SUMMARY
The amount of marginal bone loss is considered an important criterion to evaluate the implant therapy outcome and to predict the prognosis of the implant rehabilitation.
The purpose of this systematic review was to examine the available literature comparing clinical and radiological outcomes like the implant failure rates and marginal bone loss around platform switching dental implants versus platform matching ones.
English randomized controlled human clinical trials, comparing one or more PS groups with one or more PM groups, with at least 12 months of follow-up after loading and 10 implants, providing carefully the number of PS- and PM- implants used as well as implant survival and data concerning bone level changes or marginal bone loss around implants, were included. Fifteen publications, involving a total of 1439 implants and 642 patients, were eligible. More studies showed less mean marginal bone loss around PS implants and none of them showed differences in terms of implant failure rates.
This review confirmed a great effectiveness of platform switching technique to prevent marginal bone resorption. Nevertheless, this result should be interpreted cautiously because of the heterogeneity of the included studies.
Keywords: platform switching implants, platform shifting implants, implant-abutment design, marginal bone loss, review
Introduction
The rehabilitation of partial and total edentulism using dental implants showed highly satisfactory clinical outcomes (1). Crestal bone loss around dental implants of 1.5mm during the first year followed by a loss of 0.2mm in the subsequent years has been generally considered acceptable for two-piece dental implants (2, 3). Radiographic evaluation of crestal bone level changes after prosthetic restoration is considered one important criterion to evaluate clinical outcome (4).
Marginal bone loss (MBL) around dental implants has been attributed to several factors. It may be the result of the establishment of a pathogenic microflora, promoting the occurrence of peri-implant diseases with mucosal inflammation, increased pocket depth and progressive bone resorption (5, 6). Other studies suggested that marginal bone level changes may be the result of biomechanical stress due to incorrect occlusal design (7). Crestal bone loss (CBL) may also be the physiological result of incorrect three-dimensional fixture positioning. The coronal portion of bone may tend to resorb if the fixture is placed too close to the adjacent teeth/implants or to a thin residual buccal wall (8). The subcrestal positioning of the implant platform may adversely affect the stability of peri-implant marginal bone (9, 10). Crestal bone resorption is also linked to the presence of a microgap between implant and abutment and to the location of this microgap in relation to level of the crestal bone. Implants placed above the alveolar crest have been shown to prevent crestal bone resorption (11). SEM observations demonstrated biofilm formation in implant-abutment microgap permitted by a screw loosening (12). The implant-abutment connection is thought to be an important factor regarding peri-implant bone loss because of the highest number of inflammatory cells close to the implant-abutment interface (13–16). Furthermore, the biological width re-establishment may occur as result of micromovements at the implant-abutment interface (17, 18) (IAI).
The rationale behind physiological bone resorption is to be found on the re-establishment of the peri-implant biological width. It is a consistent mucosal attachment characterized by a junctional epithelium and suprabony connective fibres; the peri-implant biological width is the minimum mucosal dimension required to protect the osseointegration (19).
In 2006, Lazzara & Porter found a better long-term preservation of marginal bone around wide-diameter dental implants connected with standard-diameter components, due to commercial temporary unavailability of matching abutment (20). So, the potential benefit of platform switching (PS) was discovered casually due to a production delay of prosthetic components. X-rays of the restored implants exhibited minimal alveolar crestal bone remodelling around platform-switched implants. These X-ray observations led to development of platform switching (PS) technique, the PS effect occurs when the diameter of the abutment is less than the diameter of the implant, resulting in a horizontal offset at the top of the implant that separates the crestal bone and the connective tissue from the interface (21).
The Authors assumed that through the inward positioning of the implant/abutment junction: the distance of the junction in relation to the adjacent crestal bone and the surface area to which the soft tissue can attach and establish a biological width was increased and, therefore, bone resorption at the implant-abutment junction associated with the inflammatory cell infiltrate was reduced (45).
Biomechanical simulations using finite element analyses at implants with PS confirmed a reduction of the loading stress at the bone-implant interface (22–24). In fact, different connection geometries influences in different ways the mechanical properties of an implant system (25, 26). Microbiological evaluations assessed that implants characterized by a tube-in-tube IAI with platform switching were more resistant to bacteria as well as yeast colonization (27).
The knowledge in the field of PS could be used to create new better implant platforms, one of these is the BioPlatform, patent pending (GTB- Plan1Health Amaro, UD, Italy) (19, 28). Bio-Platform, patent pending® (GTB- Plan1Health Amaro, UD, Italy) (Figures 1, 2 and 3) has a concave and convex platform, and the connection with the abutment is switched inward and apically. This new type of implant shoulder has four important strengths:
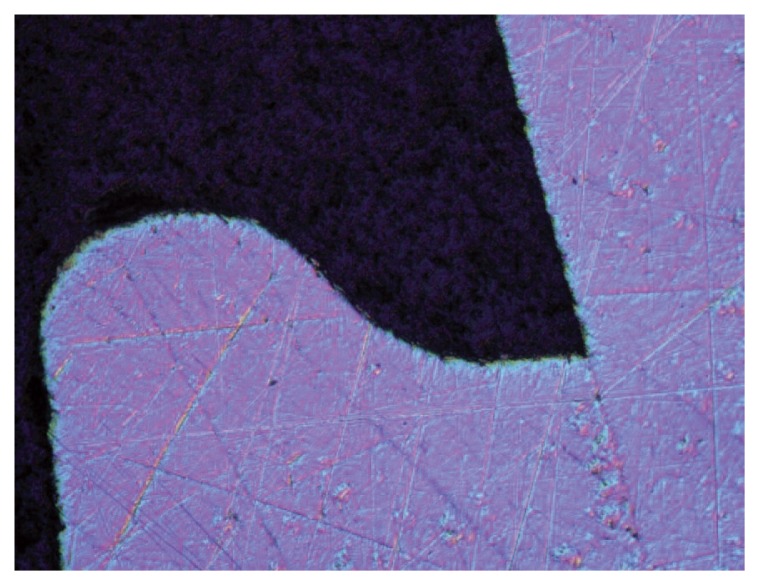
Figure 1.
Implant shoulder of BioPlatform, patent pending® (GTB-Plan1Health Amaro, UD, Italy). Image obtained using an optical microscope. The implant-abutment connection is an internal tube-in-tube connection. The concave and convex platform provides a horizontal and vertical mismatch.
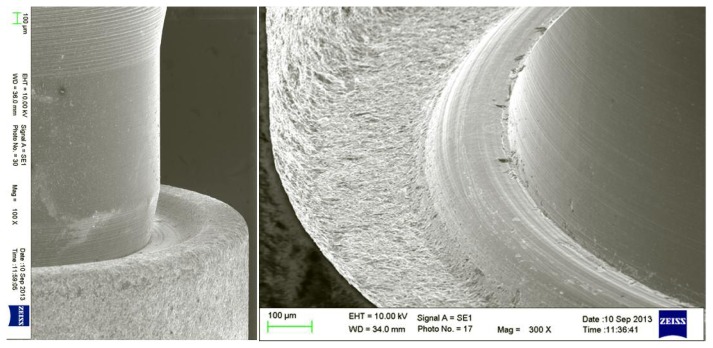
Figures 2–3.
Scanning electronic microscope observations of BioPlatform, patent pending® (GTB- Plan1Health Amaro, UD, Italy). The complex platform has a concave and convex outline. Thanks to the vertical shifting, the first implant-abutment contact is lower than the outer part of implant’s shoulder.
- the implant platform, providing both vertical and horizontal mismatch, offers a larger surface useful for the osseointegration and for the biological seal;
- thanks to a vertical and horizontal mismatch, there is a bigger distance between IAI and crestal bone;
- the IAI is lightly lower than the outer part of the implant’s shoulder so, even if implant is placed at the bone level, the biomechanical pattern may take advantage of the benefits of a subcrestal positioning;
- the concave and convex outline makes stronger the entire structure of the implant neck.
Aim of this paper is to systematically review the highest available evidence, to assess the difference in terms of implant survival and marginal bone loss between implant restored with platform matching or platform switching technique.
Methods
This systematic literature review was conducted considering the PICO format. “P” stays for population: patients undergoing implant-prosthetic rehabilitation, which were included into RCTs, comparing peri-implant marginal bone loss around endosseous implants with platform switching (PS) or platform matching (PM) configurations. “I” stays for intervention: the use of endosseous dental implants with a PM (the abutment diameter and implant neck diameter were identical) or PS (the abutment diameter was medialized compared with the implant neck diameter) implant-abutment-configuration. “C” stays for comparison and “O” for outcome: clinical studies comparing treatment outcomes using PM and PS implant-abutment connections, with special consideration of radiographically detected peri-implant MBL changes. The purpose was to find any differences, between platform switching implants (PS) compared to platform matching ones (PM), in terms of marginal bone level changes and implant survival.
Selection of studies
Only RCTs comparing PS implants with PM ones, in relation to the implant survival rate and the marginal bone loss over time, considering at least 10 implants and 12 months of follow up from loading, were included. Only articles in English language were included, too.
Published articles not meeting the inclusion criteria were excluded (i.e., publications in languages others than English, case reports, expert opinions, narrative reviews on the subject of platform switching, animal studies, in vitro experiments, clinical studies on platform switching without a control group utilizing platform matching implant-abutment configuration, articles lacking of important data like number of implants). As well, articles were excluded if implants were placed in bone modified with ridge augmentation techniques. Besides, publications were not included if they did not provide the total number of implants used, the number of PM- and PS-implant used, implant survival and data concerning bone level changes or marginal bone loss around implants and the comparison of both.
Search strategy
A bibliographical electronic research was carried out on PubMed/Medline, selecting all published articles dealing with platform switching technique.
The group of MeSH or Free text words used was: {(dentistry[MeSH Terms]) OR (dental implants[ MeSH Terms]) OR (oral implants) OR (implant restoration)} AND [(platform switching) OR (platform shifting) OR (platform-matched implants) OR (non platform-switched implants) OR (matching abutment) OR (switched abutment) OR (implant-abutment)] AND {(survival) OR (success) OR (outcome assessment[MeSH Terms])}. The electronic outcome was: (“dentistry”[MeSH Terms] OR “dental implants”[MeSH Terms] OR {(“mouth”[MeSH Terms] OR “mouth”[All Fields] OR “oral”[All Fields]) AND implants [All Fields]) OR (implant[All Fields] AND restoration [All Fields])} AND (platform[All Fields] AND switching[All Fields]) OR (platform[ All Fields] AND shifting[All Fields]) OR (platform-matched[All Fields] AND implants [All Fields]) OR (non[All Fields] AND platform-switched[All Fields] AND implants[All Fields]) OR (matching[All Fields] AND abutment[ All Fields]) OR (switched[All Fields] AND abutment[All Fields]) OR implant-abutment[ All Fields]) AND ((“mortality”[Subheading] OR “mortality”[All Fields] OR “survival”[ All Fields] OR “survival”[MeSH Terms]) OR success[All Fields] OR “outcome assessment (health care)”[MeSH Terms]).
In addition, a specific search limited to articles published between January 2010 to March 2016 in Journal of Clinical Periodontology, Journal of Dental Research, Caries Research, Oral Oncology, Monographs in Oral Science, Molecular Oral Microbiology and Clinical Oral Implants Research was performed.
Data searched
Only human clinical studies, designed as RCTs, comparing platform switched versus platform matched titanium, screw-shaped, implants and reporting implant survival and marginal bone loss were selected. Primary outcome measures considered were implant failure rate and crestal bone loss. Implant failure rate was defined as the percentage of implants lost, in relation to implants placed, at the time of observation. Again, crestal bone loss had to be expressed as the radiographically observed and numerically quantified difference in peri-implant marginal bone level between baseline and follow-up, in relation to a specified anatomical landmark.
For each included trial several data regarding number of patients, number of implants, place of positioning, implant diameter and length, length of mismatch, type of implants and reported outcomes were rewrote. A patient-based analysis was conducted, comparing PS and PM values of bone level changes in the single patient, at last follow-up.
Results
The electronic search found 315 studies (Figure 4) and the manual search provided 37 additional publications. Of the three hundred and fifteen articles, 46 were uploaded as RCTs. After abstract examination, 29 articles of forty-six were excluded because not comparing one or more PM groups with one or more PS groups, but investigating the impact of: implant micro- or macrodesign, prosthetic load, abutment materials, sinus lift or ridge augmentation, implant systems, implant surgery techniques or prosthesis’ materials.
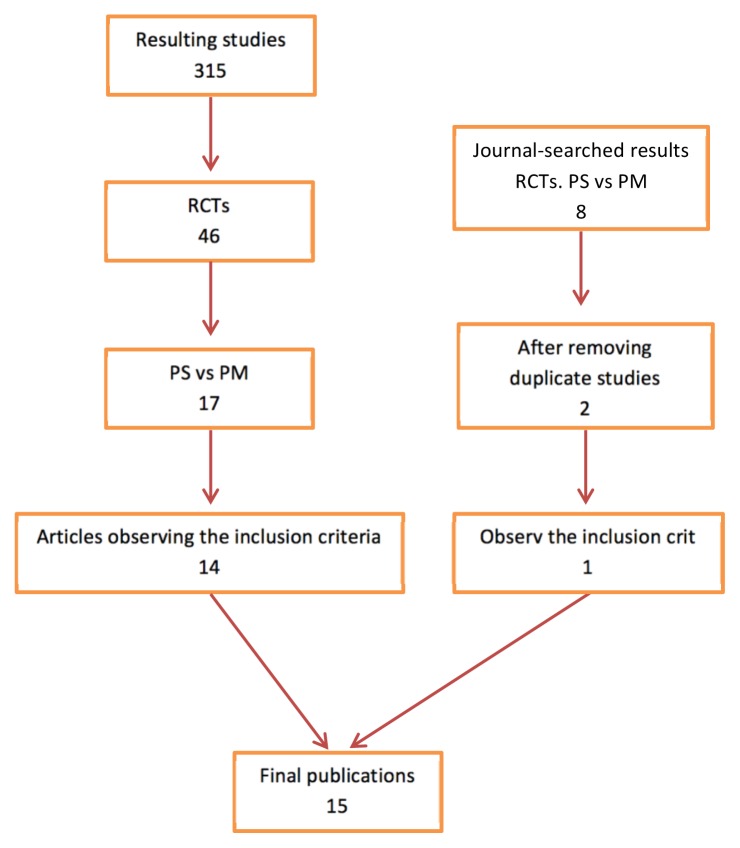
Figure 4.
Search strategy, screening for eligibility and final number of included publications. The electronic search found 315 studies regarding PS technique, 46 of them were RCTs, 14 compared PS and PM groups and were in agreement with the inclusion criteria. The manual search provided 8 RCTs, 6 of them were in common with the electronic search, 1 of them did not observe the inclusion criteria and 1 was included and evaluated. Thus, this review was finalized with 15 articles.
17 articles of forty-six were included in this review because they were RCTs analysing the role (29) of platform switching after a comparison between PS and PM groups, and 14 of them were in agreement with the inclusion criteria (28, 30–42).
The manual search provided 37 additional publications about platform switching technique; 11 were RCTs; 8 of them were RCTs comparing PS groups with PM ones. Six of eight articles were in common with the electronical research so they were included just one time, one was excluded because its deficiency of data, and only 1 article was added to the electronic research (34, 42). Thus, this review was finalized with 15 articles (43, 44).
The main characteristics of included publications are in Table 1. The selected studies were RCTs published between 2009 (39–41) and 2016 (42). The number of patients in the last follow-up in each study varied from 9 (35) to 92; and the number of implant was from 22 (40) to 149 (31). The last available follow-up was between 1 year (29, 31–34, 36, 37) and 3 years (28, 30, 35, 38, 42).
Table 1.
Comparison of bone level changes, implant survival rates and other main features of implants described in RCTs included in the present review.
| Author | Year | N° patient | N° implant | Place | Implant length | Implant diameter | Mismatch | Type of implant or connection | Survival | Bone level changes (mm) | follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pozzi* | 2014a | 34 tot | 88 tot | Posterior. Lower jaw. | 8.5mm | 4.3mm PS | 0.2mm | NobelActive (PS) | 100% | −0.83±0.27 PS | 3 year |
| 34 PS | 44 PS | 10mm | 4.0mm PM | NobelSpeedy Groovy (PM) | −1.29±0.42 PM | ||||||
| 34 PM | 44 PM | 11.5mm | |||||||||
| 13mm | |||||||||||
|
| |||||||||||
| Guerra* | 2014 | 66 tot | 144 tot | Posterior. Lower jaw. | 9mm | 3.8mm | 0.3mm | Camlog Screw-Line | 97.3% PS | −0.40±0.46 PS | 1 year |
| 33 PS | 72 PS | 11mm | 4.3mm | 0.3mm | 100% PM | −0.69±0.58 PM | |||||
| 33 PM | 72 PM | 13mm | 5.0mm | 0.35mm | |||||||
|
| |||||||||||
| Enkling | 2013 | 25 tot | 50 tot | Posteriori. Lower jaw. | 9.5mm | 4mm | 0.35mm | SIC Ace implant | 100% | −0.69±0.43 PS | 3 years |
| 25 PS | 25 PS | −0.74±0.57 PM | |||||||||
| 25 PM | 25 PM | ||||||||||
|
| |||||||||||
| Telleman* | 2013 | 92 tot | 149 tot | Posterior. Upper jaw & Lower jaw. | 8.5mm | 4mm | 0.35mm | Certain Prevail (PS) | 95.9% PS | −0.50±0.53 PS | 1 year |
| 45 PS | 73 PS | 5mm | 0.40mm | XP Certain (PM) | 92.1% PM | −0.74±0.61 PM | |||||
| 47 PM | 76 PM | ||||||||||
|
| |||||||||||
| Pozzi* | 2014b | 34 tot | 88 tot | Posterior. Lower jaw. | 10mm | 4.3mm PS | 0.2mm | NobelActive (PS) | 100% | −0.51±0.34 PS | 1 year |
| 44 PS | 13mm | 4.0mm PM | NobelSpeedy Groovy (PM) | −1.10±0.52 PM | |||||||
| 44 PM | |||||||||||
|
| |||||||||||
| Telleman* | 2014 | 17 tot | 62 tot | Posterior. Upper jaw & Lower jaw. | 8.5mm | 4mm | 0.35mm | Certain Prevail (PS) | 93,6% PS | −0.53±0.54 PS | 1 year |
| 17PS | 31PS | 5mm | 0.40mm | XP Certain (PM) | 93.6% PM | −0.85±0.65 PM | |||||
| 17 PM | 31PM | ||||||||||
|
| |||||||||||
| Telleman* | 2012 | 78 tot | 106 tot | Prem & mol. Upper jaw & Lower jaw. | 8.5mm | 4mm | 0.35mm | Certain Prevail (PS) | 94.5% PS | −0.51±0.51 PS | 1 year |
| 40 PS | 52 PS | 5mm | 0.40mm | XP Certain (PM) | 93.1% PM | −0.73±0.48 PM | |||||
| 38 PM | 54 PM | ||||||||||
|
| |||||||||||
| Canullon.p. | 2011 | 10 tot | 24 tot | Posterior. Upper jaw. | 13mm | 3.8mm | 0.25mm | Global Implant | 100% | −0.83±0.44 PS1 | 3 years |
| 6 PS1 | 6 PS1 | 4.3mm | 0.50mm | −0.49±0.22 PS2 | |||||||
| 4 PS2 | 6 PS2 | 4.8mm | 0.85mm | −0.38±0.12 PS3 | |||||||
| 6 PS3 | 6 PS3 | 5.5mm | −1.36±0.39 PM | ||||||||
| 5 PM | 6 PM | ||||||||||
|
| |||||||||||
| Pieri* | 2011 | 38 tot | 38 tot | Posterior. Upper jaw. | n.p. | n.p. | 0.35 | Morse taper for PS | 94.7% PS | −0.20±0.17 PS | 1 year |
| 18 PS | 18 PS | 100% PM | −0.51±0.24 PM | ||||||||
| 20 PM | 20 PM | ||||||||||
|
| |||||||||||
| Enkling | 2011 | 25 tot | 50 tot | Posterior. Lower jaw. | 9.5mm | 4mm | 0.35mm | SICace implant | 100% | −0.53±0.35 PS | 1 year |
| 25 PS | 25 PS | −0.58±0.55 PM | |||||||||
| 25 PM | 25 PM | ||||||||||
|
| |||||||||||
| Canullo* | 2010 | 26 tot | 61tot | Posterior. Upper jaw. | 13mm | 3.8mm | 0.25mm | Global Implant | 100% | −0.99±0.42 PS1 | 3 years |
| 17PM | 4.3mm | 0.50mm | −0.87±0.43 PS2 | ||||||||
| 17PS 1 | 4.8mm | 0.85mm | −0.64±0.32 PS3 | ||||||||
| 13PS 2 | 5.5mm | −1.48±0.42 PM | |||||||||
| 14PS 3 | |||||||||||
|
| |||||||||||
| Crespi | 2009 | 45 tot | 64 tot | Anterior and premolar. Upper and lower jaws. | 14mm PS | 4.5mm PS | n.p. | Morse cone for PS | 100% | −0.73±0.52 PS | 2 years |
| n.p. PS | 30 PS | 13mm PM | 3.5mm PS | −0.78±0.45 PM | |||||||
| n.p. PM | 34 PM | 3.8mmPM | |||||||||
| 5.0mm PM | |||||||||||
|
| |||||||||||
| Canullo* | 2009 | 22 tot | 22 tot | Anterior and premolar. Upper jaw. | 13mm | 5.5mm | 0.85mm | Double internal connection | 100% | −0.30±0.16 PS | 2 years |
| 11 PS | 11 PS | −1.19±0.38 PM | |||||||||
| 11 PM | 11 PM | ||||||||||
|
| |||||||||||
| Prosper* | 2009 | 60 tot | 360 tot | Posterior. Upper and lower jaws. | 11mm | 3.3mm | 0.25mm | Internal connection | 100% PS | PS1, PM1=MBL≤0 | 2 years |
| 60 PS1 | 120 PS | 13mm | 3.8mm | 0.35mm | 96.7 PM | −0.04±0.23 PS2 | |||||
| 60 PS2 | 240 PM | 15mm | 4.5mm | −0.27±0.47 PM3 | |||||||
| 60 PM1 | 5.2mm | ||||||||||
| 60 PM2 | |||||||||||
| 60 PM3 | |||||||||||
| 60 PM4 | |||||||||||
|
| |||||||||||
| Rocha* | 2016 | 63 tot | 135 tot | Posterior. Lower jaw. | 9mm | 3.8mm | 0.3mm | Camlog Screw-Line | 97.3% PS | −0.28±0.56 PS | 3 years |
| 69 PS | 11mm | 4.3mm | 0.35mm | 97.1% PM | −0.68±0.64 PM | ||||||
| 66 PM | 13mm | 5.0mm | |||||||||
PS= platform switching. PM= platform matching.
n.p.= not provided.
MBL=marginal bone loss
significant difference in bone level changes
Six studies reported results obtained from mandibular sites (28–30, 32, 37, 42), four studies reported data from maxilla (35, 36, 38, 40) and in five articles implants were placed in mandibula as well in maxilla (31, 33, 34, 39, 41).
All implant samples included titanium, root-form, tapered implants. The implant length varied from 8.5mm (28, 31, 33, 34) to 15mm (41); the diameters were from 3.3mm (41) to 5.5mm; the mismatch used ranged from 0.2mm per side (28, 32) to 0.85mm per side (35, 38, 40).
The implant failure reported in the last follow-up was not statistical different between the groups. It ranged from 0% with survival rate of 100% (28, 29, 30, 32, 35–42) to 7.9% with 92.1% of survival rate (31). Eight articles have an implant survival rate of 100% in both groups (28, 30, 32, 35, 38–40), and studies reporting differences in implant failure rates between PS- and PM- groups (29, 31, 33, 34, 36, 41, 42) showed no statistical difference.
The bone level changes was not over −1.48mm (38) and it was reported after 3 years of follow-up. The best bone preservation for PS groups showed a marginal bone loss (MBL) of −0.04mm (41), and the worse was −0.99mm (38). About PM groups, the best outcome was −0.27mm (41) and the worse was −1.48mm (38).
Eleven articles of fifteen showed a statistical significant difference in MBL between PS implants and PM ones, with better preservation of marginal bone in PS groups (28, 29, 31–34, 36, 38, 40–42). Three articles reported a slight difference between the two groups that failed to achieve statistical significance (30, 37, 39). One article reported only means and standard deviations for the two groups, without testing them for statistical differences (35), the difference was remarkable in favour of the PS group, but a statistical analysis to calculate the level of significance was not performed because the primary intention of the authors was to correlate clinical outcomes with immunohistochemical ones.
Discussion
This systematic review was conducted to investigate the impact of platform switching on crestal bone loss around osseointegrated implants. The amount of marginal bone loss is considered an important criterion for the evaluation of implant therapy outcome and an evidence for the presence or absence of peri-implant tissue health (4). Therefore, efforts were made to preserve the peri-implant MBL stable throughout and following the prosthetic loading phase.
Comparing subgroups available in the included studies:
- the difference in estimate marginal bone loss between PS and PM implants was significant both for studies with an implant-abutment diameter difference bigger than 0.45 mm, and for those where the difference was less than 0.45 mm; but the statistical analysis showed better results for implants with larger mismatch (35, 38);
- data related to longer follow up were associated to better results of PS implants if compared with PM ones (42);
- about timing of implant placement, PS implants showed better clinical results in subgroups of implants placed in healed sites (35, 37, 38, 41), while PS implants placed in post-extraction sites (36, 40, 39) just reached a borderline significance in the estimate treatment effect.
Although all included studies were RCTs, the analysis of the methodological quality of some of them revealed some potential criticisms, i.e. bias for reporting incomplete outcome data, due to dropouts or exclusion after randomization.
Some Authors did not report the periodontal health status of the patients included into the study. However, inclusion of periodontally compromised patients can be supposed by the fact, that patients requiring tooth removal due to periodontitis were included in two of these studies (36, 39). And, none of the studies included into this systematic review, investigated the effects of PS on peri-implant marginal bone loss among smokers compared with non-smokers.
Adding available data, 1439 implants were placed in 642 patients. 675 implants were restored following the PS technique, 764 were restored with matching abutments following the traditional technique. More studies showed better results using PS implants to prevent MBL; despite the fact that heterogeneity among the study conditions is supposed to have a crucial influence on study outcomes, a significantly less mean MBL change at PS implants compared with PM implants was found, thus confirming the supposed bone level stabilizing effect of PS implant-abutment configurations. Therefore, the present study assessed that there are differences among platform switching and conventionally restored implants in terms of marginal bone loss with better results for PS groups; on the other hand, there are no statistical differences about implant survival rates.
Conclusion
Within the limits of the present work, it could be concluded that platform switching technique is useful to reduce marginal bone loss around dental implants. More randomized controlled clinical trials with bigger samples are needed to confirm our findings, but the current evidence demonstrates that mismatches larger than 0.45mm, implants placed in healed sites and studied for long follow-up show the best performance. Due to heterogeneity of the included studies, this results should be interpreted cautiously.
New designs of the implant platform could achieve even better results. The convex and concave outline of the BioPlatform, patent pending (GTB- Plan1Health Amaro UD Italy) shifts the IAI inward and vertically simulating a subcrestal positioning even if implants are placed at the bone level, and taking advantage of the benefits of huge mismatches even using narrow implants.
Footnotes
Conflict of interest
The Authors declare no conflict of interest.
References
- 1.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. [DOI] [PubMed] [Google Scholar]
- 2.Albrektsson TO, Johansson CB, Sennerby L. Biological aspects of implant dentistry: osseointegration. Periodontol 2000. 1994;4:58–73. doi: 10.1111/j.1600-0757.1994.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 3.Tatullo M, Marrelli M, Falisi G, Rastelli C, Palmieri F, Gargari M, Zavan B, Paduano F, Benagiano V. Mechanical influence of tissue culture plates and extracellular matrix on mesenchymal stem cell behavior: A topical review. International Journal of Immunopa thology and Pharmacology. 2016;29(1):3–8. doi: 10.1177/0394632015617951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11–25. [PubMed] [Google Scholar]
- 5.Lindhe J, Meyle J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(8 Suppl):282–5. doi: 10.1111/j.1600-051X.2008.01283.x. [DOI] [PubMed] [Google Scholar]
- 6.Marrelli M, Falisi G, Apicella A, Apicella D, Amantea M, Cielo A, Bonanome L, Palmieri F, Santacroce L, Giannini S, Di Fabrizio E, Rastelli C, Gargari M, Cuda G, Paduano F, Tatullo M. Behaviour of dental pulp stem cells on different types of innovative mesoporous and nanoporous silicon scaffolds with different functionalizations of the surfaces. Journal of biological regulators and homeostatic agents. 2015;29(4):991–997. [PubMed] [Google Scholar]
- 7.Rungsiyakull C, Rungsiyakull P, Li Q, Li W, Swain M. Effects of occlusal inclination and loading on mandibular bone remodeling: a finite element study. Int J Oral Maxillofac Implants. 2011;26(3):527–37. [PubMed] [Google Scholar]
- 8.Tomasi C, Sanz M, Cecchinato D, Pjetursson B, Ferrus J, Lang NP, Lindhe J. Bone dimensional variations at implants placed in fresh extraction sockets: a multilevel multivariate analysis. Clin Oral Implants Res. 2010;21(1):30–6. doi: 10.1111/j.1600-0501.2009.01848.x. [DOI] [PubMed] [Google Scholar]
- 9.Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113–9. [PubMed] [Google Scholar]
- 10.Gargari M, Prete V, Pujia M, Ceruso FM. Development of patient-based questionnaire about aesthetic and functional differences between overdentures implant-supported and overdentures tooth-supported. Study of 43 patients with a follow up of 1 year. ORAL and Implantology. 2012;5(4):86–91. [PMC free article] [PubMed] [Google Scholar]
- 11.Farronato D, Santoro G, Canullo L, Botticelli D, Maiorana C, Lang NP. Establishment of the epithelial attachment and connective tissue adaptation to implants installed under the concept of “platform switching”: a histologic study in minipigs. Clin Oral Implants Res. 2012;23(1):90–4. doi: 10.1111/j.1600-0501.2011.02196.x. [DOI] [PubMed] [Google Scholar]
- 12.Calcaterra R, Di Girolamo M, Mirisola C, Baggi L. Effects of Repeated Screw Tightening on Implant Abutment Interfaces in Terms of Bacterial and Yeast Leakage in Vitro: One-Time Abutment Versus the Multiscrewing Technique. Int J Periodontics Restorative Dent. 2016;36(2):275–80. doi: 10.11607/prd.2082. [DOI] [PubMed] [Google Scholar]
- 13.Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL. Peri-implant inflammation defined by the implant-abutment interface. J Dent Res. 2006;85(5):473–8. doi: 10.1177/154405910608500515. [DOI] [PubMed] [Google Scholar]
- 14.Piattelli A, Vrespa G, Petrone G, Iezzi G, Annibali S, Scarano A. Role of the microgap between implant and abutment: a retrospective histologic evaluation in monkeys. J Periodontol. 2003;74(3):346–52. doi: 10.1902/jop.2003.74.3.346. [DOI] [PubMed] [Google Scholar]
- 15.Gargari M, Prete V, Pujia A, Ceruso FM. Full-arch maxillary rehabilitation fixed on 6 implants. ORAL and Implantology. 2013;6(1):1–4. [PMC free article] [PubMed] [Google Scholar]
- 16.Diamanti MV, Del Curto B, Barlattani A, Bollero P, Ottria L, Pedeferri M. Mechanical characterization of an innovative dental implant system. Journal of Applied Biomaterials and Biomechanics. 2009;7(1):23–28. [PubMed] [Google Scholar]
- 17.Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72(10):1372–83. doi: 10.1902/jop.2001.72.10.1372. [DOI] [PubMed] [Google Scholar]
- 18.Spinelli D, Ottria L, De Vico GD, Bollero R, Barlattani A, Jr, Bollero P. Full rehabilitation with nobel clinician ® and procera implant bridge®: Case report. ORAL and Implantology. 2013;6(2):25–36. [PMC free article] [PubMed] [Google Scholar]
- 19.Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996;23(10):971–3. doi: 10.1111/j.1600-051x.1996.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 20.Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9–17. [PubMed] [Google Scholar]
- 21.Gargari M, Comuzzi L, Bazzato MF, Sivolella S, di Fiore A, Ceruso FM. Treatment of peri-implantitis: Description of a technique of surgical 2 detoxification of the implant. A prospective clinical case series with 3-year follow-up. ORAL and Implantology. 2015;8(1):1–11. [Google Scholar]
- 22.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res. 2007;18(5):581–4. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 23.Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent. 2008;100:422–43. doi: 10.1016/S0022-3913(08)60259-0. [DOI] [PubMed] [Google Scholar]
- 24.Gargari M, Ottria L, Morelli V, Benli M, Ceruso FM. Conservative zirconia-ceramic bridge in front teeth. Case report. ORAL and Implantology. 2015;7(4):93–98. [Google Scholar]
- 25.Meleo D, Baggi L, Di Girolamo M, Di Carlo F, Pecci R, Bedini R. Fixture-abutment connection surface and micro-gap measurements by 3D micro-tomographic technique analysis. Ann Ist Super Sanità. 2012;48(1):53–8. doi: 10.4415/ANN_12_01_09. [DOI] [PubMed] [Google Scholar]
- 26.Ottria L, Zavattini A, Ceruso FM, Gargari M. Maxillofacial prosthesis (P.M.F): In a case of oral-nasal communication post-surgery and post-radiotherapy. ORAL and Implantology. 2014;7(2):46–50. [PMC free article] [PubMed] [Google Scholar]
- 27.Baggi L, Di Girolamo M, Mirisola C, Calcaterra R. Microbiological evaluation of bacterial and mycotic seal in implant systems with different implant-abutment interfaces and closing torque values. Implant Dent. 2013;22(4):344–50. doi: 10.1097/ID.0b013e3182943062. [DOI] [PubMed] [Google Scholar]
- 28.http://www.sympla-gtb.it/un-nuovo-progetto-in-implantoprotesi.
- 29.Pozzi A, Tallarico M, Moy PK. Three-year post-loading results of a randomised, controlled, split-mouth trial comparing implants with different prosthetic interfaces and design in partially posterior edentulous mandibles. Eur J Oral Implantol. 2014;7(1):47–61. [PubMed] [Google Scholar]
- 30.Guerra F, Wagner W, Wiltfang J, et al. Platform switch versus platform match in the posterior mandible – 1-year results of a multicentre randomized clinical trial. J Clin Periodontol. 2014;41(5):521–9. doi: 10.1111/jcpe.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Enkling N, Jöhren P, Katsoulis J, et al. Influence of platform switching on bone-level alterations: a three-year randomized clinical trial. J Dent Res. 2013;92(12 Suppl):139S–45S. doi: 10.1177/0022034513504953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Telleman G, Meijer HJ, Vissink A, Raghoebar GM. Short implants with a nanometer-sized CaP surface provided with either a platform-switched or platform-matched abutment connection in the posterior region: a randomized clinical trial. Clin Oral Implants Res. 2013;24(12):1316–24. doi: 10.1111/clr.12000. [DOI] [PubMed] [Google Scholar]
- 33.Pozzi A, Agliardi E, Tallarico M, Barlattani A. Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: randomized, controlled, split-mouth clinical trial. Clin Implant Dent Relat Res. 2014;16(1):96–106. doi: 10.1111/j.1708-8208.2012.00465.x. [DOI] [PubMed] [Google Scholar]
- 34.Telleman G, Raghoebar GM, Vissink A, Meijer HJ. Impact of platform switching on peri-implant bone remodeling around short implants in the posterior region, 1-year results from a split-mouth clinical trial. Clin Implant Dent Relat Res. 2014;16(1):70–80. doi: 10.1111/j.1708-8208.2012.00461.x. [DOI] [PubMed] [Google Scholar]
- 35.Telleman G, Raghoebar GM, Vissink A, Meijer HJ. Impact of platform switching on inter-proximal bone levels around short implants in the posterior region; 1-year results from a randomized clinical trial. J Clin Periodontol. 2012;39(7):688–97. doi: 10.1111/j.1600-051X.2012.01887.x. [DOI] [PubMed] [Google Scholar]
- 36.Canullo L, Iannello G, Götz W. The influence of individual bone patterns on peri-implant bone loss: preliminary report from a 3-year randomized clinical and histologic trial in patients treated with implants restored with matching-diameter abutments or the platform-switching concept. Int J Oral Maxillofac Implants. 2011;26(3):618–30. [PubMed] [Google Scholar]
- 37.Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: a randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2011;26(1):169–78. [PubMed] [Google Scholar]
- 38.Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S. Effect of platform switching on peri-implant bone levels: a randomized clinical trial. Clin Oral Implants Res. 2011;22(10):1185–92. doi: 10.1111/j.1600-0501.2010.02090.x. [DOI] [PubMed] [Google Scholar]
- 39.Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res. 2010;21(1):115–21. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 40.Crespi R, Capparè P, Gherlone E. Radiographic evaluation of marginal bone levels around platform-switched and non-platform-switched implants used in an immediate loading protocol. Int J Oral Maxillofac Implants. 2009;24(5):920–6. [PubMed] [Google Scholar]
- 41.Canullo L, Goglia G, Iurlaro G, Iannello G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: a preliminary report. Int J Prosthodont. 2009;22(3):277–82. [PubMed] [Google Scholar]
- 42.Prosper L, Redaelli S, Pasi M, Zarone F, Radaelli G, Gherlone EF. A randomized prospective multicenter trial evaluating the platform-switching technique for the prevention of postrestorative crestal bone loss. Int J Oral Maxillofac Implants. 2009;24(2):299–308. [PubMed] [Google Scholar]
- 43.Rocha S, Wagner W, Wiltfang J, et al. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J Clin Periodontol. 2016;43(4):374–82. doi: 10.1111/jcpe.12522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clementini M, Ottria L, Pandolfi C, Bollero P. A Novel Technique to Close Large Perforation of Sinus Membrane. ORAL and Implantology. 2013;6(1):11–14. [PMC free article] [PubMed] [Google Scholar]
- 45.Baggi L, Di Girolamo M, Vairo G, Sannino G. Comparative evaluation of osseointegrated dental implants based on platform-switching concept: influence of diameter, length, thread shape, and in-bone positioning depth on stress-based performance. Comput Math Methods Med. 2013;2013:250929. doi: 10.1155/2013/250929. Epub 2013 Jun 19. Erratum in: Comput Math Methods Med. 2014;2014:467358. Baggi Luigi [added]; Di Girolamo Michele [added] [DOI] [PMC free article] [PubMed] [Google Scholar]