Abstract
Objective
The purpose of this study was to understand the impact of living with Klinefelter syndrome (XXY) as an adolescent or an adult and to examine the factors that contribute to adaptation.
Methods
Individuals (n = 310) aged 14–75 years with self-reported XXY were recruited from online support networks to complete a self-administered survey. Perceived consequences, perceived severity, perceived stigma, and coping were measured and evaluated as correlates of adaptation.
Results
The use of problem-focused coping strategies was positively correlated with adaptation (p < 0.01) and age was negatively correlated with adaptation (p < 0.05).
Conclusion
The majority of participants reported significant negative consequences of XXY, including infertility, psychological co-morbidities and differences in appearance. How participants coped with their negative appraisals was the greatest predictor of adaptation.
Practice implications
Interventions designed to help individuals reframe negative appraisals, to increase perceived manageability of the challenges of living with XXY, and to facilitate effective coping may improve adaptation among individuals with XXY.
Keywords: Klinefelter syndrome; 47,XXY; Adaptation; Coping; Illness perceptions; Sex chromosome aneuploidy
1. Introduction
Klinefelter syndrome (XXY), or 47,XXY, is a common genetic condition caused by the presence of an extra X chromosome in males. It is estimated to occur in one in 650 males, though population-based studies in the UK and Denmark have suggested that 65–75% of individuals with XXY are undiagnosed [1,2]. While the physical and cognitive phenotype associated with XXY is highly variable, common features include tall stature, language-based learning disabilities, disorders of executive function, hypogonadism, gynecomastia, and fertility problems [3]. Approximately 15% of azoospermic and oligozoospermic men who underwent infertility workup were found to have XXY [4].
Previous research has focused on the medical and cognitive implications of XXY [5–9], with little attention given to the psychosocial implications of XXY. Those studies that have aimed to understand the personal impact of XXY have raised concerns that individuals with XXY may experience difficulty adapting to their diagnosis as a result of lowered self-esteem [10,11], increased incidence of psychiatric conditions and behavioral problems [10], and difficulties forming social relationships [12]. A recent study of 87 men with XXY in Australia found that quality of life outcomes (well-being, body image, self-esteem, mental and general health) among study participants were significantly poorer compared to general male population normative data. Phenotypic severity, employment status, and social support were the greatest predictors of psychosocial outcomes [13]. While these previous studies identified a number of factors that may influence adaptation to XXY, our understanding of these factors and whether they might be amenable to intervention is limited by small sample sizes that do not provide statistical power to detect effects of key variables on psychosocial outcomes. A better understanding of these factors is imperative to improving the psychological well-being and quality of life of boys and men living with XXY.
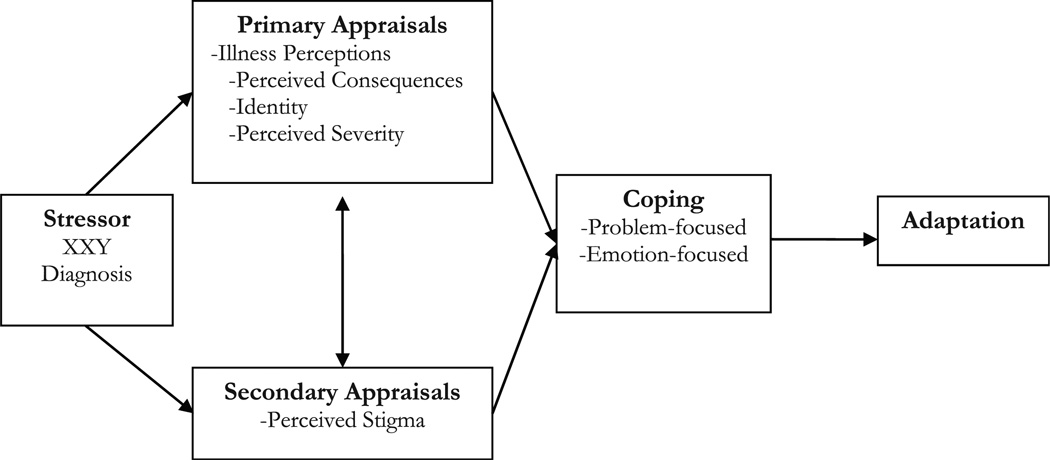
Lazarus and Folkman’s Transactional Model of Stress and Coping (TMSC) [14] provides a theoretical framework for understanding how an individual with XXY adapts to his diagnosis. According to the TMSC (Fig. 1), a person makes meaning of a stressor (XXY diagnosis) by evaluating the significance of the diagnosis on his life (primary appraisal) and deciding what he can do to minimize the negative impact of the diagnosis (secondary appraisal). In this study, perceived consequences and perceived severity were included as primary appraisals. Perceived stigma was included as a secondary appraisal as participants not only assess the significance of perceived stigma, but also their perceived resources to cope with stigma. These appraisals direct coping strategies, and coping is the process through which adaptation occurs.
Fig. 1.
Stress and coping model of adaptation to Klinefelter syndrome, adapted from Lazarus and Folkman’s transactional model of stress and coping [13].
Adaptation is defined as the dynamic, multidimensional process of successfully coming to terms with the implications of a health condition or a health threat and its observable outcomes [15]. Indicators that an individual is well adapted include coping efficacy, restored self-esteem, spiritual and psychological well-being, and social integration [15]. While these indicators may be assessed at a single point in time, they represent the dynamic adaptation process that gives insight into how effectively a person is managing the stress of a health condition or health threat [16].
The purpose of this study was to understand the impact of living with XXY as an adolescent or an adult and to understand the factors that contribute to adaptation using a validated multidimensional measure of adaptation and a sufficiently powered sample size.
2. Methods
2.1. Study participants and procedures
This study’s methods have been described previously in our publication that reported the prevalence and psychosocial correlates of clinically significant depressive symptoms among this cohort of individuals with Klinefelter syndrome [17]. Individuals 14 years or older with self-reported XXY were eligible to participate. Participants were recruited through XXY online support organizations in the United States and the United Kingdom, including Klinefelter Syndrome & Associates (KS&A), Klinefelter Syndrome Association (KSA), and Klinefelter Organisation (KO). These organizations advertised the study through newsletter mailings, website postings, and email distribution lists. Participants were also recruited in person at a KS&A national XXY conference and at a New York regional support group meeting.
Participation involved a one-time self-administered survey. Individuals could complete an electronic version of the survey through a secure Internet site, or they could contact the researcher for a paper copy of the survey. A website for individuals 18 years and older and a website for individuals under the age of 18 years were created. The latter website was password protected and required a parent or guardian to contact the researcher to provide permission for participation and to obtain the website password. Participation was anonymous and compensation was not provided.
This study was approved by the Institutional Review Board at the National Human Genome Research Institute, National Institutes of Health (Protocol # 09-HG-N142).
2.2. Study measures
2.2.1. Adaptation
Adaptation was measured using The Psychological Adaptation Scale (PAS) [16], a 20-item measure that assesses four constructs of adaptation: effective coping, self-esteem, spiritual/existential meaning and social integration. Participants were asked to insert each item into the statement, “Living with XXY has …”, and to rate each statement on a 5-point scale (1 = “not at all true” to 5 = “very much true). This scale has been shown to have good internal reliability (Cronbach’s alpha ≥ 0.90) and validity across studies [16,18,19]. Scores were summed and a mean score ranging from 1 to 5 was calculated, with higher scores indicating greater levels of adaptation.
2.2.2. Illness perceptions
The Illness Perception Questionnaire’s (IPQ) consequences sub-scale [20] was used to assess the extent to which an individual perceived his XXY diagnosis impacts his life. The sub-scale includes seven items rated on a 5-point scale (1 = “strongly disagree” to 5 = “strongly agree”), and has been shown to have good internal reliability (Cronbach’s alpha = 0.82) [20]. Results were summed and a mean score ranging from 1 to 5 was calculated. Higher scores indicated an individual perceived his condition to have significant, negative consequences on his life.
Two additional questions were included to assess perceived severity. Participants were asked to rate how severe they perceived their XXY to be, as well as how severe they perceived their XXY to be in comparison to others with XXY using a 5-point scale that ranged from “not at all severe” (1) to “very severe” (5).
2.2.3. Perceived stigma
Perceived stigma was measured using the Perceived Social Stimga Scale (PSSS) [21]. The PSSS is a 22-item measure that consists of fourteen negative attributes, such as “unhappy,” “pitiful,” and “worthless,” and eight positive attributes, such as “friendly,” “confident,” and “intelligent.” Participants were instructed to insert each attribute into the statement, “As a person with XXY others see me as …” and to rate the statement on a 4-point scale (1 = “not at all true” to 4 = “very much true”). This scale has been shown to have good internal reliability (Cronbach’s alpha = 0.91) [21]. Summed scores could range from 22 to 88. Higher scores indicated greater perceptions of stigmatization.
2.2.4. Coping
Coping was measured using the Ways of Coping Checklist-Revised (WCC-R) [22]. The WCC-R is a 42-item measure that assesses five categories of coping: problem-focused, social support seeking, self-blame, wishful thinking, and avoidance coping. Participants were asked to think about a recent stressful event related to their XXY and to estimate the frequency with which they used each coping strategy using a 4-point scale (0 = “never use” to 3 = “regularly use”). This scale has been shown to have good reliability (Cronbach’s alpha = 0.74–0.88 for each sub-scale) and construct validity [22]. While participants were not asked to report the recent stressful event they were considering, an open-ended question was included to capture the most stressful aspects of living with XXY.
Items for each sub-scale were summed and a mean score was calculated. The relative proportion of problem-focused coping used by participants was calculated by dividing the mean problem-focused coping score by the sum of all five mean scores. The relative proportion of emotion-focused coping strategies used by participants was calculated by adding the mean scores for self-blame, wishful thinking and avoidance sub-scales and dividing by the sum of all five mean scores. Previous research has suggested that relative coping scores are better suited for empirically evaluating relationships between coping and psychosocial outcomes and are especially useful in studying the TMSC [23]. Grouping the emotion-focused sub-scales into one relative score was first described by Vitaliano et al. in 1990 [24], and has since been used in several studies [25,26].
2.2.5. Depressive symptoms
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D) [27]. The CES-D is a widely used measure that was initially designed to screen for depressive symptoms in the general population. It has since been used extensively to measure depressive symptoms among individuals with a variety of medical conditions [28–30]. Reliability of the scale (Cronbach’s alpha = 0.85–0.90) and construct validity have been established [27]. The scale includes 20-items to assess the six major dimensions of depression: depressed mood, feelings of guilt and worthlessness, feelings of helplessness and hopelessness, psychomotor retardation, loss of appetite, and sleep disturbance. Participants were asked to indicate how often they had experienced each of the symptoms in the past week, using a 4-point scale (0 = “rarely or none of the time, <1 day,” 1 = “a little of the time, 1–2 days,” 2 = “occasionally or some of the time, 3–4 days,” 3 = “most or all of the time, 5–7 days”). Summed scores could range from 0 to 60, with higher scores more likely to be associated with depression. Although the CES-D is not a clinical diagnostic tool, a cut-off score of 16 has been shown to reliably distinguish between clinically depressed and non-depressed individuals [27,31,32].
2.2.6. Features of XXY
Participants were asked if they have common features of XXY, such as infertility, learning difficulties, and small testes, and to rate how challenging each feature is using a scale from 1 (least challenging) to 7 (most challenging). Participants were also asked to rate the importance of having children in the next 10 years using a 5-point sale (1 = “very unimportant” to 5 = “very important”).
2.2.7. Demographic information
Participants provided information about their age, age at diagnosis, time elapsed since learning of the diagnosis, race/ethnicity, marital status, level of education, number of children, and relationship to children. Time elapsed since learning of diagnosis accounted for individuals who were diagnosed at a certain age but were not informed of their diagnosis until later.
2.3. Analysis strategy
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 16.0.2 (SPSS Inc., Chicago, IL). Bivariate associations among all key variables were identified by Pearson correlations. A multivariate linear regression analysis was used to assess associations between the outcome, adaptation, and five key variables (perceived consequences, perceived severity, perceived stigma, emotion-focused coping, and problem-focused coping), controlling for potential confounders (depressive symptoms, age, race, education level, marital status, whether a participant had children, importance of having children in the future, and time elapsed since learning of the diagnosis). Demographic variables were dichotomized as follows: race (white/non-white), marital status (partnered/non-partnered), education (college graduate or more/some college or technical school or less). To increase precision on the key variables, while retaining true confounders as control covariates, a backwards elimination selection process was used. Potential confounders with p-values > 0.20 were dropped from an initial model that included all variables and potential confounders [33,34]. Statistical significance of associations between key variables and adaptation was evaluated using the p < 0.05 criterion.
3. Results
3.1. Descriptive statistics and bivariate relationships
A sample size calculation indicated that 243 participants were needed to have 80% power to detect the effect of a key independent variable explaining a small-to-medium effect size [35] of at least 3% of the total variance in adaptation. We surpassed this threshold with a total of 310 participants, although not all analyses included 310 responses due to missing data. The mean age of participants was 40.7 years (±14) and ranged from 14 to 75 years. Most participants were white, non-Hispanic (92.2%) and did not have children (76.4%). Nearly half of participants were diagnosed in adulthood (48%) and the average time elapsed since learning of the diagnosis was 15 years (±11.7, range 0–46). Half of participants were married or partnered (49.6%) and over one-third (37.5%) had a college or graduate degree.
The means, standard deviations, ranges, and internal reliability values for each measure are presented in Table 1. A majority of participants (76.4%) scored >3.0 on the IPQ perceived consequences sub-scale, endorsing the belief that XXY has significant negative consequences on their life. Most participants rated their XXY as “a little severe” (23.9%), “somewhat severe” (30.0%), or “severe” (25.6%). A minority considered their XXY to be either “not at all severe” (9.4%) or “very severe” (11.1%). When participants compared their severity to the severity of others living with XXY, a leftward shift was observed, indicating that many participants felt their XXY was less severe than that of others. Compared to others, most participants viewed their XXY as “not at all severe” (24.9%), “a little severe” (25.6%), or “somewhat severe” (32.9%).
Table 1.
Means, standard deviations, ranges, and reliability values for study measures.
| Variable | n (missing values) | Mean (SD) | Measured range (possible range) | Cronbach’s alpha |
|---|---|---|---|---|
| Perceived consequences | 305 (5) | 3.60 (0.76) | 1.43–5.0 (1.0–5.0) | 0.79 |
| Perceived severity | 286 (24) | 2.75 (1.04) | 1.0–5.0 (1.0–5.0) | 0.80 |
| Perceived stigma | 279 (31) | 46.23 (12.14) | 25–83 (22–88) | 0.89 |
| Coping | ||||
| Problem-focused | 259 (51) | 1.88 (0.62) | 0–3.0 (0–3.0) | 0.89 |
| Social support seeking | 256 (54) | 1.81 (0.74) | 0–3.0 (0–3.0) | 0.80 |
| Wishful thinking | 258 (52) | 2.06 (0.84) | 0–3.0 (0–3.0) | 0.90 |
| Self-blame | 257 (53) | 1.49 (1.09) | 0–3.0 (0–3.0) | 0.88 |
| Avoidance | 257 (53) | 1.63 (0.70) | 0–3.0 (0–3.0) | 0.82 |
| Depressive symptoms | 247 (63) | 24.58 (14.74) | 0–59 (0–60) | 0.93 |
| Adaptation | 251 (59) | 3.33 (0.99) | 1.0–5.0 (1.0–5.0) | 0.96 |
A majority of respondents scored ≤2.5 on the PSSS, indicating that most participants did not perceive stigmatization as a result of their diagnosis. As assessed by the CES-D, 68.8% of the study population reported a clinically significant level of depressive symptoms. Despite the high levels of perceived negative consequences and the prevalence of depressive symptoms, 64.1% of respondents scored >3.0 on the PAS, indicating that approximately two-thirds of participants reported high levels of adaptation at the time of study participation.
Emotion-focused coping strategies represented 56% of the total coping strategies, whereas 22% of respondents reported using problem-focused coping strategies. The remaining 22% reported using elements of both emotion-focused and problem-focused coping. The emotion-focused relative score and problem-focused relative score were highly and inversely correlated (r = −0.83, p < 0.01), suggesting that the two strategies are used distinctly. Bivariate analyses showed that problem-focused coping was positively correlated with adaptation (r = 0.49, p < 0.01). Emotion-focused coping (r = −0.44, p < 0.01), perceived stigma (r = −0.36, p < 0.01), perceived severity (r = −0.15, p < 0.05), and perceived consequences (r = −0.30, p < 0.01) were negatively correlated with adaptation.
3.2. Multivariate linear regression analysis
Table 2 summarizes the results of the multivariate linear regression analysis, which demonstrates that problem-focused coping was positively correlated with adaptation and age was negatively correlated with adaptation. Race was included in the model to control for a potential confounding effect. These variables accounted for 27.5% of the variance in adaptation. Perceived consequences, perceived severity, perceived stigma, and emotion-focused coping were tested and found to be non-significant (p > 0.05).
Table 2.
Multivariate linear regression model: correlates of adaptation.
| b (SE) | β | p-value | |
|---|---|---|---|
| Problem-focused coping | 3.58 (1.07) | 0.34 | <0.01 |
| Age | −0.01 (0.01) | −0.13 | 0.03 |
| Race | 0.36 (0.21) | 0.10 | 0.09 |
4. Discussion and conclusion
4.1. Discussion
This study contributes to the understanding of the psychosocial impact of living with XXY as an adolescent or an adult and is the first study to have a sample size sufficient to detect statistically significant correlations among key psychosocial variables and adaptation. While other studies have addressed the topic of adaptation to XXY [10,36,37], this is the first study to assess adaptation with a validated measure of adaptation, rather than with related but distinct variables, such as global functioning, well-being, or affect [16,38]. No studies have assessed psychosocial predictors of adaptation.
Despite the challenges and perceived negative consequences of living with XXY, the adolescents and adults in this study reported high levels of adaptation. The participants in this study had a higher mean adaptation score than adults living with bipolar disorder [39] and adults living with another chronic genetic condition, neurofibromatosis type 1 (NF1) [19], despite the fact that this study’s participants perceived their condition to have more negative consequences on their life compared to the adults with NF1 [19]. The multivariate analysis indicated that the use of problem-focused coping strategies was the greatest predictor of adaptation.
Different situations call for different coping strategies. The choice of coping strategies is influenced by a person’s appraisal of a specific situation as controllable or changeable versus uncontrollable or unchangeable, and a person’s ability to choose a coping strategy that is best aligned with the nature of the situation. Coping effectively in a changeable situation involves greater use of problem-focused coping strategies whereas coping effectively in an unchangeable situation involves greater use of emotion-focused coping strategies [14].
In this study, over half of participants used predominantly emotion-focused strategies, whereas approximately one-fourth of participants predominantly used problem-focused strategies. Another one-fourth of participants used elements of both emotion-focused and problem-focused coping. The adaptation scores in this study suggest that participants are effectively choosing appropriate coping strategies to manage challenges they face. Theoretically, this suggests that the negative consequences of XXY that participants reported were ones that participants appraised as uncontrollable or unchangeable. As such, participants employed coping strategies aimed at managing the negative emotions associated with their condition. The minority of participants who used more problem-focused coping strategies relative to emotion-focused coping strategies may have perceived specific consequences to be more manageable and within their control. Responses to open-ended questions aimed at understanding the greatest challenges of living with XXY indicated that infertility and psychological co-morbidities, such as depression and anxiety, were the two greatest challenges participants faced, followed by differences in one’s appearance and learning disabilities. Infertility, for example, represents a threat to one’s virility, loss of the potential to have a biological child, and challenge to one’s manhood. While advances in assistive reproductive technology offer options for fatherhood to men with XXY [40], emotion-focused coping strategies may be best suited to managing the uncontrollable nature of infertility.
The significant negative correlation between age and adaptation was unexpected, although age differences in stress and coping have been reported [41]. While our cross-sectional study design allows assessment of adaptation only at a fixed point in time, it is possible that some of the older participants had experienced more challenges over their lives and/or were currently facing more obstacles to their adaptation than younger participants. As individuals with XXY age, they are at increased risk for a number of co-morbidities associated with XXY, such as obesity, cardiovascular disease, osteoporosis, diabetes mellitus, and autoimmune disease [42], leading to accumulation of additional stressors with age. Another consideration is the effect of reduced fertility as individuals with XXY enter the life stage in which starting a family is often considered. Threats to a person’s life goals are known to increase stress and present challenges to adaptation [43]. Our results suggest that a general assumption that adults with XXY adapt as they age is not supported. Clinicians should be alert to the impact of adult-onset manifestations while additional studies are needed to replicate our findings.
Depressive symptoms were evaluated as a potential confounder of adaptation in light of previous research that has found the two constructs to be highly correlated [38]. Depressive symptoms were strikingly prevalent among study participants and have been previously published [17]. Although depressive symptoms dropped out of the final adaptation multivariate regression model, its initial assessment as a potential confounder revealed that depressive symptoms were significantly negatively associated with adaptation (b = −0.025, p < 0.01) and accounted for 13.9% of the total variance in adaptation.
This supports our knowledge that the two are related. However, depression and adaptation are distinct constructs, and depressive symptoms alone were insufficient to significantly affect adaptation.
A study of 482 adults with NF1 also found that depressive symptoms did not predict adaptation [19]. However, depressive symptoms were significantly negatively associated with quality of life and accounted for 25% of the total variance in quality of life. The adaptation process involves fundamental changes in one’s psychological and spiritual well-being, acceptance of oneself as a person living with a condition, a new or restored sense of self-esteem, renewed life values, and successful navigation of obstacles that have presented themselves throughout the process [15,44]. It is not inconsistent that depressive symptoms, which may be more transitory, do not interfere with the fundamental changes that occur throughout the larger process of adaptation.
Our study is the first to use a validated measure to assess perceived stigma among individuals with XXY and one of few studies to assess the relationship between perceived stigma and adaptation. The majority of participants did not perceive themselves to be stigmatized as a result of their XXY and perceived stigma was not found to be correlated with adaptation. This is inconsistent with a number of other studies that have found significant negative correlations between perceived stigma and adaptation [21,45]. It is possible that participants in our study are coping effectively with stigma. The lack of correlation between perceived severity and adaptation is consistent with the broader adaptation literature, which indicates that the severity of the condition being studied does not predict adaptation [15].
4.1.1. Limitations
The cross-sectional nature of this study allows us to measure adaptation and other key variables at a single point in time. Conclusions can be drawn regarding correlations among variables, but not to temporal relationships and causal pathways. The results of this study are not generalizable to the entire population of adolescents and adults with XXY. Participants were recruited through online support groups. We do not know the number of potential participants study advertisements reached, so we are unable to calculate a response rate. It is possible that individuals who participate in support groups differ from those who do not. Self-selection introduces a potential bias into our findings, but it is unknown whether those who responded were interested because they were in need of additional support or because they were doing well enough and were interested in study participation. The study population was overwhelmingly white, non-Hispanic. However, the external validity of our findings is increased by our large sample size, range of ages, and international participation.
4.2. Conclusions
This study explored the relationship among appraisals (perceived consequences, perceived severity, perceived stigma), coping, and adaptation and found that despite report of significant negative consequences of XXY, individuals seem to cope effectively and the majority report relatively positive adaption to living with XXY. Use of problem-focused coping strategies was the strongest predictor of adaptation. It is possible that participants using problem-focused coping strategies may perceive their XXY-related challenges to be manageable and controllable. Future studies evaluating perceived control and self-efficacy may offer additional insight into this study’s findings.
4.3. Practice implications
The results of this study suggest that interventions aimed at understanding and reframing cognitive appraisals to increase perceived manageability of the consequences associated with XXY may promote problem-focused coping and improve adaptation among adolescents and adults with XXY. Given the negative association between age and adaptation and our expectation that appraisals and adaptation vary with time, health care providers should routinely assess appraisals and coping strategies in their clinical encounters, even among patients with whom they have longstanding relationships. As people age, they may face new challenges associated with XXY.
Acknowledgments
This research was funded by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The funder had no role in the study design, writing of the paper and the decision to submit the paper. We thank the adolescents and adults who participated in this study and the XXY support groups for facilitating recruitment.
Footnotes
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Bojesen A, Juul S, Gravholt CH. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab. 2003;88:622–626. doi: 10.1210/jc.2002-021491. [DOI] [PubMed] [Google Scholar]
- 2.Abramsky L, Chapple J. 47,XXY and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counseling. Prenat Diagn. 1997;17:363–368. doi: 10.1002/(sici)1097-0223(199704)17:4<363::aid-pd79>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 3.Groth KA, Skakkebæk A, Høst C, Gravholt CH, Bojesen A. Klinefelter syndrome – a clinical update. J Clin Endocrinol Metab. 2013;98:20–30. doi: 10.1210/jc.2012-2382. [DOI] [PubMed] [Google Scholar]
- 4.Ferlin A, Arredi B, Foresta C. Genetic causes of male infertility. Reprod Toxicol. 2006;22:133–141. doi: 10.1016/j.reprotox.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Pasquali D, Arcopinto M, Renzullo A, Rotondi M, Accardo G, Salzano A, et al. Cardiovascular abnormalities in Klinefelter syndrome. Int J Cardiol. 2013 doi: 10.1016/j.ijcard.2012.09.215. [DOI] [PubMed] [Google Scholar]
- 6.Leggett V, Jacobs P, Nation K, Scerif G, Bishop DVM. Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Dev Med Child Neurol. 2010;52:119–129. doi: 10.1111/j.1469-8749.2009.03545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bojesen A, Gravholt CH. Morbidity and mortality in Klinefelter syndrome (47,XXY) Acta Paediatr. 2011;100:807–813. doi: 10.1111/j.1651-2227.2011.02274.x. [DOI] [PubMed] [Google Scholar]
- 8.Wosnitzer MS, Paduch DA. Endocrinological issues and hormonal manipulation in children and men with Klinefelter syndrome. Am J Med Genet C Semin Med Genet. 2013;163:16–26. doi: 10.1002/ajmg.c.31350. [DOI] [PubMed] [Google Scholar]
- 9.Verri A, Cremante A, Clerici F, Destefani V, Radicioni A. Klinefelter’s syndrome and psychoneurologic function. Mol Hum Reprod. 2010;16:425–433. doi: 10.1093/molehr/gaq018. [DOI] [PubMed] [Google Scholar]
- 10.Bender BG, Harmon RJ, Linden MG, Robinson A. Psychosocial adaptation of 39 adolescents with sex chromosome abnormalities. Pediatrics. 1995;96:302–308. [PubMed] [Google Scholar]
- 11.Ratcliffe S, Bancroft J, Axworthy D, McLaren W. Klinefelter’s syndrome in adolescence. Arch Dis Child. 1982;57:6–12. [PMC free article] [PubMed] [Google Scholar]
- 12.Ratcliffe S, Paul N. Prospective studies on children with sex chromosome aneuploidy. Birth Defects Orig Artic Ser. 1986;22:1–328. [PubMed] [Google Scholar]
- 13.Herlihy AS, McLachlan RI, Gillam L, Cock ML, Collins V, Halliday JL. The psychosocial impact of Klinefelter syndrome and factors influencing quality of life. Genet Med. 2011;13:632–642. doi: 10.1097/GIM.0b013e3182136d19. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 15.Biesecker BB, Erby L. Adaptation to living with a genetic condition or risk: a mini-review. Clin Genet. 2008;74:401–407. doi: 10.1111/j.1399-0004.2008.01088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biesecker B, Erby LH, Woolford S, Adcock JY, Cohen JS, Lamb A, Lewis KV, Truitt M, Turriff A, Reeve BB. Development and validation of the Psychological Adaptation Scale (PAS): use in six studies of adaptation to a health condition or risk. Patient Educ Couns. 2013;93:248–254. doi: 10.1016/j.pec.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turriff A, Levy HP, Biesecker B. Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genet Med. 2011;13:966–972. doi: 10.1097/GIM.0b013e3182227576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Educ Couns. 2012;87:233–238. doi: 10.1016/j.pec.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen J. Adaptation and quality of life among adults with neurofibromatosis type 1. Baltimore: Johns Hopkins University; 2009. [Google Scholar]
- 20.Weinman J, Petrie KJ, MossMorris R, Horne R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. 1996;11:431–445. [Google Scholar]
- 21.Rybarczyk B, Nyenhuis DL, Nicholas JJ, Cash SM, Kaiser J. Body image, perceived social stigma, and the prediction of psychosocial adjustment to leg amputation. Rehabil Psychol. 1995;40:95–110. [Google Scholar]
- 22.Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The ways of coping checklist – revision and psychometric properties. Multivar Behav Res. 1985;20:3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- 23.Vitaliano PP, Maiuro RD, Russo J, Becker J. Raw versus relative scores in the assessment of coping strategies. J Behav Med. 1987;10:1–18. doi: 10.1007/BF00845124. [DOI] [PubMed] [Google Scholar]
- 24.Vitaliano PP, DeWolfe DJ, Maiuro RD, Russo J, Katon W. Appraised changeability of a stressor as a modifier of the relationship between coping and depression: a test of the hypothesis of fit. J Pers Soc Psychol. 1990;59:582–592. doi: 10.1037//0022-3514.59.3.582. [DOI] [PubMed] [Google Scholar]
- 25.Zakowski SG, Hall MH, Klein LC, Baum A. Appraised control, coping, and stress in a community sample: a test of the goodness-of-fit hypothesis. Ann Behav Med. 2001;23:158–165. doi: 10.1207/S15324796ABM2303_3. [DOI] [PubMed] [Google Scholar]
- 26.Hooker K, Frazier LD, Monahan DJ. Personality and coping among caregivers of spouses with dementia. Gerontologist. 1994;34:386–392. doi: 10.1093/geront/34.3.386. [DOI] [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 28.Huang C-Y, Hsu M-C. Social support as a moderator between depressive symptoms and quality of life outcomes of breast cancer survivors. Eur J Oncol Nurs. 2013 doi: 10.1016/j.ejon.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 29.Kato N, Kinugawa K, Shiga T, Hatano M, Takeda N, Imai Y, et al. Depressive symptoms are common and associated with adverse clinical outcomes in heart failure with reduced and preserved ejection fraction. J Cardiol. 2012;60:23–30. doi: 10.1016/j.jjcc.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Darnall BD, Ephraim P, Wegener ST, Dillingham T, Pezzin L, Rossbach P, et al. Depressive symptoms and mental health service utilization among persons with limb loss: results of a national survey. Arch Phys Med Rehabil. 2005;86:650–658. doi: 10.1016/j.apmr.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 31.Craig TJ, Vannatta PA. Current medication use and symptoms of depression in a general population. Am J Psychiatry. 1978;135:1036–1039. doi: 10.1176/ajp.135.9.1036. [DOI] [PubMed] [Google Scholar]
- 32.Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH. Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. Am J Psychiatry. 2002;159:1862–1868. doi: 10.1176/appi.ajp.159.11.1862. [DOI] [PubMed] [Google Scholar]
- 33.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 34.Budtz-Jorgensen E, Keiding N, Grandjean P, Weihe P. Confounder selection in environmental epidemiology: assessment of health effects of prenatal mercury exposure. Ann Epidemiol. 2007;17:27–35. doi: 10.1016/j.annepidem.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Routledge Academic; 1988. [Google Scholar]
- 36.Bender BG, Harmon RJ, Linden MG, Bucher-Bartelson B, Robinson A. Psychosocial competence of unselected young adults with sex chromosome abnormalities. Am J Med Genet. 1999;88:200–206. doi: 10.1002/(sici)1096-8628(19990416)88:2<200::aid-ajmg18>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 37.Bender BG, Linden MG, Harmon RJ. Life adaptation in 35 adults with sex chromosome abnormalities. Genet Med. 2001;3:187–191. doi: 10.1097/00125817-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Stanton AL, Collins CA, Sworowski LA. Adjustment to chronic illness: theory and research. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Lawrence Erlbaum Associates; 2001. pp. 387–403. [Google Scholar]
- 39.Peay H, Rosenstein D, Biesecker BB. Adaptation to bipolar disorder and perceived risk to children: a survey of parents with bipolar disorder. BMC Psychiatry. 2013;13:327–334. doi: 10.1186/1471-244X-13-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehta A, Paduch DA, Schlegel PN. Successful testicular sperm retrieval in adolescents with Klinefelter syndrome treated with at least 1 year of topical testosterone and aromatase inhibitor. Fertil Steril. 2013;100:e27. doi: 10.1016/j.fertnstert.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 41.Folkman S, Lazarus RS, Pimley S, Novacek J. Age differences in stress and coping processes. Psychol Aging. 1987;2:171–184. doi: 10.1037//0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- 42.Swerdlow AJ, Higgins CD, Schoemaker MJ, Wright AF, Jacobs PA on behalf of the United Kingdom Clinical Cytogenetics Group. Mortality in patients with Klinefelter syndrome in Britain: a cohort study. J Clin Endocrinol Metab. 2005;90:6516–6522. doi: 10.1210/jc.2005-1077. [DOI] [PubMed] [Google Scholar]
- 43.Maes S, Leventhal H, de Ridder DTD. Handbook of coping: theory, research, applications. Oxford, England: John Wiley & Sons; 1996. Coping with chronic diseases; pp. 221–251. [Google Scholar]
- 44.Livneh H, Martz E. Psychosocial adaptation to spinal cord injury: a dimensional perspective. Psychol Rep. 2005;97:577–586. doi: 10.2466/pr0.97.2.577-586. [DOI] [PubMed] [Google Scholar]
- 45.Perlick DA, Rosenheck RA, Clarkin JF, Sirey JA, Salahi J, Struening EL, et al. Stigma as a barrier to recovery: adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatr Serv. 2001;52:1627–1632. doi: 10.1176/appi.ps.52.12.1627. [DOI] [PubMed] [Google Scholar]