Abstract
Background and aims: Radical endoscopic excision of Barrett’s epithelium performing 4 – 6 endoscopic resections during the same endoscopic session results in complete Barrett’s eradication but has a high stricture rate (40 – 80 %). Therefore radiofrequency ablation is preferred after endoscopic mucosal resection (EMR) of visible nodules. We investigated the clinical outcome of non-radical, stepwise endoscopic mucosal resection with a maximum of two endoscopic resections per endoscopic session.
Methods: We analysed our prospectively maintained database of patients undergoing esophageal EMR for early neoplasia in Barrett’s esophagus from 2009 to 2014. EMR was performed using a maximum of two band ligation mucosectomies per endoscopic session; thereafter, follow-up was 3-monthly and EMR was repeated as required for Barrett’s eradication.
Results: In total, 118 patients underwent staging EMR for early Barrett’s neoplasia. Subsequently, 27 patients underwent surgery/chemotherapy due to deep submucosal or more advanced tumor stages or were managed conservatively. The remaining 91 patients with high grade dysplasia (48), intramucosal (38) or submucosal cancer (5) in the resected nodule underwent further endoscopic therapy with a mean follow-up of 24 months. Remission of dysplasia/neoplasia was achieved in 95.6 % after 12 months treatment. Stepwise endoscopic Barrett’s resection resulted in complete Barrett’s eradication in 36/91 patients (39.6 %) in a mean of four sessions; 40/91 patients (44.0 %) had a short circumferential Barrett’s segment (< 3 cm). In this group, repeated EMR achieved complete Barrett’s excision in 85.0 %. One patient developed a stricture (1.1 %), one a delayed bleeding, and there were no perforations.
Conclusion: In patients with a short Barrett’s segment, non-radical endoscopic Barrett’s resection at the time of scheduled endoscopy follow-up allows complete Barrett’s eradication with very low stricture rate.
Introduction
During the last decades, endoscopic treatment has widely replaced esophagectomy as first choice therapy for early neoplasia related to Barrett’s esophagus. The long-term outcome of endoscopic treatment and conventional esophagectomy for high grade dysplasia and intramucosal cancer is comparable but the adverse event rate and post-procedure quality of life are significantly in favor of endoscopic therapy.
Endoscopic resection of visible nodules followed by ablation of the remaining Barrett’s epithelium and endoscopic surveillance is the currently recommended standard treatment for high grade dysplasia and intramucosal cancer in Barrett’s esophagus 1 2 3. Endoscopic resection followed by radiofrequency ablation can achieve complete remission of dysplasia in more than 90 % 3 4 5 and complete remission of intestinal metaplasia in more than 77 % of patients 6 7.
Radiofrequency ablation allows the precise ablation of the columnar lined epithelium to a depth of about 500 to 700 µm, which usually comprises the mucosa and the upper parts of the submucosa. However, the disposable catheter probes for radiofrequency ablation are expensive and the costly generator equipment is not widely available. Moreover, radiofrequency ablation works by tissue destruction thus not providing histology; this might confer the small risk of burying an endoscopically unrecognized invasive cancer 8 9.
Radical endoscopic resection for complete eradication of Barrett’s epithelium was initially proposed as a definitive therapy but has not been pursued further due to a high stricture rate (48 – 88 %) when 4 – 5 resections were performed within the same endoscopic session 4 6 10 11. However, the question remains whether a non-radical approach with stepwise endoscopic resection in more frequent endoscopic sessions would also achieve complete remission of intestinal metaplasia but could avoid such a high rate of adverse events.
In our retrospective study from a prospectively maintained database, we investigated the outcome of stepwise, non-radical endoscopic resection to achieve complete remission of dysplasia and complete remission of intestinal metaplasia using no more than two band ligation mucosectomies per session.
Methods
Patients
Between May 2009 and December 2014, consecutive patients undergoing EMR for biopsy-proven high grade dysplasia (HGD) or early esophageal cancer in Barrett’s esophagus were prospectively audited in a database and enrolled into this study. Endoscopic ultrasound was routinely carried out in all patients with visible nodules of more than 1 cm size. Patients with endosonographically detected infiltration of the muscularis propria or obvious lymph node involvement on EUS, CT or PET-CT were excluded. All patients eligible for esophageal endoscopic resection were discussed and agreed at the Upper Gastrointestinal Multidisciplinary Team (MDT) meeting.
The study adheres to the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all patients. Patients were informed in detail about the risks and benefits of the endoscopic treatment and surgical and endoscopic alternatives.
The observational nature of the study was established with the Health Research Authority and Trust R & D department. The study was therefore registered locally in accordance with Trust clinical governance guidelines.
Standard protocol for endoscopic mucosal resection (EMR) and follow-up
After a fasting period of at least 4 hours, esophagogastroduodenoscopy was performed by an interventional endoscopist or a directly supervised clinical fellow using high definition white-light endoscopy (Olympus Evis Lucera processor, GIF H260 and GIF 1T140, Olympus, Tokyo, Japan) under conscious sedation with intravenous midazolam and fentanyl. The length of the Barrett’s segment was reported according to the Prague classification 12, visible lesions were described based on the Paris endoscopic classification. The position of nodules was reported by distance from the incisors and using the clock face in neutral position of the endoscope.
Acetic acid staining (1.5 v/v%) and narrow-band imaging (NBI) were routinely applied to improve the visualization and delineation of neoplastic lesions. Targeted biopsies and Seattle protocol biopsies were taken. Biopsies and EMR specimens were examined by two expert gastrointestinal histopathologists according to the Vienna classification system of esophageal neoplasia 13.
Endoscopic mucosal resection of visible nodules and for Barrett’s eradication was performed using the band ligation technique (Duette Multiband Mucosectomy Kit, Cook Ireland Limited, Limerick, Ireland) and therapeutic endoscopes (Olympus). The endocut® setting of the diathermy unit (ERBE VIO300D; ERBE Elektromedizin, Tübingen, Germany) was used for the endoscopic resection. A maximum of two band ligation resections was performed per endoscopic session and overlapping resections were avoided when possible. All patients were discharged the same day after 1 to 2 hours of observation. Patients were advised to continue proton pump inhibitors twice daily for the duration of endoscopic treatment.
The histology of the staging EMR was reviewed and discussed at the MDT and patients were considered for surgery if the resected specimen showed esophageal adenocarcinoma with positive deep resection margins or high risk features for locally advanced disease (submucosal infiltration, lymphovascular invasion or poor differentiation). Patients with high grade dysplasia or intramucosal adenocarcinoma with negative deep resection margins were considered suitable for further endoscopic therapy. Patients with only superficial infiltration of the submucosa (< 500 μm; T1b sm1) were offered surgery or endoscopic treatment after explaining the risk of lymph node infiltration of about 2 – 8 % 14 15 16.
After initial endoscopic resection of visible nodules, endoscopies with the option for further resections of the Barrett’s epithelium aiming at complete remission of intestinal metaplasia were repeated 3-monthly for 1 year.
If no dysplasia was detected on biopsies, then the interval was extended to 6 months thereafter. When complete remission of dysplasia and intestinal metaplasia had been achieved, patients underwent annual endoscopic surveillance.
Patients with residual columnar lined epithelium after four sessions of endoscopic resection and follow-up of more than 12 months were considered for radiofrequency ablation unless they had severe comorbidities significantly reducing their life expectancy.
Argon plasma coagulation was only allowed for tiny Barrett’s islands of less than 2 mm diameter.
The presence of residual Barrett’s epithelium was assessed visually using NBI inspection and histologically by taking quadrantic biopsies.
Adverse events
When attending the follow-up endoscopies, patients were routinely asked whether adverse events such as hematemesis, melena, and dysphagia had occurred since the last endoscopy.
Dysphagia was assessed using a validated dysphagia score – 0: able to eat conventional diet, 1: able to eat some solid meal, 2: able to eat semisolid but not solid food, 3: able to drink fluids only, 4: aphagia 17.
Strictures were defined as dysphagia score ≥ 1 or the need for endoscopic dilatation.
Outcome parameters
Study end points were:
(1) The rate of complete remission of intestinal metaplasia, high grade dysplasia and malignancy post completion of endoscopic therapy as well as the rate of complete eradication of the Barrett’s epithelium after a follow-up of at least 1 year. Complete Barrett’s eradication was defined as no visible Barrett’s epithelium using narrow-band imaging (C0M0 Prague classification).
(2) Adverse events such as bleeding, perforation or stricture rate were evaluated.
Statistics
Variables analysed included patient characteristics, histological results, and frequency of complications. Values are presented as medians with 25 % to 75 % interquartile range (IQR), and 95 % confidence intervals (CIs). P values of less than 0.05 were considered statistically significant,
Results
During the study period, 118 patients underwent staging EMR for early neoplasia in Barrett’s epithelium. Subsequently, 23 patients underwent surgery/chemotherapy due to deep submucosal or more advanced tumor stages (infiltration of the submucosa with positive deep margins), and four patients were managed conservatively due to patient fitness, comorbidities, or patient choice. The flowchart for patients is illustrated in Fig. 1.
Fig. 1.
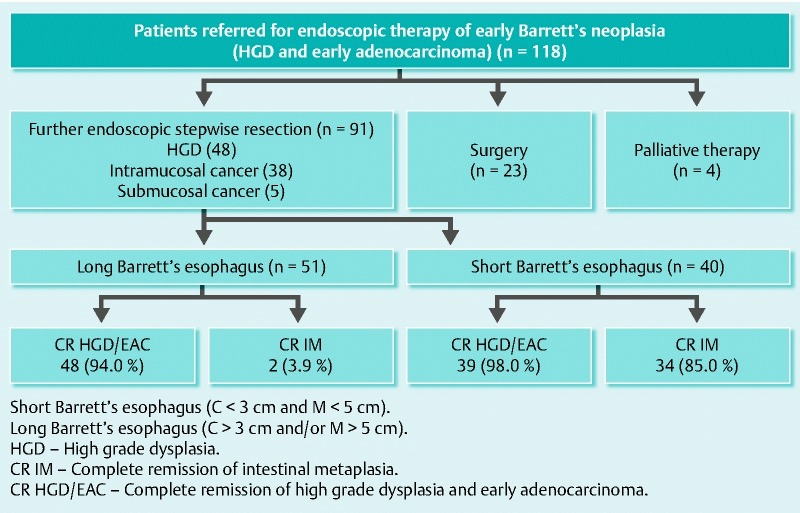
Flowchart for patients.
After reviewing the histology of the resected esophageal lesion and discussing the clinical context, 91 patients were considered suitable for further endoscopic therapy. Among the patients undergoing further endoscopic treatment, 48 patients had high grade dysplasia, 38 intramucosal cancer, and five submucosal cancer (T1sm1 defined as submucosal infiltration depth of less than 500 µm) in the endoscopically resected specimen at index endoscopy. The characteristics of the 91 patients receiving further endoscopic treatment are given in Table1. Median follow-up of the endoscopically treated patients was 30 months (IQR 16 – 52 months). Complete remission of HGD/neoplasia was achieved in 95.6 % of all endoscopically treated patients after 12 months. In four patients, high grade dysplasia or cancer was still present after 12 months: one patient with submucosal adenocarcinoma in the initial EMR specimen but unfit for surgery developed local lymphadenopathy and was treated with chemoradiotherapy. One patient with multifocal high grade dysplasia in a long Barrett’s segment suffered a hemorrhagic stroke and further endoscopic treatment was subsided. In a patient with completely resected short Barrett’s segment, a focus of intramucosal cancer was found in a residual 3 mm Barrett’s island after 12 months and completely resected endoscopically. A fourth patient with intramucosal cancer and multifocal high grade dysplasia in a long Barrett’s segment still had focal high grade dysplasia on biopsies. He underwent radiofrequency ablation after endoscopic resection of all visible nodules.
Table 1. Characteristics of patients selected for stepwise endoscopic resection of high grade dysplasia and early esophageal cancer in Barrett’s esophagus (n = 91).
| Sex, M/F | 73/18 (80.2 %/19.8 %) |
| Mean age (SD), years | 71 (11) |
| Median circumferential length (C in Prague classification) (IQR), cm | 4 (1 – 6) |
| Median maximal length (M in Prague classification) (IQR), cm | 6 (3 – 8) |
| Short Barrett’s esophagus (C < 3 cm and M < 5 cm), n (%) | 40 (43.9) |
| Histology HGD, n (%) Intramucosal cancer, n (%) Submucosal cancer, n (%) |
48 (52.7) 38 (41.8) 5 (5.5) |
| Median follow-up (IQR), months | 30 (16 – 52) |
Stepwise endoscopic Barrett’s resection resulted in complete Barrett’s eradication in 36 patients (39.6 %) in a mean of four sessions.
From the patients with remaining Barrett’s epithelium after 1 year, 31 patients with long segment Barrett’s esophagus subsequently underwent radiofrequency ablation.
Short Barrett’s esophagus
In total, 40 patients (44.0 %) had a short circumferential Barrett’s segment (C < 3 cm, M < 5 cm according to the Prague classification); the median circumferential length was 1 cm (IQR 1 – 2 cm), and the median maximal length of columnar lined epithelium was 3 cm (2 – 3 cm).
In this group, repeated EMR achieved complete remission of intestinal metaplasia in 85.0 % in a median of four EMR sessions (IQR 1 – 5). In one patient who had high grade dysplasia in the initial staging EMR, an intramucosal cancer was detected in a 3 mm Barrett’s island after 12 months follow-up (metachronous cancer) and this was subsequently completely resected. Complete remission of high grade dysplasia and early cancer was accomplished in 98.0 % of the subgroup of patients with short segment Barrett’s esophagus.
In seven patients with short Barrett’s esophagus, additional argon plasma coagulation was applied to ablate small Barrett’s islands of less than 2 mm.
Adverse events
All patients were discharged on the same day after endoscopic resection. One patient reported dysphagia to solids (dysphagia score: 1) and had developed a mild stricture (1.1 %) which was dilated with a balloon in one endoscopic session.
No perforations were observed in the total of 333 EMR sessions.
Immediate bleeding requiring endoscopic intervention during the procedure occurred in 7.1 % of patients. Intraprocedural bleeding was successfully stopped in all these patients by heater probe, hemoclips, adrenalin injection or soft-coagulation using the snare tip.
One patient with a long Barrett’s segment who was taking warfarin for atrial fibrillation developed delayed bleeding 10 days after endoscopic resection and was readmitted with melena and a drop in hemoglobin of 20 g/L. The bleeding from a resection ulcer had already stopped spontaneously at the time of endoscopy.
Discussion
The incidence of esophageal adenocarcinoma is increasing. Due to advanced endoscopic imaging techniques and improved surveillance programs for Barrett’s esophagus, detection of early esophageal neoplasia such as high grade dysplasia and intramucosal cancer has become more frequent. The recommended standard treatment for such early esophageal neoplastic alterations in Barrett’s epithelium is endoscopic resection of visible lesions followed by radiofrequency ablation of the columnar lined epithelium. Ablation of the residual Barrett’s esophagus is advised due to the high risk of metachronous cancer of about 20 % 1 18. Using these combined endoscopic treatment modalities, complete remission of dysplasia is obtained in 83 – 100 % and complete remission of intestinal metaplasia in 76 – 96 % of patients (Table 2).
Table 2. Outcome of endoscopic resection followed by radiofrequency ablation in the literature.
| Authors | n | Complete remission of dysplasia, % | Complete remission of intestinal metaplasia, % |
| Shaheen et al. (2009) 3 | 127 | 90 | 77 |
| Pouw et al. (2010) 6 | 52 | 100 | 96 |
| Alvarez Herrero et al. (2011) 19 | 26 | 83 | 79 |
| Van Vilsteren et al. (2011) 4 | 22 | 96 | 96 |
| Kim et al. (2012) 5 | 65 | 94 | 88 |
| Bulsiewicz et al. (2013) 7 | 244 | 87 | 80 |
| Haidry et al. (2015) 2 | 515 | 88 | 76 |
In contrast to radiofrequency ablation which is a tissue destroying ablation method, endoscopic resection for Barrett’s ablation provides the important advantage of histological assessment and more accurate staging. It can also detect occult synchronous cancer which might have been missed despite careful endoscopic inspection with advanced imaging methods.
Previous studies have reported high stricture rates for radical endoscopic resection of Barrett’s epithelium; when four or five mucosal resections were performed in the same endoscopic session, the stricture rate was unacceptably high at 48 – 88 % 4 19 20 (Table 2; 2 3 4 5 6 7 19). Performing only three resections per session showed lower stricture rates of 33 % 21 22. If complete endoscopic resection of a short Barrett’s segment (C < 3 cm, M < 5 cm) is achieved in a radical approach within a median of two EMR sessions, the proportion of patients requiring dilatation of a stricture was 36.8 % 23.
In our cohort, the stricture rate after non-radical stepwise endoscopic resection was very low (1/91; 1.1 %) and multiple dilatations were not required. We did not observe a high complication rate as reported for radical complete endoscopic resection in other studies (Table 3; 4 10 20 21 22 23 24), and we explain our favorable outcome by the low number of resections per endoscopic session; a maximum of two band ligation resections were performed and we avoided overlapping resections when possible. If overlapping resections were required, we tended to resect more proximal or distal to the mucosal defect rather than horizontally at the same distance from the incisors. None of the resections affected more than the semi-circumference. This means that the mucosal defect in regard to the circumference was relatively small which seems to reduce the risk of stricture development. It is known that the stricture risk is highest when circumferential resection is performed. Qumseya et al. identified the number of resections in the index procedure and the size of the lesions removed as risk factors in developing a stricture 25.
Table 3. Stricture rate after endoscopic mucosal resection related to the number of resections per endoscopic session.
Other EMR studies have followed intensified protocols, offering shortened intervals for repeat EMR at 6 – 8 weeks 23. Although the optimum interval for a repeat procedure is unclear, we find that repeating 3-monthly gastroscopies/EMRs is sufficient, since it does not lead to an increased rate of metachronous cancers in short segment Barrett’s and allows the ligation ulcers to heal. However, careful inspection of the Barrett’s epithelium, preferably using narrow-band imaging and/or acetic acid chromoendoscopy is mandatory at each endoscopic session to minimize the risk of leaving neoplastic tissue behind for a further 3 months. Obviously, a less aggressive protocol which reflects the conventional follow-up intervals reduces inconvenience to the patient and the endoscopy unit’s burden.
Endoscopic mucosal resection using the band ligation technique has a favorable safety profile as also demonstrated in our study. In large cohorts, major events such as bleeding or perforation are very uncommon. As the stricture rate is very low when using only two band ligations per session, further endoscopic resection is not hindered by stenosis in later resections. We also did not encounter fibrosis after previous endoscopic resections which could render the suction of the mucosa into the attached cap difficult during subsequent band ligations.
After radiofrequency ablation, the rate of strictures requiring endoscopic dilation is also substantial and is reported to be 6 % in the American registry 26. In the UK registry, an improvement in the stricture rate after radiofrequency ablation could be observed from 9.2 % in the years 2008 – 2010 to 6.2 % between 2011 and 2013 27.
Our findings support stepwise, non-radical endoscopic resection in short segment Barrett’s esophagus as a safe, highly effective and less expensive alternative to radiofrequency ablation with an even lower stricture rate.
Within a year and up to eight endoscopic band ligation resections, 85 % of the short Barrett’s segments (C < 3 cm) could be completely eradicated endoscopically in our study. The median diameter of the resected specimen was 18 mm giving an approximate mucosal area of 2.5 cm2 when assuming a circular shape (πr 2). A typical 25 mm diameter Barrett’s esophagus of longer than C3M3 would have an approximate surface area of > 23.4 cm2 (2πr × 30 mm = 78 mm × 30 mm = 23.4 cm2). This implies that a long Barrett’s esophagus would require more than nine band ligation resections to cover the area and explains why only two (3.9 %) of the patients with longer Barrett’s segments achieved complete remission of intestinal metaplasia within four endoscopic sessions in our study.
To prevent stricture formation after extensive endoscopic resection, the use of oral steroids, the endoscopic injection of steroids or topical application of hemostatic powder or polyglycolic acid sheets have recently been suggested 28 29 30 31 32. Although these techniques seem to be promising, none of the available preventive methods is efficient and safe enough to justify recommendation for routine use in clinical practice 33.
The main limitation of our single center/single operator study is its retrospective uncontrolled design; however, complications and outcome have been continuously audited in a prospectively maintained database since 2009. It must be borne in mind that we are a tertiary center practicing advanced endoscopic imaging and interventional procedures routinely, and our results may not be replicated in every other endoscopy unit setting. However, we believe that patients with early esophageal neoplasia should be treated in high volume expert centers with multidisciplinary teams and with expertise in advanced endoscopic imaging, endoscopic treatment, minimally invasive surgery, oncology, and pathology. Randomized controlled multicenter studies with direct comparison between radiofrequency ablation and non-radical stepwise endoscopic resection in short segment Barrett’s esophagus are desirable.
To our knowledge, this is the first cohort of patients with short segment Barrett’s esophagus treated with consecutive EMR resections, with a maximum of two resections per session. This less aggressive resection protocol that we propose has not been systemically evaluated in the past.
In conclusion, stepwise, non-radical endoscopic resection is a well-tolerated, safe and effective alternative to radiofrequency ablation in short segment Barrett’s esophagus; it achieves complete remission of dysplasia and intestinal metaplasia with low complication rates. In contrast to a more radical approach with multiple resections in a single endoscopic session, the stepwise non-radical approach results in a low stricture rate.
Footnotes
Competing interests: None
References
- 1.Fitzgerald R C, di Pietro M, Ragunath K. et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut. 2014;63:7–42. doi: 10.1136/gutjnl-2013-305372. [DOI] [PubMed] [Google Scholar]
- 2.Haidry R J, Lipman G, Banks M R. et al. Comparing outcome of radiofrequency ablation in Barrett’s with high grade dysplasia and intramucosal carcinoma: a prospective multicenter UK registry. Endoscopy. 2015;47:980–987. doi: 10.1055/s-0034-1392414. [DOI] [PubMed] [Google Scholar]
- 3.Shaheen N J, Sharma P, Overholt B F. et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. NEJM. 2009;360:2277–2288. doi: 10.1056/NEJMoa0808145. [DOI] [PubMed] [Google Scholar]
- 4.van Vilsteren F GI, Pouw R E, Seewald S. et al. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett’s oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial. Gut. 2011;60:765–773. doi: 10.1136/gut.2010.229310. [DOI] [PubMed] [Google Scholar]
- 5.Kim H P, Bulsiewicz W J, Cotton C C. et al. Focal endoscopic mucosal resection before radiofrequency ablation is equally effective and safe compared with radiofrequency ablation alone for the eradication of Barrett’s esophagus with advanced neoplasia. Gastrointest Endosc. 2012;76:733–739. doi: 10.1016/j.gie.2012.04.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pouw R E, Wirths K, Eisendrath P. et al. Efficacy of radiofrequency ablation combined with endoscopic resection for barrett’s esophagus with early neoplasia. Clin Gastroenterol Hepatol. 2010;8:23–29. doi: 10.1016/j.cgh.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Bulsiewicz W J, Kim H P, Dellon E S. et al. Safety and efficacy of endoscopic mucosal therapy with radiofrequency ablation for patients with neoplastic Barrett’s esophagus. Clin Gastroenterol Hepatol. 2013;11:636–642. doi: 10.1016/j.cgh.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gray N A, Odze R D, Spechler S J. Buried metaplasia after endoscopic ablation of Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2011;106:1899–1908. doi: 10.1038/ajg.2011.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee J K, Cameron R G, Binmoeller K F. et al. Recurrence of subsquamous dysplasia and carcinoma after successful endoscopic and radiofrequency ablation therapy for dysplastic Barrett’s esophagus. Endoscopy. 2013;45:571–574. doi: 10.1055/s-0032-1326419. [DOI] [PubMed] [Google Scholar]
- 10.Alvarez Herrero L, Pouw R E, van Vilsteren F GI. et al. Safety and efficacy of multiband mucosectomy in 1060 resections in Barrett’s esophagus. Endoscopy. 2011;43:177–183. doi: 10.1055/s-0030-1256095. [DOI] [PubMed] [Google Scholar]
- 11.Pouw R E, Peters F P, Sempoux C. et al. Stepwise radical endoscopic resection for Barrett’s esophagus with early neoplasia: report on a Brussels’ cohort. Endoscopy. 2008;40:892–898. doi: 10.1055/s-2008-1077675. [DOI] [PubMed] [Google Scholar]
- 12.Sharma P, Dent J, Armstrong D. et al. The development and validation of an endoscopic grading system for Barrett’s esophagus: the Prague C & M criteria. Gastroenterology. 2006;131:1392–1399. doi: 10.1053/j.gastro.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 13.Schlemper R J, Riddell R H, Kato Y. et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–255. doi: 10.1136/gut.47.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manner H, Pech O, Heldmann Y. et al. The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc. 2015;29:1888–1896. doi: 10.1007/s00464-014-3881-3. [DOI] [PubMed] [Google Scholar]
- 15.Ancona E, Rampado S, Cassaro M. et al. Prediction of lymph node status in superficial esophageal carcinoma. Ann Surg Oncol. 2008;15:3278–3288. doi: 10.1245/s10434-008-0065-1. [DOI] [PubMed] [Google Scholar]
- 16.Liu L, Hofstetter W L, Rashid A. et al. Significance of the depth of tumor invasion and lymph node metastasis in superficially invasive (T1) esophageal adenocarcinoma. Am J Surg Pathol. 2005;29:1079–1085. [PubMed] [Google Scholar]
- 17.Knyrim K, Wagner H J, Bethge N. et al. A controlled trial of an expansile metal stent for palliation of esophageal obstruction due to inoperable cancer. NEJM. 1993;329:1302–1307. doi: 10.1056/NEJM199310283291803. [DOI] [PubMed] [Google Scholar]
- 18.Pech O, Behrens A, May A. et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008;57:1200–1206. doi: 10.1136/gut.2007.142539. [DOI] [PubMed] [Google Scholar]
- 19.Alvarez Herrero L, van Vilsteren F GI, Pouw R E. et al. Endoscopic radiofrequency ablation combined with endoscopic resection for early neoplasia in Barrett’s esophagus longer than 10 cm. Gastrointest Endosc. 2011;73:682–690. doi: 10.1016/j.gie.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 20.Pouw R E, Seewald S, Gondrie J J. et al. Stepwise radical endoscopic resection for eradication of Barrett’s oesophagus with early neoplasia in a cohort of 169 patients. Gut. 2010;59:1169–1177. doi: 10.1136/gut.2010.210229. [DOI] [PubMed] [Google Scholar]
- 21.Chung A, Bourke M J, Hourigan L F. et al. Complete Barrett’s excision by stepwise endoscopic resection in short-segment disease: long term outcomes and predictors of stricture. Endoscopy. 2011;43:1025–1032. doi: 10.1055/s-0030-1257049. [DOI] [PubMed] [Google Scholar]
- 22.Larghi A, Lightdale C J, Ross A S. et al. Long-term follow-up of complete Barrett’s eradication endoscopic mucosal resection (CBE-EMR) for the treatment of high grade dysplasia and intramucosal carcinoma. Endoscopy. 2007;39:1086–1091. doi: 10.1055/s-2007-966788. [DOI] [PubMed] [Google Scholar]
- 23.Bahin F F, Jayanna M, Hourigan L F. et al. Long-term outcomes of a primary complete endoscopic resection strategy for short-segment Barrett’s esophagus with high-grade dysplasia and/or early esophageal adenocarcinoma. Gastrointest Endosc. 2016;83:68–77. doi: 10.1016/j.gie.2015.04.044. [DOI] [PubMed] [Google Scholar]
- 24.Soehendra N, Seewald S, Groth S. et al. Use of modified multiband ligator facilitates circumferential EMR in Barrett’s esophagus (with video) Gastrointest Endosc. 2006;63:847–852. doi: 10.1016/j.gie.2005.06.052. [DOI] [PubMed] [Google Scholar]
- 25.Qumseya B, Panossian A M, Rizk C. et al. Predictors of esophageal stricture formation post endoscopic mucosal resection. Clin Endosc. 2014;47:155–161. doi: 10.5946/ce.2014.47.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li N, Pasricha S, Bulsiewicz W J. et al. Effects of preceding endoscopic mucosal resection on the efficacy and safety of radiofrequency ablation for treatment of Barrett’s esophagus: results from the United States Radiofrequency Ablation Registry. Dis Esophagus. 2016;29:537–543. doi: 10.1111/dote.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haidry R J, Butt M A, Dunn J M. et al. Improvement over time in outcomes for patients undergoing endoscopic therapy for Barrett’s oesophagus-related neoplasia: 6-year experience from the first 500 patients treated in the UK patient registry. Gut. 2015;64:1192–1199. doi: 10.1136/gutjnl-2014-308501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanaoka N, Ishihara R, Takeuchi Y. et al. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy. 2012;44:1007–1011. doi: 10.1055/s-0032-1310107. [DOI] [PubMed] [Google Scholar]
- 29.Hashimoto S, Kobayashi M, Takeuchi M. et al. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1389–1393. doi: 10.1016/j.gie.2011.07.070. [DOI] [PubMed] [Google Scholar]
- 30.Beye B, Barret M, Alatawi A. et al. Topical hemostatic powder promotes reepithelialization and reduces scar formation after extensive esophageal mucosal resection. Dis Esophagus. 2016;29:520–527. doi: 10.1111/dote.12378. [DOI] [PubMed] [Google Scholar]
- 31.Iizuka T, Kikuchi D, Yamada A. et al. Polyglycolic acid sheet application to prevent esophageal stricture after endoscopic submucosal dissection for esophageal squamous cell carcinoma. Endoscopy. 2015;47:341–344. doi: 10.1055/s-0034-1390770. [DOI] [PubMed] [Google Scholar]
- 32.Bahin F F, Jayanna M, Williams S J. et al. Efficacy of viscous budesonide slurry for prevention of esophageal stricture formation after complete endoscopic mucosal resection of short-segment Barrett’s neoplasia. Endoscopy. 2016;48:71–74. doi: 10.1055/s-0034-1392603. [DOI] [PubMed] [Google Scholar]
- 33.Barret M, Beye B, Leblanc S. et al. Systematic review: the prevention of oesophageal stricture after endoscopic resection. Aliment Pharmacol Ther. 2015;42:20–39. doi: 10.1111/apt.13254. [DOI] [PubMed] [Google Scholar]


