002;4(3):156–72. doi: 10.1111/j.1708-8208.2002.tb00167.x. [DOI] [PubMed] [Google Scholar]
- 17.Marrelli M, Falisi G, Apicella A, Apicella D, Amantea M, Cielo A, Bonanome L, Palmieri F, Santacroce L, Giannini S, Di Fabrizio E, Rastelli C, Gargari M, Cuda G, Paduano F, Tatullo M. Behaviour of dental pulp stem cells on different types of innovative mesoporous and nanoporous silicon scaffolds with different functionalizations of the surfaces. Journal of biological regulators and homeostatic agents. 2015;29(4):991–997. [PubMed] [Google Scholar]
- 18.Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer Technology Applications in Surgical Implant Dentistry: A Systematic Review. Int J Oral Maxillofac Implants. 2014;29(Supplement):25–42. doi: 10.11607/jomi.2014suppl.g1.2. [DOI] [PubMed] [Google Scholar]
- 19.Baggi L, Pastore S, Di Girolamo M, Vairo G. Implantbone load transfer mechanisms in complete-arch prostheses supported by four implants: a three-dimensional finite element approach. J Prosthet Dent. 2013;109(1):9–21. doi: 10.1016/S0022-3913(13)60004-9. [DOI] [PubMed] [Google Scholar]
- 20.Cecchetti F, Germano F, Bartuli FN, Arcuri L, Spuntarelli M. Simplified type 3 implant placement, after alveolar ridge preservation: a case study. Oral Implantol (Rome) 2014;7(3):80–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Gargari M, Comuzzi L, Bazzato MF, Sivolella S, di Fiore A, Ceruso FM. Treatment of peri-implantitis: Description of a technique of surgical 2 detoxification of the implant. A prospective clinical case series with 3-year follow-up. ORAL and Implantology. 2015;8(1):1–11. [Google Scholar]
- 22.Spinelli D, Ottria L, De Vico GD, Bollero R, Barlattani A, Jr, Bollero P. Full rehabilitation with nobel clinician ® and procera implant bridge®: Case report. ORAL and Implantology. 2013;6(2):25–36. [PMC free article] [PubMed] [Google Scholar]
- 23.Gargari M, Ottria L, Morelli V, Benli M, Ceruso FM. Conservative zirconia-ceramic bridge in front teeth. Case report. ORAL and Implantology. 2015;7(4):93–98. [Google Scholar]
- 24.Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dental Materials Journal. 2009;28(1):44–56. doi: 10.4012/dmj.28.44. [DOI] [PubMed] [Google Scholar]
- 25.Ali AO. Accuracy of Digital Impressions Achieved from Five Different Digital Impression Systems. Dentistry OMICS International. 2015;05(05) [Google Scholar]
- 26.Diamanti MV, Del Curto B, Barlattani A, Bollero P, Ottria L, Pedeferri M. Mechanical characterization of an innovative dental implant system. Journal of Applied Biomaterials and Biomechanics. 2009;7(1):23–28. [PubMed] [Google Scholar]
- 27.Vandeweghe S, Vervack V, Dierens M, De Bruyn H. Accuracy of digital impressions of multiple dental implants: an in vitro study. Clin Oral Implants Res. 2016 May 6; doi: 10.1111/clr.12853. [DOI] [PubMed] [Google Scholar]
- 28.Rossi R, Morales RS, Frascaria M, Benzi R. Planning implants in the esthetic zone using a new implant 3D navigation system. Eur J Esthet Dent. 2010;5(2):172–88. [PubMed] [Google Scholar]
- 29.Marchack CB. CAD/CAM-guided implant surgery and fabrication of an immediately loaded prosthesis for a partially edentulous patient. J Prosthet Dent. 2007;97(6):389–94. doi: 10.1016/S0022-3913(07)60028-6. [DOI] [PubMed] [Google Scholar]
- 30.Höckl K, Stoll P, Stoll V, Bähr W, Bach G. Flapless implant surgery and its effect on periimplant soft tissue. Int J Oral Maxillofac Surg. 2011;40(10):e24. [Google Scholar]
- 31.Seelbach P, Brueckel C, Wöstmann B. Accuracy of digital and conventional impression techniques and workflow. Clin Oral Invest. 2012;17(7):1759–64. doi: 10.1007/s00784-012-0864-4. [DOI] [PubMed] [Google Scholar]
- 32.Gjelvold B, Chrcanovic BR, Korduner EK, Collin Bagewitz I, Kisch J. Intraoral Digital Impression Technique Compared to Conventional Impression Technique. A Randomized Clinical Trial. J Prosthodont. 2016;25(4):282–7. doi: 10.1111/jopr.12410. [DOI] [PubMed] [Google Scholar]
- 33.Wismeijer D, Mans R, Genuchten M, Reijers HA. Patients& apos; preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin Oral Implants Res. 2014;25(10):1113–8. doi: 10.1111/clr.12234. [DOI] [PubMed] [Google Scholar]










