Abstract
Ductal carcinoma in situ (DCIS) refers to breast epithelial cells that have become “cancerous” but still reside in their normal place in the ducts and lobules. In this setting, cancerous means that there is an abnormal increase in the growth of the epithelial cells, which accumulate within and greatly expand the ducts and lobules. DCIS is a nonlethal type of cancer because it stays in its normal place. However, DCIS is very important because it is the immediate precursor of invasive breast cancers, which are potentially lethal. This article provides a general overview of DCIS, including historical perspective, methods of classification, current perspective, and future goals.
The normal female human breast contains tens of thousands of lobules, which are small grape-like clusters of glands lined by epithelial cells specialized to produce milk (1). The lobules are interconnected by small ducts, which join to form larger ducts that eventually exit through the nipple, transmitting milk to nourish our young (Figure 1). Ductal carcinoma in situ (DCIS) refers to breast epithelial cells that have become “cancerous” but still reside in their normal place in the ducts and lobules. In this setting, cancerous means that there is an abnormal increase in the growth of the epithelial cells, which accumulate within and greatly expand the ducts and lobules (Figure 1). DCIS is a nonlethal type of cancer because it stays in its normal place. However, DCIS is very important because it is the immediate precursor of invasive breast cancers (IBCs), which are potentially lethal (2–4).
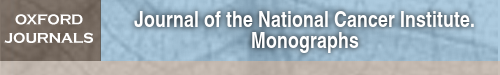
Figure 1.
The female human breast is composed of thousands of grape-like clusters of small glands lined by epithelial cells that produce milk, referred to as terminal duct lobular units (TDLUs). The milk is propagated outward through a series of interconnecting and increasingly large ducts that exit the nipple. Ductal carcinoma in situ (DCIS) refers to breast epithelial cells that have become “cancerous” but still reside in their normal place. In this setting, cancerous means that there is an abnormal increase in the growth of the epithelial cells, which accumulate within and greatly expand the glands and ducts.
The recognition of DCIS as a specific disease distinct from IBC occurred gradually, primarily during the first half of the 20th century (3,5–10). It was rare during that time, accounting for only 1%–2% of newly diagnosed breast cancers, and was usually detected when it formed a large palpable mass (11). Mastectomy became the standard therapy, and it essentially cured patients (11).
Three developments occurred during the latter half of the 20th century, which dramatically changed our perception, awareness, and treatment of DCIS. First was the general acceptance by the scientific and medical communities that DCIS was indeed the immediate precursor of IBC (4,12–17) and, therefore, required effective therapy—ideally something less disfiguring than mastectomy because it is nonlethal. Second was screening mammography, which enabled DCIS to be detected early, when it was small and before it had progressed to IBC. Mammography primarily identifies microscopic calcifications, which are commonly associated with DCIS, and is highly sensitive. Screening greatly increased the frequency of detection, and now DCIS accounts for 20%–30% of all newly diagnosed breast cancers in populations with easy access to this technology (11,18). Third was the adoption of effective therapies for DCIS that allowed patients to keep their breasts, including lumpectomy, postoperative radiation, and adjuvant endocrine therapy (11,19,20). These therapies were originally developed to treat IBC.
Since it was first recognized, clinical and scientific research on DCIS has increased at an accelerating pace, and there is a large body of literature on the subject today. Early achievements included the development of methods of classifying DCIS based on gross and histological features viewed under the microscope. These features included the architectural arrangement or growth pattern of cells, the size and shape of cells and their nuclei, estimates of growth rate based on counting dividing cells referred to as mitotic figures, and the amount of cell necrosis.
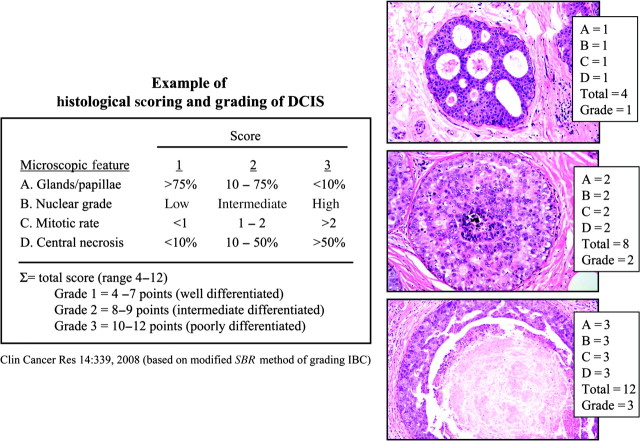
In the pre-mammography era, the most commonly encountered DCIS were composed of large, irregularly shaped, rapidly dividing cells growing as a solid mass within ducts, with abundant necrosis in the center. They usually formed a large palpable mass and were referred to as “comedo” DCIS because the necrotic cell debris grossly oozed from the ducts when the excised tumor was squeezed, resembling comedones (as in acne) (7). The other types of DCIS, which were encountered more rarely before mammography, were usually not palpable or visible grossly and were classified primarily on their predominant microscopic growth pattern, which included cribriform, solid, papillary, and micropapillary (Figure 2, B–E). In general, the cells in these tumors were also smaller, more normal appearing, and less necrotic than in comedo DCIS, so they were often referred to collectively as “non-comedo” DCIS (7). However, a large proportion of DCIS shows complex combinations of growth patterns and cellular features (Figure 2, F), and a shortcoming of this method of classification is its inability to convey intratumor diversity, which is almost certainly important clinically, although we are just beginning to understand how and why (15,16,21).
Figure 2.
A historical method of classifying ductal carcinoma in situ (DCIS) is based on their predominant microscopic growth pattern and includes comedo (A), cribriform (B), solid (C), micropapillary (D), and papillary (E) subtypes. However, a large proportion of DCIS shows complex mixtures of growth patterns (F), which is difficult to categorize.
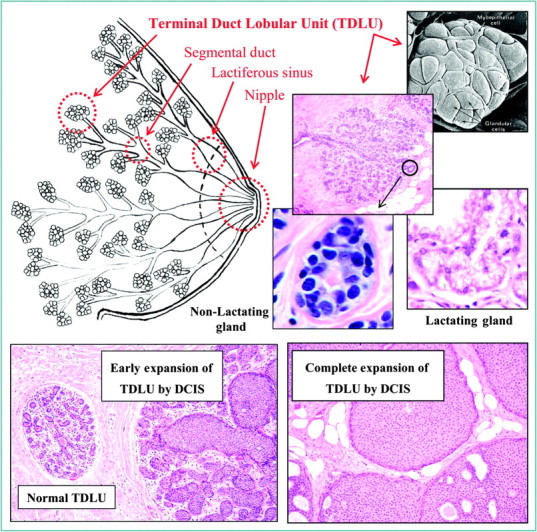
More recent methods of taxonomy and terminology attempt to convey the relative degree that tumor cells in DCIS resemble normal cells, referred to as differentiation, and how rapidly they are dividing. Numerical scoring and grading systems were developed to reflect differentiation and growth. There are several and the details vary somewhat, but most ultimately recognize three grades, corresponding to well (grade 1), moderately (grade 2), and poorly (grade 3) differentiated DCIS (Figure 3) (22,23). When applied to previous terminology, comedo DCIS are poorly differentiated, whereas the non-comedo types are variable, although the majority are well to moderately differentiated. Current methods of histological grading are also unable to convey information about diversity within individual cases of DCIS (Figure 2, F). Grading DCIS was patterned after preexisting methods developed for grading IBCs, where a direct relationship between differentiation and clinical aggressiveness had been appreciated for a long time (24,25). All of these methods of classifying DCIS are still in use today, often interchangeably, which can be confusing and which could be improved.
Figure 3.
A relatively recent approach to classifying ductal carcinoma in situ is based on the degree that the tumor cells resemble normal cells (referred to as differentiation), and the rate the cells are proliferating. Histological grading systems have been developed, which assign scores or points to convey the magnitude of certain cellular features in the tumor, such as the degree of gland or papillae formation, nuclear size and shape, mitotic rate, and the amount of central necrosis. There are several methods and their details vary, but most recognize three grades corresponding to well (grade 1), moderately (grade 2), and poorly (grade 3) differentiated. However, there is no accepted standard method of grading. DCIS = ductal carcinoma in situ.
Current thinking is that most IBCs evolve through a nonobligatory series of increasingly abnormal “stages” over long periods of time, probably decades in most cases (Figure 4). In order, the stages are generally referred to as hyperplasia, atypical hyperplasia, and in situ carcinoma. DCIS is the most common (80%–90%) type of in situ carcinoma in the breast, it represents an advanced or late stage of premalignant tumor progression, and it is the direct precursor of most IBCs, which is supported by a great deal of indirect but compelling evidence (4). For example, nearly all IBCs are accompanied by DCIS, and foci of histological continuity can be found between them (Figure 4) (21). The major risk factors for developing IBC are the same for DCIS (11,26). Furthermore, DCIS diagnosed in the past, especially if not completely excised, is a strong risk factor for developing IBC in the future (7,27–29). DCIS and IBC share many identical genetic abnormalities, especially when they are in the same breast (4,30). Genetically engineered animal models of breast cancer progress from in situ to invasive disease (31,32). Progression of noninvasive to invasive cancer occurs in other organs where it is easier to observe, such as skin and cervix, so there is ample biological precedence.
Figure 4.
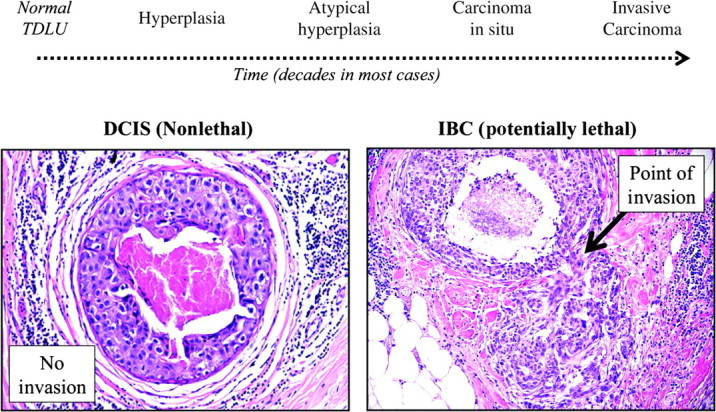
Invasive breast cancers (IBCs) are thought to evolve through a nonobligatory series of increasingly abnormal “stages,” referred to as hyperplasia, atypical hyperplasia, and carcinoma in situ over long periods of time, probably decades in most cases. Ductal carcinoma in situ (DCIS) is the main type of carcinoma in situ in the breast (80%–90%) and a late stage of breast cancer evolution. Many types of evidence support the hypothesis that DCIS are the immediate precursor of IBCs, including points of histological continuity (right photomicrograph).
There have been many studies of the biological and molecular features of DCIS, especially during the past 30–40 years. For the most part, nearly everything known about DCIS was studied first in IBC (4,33–36). Surprisingly, we learned that the tumor cells of DCIS and IBC are highly similar at the cellular and molecular levels, even though one is invasive and the other is not (12,15,34,37–40). The similarities extend even to global gene expression profiles where DCIS has recently been classified into luminal, basal, and erbB2 intrinsic molecular subtypes that were originally defined in microarray studies of IBC (21). Obviously, however, there must be biological differences between the tumor cells of DCIS and IBC that are responsible for invasion, but they have been surprisingly difficult to identify so far. Relatively recently, we learned that adjacent stromal cells must cooperate with tumor cells for invasion to occur, and that invasive tumors have many similarities with healing wounds (15,41–44). Investigators are currently working hard to determine the cellular and molecular mechanisms of these epithelial–stromal interactions.
It would be very useful to know the natural history of DCIS, including how it develops, whether it will progress to IBC, and when (14–16). We know that some DCIS progress in an average lifespan because nearly all IBCs are found intermingled with genetically similar DCIS, which they evolved from (21). We do not know the proportion of DCIS overall that progress to IBC because they are either detected and excised or, unfortunately, not detected at all. However, there are a few small clinical follow-up studies of patients with DCIS that were originally misdiagnosed as benign, so they were not completely excised surgically, suggesting that at least a third, and possibly more, eventually progress to IBC if undetected (29,45–48).
If detected, current therapy for DCIS is actually quite effective, although there is still much room for improvement (11,19,20,49). Better methods of detection, and improved access to them, would be highly beneficial. New methods that precisely identify the boundaries of DCIS would enable surgeons to completely excise them, eliminating local recurrences (19). A deeper understanding of the molecular mechanisms of invasion could lead to new therapeutic strategies to treat DCIS, or prevent it from developing, as well as new methods to determine the likelihood of progression, so therapy could be individualized. This symposium will review the state-of-the-science regarding the detection, treatment, and scientific knowledge of DCIS.
Funding
This work was partially supported by the Breast Cancer Research Foundation.
References
- 1.Osborne MP. Breast anatomy and development. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors; Harris JRLM, Morrow M, Hellman S, Osborne CK, translators. Diseases of the Breast. 3rd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2004. pp. 3–14. trans. [Google Scholar]
- 2.Allred DC. Biological characteristics of ductal carcinoma in situ. In: Silverstein ML, editor. Ductal Carcinoma In Situ of the Breast. 2nd ed. Philadelphia, PA: Lipincott: Williams and Wilkins; 2002. pp. 37–48. [Google Scholar]
- 3.Wellings RR, Jensen HM. On the origin and progression of ductal carcinoma in the human breast. J Natl Cancer Inst. 1973;50(5):1111–1118. doi: 10.1093/jnci/50.5.1111. [DOI] [PubMed] [Google Scholar]
- 4.Allred DC. Biological features of human premalignant breast disease and the progression to cancer. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the Breast. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2009. pp. 323–334. [Google Scholar]
- 5.Cheatle GL, Cutler M. Malignant epithelial neoplasia. Carcinoma. The precancerous or potentially carcinomatous state. In: Cheatle GL, Cutler M, editors. Tumours of the Breast. 1st ed. Philadelphia, PA: Lippincott; 1926. pp. 161–332. [Google Scholar]
- 6.Foote FW, Stewart FW. Comparative studies of cancerous versus noncancerous breasts. Ann Surg. 1945;121(1):6–53. doi: 10.1097/00000658-194501000-00002. 197–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Page DL, Rogers LW. Carcinoma in situ (CIS) In: Page DL, Anderson TJ, editors. Diagnostic Histopathology of the Breast. 1st ed. New York, NY: Churchill Livingston; 1987. pp. 157–174. [Google Scholar]
- 8.Wellings SR, Jensen HM, Marcum RG. An atlas of subgross pathology of the human breast with special reference to possible precancerous lesions. J Natl Cancer Inst. 1975;55(2):231–273. [PubMed] [Google Scholar]
- 9.Muir R. The evolution of carcinoma of the mamma. J Pathol Bacteriol. 1941;LII(2):155–172. [Google Scholar]
- 10.Fechner RE. History of ductal carcinoma in situ. In: Silverstein ML, editor. Ductal Carcinoma In Situ of the Breast. 2nd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2002. pp. 3–16. [Google Scholar]
- 11.Morrow M, Harris JR. Ductal carcinoma in situ and microinvasive carcinoma. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the Breast. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. pp. 521–537. [Google Scholar]
- 12.Allred DC, Mohsin SK, Fuqua SA. Histological and biological evolution of human premalignant breast disease. Endocr Relat Cancer. 2001;8(1):47–61. doi: 10.1677/erc.0.0080047. [DOI] [PubMed] [Google Scholar]
- 13.Dalgin GS, Alexe G, Scanfeld D, et al. Portraits of breast cancer progression. BMC Bioinformatics. 2007;8:291. doi: 10.1186/1471-2105-8-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erbas B, Provenzano E, Armes J, Gertig D. The natural history of ductal carcinoma in situ of the breast: a review. Breast Cancer Res Treat. 2006;97(2):135–144. doi: 10.1007/s10549-005-9101-z. [DOI] [PubMed] [Google Scholar]
- 15.Kuerer HM, Albarracin CT, Yang WT, et al. Ductal carcinoma in situ: state of the science and roadmap to advance the field. J Clin Oncol. 2009;27(2):279–288. doi: 10.1200/JCO.2008.18.3103. [DOI] [PubMed] [Google Scholar]
- 16.Polyak K. Breast cancer: origins and evolution. J Clin Invest. 2007;117(11):3155–3163. doi: 10.1172/JCI33295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schnitt SJ, Silen W, Sadowsky NL, Connolly JL, Harris JR. Ductal carcinoma in situ (intraductal carcinoma) of the breast. N Engl J Med. 1988;318(14):898–903. doi: 10.1056/NEJM198804073181406. [DOI] [PubMed] [Google Scholar]
- 18.Ernster VL, Barclay J. Increases in ductal carcinoma in situ (DCIS) of the breast in relation to mammography: a dilemma. Natl Cancer Inst Monogr. 1997;22:151–156. doi: 10.1093/jncimono/1997.22.151. [DOI] [PubMed] [Google Scholar]
- 19.Silverstein MJ, Lagios MD, Groshen S, et al. The influence of margin width on local control of ductal carcinoma in situ of the breast. N Engl J Med. 1999;340(19):1455–1461. doi: 10.1056/NEJM199905133401902. [DOI] [PubMed] [Google Scholar]
- 20.Solin LJ, Kurtz J, Forquet A, et al. Fifteen-year results of breast-conserving surgery and definitive breast irradiation for the treatment of ductal carcinoma in situ of the breast. J Clin Oncol. 1996;14(3):754–763. doi: 10.1200/JCO.1996.14.3.754. [DOI] [PubMed] [Google Scholar]
- 21.Allred DC, Wu Y, Mao S, et al. Ductal carcinoma in situ and the emergence of diversity during breast cancer evolution. Clin Cancer Res. 2008;14(2):370–378. doi: 10.1158/1078-0432.CCR-07-1127. [DOI] [PubMed] [Google Scholar]
- 22.Shoker BS, Sloane JP. DCIS grading schemes and clinical implications. Histopathology. 1999;35(5):393–400. doi: 10.1046/j.1365-2559.1999.035005393.x. [DOI] [PubMed] [Google Scholar]
- 23.Tavassoli FA, Schitt SJ, Hoefler H, et al. Intraductal proliferative lesions. In: Tavassoli FA, Devillee P, editors. Pathology & Genetics. Tumours of the Breast and Female Genital Organs. Lyon, France: IARC Press; 2003. pp. 63–73. [Google Scholar]
- 24.Elston EW, Ellis IO. Method for grading breast cancer. J Clin Pathol. 1993;46(2):189–190. doi: 10.1136/jcp.46.2.189-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rakha EA, El-Sayed ME, Lee AH, et al. Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol. 2008;26(19):3153–3158. doi: 10.1200/JCO.2007.15.5986. [DOI] [PubMed] [Google Scholar]
- 26.Bernstein L. The epidemiology of breast carcinoma in situ. In: Silverstein ML, editor. Ductal Carcinoma In Situ of the Breast. 2nd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2002. pp. 22–34. [Google Scholar]
- 27.Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985;312(3):146–151. doi: 10.1056/NEJM198501173120303. [DOI] [PubMed] [Google Scholar]
- 28.Page DL. Cancer risk assessment in benign breast biopsies. Human Pathol. 1986;17(9):871–874. doi: 10.1016/s0046-8177(86)80636-0. [DOI] [PubMed] [Google Scholar]
- 29.Sanders ME, Schuyler PA, Dupont WD, Page DL. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103(12):2481–2484. doi: 10.1002/cncr.21069. [DOI] [PubMed] [Google Scholar]
- 30.O’Connell P, Pekkel V, Fuqua SAW, Osborne CK, Allred DC. Loss-of-heterozygosity analysis in 399 premalignant breast lesions at 15 genetic loci. J Natl Cancer Inst. 1998;(90):697–703. doi: 10.1093/jnci/90.9.697. [DOI] [PubMed] [Google Scholar]
- 31.Allred DC, Medina D. The relevance of mouse models to the development and progression of human breast cancer. J Mammary Gland Biol Neoplasia. 2008;(13):279–288. doi: 10.1007/s10911-008-9093-5. [DOI] [PubMed] [Google Scholar]
- 32.Miller FR. Xenograft models of premalignant breast disease. J Mammary Gland Biol Neoplasia. 2000;5(4):379–391. doi: 10.1023/a:1009577811584. [DOI] [PubMed] [Google Scholar]
- 33.Bobrow LG, Happerfield LC, Gregory WM, Springall RD, Millis RR. The classification of ductal carcinoma in situ and its association with biological markers. Semin Diag Pathol. 1994;11(3):199–207. [PubMed] [Google Scholar]
- 34.Gupta SK, Douglas-Jones AG, Morgan JM, Mansel RE. The clinical behavior of breast carcinoma is probably determined at the preinvasive stage (ductal carcinoma in situ) Cancer. 1997;80(9):1740–1745. [PubMed] [Google Scholar]
- 35.Moreno A, Lloveras B, Figueras A, et al. Ductal carcinoma in situ of the breast: correlation between histologic classifications and biologic markers. Mod Pathol. 1997;10(11):1088–1092. [PubMed] [Google Scholar]
- 36.Poller DN, Silverstein MJ, Galea M, et al. Ductal carcinoma in situ of the breast: a proposal for a new simplified histological classification association between cellular proliferation and c-erbB-2 protein expression. Mod Pathol. 1994;7(2):257–262. [PubMed] [Google Scholar]
- 37.Ma XJ, Salunga R, Tuggle JT, et al. Gene expression profiles of human breast cancer progression. Proc Natl Acad Sci U S A. 2003;100(10):5974–5979. doi: 10.1073/pnas.0931261100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Porter D, Lahti-Domenici J, Keshaviah A, et al. Molecular markers in ductal carcinoma in situ of the breast. Mol Cancer Res. 2003;1(5):362–375. [PubMed] [Google Scholar]
- 39.Castro NP, Osorio CA, Torres C, et al. Evidence that molecular changes in cells occur before morphological alterations during the progression of breast ductal carcinoma. Breast Cancer Res. 2008;10(5):R87. doi: 10.1186/bcr2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hannemann J, Velds A, Halfwerk JB, Kreike B, Peterse JL, van de Vijver MJ. Classification of ductal carcinoma in situ by gene expression profiling. Breast Cancer Res. 2006;8(5):R61. doi: 10.1186/bcr1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allinen M, Beroukhim R, Cai L, et al. Molecular characterization of the tumor microenvironment in breast cancer. Cancer Cell. 2004;6(1):17–32. doi: 10.1016/j.ccr.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 42.Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat Rev Cancer. 2006;6(5):392–401. doi: 10.1038/nrc1877. [DOI] [PubMed] [Google Scholar]
- 43.Park CC, Bissell MJ, Barcellos-Hoff MH. The influence of the microenvironment on the malignant phenotype. Mol Med Today. 2000;6(8):324–329. doi: 10.1016/s1357-4310(00)01756-1. [DOI] [PubMed] [Google Scholar]
- 44.Polyak K, Hu M. Do myoepithelial cells hold the key for breast tumor progression? J Mammary Gland Biol Neoplasia. 2005;10(3):231–247. doi: 10.1007/s10911-005-9584-6. [DOI] [PubMed] [Google Scholar]
- 45.Bestill WL, Jr, Rosen PP, Lieberman PH, Robbins GF. Intraductal carcinoma: long-term follow-up after treatment by biopsy alone. JAMA. 1978;239(18):1863–1867. doi: 10.1001/jama.239.18.1863. [DOI] [PubMed] [Google Scholar]
- 46.Eusebi V, Feudale E, Foschini MP, et al. Long-term follow-up of in situ carcinoma of the breast. Sem Diag Pathol. 1994;11:223–235. [PubMed] [Google Scholar]
- 47.Page DL, Dupont WD, Rogers LW, Landenberger M. Intraductal carcinoma of the breast: follow-up after biopsy only. Cancer. 1982;49(4):751–758. doi: 10.1002/1097-0142(19820215)49:4<751::aid-cncr2820490426>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 48.Rosen PP, Braun DW, Jr, Kinne DE. The clinical significance of preinvasive breast carcinomas. Cancer. 1980;46:919–925. doi: 10.1002/1097-0142(19800815)46:4+<919::aid-cncr2820461311>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 49.O’Sullivan MJ, Morrow M. Ductal carcinoma in situ—current management. Surg Clin North Am. 2007;87(2):333–351. doi: 10.1016/j.suc.2007.01.006. viii. [DOI] [PubMed] [Google Scholar]