SUMMARY
Nowadays computer-guided “flap-less” surgery for implant placement using stereolithographic tem-plates is gaining popularity among clinicians and patients. The advantages of this surgical protocol are its minimally invasive nature, accuracy of implant placement, predictability, less post-surgical discomfort and reduced time required for definitive rehabilitation. Aim of this work is to describe a new protocol (Smart Fusion by Nobel Biocare), thanks to which is now possible to do a mini-invasive static guided implant surgery, in partially edentulous patients with at least 6 remaining teeth, without the use of a radiographic guide. This is possible thanks to a procedure named surface mapping based on the matching between numerous points on the surface of patient’s dental casts and the corresponding anatomical surface points in the CBCT data. The full protocol is examined focusing the attention on the clinical and laboratory procedures.
Conclusions
Also with some critical points and needing an adequate learning curve, this protocol allows to select the ideal implant position in depth, inclination and mesio-distal distance between natural teeth and or other implants enabling a very safe and predictable rehabilitation compared with conventional surgery.
It represents a good tool for the best compromise between anatomy, function and aesthetic, able to guarantee better results in all clinical situations.
Keywords: smart fusion, dental implants, digital dental casts, surface mapping, CBCT, guided implant surgery
Introduction
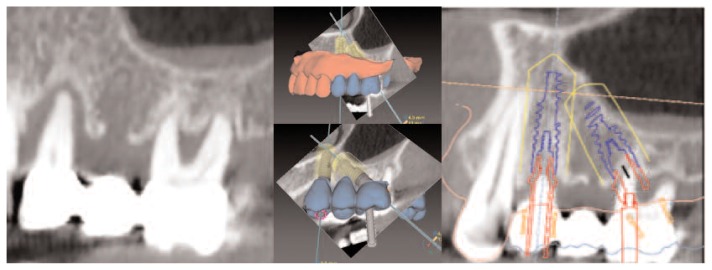
In the last years, the developments of computer-aided-design/computer-assisted-manufacturing (CAD/CAM) technologies have brought great improvements in all daily dentistry (1) specially in the field of oral implant surgery (2–4). The introduction of digital systems into the diagnostic routine, and their application together with 3D data of the bone topography, have made it possible to reconcile the two central aspects of oral implant surgery: planning an ideal prosthetic solution (first) with the given anatomic situation (second) (Figure 1). Companies such as Nobel Biocare and its Nobel Clinician, Materialise Dental and the SimPlant digital alternatives, Dental Wings and the development of CoDiagnostiX software, Sirona with Cerec solutions, Align Technology with its iTero scanner, and the 3 Shape Dental system are some of the most renowned names in the development of digital impressions and virtual surgical solutions.
Figure 1.
Procera software planning program allows for prosthetic guided implant positioning.
Thanks to these technologies (e.g. Nobel Clinician-Nobel Biocare) it is now possible to predetermine the precise 3D position of the implants, and then transfer the planning information into special stereolithographic surgical templates (5, 6) (Figure 2).
Figure 2.
CAD/CAM manufactured surgical template.
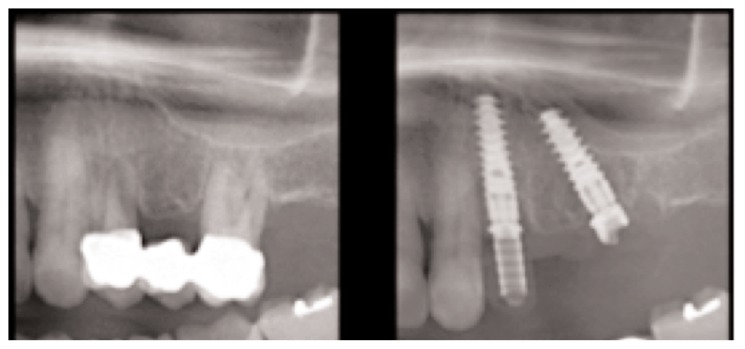
The advantages of this surgical protocol are its minimally invasive nature, accuracy of implant placement (7–10), predictability, less post-surgical discomfort and reduced time required for definitive rehabilitation while maintaining similar survival rates to conventional implant placement procedures (11, 12). The available bone can be used optimally and bone grafting can be avoided, or at least planned in advance in the best possible way (12, 13) (Figure 3).
Figure 3.
Pre and postoperative radiographs of a periodontal compromised extraction case.
That increases the quality of both the surgery and the restoration and results in a predictable surgical outcome and subsequently, a restorative treatment outcome. Until recently most of the digital surgical planning software available needed obligatorily a radiographic guide with fiducial or radiopaque markers and started with the patient’s tomography according to the double scan technique (13–15). For this reason was it necessary to enlist a laboratory technician to fabricate an Rx-template. Thus, the patient, wearing the radiographic guide stabilized with a rigid silicone index (rigid vinyl polysiloxane) was scanned with the occlusal plane parallel to the axial slices. Immediately after, a second scan of the template itself was performed using the same CT scanner settings and the same orientation as in the patient’s mouth (16) (Figure 4).
Figure 4.
Radiographic guide stabilized with a rigid silicon index.
Based on the automated matched positions of the fiducial markers, the two scan were then superimposed (Figure 5) in a procedure called matching. The reformatted data was then returned to the restorative team for choosing the ideal implant position by means of a 3D implant software. Later the surgical planning was transferred to a milling center for the fabrication of a stereo-lithographic surgical template, using the scanned radiographic guide as reference, giving the clinician the opportunity to perform a predictable, personalized and noninvasive implant intervention. This protocol, also representing a revolution in dentistry enabling to optimize several treatment processes also in situations where complex anatomical limitations had previously precluded the treatment, represented a problem in all patients that already had a 3D examination but made without a radiographic guide. These cases in-fact led the clinician to the dilemma: if to proceed with a new examination with a radiographic template, and thus being able to approach totally the benefits of a mini-invasive guided implant surgery or not, and choosing to proceed in a traditional way. Generally only in presence of serious problems of health of the patients or in complex surgical cases, the clinician often chose to repeat the examination according to the double scan protocol. However in spite of the absence of prosthetic information, before surgery, also the “free hand” cases were studied using a 3D implant planning software (e.g. Nobel Clinician-Nobel Biocare) (Figure 6).
Figure 5.
Radiographic guide with radiopaque gutta-percha markers.
Figure 6.
In spite of the absence of prosthetic information, before surgery, also these “free hand” cases were studied using a software for computer guided implant planning.
Nowadays, in partial edentulous cases, thanks to new protocols (e.g. Smart Fusion by Nobel Biocare AB) and a new procedure named surface mapping enabling the matching between 4–5 points on patient’s dental casts and the corresponding anatomical surface points in the CBCT data, is possible to exceed such limitation and proceed to a full guided surgery, provided that the patients have at least 6 remaining teeth distributed on two quadrants (14, 17, 18).
Clinical protocol: planning and diagnostic phase
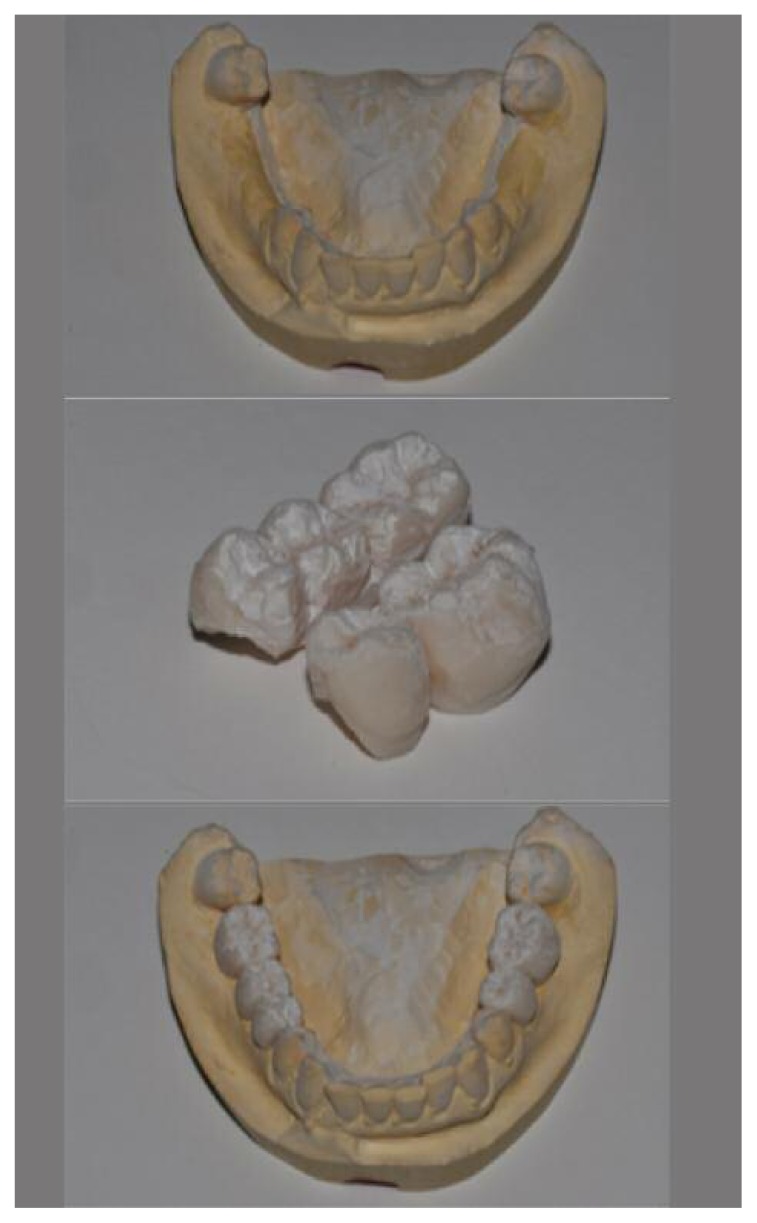
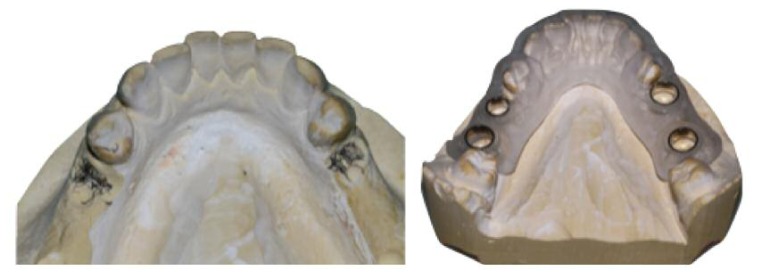
This new protocol is applicable only on patients with at least 6 remaining teeth in at least 2 quadrants. That is important in order to obtain a good stabilization of the surgical template during the surgery. Its indications are therefore the partial edentulous situations both healed or post-extractive starting from the single implant in very challenging area till the posterior edentulism (19). Anyway the first step is to study the case clinically and to prescribe to the patient a 3D examination. After that the operator will control the CBTC with a dedicate software and verify the possibility of an implant supported rehabilitation. Obviously in the hypothesis to use an exam already done by the patient, the operator, with his experience, will check it carefully deciding to repeat it in cases of too much old examinations or in cases of big image splitting (15, 16, 20–22). Once assessed the feasibility of the surgery, all anatomic landmarks are obtained from well-extended impressions of the arches of the patient mounted on an articulator (Figure 7). In order to avoid inaccuracies in the surface mapping registration, accurate impressions and casts must be made to create a precise mechanical fit of the templates in the patient’s mouth.
Figure 7.
Well-extended impressions of the arches of the patient are mounted on an articulator.
Therefore on the master cast the dental technician will prepare a removable wax-up of the teeth in the desired and corrected final position considering the clinician indications (Figure 8). After that with a laboratory scanner (e.g. Nobel Procera 2G), he will scan the models with and without wax-up charging the two relative STL files on Nobel Connect (Figure 9).
Figure 8.
On the master cast the dental technician will prepare a removable wax-up of the teeth in the desired and corrected final position.
Figure 9.
The dental technician will scan the models with and without wax-up charging the two relative files STL on Nobel Connect.
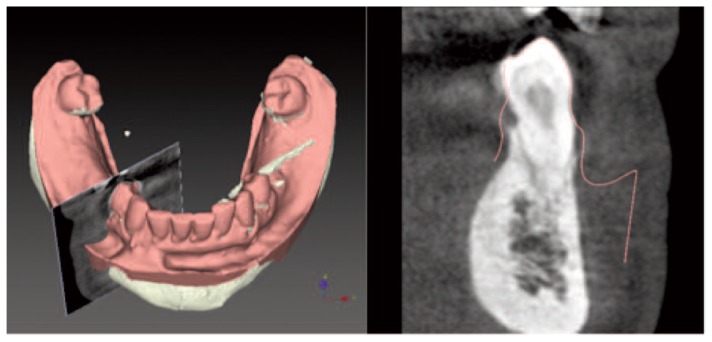
Then it will be possible for the clinician to download and match them with CBCT data (17, 23) (Figure 10).
Figure 10.
Fusion between digital dental casts and cone beam computed tomography.
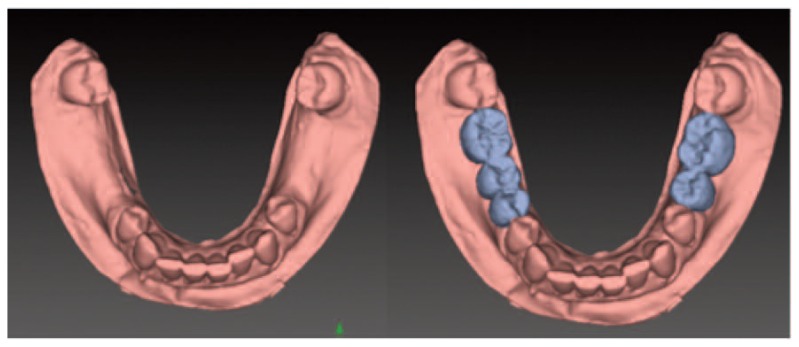
The software, first of all tries an automatic alignment of the different files. If it does not work, as in presence of big scattering or in situations where the remaining teeth are less than 6, the operator has to resort to a procedure of manual alignment called process of initialization. The same process is necessary when the alignment works, but it does not fulfill the clinician requirements. Afterwards the clinician is supposed to select three couples of points between the dental anatomical characterizations such as cusps, angles or margins, and then start again with the Smart Fusion calculation.
In some difficult cases this operation will be repeated different times before obtaining a good alignment. Once the alignment is acquired, it will be however controlled and verified carefully through a so called check alignment function (24) (Figure 11).
Figure 11.
Check alignment: this is a fundamental step in order to verify the correct superimposition between the two different files (STL and DICOM).
The operator, thanks to different and predefined colors for the patient’s anatomical model (yellow) and the prosthetic model (red), will be able to verify the correct matching point by point, sliding ahead and behind on the arch and magnifying the images (Figure 12).
Figure 12.
The operator, thanks to different and predefined colors for the patient’s anatomical model and the prosthetic model, will be able to verify the correct matching point by point.
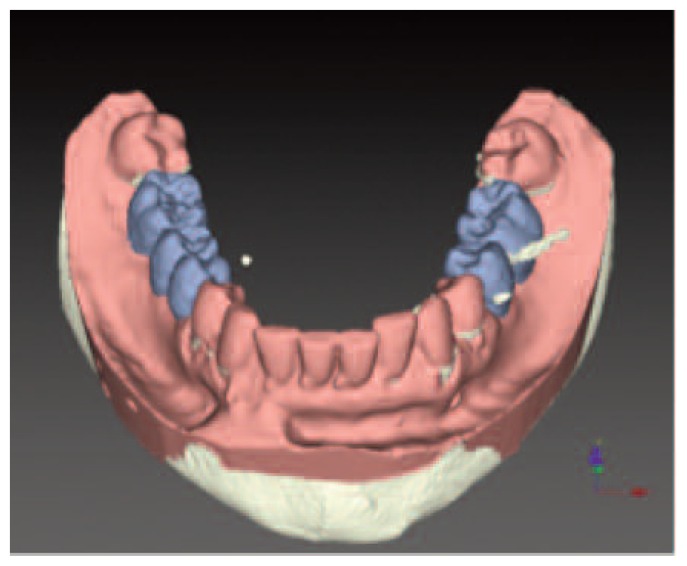
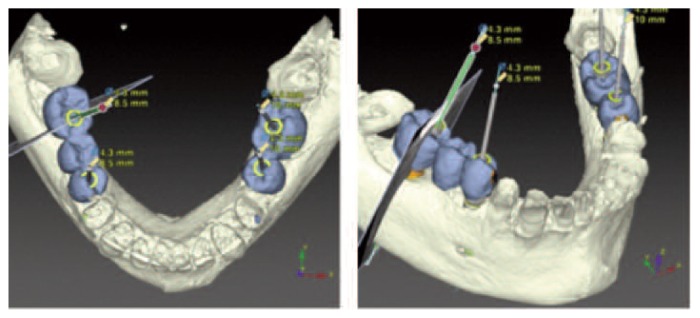
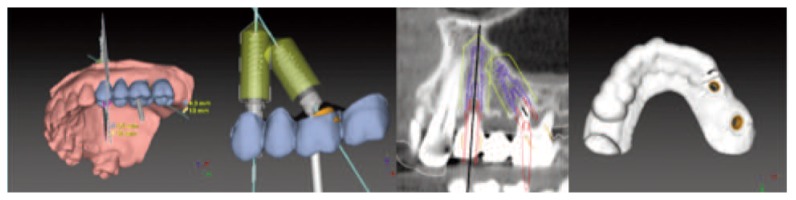
Once obtained a good alignment, the treatment planning can be performed using a dedicated 3D software (e.g. Nobel Clinician, Nobel Biocare AB) that allows for a prosthetic guided implant positioning (Figures 13, 14, 15).
Figure 13.
Procera Software Planning Program allows for prosthetic guided implant positioning.
Figure 14.
An ideal implant positioning can be achieved thanks to the 3D software.
Figure 15.
First of all the dental technician will verify the correct adaptation of the surgical template on the master model discarding some points of precontacts or friction.
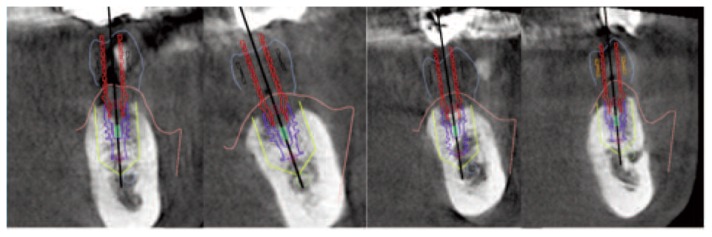
The virtual scene with the patient’s CT data is inspected with a 3D viewer, presenting a general overview of the scene. To visualize the cross-sectional reslice, the clinician interactively manipulates a curve that guides this reslice along the maxillary crest. With the zoom, rotate, and translate tools, every detail can be inspected. By a simple click of the mouse, the prosthesis informations can thus be introduced or removed from the image. Placing an implant is finally done intuitively by indicating a point on top of the bone crest and another more apically, mimicking the use of a drill. When the implant is thus apparent, the clinician can change the length, width, inclination or position taking also in consideration the distance between natural teeth or other implants. To such purpose a safety margin of 1.5 to 2 mm is always recommended. In this phase the operator, in order to avoid to include braces of forces in the final restoration could choose in advance between different prosthetic solutions (straight or tilted implants, screw retained or cemented restorations). It is obvious that the prosthetic components, also concurring to compensate problems of parallelism between implants, thanks to tilted abutments till 30°, unavoidably it will generate braces of forces. These will be able to alter in the time the health of the implant-supported complex, putting to hard the resistance of the mechanic components. The idea to have parallel implants, in the full respect of the anatomy, of the dental morphology and of the masticatory function, it can sure represent a large advantage from the biomechanic point of view. On the other hand the idea to have tilted implants, also representing an optimal rehabilitative compromise and a grate surgical simplification (18–31), little it’s suited to the idea of a prosthetic driven implant surgery, being neighbour to an old idea of implant surgery guided mainly by the existing bone. In such sense, this protocol represents nowadays one of the best solution available on dental market, in order to formulate an ideal treatment plan in terms of anatomy, function and aesthetic. At last, and this is an another of the news introduced from this protocol, at the end of the computer implant planning, the clinician will choose between two different type of surgical template, the traditional “full guided” one and another one in which only the first drill (a pilot drill Ø 2.0) is guided but all the other steps will be “free hand” without surgical template, included the finally implant positioning. To such purpose in recent review Van Assche et al. (25, 32, 33) illustrated that one has to accept a certain in-accuracy for guided surgery, which seems big at first view, but it is clearly lesser than that for non-guided surgery (26, 27, 34, 35).
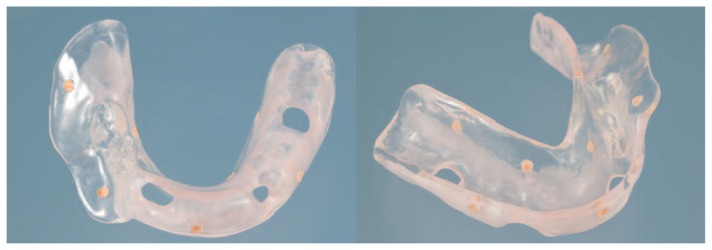
Laboratory procedure
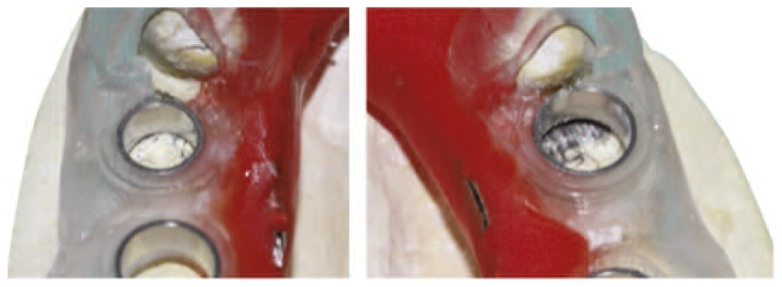
In case of immediate provisional restoration the surgical template provide all the necessary information (implant position, soft-tissue and teeth geometry) to make a pre-surgical stone model. First of all the dental technician will verify the correct adaptation of the surgical template on the master cast discarding some friction or contact points (Figures 16, 17).
Figure 16.
After the adjustment the surgical template seat well on the master cast.
Figure 17.
In many cases the Authors reinforce the surgical guide with acrylic resin.
After that the laboratory procedures include marking the implant approximate positions on the model through the sleeve of the template, cutting this section away from the cast and checking the correct position of the surgical guide over the model. In case of full guided surgical template, Nobel Guide specific laboratory components and implant replicas are attached, silicone gingiva applied and the removed section of the stone model filled with stone cast.
Instead in case of a “simple” surgical template, the dental technician after marking the implant approximate positions on the model through the sleeve, will cut this section away and put the implant replicas inside without specific laboratory components filling it again with plaster and silicone gingiva. It goes from that in these last cases the position of the implant’s replica will be able to differ from the planned position for depth and/or inclination. But this will not represent a problem from the moment that the temporary abutments will be blocked directly in patient’s mouth after surgery and so eventual discrepancies will be overwhelmed in that phase.
Surgical protocol
The day of the surgery the template will be checked in patient’s mouth, assessing any fit inaccuracies fit or surgical access inconveniences. In many cases the Authors also reinforce it with acrylic resin (Figures 18, 19).
Figure 18.
The day of the surgery the template will be checked in patient’s mouth, discarding some friction points.
Figure 19.
Surgical guide before and after relayning.
In these cases of partial edentulism with more than 6 teeth remaining generally the authors plan the surgical template without anchor pins. On their clinical experience they noticed in fact that the relayning of the template guarantees a very good stability during surgery but at the same time the possibility to remove it easily during the procedure. The reasons to remove the template during surgery could be different. First of all to remove more comfortably the excised oral mucosa after the use of the guided tissue punch otherwise difficult through the sleeves. Second but not less important to be able, in patients with limited mouth opening, to entry simultaneously with the complex template, drill and drill guide. Moreover it is not always easy to plan and put anchor pins between the dental roots. So the first step before surgery is the relayning of the surgical template with acrylic resin with a low percentage of contraction (e.g. Pattern Resin, GC) (Figure 20).
Figure 20.
Provisional and final restorations with the OPG and peri-apical control X-rays.
After that with the placement of the surgical template, a flap-less implant surgery is performed under local anesthetic, following the manufacturer’s instructions and a calibrated drilling protocol. The osteotomy site is prepared using the appropriate drilling guides and drills and finally the preplanned length and diameter of the implant is placed using an implant guide only in case of full guided surgical template. It goes specified that a flap approach is adopted in cases with lack or insufficient keratinized mucosa. Moreover in case of serious atrophied edentulous arches, where a simultaneous bone regeneration is needed, a simplified surgical template is used to guide the first drill and completing the surgical procedure “free hand”.
In fully guided cases with more than an implant, after the insertion of the first fixture a template abutment is inserted, which connected the surgical template to the placed implant, providing additional stability to the template. The other implants planned are inserted using the same drilling guides and twist drills make attention to put before the implants in the opposite side of the arch to guarantee the cross stabilization of the surgical guide.
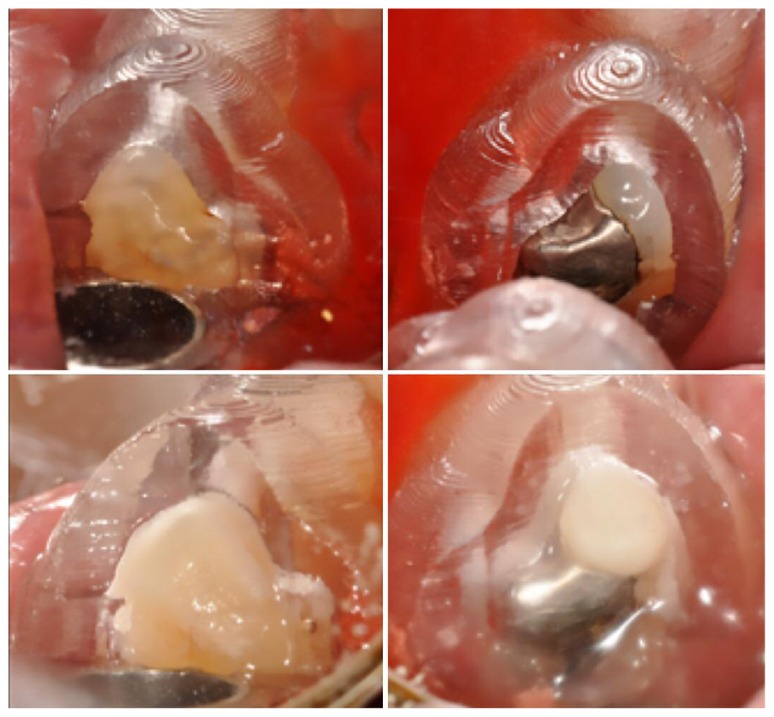
The authors always recommend after every single drill an additional cooling with cold physiological solution (28, 36). After implants placement, the surgical template is removed and when a good primary implant stability is achieved (35–45 N/cm) the abutments are screwed with a torque of 30 N/cm and the temporary crowns (cemented or screw-retained) are delivered after occlusal adjustment where needed (Figure 21).
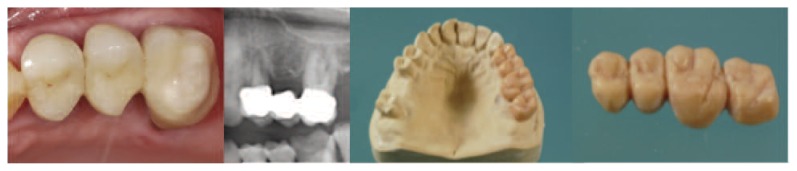
Figure 21.
Smart fusion protocol in post-extraction cases: initial situation and wax-up after removing teeth from master cast.
To such purpose the provisional restorations should be fabricated with narrow occlusal platforms, flat cusps, and light occlusal contacts to minimize the lateral forces.
The Authors prefer screw retained restorations because the risk of decementation of the other one during the first period of implant’s osteointegration, could represent a big problem. Completed the osteointegration phase a conventional protocol is followed to take an impression for manufacturing the definitive prosthesis.
Discussion
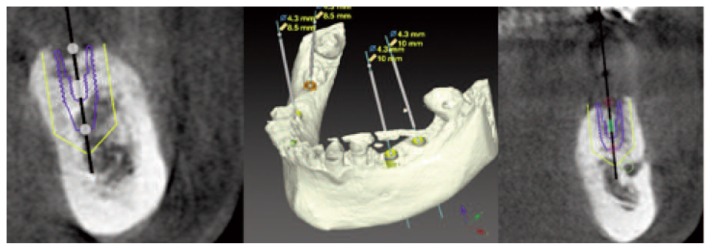
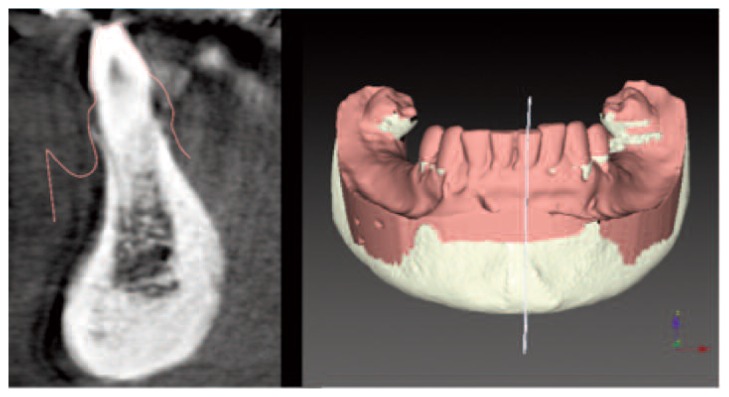
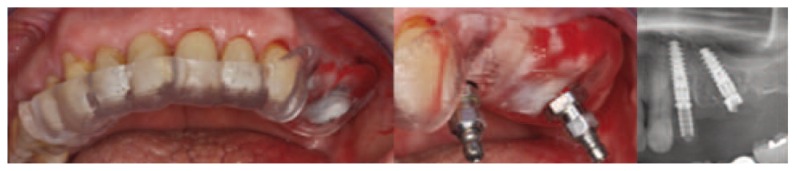
Computer guided (static) implant surgery is defined by the use of a static surgical template, using a scanned radiographic guide as reference, giving the clinician the opportunity to perform a predictable, personalized and non-invasive implant intervention that does not allow intra-operative modification of the planned implant position. Although concerns about the accuracy of computer guided implant surgery still exist, the rapid involving of the digital technology will sure enable further improvements in reducing the inaccuracy extending the indications of treatment also to the more complex cases. A crucial factor for the improvement of the accuracy seems to be to reduce the number of the steps needed from the preoperative examination to the actual execution of the guided surgery. To such care, the Authors want to emphasize the great advantage of the presented protocol, that in partially edentulous cases, permit to perform a full guided implant workflow without a radiographic template and a double scanning protocol. As a result, treatment time and laboratory work are reduced. Moreover there is no need for the clinician to try and personally accompany the patients in radiology in order to make sure itself of the correct positioning of the radiographic template, especially in post-extraction cases with disassembled template more difficult to manage (29, 37) (Figures 22, 23, 24). In double scanning procedure if the radiographic guide is placed wrongly, in fact, the implants could be planned and consequently placed incorrectly with the risk of vital structure lesion. In other words, nowadays, also patients who have already a valid 3D examination can enjoy totally the advantages of a minimally invasive guided implant surgery. This means that there is no more necessity of repeating a new examination with a radiographic guide with a consequent lengthening of the times and increasing of the economic and biological costs. This is possible thanks to the superimposition between the 3D reconstruction of the CBCT files and the digitalization of patient’s dental casts. To such purpose because the implant planning is generally done in the maxilla or in the mandible in separate stages, a convenient recommendation is to place an object between the superior and inferior teeth that is not detected by the CBCT (e.g. cotton rolls) to allow a separation between the jaws. Otherwise there is the risk of a wrong or impossible alignment between the two files. Another news of Smart Fusion protocol is represented by the fact that the surgical template can be fully or partially guided. In some challenging cases, such as in situation where is needed a simultaneous GBR, the clinician can choose for a simplified surgical guide with only the hole for the first drill (Ø2.0) and perform all the other surgical step free hand. However also this protocol have some critical steps that must be studied and analyzed. One of the technique’s first limitation is that this cannot be applied to fully edentulous patients. In order to guarantee the best fusion of the information and the ideal stability of the template during surgery is mandatory that patients have at least 6 teeth remaining distributed in 2 quadrants with less possible metallic restorations. This last condition is necessary to reduce artifacts and problems during the critical step of the alignment phase. As we said this must often to be completed manually. The clinician in fact have to choose “arbitrarily” at least three couple of points in common between the patient’s anatomical model (DICOM) and the digitalized dental cast. In cases with many metallic restorations this is not possible due to the big scattering and the clinician will be forced to follow a traditional protocol starting with a radiographic guide. In second place this new protocol like other protocol involving a surgical template may be contraindicated in patients with limited oral opening. The most common problem is in-fact a limited access in posterior areas during surgical procedures because of the longer than traditional drills and the bulk of the surgical guide. Moreover, in such kind of surgery, an additional effort must be made to ensure proper cooling during osteotomy preparation. As described before the authors always recommend after every single drill an additional cooling with cold physiological solution directly through the sleeve of the surgical template. Other surgical complications can include planning and placement of the implants too deeply into the osseous tissues with bony interferences that can prevent the complete seating of the prosthesis. In these cases, using a specifically designed bone mill, it is important to clear the excess of bone around the heads of the placed implants. Although an unavoidable increase of the cost and the planning time and the necessity of an adapted learning curve, the opinion of the Authors is that the Smart Fusion protocol, allowing to idealize the implant position in depth, inclination and mesio-distal distance between natural teeth or other implants (30, 38), could represent a good instrument for the best compromise between anatomy, function and aesthetic guaranteeing better results in all clinical situations (31, 39).
Figure 22.
Computer guided implant planning after the fusion between CBCT and the dental cast digitalized.
Figure 23.
Surgical procedure with stereolithographic template after removing the compromised teeth (mobility 3rd grade) and post-surgery Rx control.
Figure 24.
Final clinical situation with Rx-control.
Conclusions
Although once again it goes emphasized that caution should be exercised in the early stages of acquiring these skills, Smart Fusion protocol is one of the solution present on dental market enabling today to resolve many difficult cases, previously possible only in expert hands. Optimizing several treatment processes both in situations where complex anatomical limitations had previously precluded treatment or in critical esthetic cases. This could be done with or without immediate loading both with traditional or flapless approach which can lead to reduced morbidity. This improves the predictability of treatment goal, allows for a better risk management, and provides more individual information for the patient. These are the most important aspects of this technology, which may contribute to establish higher quality standards in implantology. Treatment planned in this way is fast, minimally invasive, and most importantly, predictable.
Elderly or medically compromised patients, and people suffering from fear or anxiety of surgical treatment may benefit greatly from the use of these protocol (32, 33, 40, 41). Last but not least, Smart Fusion not needing anymore a radiographic template, slims the digital workflow, involving a remarkable cost reduction, but moreover a great time contraction from the digital planning to the surgery. Finally, future improvements of the intra-oral scanners and the possibility to have a digital dental library within the planning software will concur a fully digital workflow from initial data capture till the final implant positioning. This promise to result in reduced cost and working time, and to involve more dental professionals in providing therapy earlier in their careers, making implants available to millions more patients who could benefit from them.
Acknowledgements
The authors would like to thank Prof. Alberto Barlattani for his precious scientific contribute and Ideal Laboratory of Rome for the technical work. The Authors reported no conflicts of interest related to this study.
References
- 1.De Vico G, Ottria L, Bollero P, Bonino M, Cialone M, Barlattani A, Jr, Gargari M. Aesthetic and functionality in fixed prosthodontic: sperimental and clinical analysis of the CAD-CAM systematic 3Shape. ORAL & Implantology. 2008;1(3–4):104–115. [PMC free article] [PubMed] [Google Scholar]
- 2.Marchack C. An immediately loaded CAD/CAM-guided definitive prosthesis: A clinical report. J Prosthet Dent. 2005;93:8–12. doi: 10.1016/j.prosdent.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Spinelli D, Ottria L, De Vico G, Bollero R, Barlattani A, Bollero P. Full Rehabilitation with Nobel Clinician ® and Procera Implant Bridge®: case report. ORAL & Implantology. 2013;VI(2):25–36. [PMC free article] [PubMed] [Google Scholar]
- 4.Pozzi A, Gargari M, Barlattani A. CAD/CAM technologies in the surgical and prosthetic treatment of the edentulous patient with biomimetic individualized approach. Oral & Implantology. 2008;I(1):2–14. [PMC free article] [PubMed] [Google Scholar]
- 5.Abboud M, Gerhard W, Calvo JLG, Gary O. Application and success of two stereolithographic surgical guide system for implant placement with immediate loading. JOMI. 2012;27:634–643. [PubMed] [Google Scholar]
- 6.Diamanti MV, Del Curto B, Barlattani A, Bollero P, Ottria L, Pedeferri M. Mechanical characterization of an innovative dental implant system. Journal of Applied Biomaterials and Biomechanics. 2009;7(1):23–28. [PubMed] [Google Scholar]
- 7.Eggers G, Patellis E, Munhling J. Accuracy of template-based dental implant placement. JOMI. 2009;24:447–454. [PubMed] [Google Scholar]
- 8.Van Assche N, Van Steenberghe D, Quirynen M, Jacobs R. Accuracy assestment of computer assisted flawless implant placement in partial edentulism. Journal of clinical periodontology. 2010;37:398–403. doi: 10.1111/j.1600-051X.2010.01535.x. [DOI] [PubMed] [Google Scholar]
- 9.Schneider D, Marquardt P, Zwahlen M, Jung RE. A sistematyc review on the accuracy and clinical outcome of computer guided template-based implant dentistry. COIR. 2009:73–86. doi: 10.1111/j.1600-0501.2009.01788.x. [DOI] [PubMed] [Google Scholar]
- 10.Gargari M, Prete V, Pujia M, Ceruso FM. Development of patient-based questionnaire about aesthetic and functional differences between overdentures implant-supported and overdentures tooth-supported. Study of 43 patients with a follow up of 1 year. ORAL and Implantology. 2012;5(4):86–91. [PMC free article] [PubMed] [Google Scholar]
- 11.Lin GH, Chan H-L, Bashutski JD, Oh T-J, Wang H-L. The effect of flapless surgery on implant survival and marginal bone level: A systematic review and meta analysis. Journal Periodontal. 2014;85:e91–e103. doi: 10.1902/jop.2013.130481. [DOI] [PubMed] [Google Scholar]
- 12.Vercruyssen M, Laleman I, Jacobs R, Quitynen M. Computer-supported planning and guided surgery: a narrative review. Clin Oral Impl Res. 2015;26(Suppl 11):69–76. doi: 10.1111/clr.12638. [DOI] [PubMed] [Google Scholar]
- 13.Pozzi A, Moy PK. Minimally Invasive Transcrestal Guided Sinus Lift (TGSL): A Clinical Prospective Proof-of-Concept Cohort Study up to 52 Months. Clinical Implant Dentistry and Related Research. 2013:1–12. doi: 10.1111/cid.12034. [DOI] [PubMed] [Google Scholar]
- 14.van Steenberghe D, Naert I, Andersson M, Brajnovic I, Van Cleynenbreugel J, Suetens P. A custom template and definitive prosthesis allowing immediate implant loading in the maxilla: a clinical report. Int J Oral Maxillofac Implants. 2002;17:663–670. [PubMed] [Google Scholar]
- 15.Clementini M, Ottria L, Pandolfi C, Bollero P. A Novel Technique to Close Large Perforation of Sinus Membrane. ORAL and Implantology. 2013;6(1):11–14. [PMC free article] [PubMed] [Google Scholar]
- 16.Tatullo M, Marrelli M, Falisi G, Rastelli C, Palmieri F, Gargari M, Zavan B, Paduano F, Benagiano V. Mechanical influence of tissue culture plates and extracellular matrix on mesenchymal stem cell behavior: A topical review. International Journal of Immunopa thology and Pharmacology. 2016;29(1):3–8. doi: 10.1177/0394632015617951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Vico G, Spinelli D, Bonino M, Schiavetti R, Pozzi A, Ottria L. Computer assisted virtual treatment planning combined with flawless surgery and immediate loading in the rehabilitation of partial edentulies. ORAL&Implantology. 2012;V(1):3–10. [PMC free article] [PubMed] [Google Scholar]
- 18.Gargari M, Comuzzi L, Bazzato MF, Sivolella S, di Fiore A, Ceruso FM. Treatment of peri-implantitis: Description of a technique of surgical 2 detoxification of the implant. A prospective clinical case series with 3-year follow-up. ORAL and Implantology. 2015;8(1):1–11. [Google Scholar]
- 19.Ottria L, Zavattini A, Ceruso FM, Gargari M. Maxillofacial prosthesis (P.M.F): In a case of oral-nasal communication post-surgery and post-radiotherapy. ORAL and Implantology. 2014;7(2):46–50. [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Rawi B, Hassan B, Vanderberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from Cone Beam Computed Tomography scans. Journal of Oral Rehabilitation. 2010;37:352–358. doi: 10.1111/j.1365-2842.2010.02065.x. [DOI] [PubMed] [Google Scholar]
- 21.Vandenberghe B, Jacobs R, Bosmans H. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur Radiol. 2010;20:2637–2655. doi: 10.1007/s00330-010-1836-1. [DOI] [PubMed] [Google Scholar]
- 22.Marrelli M, Falisi G, Apicella A, Apicella D, Amantea M, Cielo A, Bonanome L, Palmieri F, Santacroce L, Giannini S, Di Fabrizio E, Rastelli C, Gargari M, Cuda G, Paduano F, Tatullo M. Behaviour of dental pulp stem cells on different types of innovative mesoporous and nanoporous silicon scaffolds with different functionalizations of the surfaces. Journal of biological regulators and homeostatic agents. 2015;29(4):991–997. [PubMed] [Google Scholar]
- 23.Rangel FA, Male Tj, Bronkhorst EM, Breuning KH, Schols JG, Bergè SJ, Kuijpers-Jagtman AM. Accuracy and Reliability of a Novel Method for Fusion of Digital Dental Casts and Cone Beam Computed Tomography Scans. PLOS ONE. 2013;8(3):1–8. doi: 10.1371/journal.pone.0059130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gargari M, Prete V, Pujia A, Ceruso FM. Full-arch maxillary rehabilitation fixed on 6 implants. ORAL and Implantology. 2013;6(1):1–4. [PMC free article] [PubMed] [Google Scholar]
- 25.Maló P, Nobre MdA, Lopes A, Ferro A, Gravito I. Allon-4® Treatment Concept for the Rehabilitation of the Completely Edentulous Mandible: A 7-Year Clinical and 5-Year Radiographic Retrospective Case Series with Risk Assessment for Implant Failure and Marginal Bone Level. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e531–541. doi: 10.1111/cid.12282. [DOI] [PubMed] [Google Scholar]
- 26.Lopes A, Maló P, Nobre MdA, Sanchez-Fernández E. The NobelGuide® All-on-4® Treatment Concept for Rehabilitation of Edentulous Jaws: A Prospective Report on Medium- and Long-Term Outcomes. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e 406–416. doi: 10.1111/cid.12260. [DOI] [PubMed] [Google Scholar]
- 27.Malo P, Nobre MdA, Lopes A. The use of computer-guide flap less implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirteen months. J Prosthet Dent. 2007;97:526–534. doi: 10.1016/S0022-3913(07)60005-5. [DOI] [PubMed] [Google Scholar]
- 28.Maló P, Rangert B, Nobre M. All-on-Four immediate-function concept with Brånemark system implants for completely edentulous mandible: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2–9. doi: 10.1111/j.1708-8208.2003.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 29.Aparicio C, Perales P, Rangert B. Tilted implants as an alternative to maxillary sinus grafting: a clinical, radiologic, and periotest study. Clin Implant Dent Relat Res. 2001;3:39–49. doi: 10.1111/j.1708-8208.2001.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 30.De Vico G, Bonino M, Spinelli D, Schiavetti R, Sannino G, Pozzi A, Ottria L. Rationale for tilted implants. FEA considerations and clinical reports. ORAL&Implantology. 2011;4(3–4):23–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Krekmanov L, Kahn M, Rangert B, Lindstrom H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxiliofac Implants. 2000;15:405–414. [PubMed] [Google Scholar]
- 32.Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M. Accuracy of computer aided implant placement. COIR. 2012;23(Suppl 6):112–23. doi: 10.1111/j.1600-0501.2012.02552.x. [DOI] [PubMed] [Google Scholar]
- 33.Gargari M, Ottria L, Morelli V, Benli M, Ceruso FM. Conservative zirconia-ceramic bridge in front teeth. Case report. ORAL and Implantology. 2015;7(4):93–98. [Google Scholar]
- 34.Vercruyssen M, Cox C, Coucke W, Naert I, Jacobs R, Quirynen M. An RCT comparing guided implant surgery (bone or mucosa supported) with mental navigation or the use of a pilot-drill template. Journal of Clinical Periodontology. 2014;41:717–723. doi: 10.1111/jcpe.12231. [DOI] [PubMed] [Google Scholar]
- 35.Pozzi A, Tallarico M, Marchetti M, Scarfò B, Esposito M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1 year post- loading results of a multicentre randomized controlled trial. European Journal of Oral Implantology. 2014;3:229–242. [PubMed] [Google Scholar]
- 36.Misir AF, Sumer M, Yenisey M, Ergioglu E. Effect of surgical drill guide on heat generated from implant drilling. J Oral Maxillofac Surg. 2009;67:2663–8. doi: 10.1016/j.joms.2009.07.056. [DOI] [PubMed] [Google Scholar]
- 37.Cantone T, Polizzi G. Implant treatment planning in fresh extraction sockets: Use of a novel radiographic guide and CAD/CAM technology. Quintessence International. 2009;40(9):773–781. [PubMed] [Google Scholar]
- 38.Tarnow DP, Cho SC, Wallace SS. The effect of the inter- implant distance on the height of inter implant bone crest. Journal of periodontology. 2000;4:546–549. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 39.Van Assche N, van Steenberghe D, Guerrero ME, Hirsch E, Schutyser F, Quirynen M, Jacobs R. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. J Clin Periodontol. 2007;34:816–21. doi: 10.1111/j.1600-051X.2007.01110.x. [DOI] [PubMed] [Google Scholar]
- 40.Brand HS, Gortzak RA, Palmer-Bouva CC, Abraham RE, Abraham-Inpijn L. Cardiovascular and neuroendocrine responses during acute stress induced by different types of dental treatment. International Dental Journal. 1995;45:45–48. [PubMed] [Google Scholar]
- 41.Wong M, Lytle WR. A comparison of anxiety levels associated with root canal therapy and oral surgery treatment. Journal of Endodontics. 1991;17:461–465. doi: 10.1016/S0099-2399(07)80138-5. [DOI] [PubMed] [Google Scholar]