SUMMARY
Purpose
This study aims to evaluate differences in implant stability between post-extractive implants vs immediately placed post-extractive implants by resonance frequency analysis (RFA).
Materials and methods
Patients were grouped into two different categories. In Group A 10 patients had an immediate post-extractive implant, then a provisional, acrylic resin crown was placed (immediate loading). In Group B (control group) 10 patients only had an immediate post-extractive implant. Both upper and lower premolars were chosen as post-extractive sites. Implant Stability Quotient (ISQ) was measured thanks to RFA measurements (Osstell®). Five intervals were considered: immediately after surgery (T0) and every four weeks, until five months after implant placement (T1, T2, T3, T4,T5). A statistical analysis by means of Student’s T-test (significance set at p<0.05) for independent sample was carried out in order to compare Groups A and B.
Results
The ISQ value between the two groups showed a statistically significant difference (p<0.02) at T1. No statistically significant difference in ISQ was assessed at T0, T2, T3, T4 and T5.
Conclusions
After clinical assessment it is possible to confirm that provisional and immediate prosthetic surgery in post-extraction sites with cone-shaped implants, platform-switching abutment and bioactive surface can facilitate osseointegration, reducing healing time.
Keywords: post-extractive implants, immediate loading, implants stability quotient
Introduction
Implant placement in post-extractive sites in a single-session surgery (the so called post-extractive implants) shows high success rates, ranging from 92,7 to 98%, depending on the observed clinical records (1, 2). A Cochrane review shows that patients have higher satisfaction levels in case of placement techniques in post-extractive implants, when compared to conventional techniques in which complete healing is expected in post-extractive sites. As the alveolar bone is preserved, enhanced aesthetic results can be guaranteed. Post-extractive implants are biologically and functionally efficient, as they also reduce treatment time (3).
Preserving vestibular cortical bone allows precise implant placement; it enhances the external prosthetic profile; it also preserves the morphology of peri-implant soft tissues, thus getting higher aesthetic-prosthetic performance (4).
Nevertheless, this methodology requires specific prosthetic and implant procedures in order to achieve and maintain aesthetic and functional results (5).
The development of immediate prosthetic techniques – the so called immediate loading – enhanced healing procedures, keeping both hard and soft tissues around post-extractive implants. Data show that immediate loading can guarantee the same implant survival rates observed in classical techniques (6, 7).
An optimal aesthetic and functional result can be obtained using platform-switching implants (8). Primary implant stability still remains an essential requisite in order to obtain implant success both in delayed and post-extractive methodologies (9).
During the osseointegration process, primary mechanical stability is gradually replaced by biological stability. When the healing phase is completed, primary mechanical stability is totally replaced by biological stability (10).
Two variables can be involved in the osseointegration process: one is represented by implant surface, while the other one is represented by possible mechanical strains that can affect the surrounding bone (11–13).
Weak or physiological forces can permit peri-implant osteogenesis, ensuring high survival rates in immediately loaded implants (14–16).
Thanks to resonance frequency analysis it is possible to control implant stability non-invasively throughout the entire healing period (17–21).
This work aimed at monitoring any variation in Implant Stability Quotient (ISQ) values of post-extractive implants with immediate loading vs post-extractive implants without immediate loading.
Material and methods
Patient recruitment: twenty non-smoker patients in good health were enrolled for this study. All patients had good oral hygiene and did not show periodontal diseases. No pregnant or lactating patients were chosen for this study. An informed consent was obtained for each enrolled patient.
Implant site selection: a) only post-implant sites in both upper and lower premolar zone were considered; b) each post-extraction site had to show four intact alveolar walls: implants had to be inserted 2 mm below the vestibular bone margins; c) no sign of granulomatous wounds from extracted teeth had to be shown; d) adjacent teeth did not show periodontal pocket. Preliminary assessment was carried out by means of OPT X-ray tests, intraoral X-ray tests, cone-beam TC and periodontal probes.
Patients were randomly gathered into two groups: Group A and Group B. In Group A were assigned patients planned for post-extractive implant and immediate prosthetic techniques while in Group B were gathered patients planned for non-loaded post-extractive implants.
Surgical technique: all patients started the antibiotic profilaxis the day before the surgery, using amoxicillin and clavulanic acid (1g for bid). Articaine 1:200.000 was chosen as local anesthetic. Tooth extraction was extremely conservative in order to preserve soft and hard tissues: no flaps were elevated. Depending on the extraction difficulties, syndesmotomes, sonic systems (SonicLine, KOMET Lemgo - Germany), levers and clamps were used in order to ensure the highest alveolar integrity during extraction. Probes and curettes were used to explore the alveolar area accurately. Then, the sequence of measured pilot drills to prepare the implant site was used. The implant was screwed making sure that the margin of the implant neck was about 2 mm from the vestibular alveolar margin; eventual gaps between bone walls and implant surface were filled with calcium sulphate (P30 Surgi-plaster®, GHIMAS - Casalecchio di Reno, Bologna, Italy). Patients in Group B received a 4-mm healing abutment. An acrilic resin-based temporary abutment relined on Single-Temp (GEASS®) and screwed on the abutment was prepared for Group A. The abutment was unscrewed in order to finish its surface. When the temporary abutment was screwed again, the occlusal surface was refined. Adjustment was suspended when the film, 60 μ thick, (Arti-fol®, Bausch, Germany) could pass through the occlusal surface of the temporary abutment without impediments when both dental arches were fastened. After polishing the temporary abutment, it was screwed manually. Then, the hole for the abutment’s tightening screw was sealed with a cotton and temporary filling material pellet. Patients were discharged prescribing them ibuprofen-based analgesics (600 mg) and a chlorhexidine 0,12 three times a day for the following four weeks.
Implant type: implants used in this study (Way - Milan® manufactured by GEASS s.r.l. - Pozzuolo del Friuli, Udine, Italy) were screwed, cone-shaped with platform-switching prosthetic abutment. Implant surface (Syntegra®) had a laser surface treated micro-topography made of 20 μm pores with a 30 μm distance; they were homogeneously deployed on the whole implant surface (22).
ISQ measurement: in order to assess resonance values, an Osstell® Mentor tool with its corresponding SmartPegs (Integration Diagnostics AB, Goteborg, Sweden) was used. The first assessment was carried out both on Group A and B after implant placement. Patients were re-called 5 times every 28 days for ordinary check-ups and ISQ measurements. Data obtained were entered in a database. After five months, using ISQ-related monitoring data, each implant was completed by insertion a final crowns.
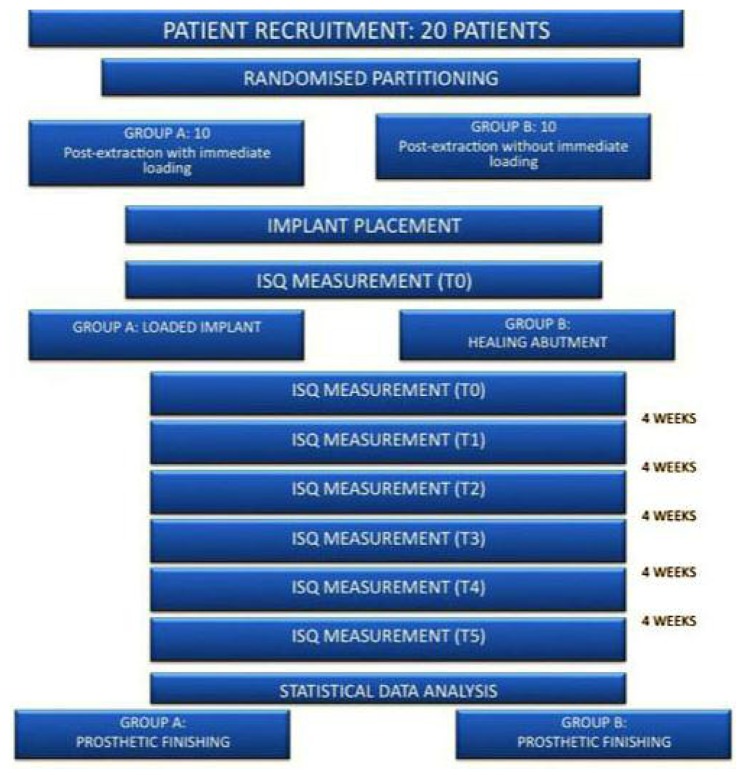
Statistical analysis: all measurements collected were subject to statistical analysis by means of Student’s T-test for independent sample in order to compare Group A and Group B. For each statistical assessment significance was set at p<0.05 (Figure 1).
Figure 1.
Summary of the clinical sequence used for the comparative study.
Results
Table 1 shows personal data and implant characteristics of the patients enrolled for this study. The patients enrolled were 5 men and 15 women, ranged in age from 28 to 61 years (mean age 44,85). Six implants were placed in area 1.4, 4 implants were placed in area 2.4, 4 implants were placed in area 1.5, 3 implants were placed in area 2.5, 2 implants were placed in area 3.5 and 1 implant was placed in area 4.5. Different implants were used. One implant was 11 mm in height and 3,8 mm in diameter; 4 implants were 12 mm in height and 3,8 mm in diameter; 1 implant was 13 mm in height and 3,8 mm in diameter; 2 implants were 10 mm in height and 4,5 mm in diameter; 1 implant was 11 mm in height and 4,5 mm in diameter; 5 implants were 12 mm in height and 4,5 mm in diameter; 6 implants were 13 mm in height and 4,5 mm in diameter. Group A (post-extraction with immediate loading) was made of 10 women with a mean age of 43,3 years. Four implants were placed in area 1.4, 3 implants were placed in area 2.4, 1 implant was placed in area 1.5, 1 implant was placed in area 2.5, 1 implant was placed in area 4.5. Different implants were used. One implant was 11 mm in height and 3,8 mm in diameter; 3 implants were 12 mm in height and 3,8 mm in diameter, 1 implant was 10 mm in height and 4,5 mm in diameter, 2 implants were 12 mm in height and 4,5 mm in diameter, 3 implants were 13 mm in height and 4,5 mm in diameter.
Table 1.
Demographic data and implant characteristics of enrolled patients.
| Patient # | Sex | Age | Implant location | Implant characteristics |
|---|---|---|---|---|
| Group A: Immediate loading | ||||
| 1 | W | 43 | 2.4 | 13 mm – Ø 4.5 mm |
| 2 | W | 46 | 1.4 | 12 mm – Ø 3.8 mm |
| 3 | W | 40 | 1.5 | 12 mm – Ø 4.5 mm |
| 4 | W | 43 | 1.4 | 13 mm – Ø 4.5 mm |
| 5 | W | 62 | 4.5 | 11 mm – Ø 3.8 mm |
| 6 | W | 46 | 1.4 | 13 mm – Ø 4.5 mm |
| 7 | W | 28 | 2.4 | 12 mm – Ø 3.8 mm |
| 8 | W | 50 | 2.5 | 12 mm – Ø 3.8 mm |
| 9 | W | 35 | 2.4 | 12 mm – Ø 4.5 mm |
| 10 | W | 40 | 1.4 | 10 mm – Ø 4.5 mm |
| Total: 10 | M:W=0:10 | Mean=43,3 | 4:1.4, 3:2.4 | n:1 11mmXØ3.8mm implants |
| 1:1.5, 1:2.5 | ||||
| 1:4.5 | n:3 12mmXØ3.8mm implants | |||
| n:1 10mmXØ4.5mm implants | ||||
| n:2 12mmXØ4.5mm implants | ||||
| n:3 13mmXØ4.5mm implants | ||||
| Group B: No immediate loading | ||||
| 1 | M | 42 | 1.5 | 13 mm – Ø 4.5 mm |
| 2 | W | 61 | 1.5 | 12 mm – Ø 4.5 mm |
| 3 | M | 44 | 3.5 | 13 mm – Ø 4.5 mm |
| 4 | W | 47 | 2.4 | 13 mm – Ø 3.8 mm |
| 5 | W | 39 | 2.5 | 11 mm – Ø 4.5 mm |
| 6 | M | 48 | 3.5 | 10 mm – Ø 4.5 mm |
| 7 | W | 46 | 1.5 | 12 mm – Ø 4.5 mm |
| 8 | W | 46 | 2.5 | 12 mm – Ø 4.5 mm |
| 9 | M | 43 | 1.4 | 13 mm – Ø 4.5 mm |
| 10 | M | 48 | 1.4 | 12 mm – Ø 3.8 mm |
| Total: 10 | M:W=5:5 | Mean=46,4 | 2:1.4, 1:2.4 | n:1 12mmXØ3.8mm implants |
| 3:1.5, 2:2.5 | n:1 13mmXØ3.8mm implants | |||
| 2:3.5 | n:1 10mmXØ4.5mm implants | |||
| n:1 11mmXØ4.5mm implants | ||||
| n:3 12mmXØ4.5mm implants | ||||
| n:3 13mmXØ4.5mm implants | ||||
| Group A + Group B | ||||
| Total: 20 | M:W=5:15 | Mean=44,85 | 6:1.4, 4:2.4 | n:1 11mmXØ3.8mm implants |
| 4:1.5, 3:2.5 | n:4 12mmXØ3.8mm implants | |||
| 2:3.5, 1:4.5 | n:1 13mmXØ3.8mm implants | |||
| n:2 10mmXØ4.5mm implants | ||||
| n:1 11mmXØ4.5mm implants | ||||
| n:5 12mmXØ4.5mm implants | ||||
| n:6 13mmXØ4.5mm implants | ||||
Group B (post-extraction without immediate loading) was made of 5 women and 5 men with a mean age of 46,6 years. Two implants were placed in area 1.4, 1 implant was placed in area 2.4, 3 implants were placed in area 1.5, 2 implants were placed in area 2.5, 2 implants were placed in area 4.5. Different implants were used. One implant was 12 mm in height and 3,8 mm in diameter; 1 implant was 13 mm in height and 3,8 mm in diameter, 1 implant was 10 mm in height and 4,5 mm in diameter, 1 implant was 11 mm in height and 4,5 mm in diameter, 3 implants were 12 mm in height and 4,5 mm in diameter, 3 implants were 13 mm in height and 4,5 mm in diameter.
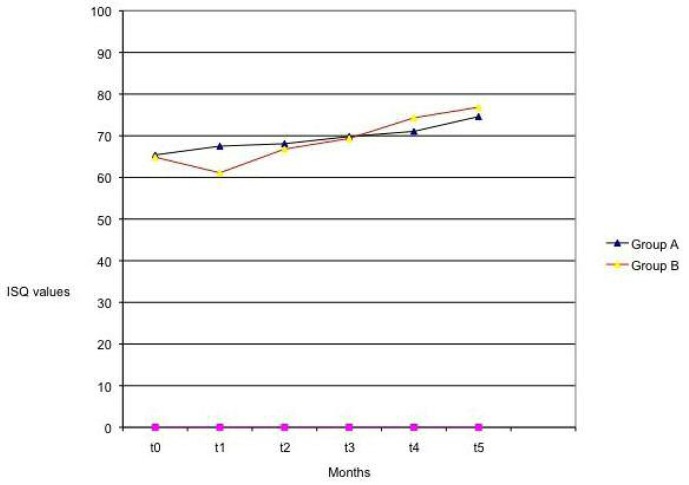
Table 2 shows ISQ values for every group at T0 (during surgery) and every four weeks (T1, T2, T3, T4, T5). A chart in Figure 2 shows the ISQ trend in both groups. At T1 it is possible to observe a difference in ISQ values corresponding to enhanced stability in Group A when compared to Group B. No statistical variation in ISQ values was observed at T0, T2, T3, T4, T5.
Table 2.
ISQ-related data.
| ISQ (mean ± DS) | ||||||
|---|---|---|---|---|---|---|
| Time (T= 4 week) | T0 | T1 | T2 | T3 | T4 | T5 |
| Group A | 63,80 ± 3,43 | 66,40 ± 3,43 | 66,20 ± 7,16 | 68,90 ± 4,53 | 70,00 ± 5,35 | 73,90 ± 4,15 |
| Group B: | 63,20 ± 4,47 | 59,40 ± 9,67 | 65,80 ± 8,89 | 68,50 ± 8,42 | 73,50 ± 7,38 | 76,70 ± 3,86 |
| A vs B P<0,05 |
NS | 0.02 | NS | NS | NS | NS |
Figure 2.
ISQ trend in both groups.
Discussion
ISQ is broadly used in order to assess variations in implant stability during the osseointegration process. This assessment was also used in order to compare immediately vs non immediately loaded implants.
Clauser et al. measured resonance frequency in order to assess the success rate of immediate or early loading in post-extractive sites with GBR procedure. Their results showed that 11,2% of implant failed to integrate, and resonance values decreased progressively in failed implants (20). Results obtained by Bischof et al., in which ISQ was measured depending on bone types and on the two different loading modalities (immediate and non-immediate) in mature sites, indicated that ISQ values remain stable or grow slightly during the first 4–6 weeks of osseointegration; in addition, there was no difference in the two compared groups, thus making immediate loading implants as predictable as delayed loading implants (18).
Ersanli et al. used resonance frequency analysis measurements in order to assess variations during the osseointegration period in 122 implants. Implants with non-immediate loading monitored 3 and 6 weeks after surgery, 3 and 6 months after being loaded, showed a reduction in ISQ values when controlled after 3 and 6 weeks after surgery; these data are similar to some findings by Raghavendra concerning variation in implant stability during the osseointegration process (10, 19). Finally, West et al. assessed variations in resonance value in implants placed in mature sites and in implants placed in post-extractive sites with evaluations being carried out every 4 weeks after implant placement. Immediately placed implants showed an initial ISQ reduction (15%) while it conforms in the following weeks (23).
At present, even post-extractive implants received clinical interest as for immediate prosthetic techniques is concerned.
Canullo et al. analysed 10 implants with platform-switching prosthetic abutments and post-extractive with immediate prosthetic techniques, respectively. Their assessment was based on X-ray and periodontal parameters, indicating that this procedure can preserve peri-implant soft and hard tissues (observation period: 36 months) (8). In a study that compared two groups including 20 post-extractive implants with immediate prosthesis and 20 post-extractive implants, Crespi et al. observed that both groups showed a 100% success rate after two years: in addition, any possible bone resorption showed no statistical difference (7). Calvo-Guirado et al. showed a 96,7% success rate twelve months after placement; crestal bone loss was minimal and RFA values were 71,1±6,2 (6). In a 5-year retrospective study carried out by Mura, 79 post-extractive, immediately loaded implants showed a 100% success rate with a minimal crestal resorption, thus validating this methodology (24). In a study with 64 implants, Malchiodi et al. showed that this implant-prosthetic approach had predictable results with a 100% success rate, with soft tissues being preserved at three-year follow-up (25).
This study demonstrates that post-extractive implants immediately loading, provide enhanced implant stability when compared to non-immediately loading implants. This data proves to be significant during the first four weeks after placement, that is the most important period of the osseointegration process. In addition, the possibility to insert a temporary element in the patient’s oral cavity immediately after post-extractive surgery surely represents a positive perspective for any patient. Using acrilic resin-based crowns in infraocclusive conditions (as indicated by Appleton) allow the forces developed in the implant area (16,1 N on average) and the peri-implant osteogenesis can be favoured (26, 27).
Though this study has some limits due to the size of the observed sample and a non-split mouth randomisation, it offers new perspectives. Cone-shaped implants were chosen for this study as some experimental models indicate that they offer higher primary implant stability (28).
Another implant-related characteristic was the platform-switching prosthetic abutment: it seems a decisive choice as it ensures an enhanced distribution of mastication strains both in implant necks and implant frameworks (29, 30). Additional important characteristic is represented by the implant surface. At present there are new surface treatments which ensure enhanced implant-related macroscopic potentialities, making immediate loading procedures more suitable (22). Immediate loading in post-extractive implants may influence prosthodontic (31–34) and endodontic (35, 36) clinical outcomes. In addiction the use of general and local anesthesia may have side effects (37–40) and severe complications (41).
Provisional and immediate prosthetic techniques in post-extractive sites with cone-shaped implants, platform-switching abutment and bioactive surface may enhance ISQ values after four weeks, thus facilitating osseointegration and reducing healing time, as well as making this methodology predictable.
References
- 1.Grunder U, Polizzi G, Goene R, Hatano N, Henry P, Jackson WJ, Kawamura K, Kohler S, Renouard F, Rosenberg R, Triplett G, Werbitt M, Lithner B. A 3-year prospective multicenter follow-up report on the immediate and delayed-immediate placement of implants. Int J Oral Maxillofac Implants. 1999;14(2):210–6. [PubMed] [Google Scholar]
- 2.Tolman DE, Keller EE. Endosseous implant placement immediately following dental extraction and alveoloplasty: preliminary report with 6-year follow-up. Int J Oral Maxillofac Implants. 1991;6(1):24–8. [PubMed] [Google Scholar]
- 3.Esposito M, Grusovin MG, Tzanetea E, Piattelli A, Worthington HV. Interventions for replacing missing teeth: treatment of perimplantitis. Cochrane Database Syst Rev. 2010;6:CD004970. doi: 10.1002/14651858.CD004970.pub4. [DOI] [PubMed] [Google Scholar]
- 4.Arlin M. Immediate placement of dental implants into extraction sockets: surgically-related difficulties. Oral Health. 1993;83(7):23–4. 27–8, 31. passim. [PubMed] [Google Scholar]
- 5.Lops D, Chiapasco M, Rossi A, Bressan E, Romeo E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket: 1-year prospective study. Clin Oral Implants Res. 2008;19(11):1135–40. doi: 10.1111/j.1600-0501.2008.01580.x. [DOI] [PubMed] [Google Scholar]
- 6.Calvo-Guirado JL, Ortiz-Ruiz AJ, Lopez-Mari L, Delgado-Ruiz R, Mate-Sanchez J, Bravo Gonzalez LA. Immediate maxillary restoration of single-tooth implants using platform switching for crestal bone preservation: a 12-month study. Int J Oral Maxillofac Implants. 2009;24(2):275–81. [PubMed] [Google Scholar]
- 7.Crespi R, Cappare P, Gherlone E, Romanos GE. Immediate versus delayed loading of dental implants placed in fresh extraction sockets in the maxillary esthetic zone: a clinical comparative study. Int J Oral Maxillofac Implants. 2008;23(4):753–8. [PubMed] [Google Scholar]
- 8.Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: a proof-of-concept study with 12- to 36-month follow-up. Int J Oral Maxillofac Implants. 2007;22(6):995–1000. [PubMed] [Google Scholar]
- 9.Bhola M, Neely AL, Kolhatkar S. Immediate implant placement: clinical decisions, advantages, and disadvantages. J Prosthodont. 2008;17(7):576–81. doi: 10.1111/j.1532-849X.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 10.Raghavendra S, Wood MC, Taylor TD. Early wound healing around endosseous implants: a review of the literature. Int J Oral Maxillofac Implants. 2005;20(3):425–31. [PubMed] [Google Scholar]
- 11.Puleo DA, Nanci A. Understanding and controlling the bone-implant interface. Biomaterials. 1999;20(23–24):2311–21. doi: 10.1016/s0142-9612(99)00160-x. [DOI] [PubMed] [Google Scholar]
- 12.Puleo DA, Thomas MV. Implant surfaces. Dent Clin North Am. 2006;50(3):323–38. v. doi: 10.1016/j.cden.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Leucht P, Kim JB, Wazen R, Currey JA, Nanci A, Brunski JB, Helms JA. Effect of mechanical stimuli on skeletal regeneration around implants. Bone. 2007;40(4):919–30. doi: 10.1016/j.bone.2006.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Degidi M, Piattelli A. 7-year follow-up of 93 immediately loaded titanium dental implants. J Oral Implantol. 2005;31(1):25–31. doi: 10.1563/0-730.1. [DOI] [PubMed] [Google Scholar]
- 15.Cornelini R, Cangini F, Covani U, Barone A, Buser D. Immediate restoration of single-tooth implants in mandibular molar sites: a 12-month preliminary report. Int J Oral Maxillofac Implants. 2004;19(6):855–60. [PubMed] [Google Scholar]
- 16.Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micro-motion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res. 1998;43(2):192–203. doi: 10.1002/(sici)1097-4636(199822)43:2<192::aid-jbm14>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 17.Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003;18(5):641–51. [PubMed] [Google Scholar]
- 18.Bischof M, Nedir R, Szmukler-Moncler S, Bernard JP, Samson J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin Oral Implants Res. 2004;15(5):529–39. doi: 10.1111/j.1600-0501.2004.01042.x. [DOI] [PubMed] [Google Scholar]
- 19.Ersanli S, Karabuda C, Beck F, Leblebicioglu B. Resonance frequency analysis of one-stage dental implant stability during the osseointegration period. J Periodontol. 2005;76(7):1066–71. doi: 10.1902/jop.2005.76.7.1066. [DOI] [PubMed] [Google Scholar]
- 20.Glauser R, Sennerby L, Meredith N, Ree A, Lundgren A, Gottlow J, Hammerle CH. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs. failing implants. Clin Oral Implants Res. 2004;15(4):428–34. doi: 10.1111/j.1600-0501.2004.01036.x. [DOI] [PubMed] [Google Scholar]
- 21.Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P. The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implants Res. 1997;8(3):234–43. doi: 10.1034/j.1600-0501.1997.080310.x. [DOI] [PubMed] [Google Scholar]
- 22.Lepore S, Milillo L, Trotta T, Castellani S, Porro C, Panaro MA, Santarelli A, Bambini F, Lo Muzio L, Conese M, Maffione AB. Adhesion and growth of osteoblastlike cells on laser-engineered porous titanium surface: expression and localization of N-cadherin and betacatenin. J Biol Regul Homeost Agents. 2013;27(2):531–41. [PubMed] [Google Scholar]
- 23.West JD, Oates TW. Identification of stability changes for immediately placed dental implants. Int J Oral Maxillofac Implants. 2007;22(4):623–30. [PubMed] [Google Scholar]
- 24.Mura P. Immediate loading of tapered implants placed in postextraction sockets: retrospective analysis of the 5-year clinical outcome. Clin Implant Dent Relat Res. 2012;14(4):565–74. doi: 10.1111/j.1708-8208.2010.00297.x. [DOI] [PubMed] [Google Scholar]
- 25.Malchiodi L, Cucchi A, Ghensi P, Nocini PF. Evaluation of the esthetic results of 64 nonfunctional immediately loaded postextraction implants in the maxilla: correlation between interproximal alveolar crest and soft tissues at 3 years of follow-up. Clin Implant Dent Relat Res. 2013;15(1):130–42. doi: 10.1111/j.1708-8208.2011.00424.x. [DOI] [PubMed] [Google Scholar]
- 26.Hattori Y, Satoh C, Kunieda T, Endoh R, Hisamatsu H, Watanabe M. Bite forces and their resultants during forceful intercuspal clenching in humans. J Biomech. 2009;42(10):1533–8. doi: 10.1016/j.jbiomech.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 27.Appleton RS, Nummikoski PV, Pigno MA, Cronin RJ, Chung KH. A radiographic assessment of progressive loading on bone around single osseointegrated implants in the posterior maxilla. Clin Oral Implants Res. 2005;16(2):161–7. doi: 10.1111/j.1600-0501.2004.01089.x. [DOI] [PubMed] [Google Scholar]
- 28.Aleo E, Varvara G, Scarano A, Sinjari B, Murmura G. Comparison of the primary stabilities of conical and cylindrical endosseous dental implants: an in-vitro study. J Biol Regul Homeost Agents. 2012;26(1):89–96. [PubMed] [Google Scholar]
- 29.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res. 2007;18(5):581–4. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 30.Chang CL, Chen CS, Hsu ML. Biomechanical effect of platform switching in implant dentistry: a three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2010;25(2):295–304. [PubMed] [Google Scholar]
- 31.Ottria L, Zavattini A, Ceruso FM, Gargari M. Maxillofacial prosthesis (P.M.F): in a case of oral-nasal communication post-surgery and post-radiotherapy. Oral Implantol (Rome) 2014;7(2):46–50. [PMC free article] [PubMed] [Google Scholar]
- 32.Gargari M, Gloria F, Cappello A, Ottria L. Strength of zirconia fixed partial dentures: review of the literature. Oral Implantol (Rome) 2010;3(4):15–24. [PMC free article] [PubMed] [Google Scholar]
- 33.De Vico G, Ottria L, Bollero P, Bonino M, Cialone M, Barlattani A, Jr, Gargari M. Aesthetic and functionality in fixed prosthodontic: sperimental and clinical analysis of the CAD-CAM systematic 3Shape. Oral Implantol (Rome) 2008;1(3–4):104–15. [PMC free article] [PubMed] [Google Scholar]
- 34.Moretto D, Gargari M, Nordsjo E, Gloria F, Ottria L. Immediate loading: a new implant technique with immediate loading and aesthetics: Nobel Active. Oral Implantol (Rome) 2008;1(2):50–5. [PMC free article] [PubMed] [Google Scholar]
- 35.Fanucci E, Nezzo M, Neroni L, Montesani L, Jr, Ottria L, Gargari M. Diagnosis and treatment of paranasal sinus fungus ball of odontogenic origin: case report. Oral Implantol (Rome) 2013;6(3):63–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Gargari M, Ottria L, Nezzo M, Neroni L, Fanucci E. Cone Beam CT use in the pre-prosthetic evaluation of endodontically treated of the rear maxilla. Oral Implantol (Rome) 2012;5(2–3):42–6. [PMC free article] [PubMed] [Google Scholar]
- 37.Feltracco P, Gaudio RM, Barbieri S, Tiano L, Iacobone M, Viel G, Tonetti T, Galligioni H, Bortolato A, Ori C, Avato FM. The perils of dental vacation: possible anaesthetic and medicolegal consequences. Med Sci Law. 2013;53(1):19–23. doi: 10.1258/msl.2012.012047. [DOI] [PubMed] [Google Scholar]
- 38.Feltracco P, Barbieri S, Galligioni H, Pasin L, Gaudio RM, Tommasi A, Zucchetto A, Trevisiol P, Ori C, Avato FM. A fatal case of anaphylactic shock during paragliding. J Forensic Sci. 2012;57(6):1656–8. doi: 10.1111/j.1556-4029.2012.02187.x. [DOI] [PubMed] [Google Scholar]
- 39.Feltracco P, Gaudio RM, Avato FM, Ori C. Authors’ Response (Letter) Journal of Forensic Sciences. 2012;57(5) doi: 10.1111/j.1556-4029.2012.02187.x. [DOI] [PubMed] [Google Scholar]
- 40.Gaudio RM, Barbieri S, Feltracco P, Tiano L, Galligioni H, Uberti M, Ori C, Avato FM. Traumatic dental injuries during anaesthesia. Part II: medico-legal evaluation and liability. Dent Traumatol. 2011;27(1):40–5. doi: 10.1111/j.1600-9657.2010.00956.x. [DOI] [PubMed] [Google Scholar]
- 41.Gaudio RM, Barbieri S, Feltracco P, Spaziani F, Alberti M, Delantone M, Trevisiol P, Righini F, Talarico A, Sanchioni R, Spagna A, Pietrantonio V, Zilio G, Dalla Valle R, Vettore G, Montisci M, Bortoluzzi A, Sacco A, Ramacciato G, Pasetti A, Mognato E, Ferronato C, Costola A, Ori C, Avato FM. Impact of alcohol consumption on winter sports-related injuries. Med Sci Law. 2010;50(3):122–5. doi: 10.1258/msl.2010.010007. [DOI] [PubMed] [Google Scholar]