Abstract
Purpose of review
Polypropylene mesh has been widely used in the surgical repair of pelvic organ prolapse. However, low but persistent rates of complications related to mesh, most commonly mesh exposure and pain, have hampered its use. Complications are higher following transvaginal implantation prompting the Food and Drug Administration to release two public health notifications warning of complications associated with transvaginal mesh use (PHN 2008 and 2011) and to upclassify transvaginal prolapse meshes from Class II to Class III devices. Although there have been numerous studies to determine the incidence and management of mesh complications as well as impact on quality of life, few studies have focused on mechanisms.
Recent findings
In this review, we summarize the current understanding of how mesh textile properties and mechanical behavior impact vaginal structure and function, as well as the local immune response. We also discuss how mesh properties change in response to loading.
Summary
We highlight a few areas of current and future research to emphasize collaborative strategies that incorporate basic science research to improve patient outcomes.
Keywords: host response, polypropylene prolapse mesh, pore stability, mechanical behavior, textile properties
INTRODUCTION
Polypropylene meshes have been increasingly used in the surgical repair of pelvic organ prolapse [1,2]. In the USA in 2011, roughly 300 000 prolapse surgeries were performed of which at least one-third involve the use of mesh [3] and about three-quarters are implanted transvaginally [4]. The goal of mesh is to improve anatomical outcomes over native tissue repairs and to improve the integrity of what is likely to be a biochemically and biomechanically compromised tissue. While Level I evidence supports the use of polypropylene mesh in terms of anatomical outcomes in abdominal sacrocolpopexy, evidence is less robust in supporting transvaginal mesh kits balancing anatomical successes with complications [5▪]. Complications after sacrocolpopexy appear to increase over time with cumulative incidence of mesh exposure at 10.5% over a 7-year period [6] and those following transvaginal application occur at rates roughly two-fold higher [7]. Mesh complications include exposure through the vaginal wall, erosion into adjacent structures, infection, and pain prompting the Food and Drug Administration (FDA) to issue two public statements – the first in 2008 warning of serious complications associated with the transvaginal placement of surgical mesh and a second in 2011 warning that mesh complications are not rare events (2874 reports over 3 years in MAUDE database). More recently, transvaginal meshes for pelvic organ prolapse were upclassified from Class II devices (generally moderate risk devices) to Class III devices (generally high risk devices), meaning new products will need more rigorous clinical data for premarket approval by the FDA before they are marketed. Thus, an improved understanding of the behavior of mesh in vivo and its impact on the vagina is imperative for both physicians and patients alike.
While the etiology of mesh complications is still not clear, it is likely that multiple factors contribute including the quality of host tissue (stage of prolapse, age, and genetics), the patient’s health at the time which the mesh is placed (hormone levels, diabetes, obesity, and tobacco use), surgical technique (thickness of the dissection), route of implantation (vaginal vs. abdominal), host immune response, textile properties of the mesh (porosity, pore size, weight, and knit pattern) and mechanical behavior. The focus of this review will be placed on basic science discoveries on mesh properties, mechanical behavior, host immune response and impact on tissue structure and function. Exploration of novel meshes for future prolapse repair will also be reviewed.
KEY POINTS.
Textile properties of synthetic prolapse meshes such as knit pattern, weight, pore size, porosity are closely related to their structural properties and mechanical behaviors.
Lighter weight meshes with higher porosity and lower stiffness usually achieve more favorable host responses and better tissue in-growth compared with heavier weight meshes with lower porosity and higher stiffness.
Maintaining the stability of mesh pore geometry under loading conditions is important to prevent mesh deformation, such as mesh shrinking, wrinkling, buckling, and/or folding, when implanted in vivo.
TEXTILE PROPERTIES OF POLYPROPYLENE MESH: IMPACT ON HOST RESPONSE
It has been well established in the hernia literature that mesh textile properties, that is, knit pattern, weight (g/m2), porosity, and pore size are important parameters in directing host responses to mesh implants. Synthetic meshes can be composed of fibers that are woven or knitted. Knitted meshes are generally preferred as they are more porous and conformable/flexible relative to woven meshes. Additionally, woven meshes are associated with higher complication rates, as fibers in woven materials can slide together resulting in spaces that are big enough to allow the passage of bacteria but too small for the passage of immune cells resulting in chronic infection [8–10]. In terms of weight, heavier meshes tend to induce a more pronounced and prolonged inflammatory response, more apoptotic cells in the area of the mesh fibers and increased turnover of tissues surrounding mesh fibers up to 1 year after implantation as shown in animal abdominal wall and sacrocolpopexy models [11–13,14▪,15,16▪]. On the other hand, lighter weight meshes achieved by thinner fibers and larger pore sizes have shown improved biocompatibility compared with heavy weight meshes [17].
Arguably, pore size and porosity are the two most important textile properties that impact both the short-term and long-term host immune response to mesh. Large pore sizes in hernia meshes have corresponded to a more favorable host response with increased tissue in-growth, greater vascular penetration, and decreased risk of bacteria colonization [17]. Additionally, large pore and high porosity meshes yield less inflammation, less fibrous tissue, and decreased potential for adhesion formation relative to meshes with small pores and lower porosity [18,19]. Mesh pore size is also inversely related to bridging fibrosis (i.e. as pore size increases, the incidence of bridging fibrosis decreases) [18,19]. Bridging fibrosis refers to a phenomenon that occurs when the foreign body response to a single mesh fiber overlaps or merges with that of a neighboring fiber resulting in a continuous fibrotic response or encapsulation of the mesh. The latter, can lead to pain, contraction, and the perception of shrinkage of the mesh. When using polypropylene meshes, to prevent bridging fibrosis and optimize tissue in-growth it is recommended that pore sizes be ≥1 mm [19,20].
STRUCTURAL PROPERTIES AND MECHANICAL BEHAVIOR OF POLYPROPYLENE MESH
On the basis of the success of hernia meshes, the majority of surgeons who use prolapse meshes have turned to knitted, lightweight (18–42 g/m2), large pore (>1500 mm), high porosity (>55%), monofilament polypropylene. The prototype polypropylene mesh, Gynemesh PS (Ethicon), is known as Prolene Soft when used in hernia repair. As Gynemesh was introduced into the market, numerous vendors marketed their own products, all of which were hernia meshes simply remarketed for the indication of prolapse. The newer meshes were found to be significantly lighter than Gynemesh and to have higher porosities (Table 1). Additionally, when subjected to a simple uniaxial load to failure test and the multiaxial ball burst test, current widely used prolapse meshes showed vastly different structural properties [22]. Stiffness is a term that describes the ability of a material to resist deformation under an applied load. Mesh weight and porosity have been found to be strongly correlated with mesh stiffness [22]. Furthermore, for some meshes (e.g. Gynemesh PS, Alyte, Restorelle, and UltraPro) structural properties are highly dependent on the direction in which the mesh is loaded [22,23▪]. These meshes are considered to be anisotropic – a property that is associated with the knit pattern of the mesh.
Table 1.
Characteristics of prolapse meshes with names when applied transabdominally vs. transvaginally
| Transabdominal | Vaginal | Vendor | Weight (g/m2) | Pore Size (mm) | Porosity (%) | Stiffness (N/mm) |
|---|---|---|---|---|---|---|
| Gynemesh PS | Proliftb | Ethicon | 42 | 2.5 | 62 | 0.29 |
| Upsylon | Uphold lite | Boston Sci | 25 | 2.8 | 72 | 0.2 |
| Alyte vaginal | Avaultab | Bard | 18 | 2.8 | 75 | 0.16 |
| Ultraproa | Prolift plus Mb | Ethicon | 28 | 3.8 | 68 | 0.01 |
| Restorelle | Direct Fix | Coloplast | 19 | 1.8 | 78 | 0.18 |
| Novasilk | Exair | Coloplast | 19 | 1.5 | 67 | 0.072 |
| IntePro Lite | Elevate | AMS | 26 | 2.4 | 68 | 0.071 |
Adapted with permission from [21].
UltraPro (aka Artisyn), measurements made after absorbable component absorbed; stiffness determined in a uniaxial load to failure test.
No longer available on the market.
Although mesh stiffness is needed to sustain load in prolapse surgeries, an inappropriately high stiffness of implants can result in ‘stress shielding’. The latter describes a phenomenon that occurs when two objects are physically connected. When loaded, the stiffer material (mesh) bears the majority of the load. The less stiff material (soft tissue) now shielded from the load it normally experiences undergoes a maladaptive remodeling response characterized by degeneration and atrophy (loss of collagen, elastin, and skeletal/smooth muscle). In this way, prosthetic devices that are significantly stiffer than the native tissue they are designed to augment are associated with an increased rate of long-term complications. In prolapse mesh repair, it can be assumed that movement toward a lower stiffness mesh would be associated with better patient outcomes as the properties of the mesh would be better matched with those of the underlying vagina. Given the positive correlation between stiffness and mesh weight/porosity, lower stiffness materials would also be expected to be associated with a more favorable host foreign body response and better tissue incorporation.
In vivo, synthetic mesh is predominantly exposed to uniaxial forces. Assessing prolapse meshes uniaxially and in response to physiologic loads has provided key information regarding the mechanical behavior of mesh. When subjected to repetitive loading, prolapse meshes tend to permanently deform and this deformation is irreversible [24,25]. A mesh in which deformation is reversible will instead display an elastic-like behavior. When loaded, prolapse meshes are also impacted by the applied boundary conditions (i.e. the way in which forces/displacements are applied and how movement is allowed/restricted). Sutures used to attach prolapse mesh to the vagina and the pelvic sidewall or sacrum essentially act as point loads. Applying point loads during uniaxial loading results in out-of-plane deformation resulting in mesh wrinkling, buckling, and/or folding [26▪]. Additionally, increasing the number of point loads leads to a greater degree of mesh wrinkling. In the areas wherein the mesh has wrinkled, there is an increased amount of material and it is likely that the foreign body response to the mesh in this area is enhanced.
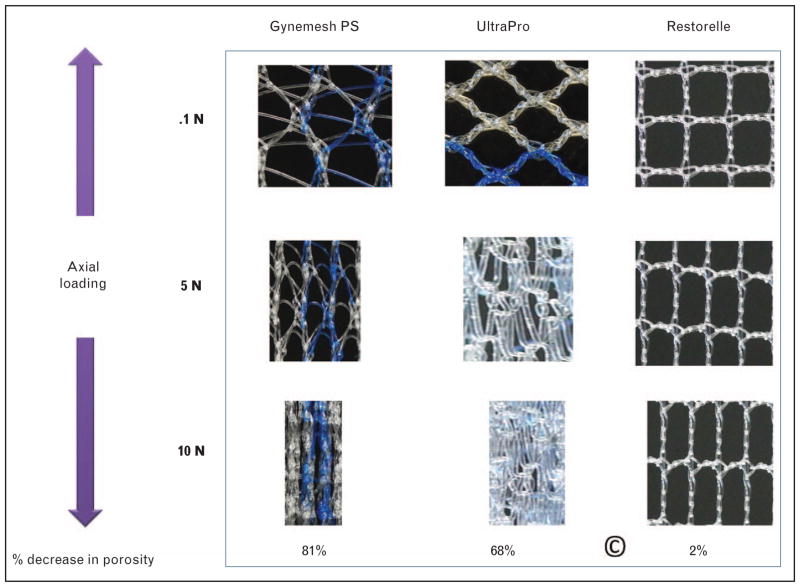
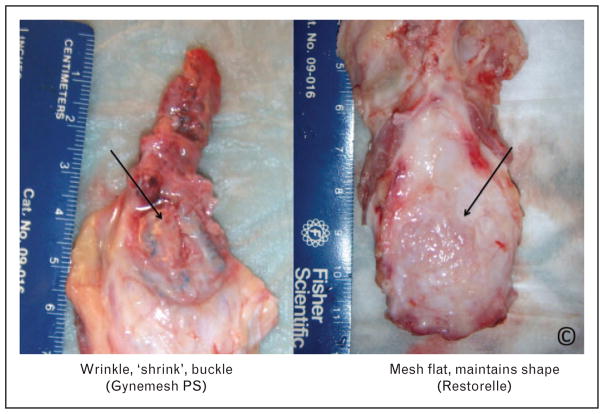
In addition to wrinkling with uniaxial loading, prolapse meshes exhibit a marked decrease in pore size accompanied by a loss in porosity (i.e. pore collapse). After exposing the transvaginal meshes Prolift and Prolift plus M (also known as Gynemesh and UltraPro or Artisyn) to relatively small loads, Otto et al. [27] observed a loss of porosity in both the arms and central body of the mesh. In a further assessment of prolapse meshes loaded in a sacrocol-popexy model, Barone et al. [23▪] saw similar results. When loaded to 5 N (1.1 lbs), Gynemesh PS, Alyte and UltraPro demonstrated a loss in porosity ranging from 2 to 87% and by 10 N most experienced a complete loss of porosity with virtually no pores ≥1 mm (Fig. 1). The direction of loading and orientation of the pores were found to play a critical role in the degree of pore collapse. For example, Restorelle (Coloplast) has a square pore. When loaded in the square configuration at 5 N and 10 N, the mesh demonstrated a markedly stable geometry experiencing a loss of porosity of only 2% after loading to 10 N with all pores remaining >1 mm (Fig. 1). However, rotating the pores of Resorelle by 45°, a 90% reduction in porosity was observed [23▪]. Given the importance of pore size and porosity, the reduction in pore size (less than 1 mm), porosity, and effective porosity all potentially decrease the biocompatibility of synthetic mesh (Fig. 2). This may also lead to an increased risk of bridging fibrosis, inflammation, poor tissue integration, and fibrosis, which may ultimately result in poor patient outcomes.
FIGURE 1.
Uniaxial tensile loading dramatically alters the pore size and pore geometries of nearly all mesh products. As shown, Gynemesh PS and UltraPro significantly deform at low loads (10 N). Macroscopically, the meshes undergo lateral contraction (Poisson’s effect). Microscopically pore dimensions are drastically reduced bringing filaments closer together. These behaviors are consistent with a markedly unstable geometry. In contrast, Restorelle (square pore) is stable, with minimal loss of porosity at 10 N [23▪]. Adapted with permission from [23▪].
FIGURE 2.
Mesh vagina complex excised 3 months after insertion of mesh of identical dimensions in the primate by sacrocolpopexy. While Gynemesh PS buckles, laterally contracts and loses porosity when loaded, Restorelle (square pore) maintains its original flat conformation [28]. Adapted with permission from [28].
MESH-TISSUE INTERACTION: IMPACT ON HOST RESPONSE AND TISSUE INTEGRITY
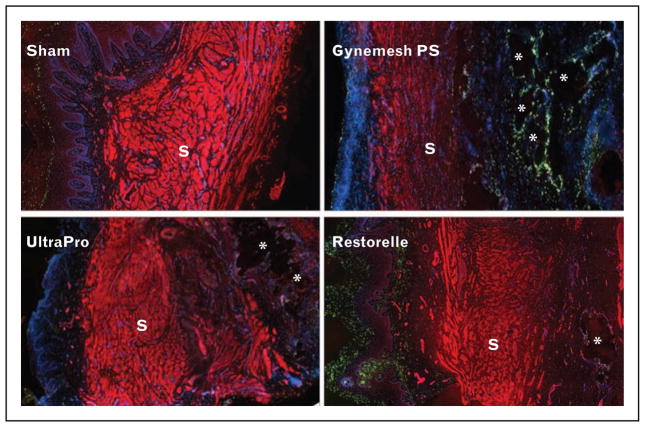
To test the hypothesis that lower weight, higher porosity, lower stiffness prolapse meshes would be associated with a more favorable host response, prolapse meshes in which these characteristics varied were implanted by sacrocolpopexy in non-human primates. The results showed that Restorelle, the lowest weight, highest porosity and lowest stiffness mesh available on the market exhibited minimal negative impact on the underlying vaginal tissue as determined using functional, structural, and morphological endpoints. In contrast, meshes with heavier weight, lower porosity and higher stiffness such as Gynemesh PS, induced degradation of key matrix structural proteins (collagen and elastin), impaired smooth muscle contractility and inferior mechanical properties (Fig. 3) [15,28,29▪]. The tissue incorporation into the mesh was poor with increased cell apoptosis; particularly in the area of mesh fibers. Increased collagen and elastin degradation were accompanied by an increase in active matrix metalloproteinase (MMP)-1, -8, -13, and total MMP-2 and -9 indicative of ongoing tissue destruction [30▪]. While these degenerative changes could be attributed to ‘stress shielding’ as Gynemesh is one of the stiffest prolapse meshes, it is not clear whether the response is purely mechanical or the host is simply responding to an increased mesh burden since mesh stiffness is directly related to mesh weight and porosity.
FIGURE 3.
Immunofluorescent labeling of smooth muscle and in situ cell apoptosis in the vagina of rhesus macaque following the implantation of Gynemesh PS, UltroPro and Restorelle at 3 months. The red signal represents positive staining of α-SMA; the green signal represents apoptotic cells; the blue signal represents nuclei. S indicates the smooth muscle layer. * indicates the area of mesh fibers. The thickness of smooth muscle layer was significantly reduced in the Gynmesh PS group. In addition, following implantation with Gynemesh PS, the number of apoptotic cells was significantly increased in the subepithelium and adventitia compared to Sham and lower stiffness meshes, predominantly surrounding the mesh fibers. For the lower stiffness meshes, apoptotic cells were higher following implantation of UltraPro than Restorelle. Magnification: 100× [15]. Adapted with permission from [15].
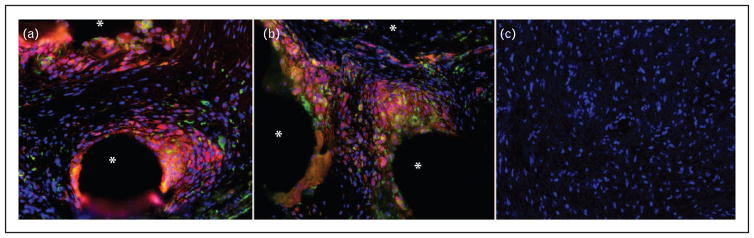
Similar to any synthetic material, polypropylene prolapse mesh behaves as a foreign body when implanted, inducing a robust inflammatory response [17,31] to each individual mesh fiber with the inflammatory reaction positively correlated to the amount of material implanted [32]. While early on in the healing process, mild to moderate inflammation may be beneficial for tissue incorporation, persistent or chronic inflammation is thought to be related to the development of complications such as pain, exposure, and erosion. In prolapse repair, lower weight higher porosity meshes have been shown to induce less pronounced inflammatory response associated with increased tissue incorporation consistent with a reconstructive response compared with heavier weight lower porosity mesh [14▪]. Such different outcomes may be dictated by macrophage phenotype differentiation in the early stage, a crucial cellular response in determining downstream long-term functional outcomes [33]. As one of the primary cell types responding to mesh implants, macrophages can differentiate into different phenotypes that exist along a continuum ranging from M1 (classically activated and pro-inflammatory) to M2 (anti-inflammatory, homeostatic, and wound-healing) with differential functional properties and patterns of gene expression in response to microenviromental cues. An M1 dominant reaction tends to be proinflammatory associated with increased release of high level of inducible nitric oxide synthase, toxic reactive oxygen species, and proinflammatory cytokines such as IL-1β, IL-6, and tumor necrosis factor (TNF)-α affording removal of pathogens and tissue debris but in the process also inducing damage to host tissues. In contrast, an M2 polarized reaction (subpopulations M2a, M2b, and M2c) is associated with the production of remodeling/reconstruction cytokines such as low molecular weight IL-12 and IL-23, and high molecular weight IL-10, and other molecules that favor constructive remodeling. In a recent study examining mesh-vaginal tissue complexes that were excised from women with the complications of pain and mesh exposure, a predominantly M1 proinflammatory response that persisted years after implantation has been observed around the mesh fibers with increased inflammatory cytokines and chemokines such as TNF-α, IL-12p40p70, IL-12p70, CXCL10, and CCL17 (Fig. 4). Specimens for which the mesh had been removed for the indication of exposure had increased levels of MMP-9 relative to mesh specimens removed for the indication of pain, suggesting ongoing tissue degradation in tissues associated with mesh exposure [16▪].
FIGURE 4.
Immunofluorescent labeling of pan-macrophage marker CD68 (red), M1 pro-inflammatory marker CD86 (orange), M2 pro-remodeling macrophage marker CD206 (green), and DAPI (blue). (a) a mesh-tissue section from a patient presenting with an exposure and implanted with the AMS Perigee prolapse mesh for 93 months; (b) a mesh-tissue section from a patient presenting with pain and implanted with the Gynecare TVT Secur for 6 months; (c) control tissue from patients without graft implantation. A predominance of pro-inflammatory M1 macrophages surround mesh fibers (*) consistent with a prolonged immune response could be observed in both (a) and (b); however, this response is limited to the area immediately adjacent to mesh fibers. Control tissue contained few or no macrophages as compared to mesh patient tissue. Magnification 200× [16▪]. Adapted with permission from [16▪].
FUTURE PROLAPSE MESHES
Given the importance of pore size and porosity in the host response, it can be argued that maintaining these properties of a mesh is crucial for biocompatibility and positive patient outcomes. Unfortunately, the majority of current synthetic meshes have unstable geometries when loaded with collapse of pores, nonplanar deformation (buckling and wrinkling) and narrowing at the midportion of the mesh (Poisson’s effect). Thus, a future goal of synthetic mesh is the development of a mesh that maintains a stable geometry with loading, does not experience pore collapse or narrowing, regardless of thedirection in which the load is applied. There are numerous ways in which this can be accomplished including reenforcing the mesh such that the pores remain stable (i.e. open) early after implantation or changing the geometry of the pores such that they remain open in response to loading. Regardless of the approach taken, it is believed that preventing the reduction in pore size and loss of porosity in response to loading will allow for adequate tissue in-growth and integration possibly reducing the risk of mesh-related complications. Finally, developing meshes from an elastomeric material that does not permanently deform when loaded but rather returns to its original shape, is a desirable feature of future meshes.
CONCLUSION
Current polypropylene prolapse meshes are associated with persistent rates of complications; particularly, mesh exposure and pain. Insight into the mechanisms of complications has provided us with tools to develop new materials that are more compatible with conditions imposed on the meshes when implanted on the vagina.
Acknowledgments
We would like to thank Dr William R. Barone for his assistance with the manuscript.
Financial support and sponsorship
This work was supported by National Institute of Health (R01 HD061811-01) and Department of Obstetrics, Gynecology & Reproductive Sciences, University of Pittsburgh, USA.
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
- 1.Maher C, Baessler K. Surgical management of anterior vaginal wall prolapse: an evidence based literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:195–201. doi: 10.1007/s00192-005-1296-3. [DOI] [PubMed] [Google Scholar]
- 2.Mistrangelo E, Mancuso S, Nadalini C, et al. Rising use of synthetic mesh in transvaginal pelvic reconstructive surgery: a review of the risk of vaginal erosion. J Minim Invasive Gynecol. 2007;14:564–569. doi: 10.1016/j.jmig.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Shah AD, Kohli N, Rajan SS, et al. The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:421–428. doi: 10.1007/s00192-007-0457-y. [DOI] [PubMed] [Google Scholar]
- 4.Jonsson Funk M, Edenfield AL, Pate V, et al. Trends in use of surgical mesh for pelvic organ prolapse. Am J Obstet Gynecol. 2013;208:79, e71–77. doi: 10.1016/j.ajog.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5▪.Maher C, Feiner B, Baessler K, et al. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079. doi: 10.1002/14651858.CD012079. This is the most recent comprehensive review of randomized controlled trials comparing different types of vaginal repair (mesh, biological graft, or native tissue). This article suggests that the transvaginal mesh has limited utility in primary surgery based on the risk-benefit profile. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016–2024. doi: 10.1001/jama.2013.4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004014. doi: 10.1002/14651858.CD004014.pub5. [DOI] [PubMed] [Google Scholar]
- 8.Chen CC, Ridgeway B, Paraiso MF. Biologic grafts and synthetic meshes in pelvic reconstructive surgery. Clin Obstet Gynecol. 2007;50:383–411. doi: 10.1097/GRF.0b013e31804b184c. [DOI] [PubMed] [Google Scholar]
- 9.Cobb WS, Peindl RM, Zerey M, et al. Mesh terminology 101. Hernia. 2009;13:1–6. doi: 10.1007/s10029-008-0428-3. [DOI] [PubMed] [Google Scholar]
- 10.Wohlrab KJ, Erekson EA, Myers DL. Postoperative erosions of the Mersilene suburethral sling mesh for antiincontinence surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:417–420. doi: 10.1007/s00192-008-0787-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klinge U, Junge K, Stumpf M, et al. Functional and morphological evaluation of a low-weight, monofilament polypropylene mesh for hernia repair. J Biomed Mater Res. 2002;63:129–136. doi: 10.1002/jbm.10119. [DOI] [PubMed] [Google Scholar]
- 12.Novitsky YW, Cristiano JA, Harrell AG, et al. Immunohistochemical analysis of host reaction to heavyweight-, reduced-weight-, and expanded polytetrafluoroethylene (ePTFE)-based meshes after short- and long-term intraabdominal implantations. Surg Endosc. 2008;22:1070–1076. doi: 10.1007/s00464-007-9737-3. [DOI] [PubMed] [Google Scholar]
- 13.Costello CR, Bachman SL, Grant SA, et al. Characterization of heavyweight and lightweight polypropylene prosthetic mesh explants from a single patient. Surg Innov. 2007;14:168–176. doi: 10.1177/1553350607306356. [DOI] [PubMed] [Google Scholar]
- 14▪.Brown BN, Mani D, Nolfi AL, et al. Characterization of the host inflammatory response following implantation of prolapse mesh in rhesus macaque. Am J Obstet Gynecol. 2015;213:668, e661–610. doi: 10.1016/j.ajog.2015.08.002. This article highlights the importance of mesh textile and structural properties in macrophage responses and phenotype dichotomization in the vaginal foreign body reaction caused by mesh implantation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang R, Abramowitch S, Knight K, et al. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG. 2013;120:233–243. doi: 10.1111/1471-0528.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16▪.Nolfi AL, Brown BN, Liang R, et al. Host response to synthetic mesh in women with mesh complications. Am J Obstet Gynecol. 2016 doi: 10.1016/j.ajog.2016.04.008. Epub ahead of print This article provides important evidence of the prolonged inflammatory responses up to years after implantation of synthetic meshes and highlights its possible role in the development of mesh complications (exposure and pain). It also reveals the role of MMP9 in the process of mesh exposure. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel H, Ostergard DR, Sternschuss G. Polypropylene mesh and the host response. Int Urogynecol J. 2012;23:669–679. doi: 10.1007/s00192-012-1718-y. [DOI] [PubMed] [Google Scholar]
- 18.Orenstein SB, Saberski ER, Kreutzer DL, et al. Comparative analysis of histopathologic effects of synthetic meshes based on material, weight, and pore size in mice. J Surg Res. 2012;176:423–429. doi: 10.1016/j.jss.2011.09.031. [DOI] [PubMed] [Google Scholar]
- 19.Klinge U, Klosterhalfen B, Birkenhauer V, et al. Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res. 2002;103:208–214. doi: 10.1006/jsre.2002.6358. [DOI] [PubMed] [Google Scholar]
- 20.Klinge U, Klosterhalfen B. Modified classification of surgical meshes for hernia repair based on the analyses of 1,000 explanted meshes. Hernia. 2012;16:251–258. doi: 10.1007/s10029-012-0913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barone WR, Abramowitch SD, Moalli P. The impact of host response on biomaterial selection, host response to surgical mesh materials used for pelvic floor reconstruction. In: Badylak S, editor. Host response to biomaterials. 1. Academic Press, Elsevier; 2015. pp. 1111–1123. [Google Scholar]
- 22.Feola A, Barone W, Moalli P, et al. Characterizing the ex vivo textile and structural properties of synthetic prolapse mesh products. Int Urogynecol J. 2013;24:559–564. doi: 10.1007/s00192-012-1901-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪.Barone WR, Moalli PA, Abramowitch SD. Textile properties of synthetic prolapse mesh in response to uniaxial loading. Am J Obstet Gynecol. 2016 doi: 10.1016/j.ajog.2016.03.023. Epub ahead of print This article highlights that nearly none of the current prolapse meshes have stability of pore geometry under loading conditions. It not only improves our understanding of the impact of mechanical loading on the textile properties of mesh, but also has instructive implications for the development of more effective devices for prolapse repair. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones KA, Feola A, Meyn L, et al. Tensile properties of commonly used prolapse meshes. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:847–853. doi: 10.1007/s00192-008-0781-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shepherd JP, Feola AJ, Abramowitch SD, et al. Uniaxial biomechanical properties of seven different vaginally implanted meshes for pelvic organ prolapse. Int Urogynecol J. 2012;23:613–620. doi: 10.1007/s00192-011-1616-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪.Barone WR, Amini R, Maiti S, et al. The impact of boundary conditions on surface curvature of polypropylene mesh in response to uniaxial loading. J Biomech. 2015;48:1566–1574. doi: 10.1016/j.jbiomech.2015.02.061. This is the first publication using a computational model to demonstrate the mechanism of mesh wrinkling, buckling, and/or folding that have been observed clinically in mesh complications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Otto J, Kaldenhoff E, Kirschner-Hermanns R, et al. Elongation of textile pelvic floor implants under load is related to complete loss of effective porosity, thereby favoring incorporation in scar plates. J Biomed Mater Res A. 2014;102:1079–1084. doi: 10.1002/jbm.a.34767. [DOI] [PubMed] [Google Scholar]
- 28.Feola A, Abramowitch S, Jallah Z, et al. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. BJOG. 2013;120:224–232. doi: 10.1111/1471-0528.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪.Jallah Z, Liang R, Feola A, et al. The impact of prolapse mesh on vaginal smooth muscle structure and function. BJOG. 2016;123:1076–1085. doi: 10.1111/1471-0528.13514. This article provides important evidence that heavier, less porous and stiffness meshes have negative impact on the vaginal smooth muscles and innervations. It highlights the importance of mesh textile and structural properties in determining host–mesh interaction and tissue structures. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪.Liang R, Zong W, Palcsey S, et al. Impact of prolapse meshes on the metabolism of vaginal extracellular matrix in rhesus macaque. Am J Obstet Gynecol. 2015;212:174, e171–177. doi: 10.1016/j.ajog.2014.08.008. This article is the first publication to demonstrate on the molecular level the negative impact of a heavier, less porous and stiffer mesh on the vaginal connective tissue remodeling. It highlights the importance of mesh textile and structural properties in host–mesh interaction and tissue remodeling. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clave A, Yahi H, Hammou JC, et al. Polypropylene as a reinforcement in pelvic surgery is not inert: comparative analysis of 100 explants. Int Urogynecol J. 2010;21:261–270. doi: 10.1007/s00192-009-1021-8. [DOI] [PubMed] [Google Scholar]
- 32.Rosch R, Junge K, Schachtrupp A, et al. Mesh implants in hernia repair. Inflammatory cell response in a rat model. Eur Surg Res. 2003;35:161–166. doi: 10.1159/000070045. [DOI] [PubMed] [Google Scholar]
- 33.Brown BN, Ratner BD, Goodman SB, et al. Macrophage polarization: an opportunity for improved outcomes in biomaterials and regenerative medicine. Biomaterials. 2012;33:3792–3802. doi: 10.1016/j.biomaterials.2012.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]