Abstract
Introduction
Hydatid disease is an endemic anthropozoonosis with usual localization in liver and lungs. Rarely it localizes in uncommon sites as spleen, skeleton, kidney, brain, cardiac muscle, peritoneum, sub cutis. Complications of uncommon localizations are the same that for usual ones.
Material and methods
Review of the literature on rare and atypical localization of hydatid cysts in soft tissues. Key-words used on Pub-Med [(echinococ OR hydatid) AND (soft tissue OR subcutaneous OR cutaneous)] without time limit. There were found 282 articles; 242 were excluded because of muscular or bone localizations. 40 were coherent.
Results
Different variables are taken into account: age, sex, geographic area, anatomic localization of the cyst, dimension, symptoms, signs, mobility, blood exams and specific serological tests, imaging techniques for diagnosis, existing of septa in the structure, treatment, anaesthesia, spillage, neo-adjuvant and adjuvant treatment, follow-up period, recurrent lesions.
Conclusion
It would be useful create an homogeneous and standardized collection of data of these rare and potentially life-threatening conditions in order to create guide-line of diagnostic and therapeutic process and create (or adopt) unique classification of the lesions.
Keywords: Hydatid cyst, Uncommon localizations, Subcutaneous hydatid cyst, Review
Introduction
Hydatid disease is an anthropozoonosis caused by Echinococcus species. The species involved in the disease are E. granulosus, E. multilocularis, E. oligarthrus and E. vogeli. E. granulosus is the most common responsible of cystic formation (1).
Canids are the definitive hosts in which the adult tapeworm lives inside small intestine. The eggs (gravid proglottids), scattered through faeces, are ingested by herbivores (intermediate host) during fodder, and larvae (oncospheres) are released in the small intestine. The specific conformation gives them the ability to penetrate the intestinal wall, reaching the circulatory system and potentially to land in every part of the body, usually localizing in liver (68.8–80%) and lungs (10–22.4%), where the larvae develop into hydatid cyst (metacestode). Humans represent intermediate hosts in parasite life cycle when occasionally ingest eggs. Rare localizations are represented by spleen (0.9–8%), skeleton (0.2–3%), kidney (0.4–3.7%), brain (0.4–1%), cardiac muscle (0.02–1.1%), peritoneum (2–5.2%), sub cutis (1.6%) (2, 3).
Material and methods
In order to perform a review of the literature on rare and atypical localization of hydatid cysts in soft tissues there were used key-words such as [(echinococ OR hydatid) AND (soft tissue OR subcutaneous OR cutaneous)] on PubMed, without time limit. There were found 282 articles; 242 were excluded because of muscular or bone localizations. The remaining 40 were coherent with formulated criteria, in a period from 1991 to 2014; 4 are in Turkish, 2 in French and the remaining in English.
Different variables are taken into account: age, sex, geographic area, anatomic localization of the cyst, dimension, symptoms, signs, mobility, blood exams and specific serological tests, imaging techniques for diagnosis, existing of septa in the structure, treatment, anaesthesia, spillage, neo-adjuvant and adjuvant treatment, follow-up period, recurrent lesions.
Data are often incomplete and rarely detailed. Geographic area is usually leaved out and deduced by authors’ origin.
Results
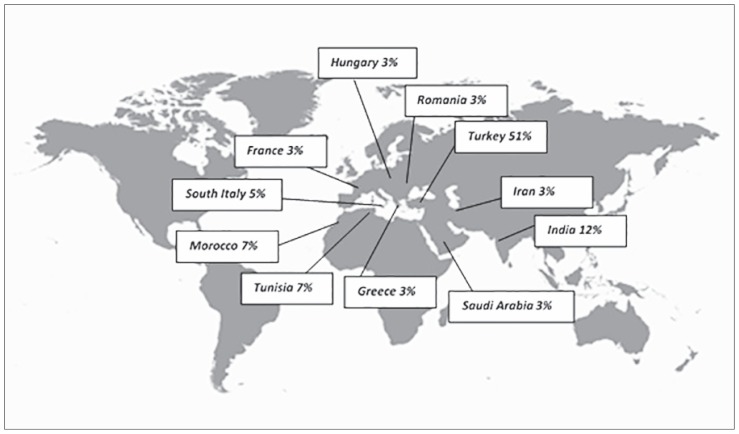
Of selected cases, 67.5% come from endemic area: 20 from Turkey, 3 from Morocco, 2 from South-Italy, 1 from Greece, 3 from Tunisia, 1 from Arabia, 5 from India, 1 from Iran, 1 from Romania and 1 from French. Only one case comes from non-endemic area: Hungary (3) (Fig. 1).
Figure 1.
Distribution of subcutaneous hydatid cyst in the world.
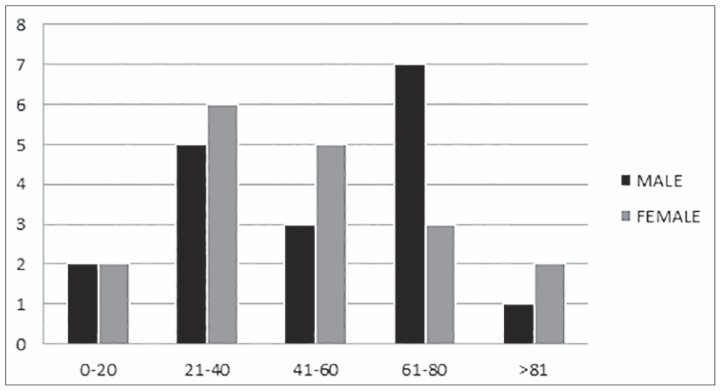
Age ranges from 7 to 84 years, median age 46.95. F/M ratio is 1.22–22 F and 18 M (Fig. 2).
Figure 2.
Age and sex distribution of subcutaneous hydatid cyst.
27.5% live in rural area, in remaining cases specific data are not available.
45% of anatomic localizations are lower limbs −77.8% thigh. 17.5% head/neck region, 10% upper limbs (armpit 3 cases, shoulder 2 cases). The remaining 30% chest and lumbar region.
Dimensions are variable from 1.1 to 35 cm, with a median of 7.85 cm.
92.5% present a visible swelling; 65% are not symptomatic, 20% with spontaneous pain (not qualitatively specified); 5% report achiness with palpation; in 10% of cases there are not enough data.
Mobility of the lesions is described in 37.5% of cases, 22.5% are described as fixed lesions, 5% as partially fixed lesions. In 35% is not specified.
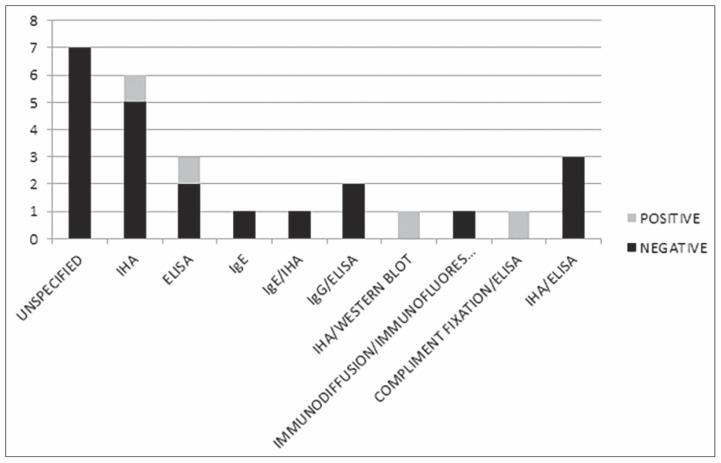
Blood exam investigations used are: ELISA, Western Blot, Immunofluorescence, Immunodiffusion, Indirect Haemoagglutination (IHA), specific IgE, specific IgG, fixation of complement. 65.5% of cases undergo serological investigations, and 19.2% of these result positive (Fig. 3).
Figure 3.
Serology.
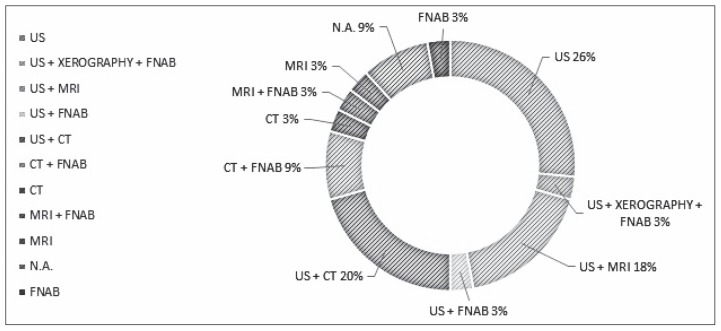
Definitive diagnosis is confirmed with a unique radiological exam as follow: US-scan – 9 cases, MRI – 1 case, CT-scan – 1 case. Some cases needed furthermore integration in radiological investigations as follow: US/MRI - 6 cases, US/CT scan – 7 cases. 50% of lesions are described with locularity – 75% with multiple septa. The remaining 50% lack of this information. In 12.5% diagnosis is completed by FNAB with 22G needle (2 cases after CT scan), 25 G (1 case after US-scan), not specified needle Gauge in 2 cases after US and CT scan (Fig. 4).
Figure 4.
Diagnostic methods.
Surgical operation in local anaesthesia is performed in all the cases unless 1 disagreement and 1 death before operation for heart failure. In 25% of cases it was used hypertonic solution during excision: 1 case with contemporary use of methylene chloride and 3 with povidone-iodine and alcohol.
Neoadjuvant treatment is mentioned in 17.5% – 87.7% with not standardized and various data on dosage and time of treatment with Albendazole; 1 case reported Mebendazole use.
Adjuvant treatment is used in 65% of patients, also when cyst is completely excised and no spillage is reported. It was administered Albendazole 10–15 mg/Kg/die with a median period of treatment of 72.2 days. Period of treatment is not always specified nor posology.
Follow-up time is variable from 3 to 72 months with a median of 18.73, and specified in only 25 case reports.
26 patients are mentioned as negative for relapse during follow-up time; only one patient had 2 relapses during a follow-up time of 10 months. No data are available for remaining 13 cases.
Discussion
Hydatid disease is an anthropozoonosis caused by Echinococcus species; humans represent intermediate hosts in parasite life cycle when occasionally ingest eggs through contaminated food or water (3, 4).
The shell of eggs’ parasite opens thanks to acidity of upper gastrointestinal tract. Oncospheres so released in small bowel penetrate the intestinal wall, and are carried out through portal circulation in liver. Crossed out portal filter, they could potentially reach every organ. Otherwise it is hypothesized lymphatic drainage of the oncospheres, inhalation of contaminated air and direct inoculation after trauma or bug’s sting as alternative ways of infection and uncommon localization of the disease (4, 5). One case reports a bee sting as possible responsible of transmission (6); inoculated eggs could find optimal pH condition in order to open the shell thanks to lactic acid and acid hydrolase of muscles production after trauma and inflammation (6). It could be supposed an alternative modality of diffusion through a co-prophagus bee after faeces contamination on a skin lesion. The hypothesis of direct contamination in absence of circulation diffusion is confirmed by serological negativity in 80.8% (7, 9, 12, 14–16, 19–22, 24–27, 30, 31, 34, 37, 39).
Another compatible hypothesis is the primitive hepatic localization with spontaneous resolution but with systemic diffusion of the parasite and positivity of serological exams (5, 8, 13, 17, 18).
The analysis of anatomic data shows the main implication of the thigh (7–16) and then of the glutei (5, 17–19), axilla (20–22), back (23–34), head/neck (26, 35–39), and limbs (12, 37). Skin trauma or bee sting or major blood flux of these anatomical sites can justify this localization (28).
Cysts are mostly asymptomatic, so that patients are often examined after clinical evidence of mass or vague symptoms. This presentation justifies the delay on diagnosis and the lack of data on the possible real moment of the infection.
Diagnosis is confirmed by clinical evidence, anamnestic data such as epidemiology and radiological support. US could be identified as gold standard. WHO classification (20, 23) was made in order to classify liver disease; only in three cases it was suggested for uncommon localizations and could be useful to standardize it in every possible localization.
CT scan and MRI often offer the possibility to better define anatomic relations.
Gold standard treatment is the total excision of the cyst, avoiding its rupture and spillage; anaphylactic shock is the major risk connected. No related complications to surgical operation are mentioned in the selected cases.
In the cases where spillage is mentioned, aspiration and using of hypertonic solution (10 minutes of direct contact) was performed. Iodopovidone, when used after cyst removal, seems to be not related with minor recrudescence incidence.
Recrudescence is mentioned in only two cases, after surgical excision, preceded by FNAB that could have disseminate the parasite (40), even though no detailed informations are provided by the articles mentioned. One of the two cases reports both neo- and adjuvant treatment with Mebendazole, whose use benefit is unknown, less useful drug than Albendazole (40, 41) for the high liver metabolism and less absorption after eating (42); it needs longer time of administration and its efficacy is altered by dosage, age of the cyst, patient’s compliance.
The gold-standard drug to administer in adjuvant therapy is the Albendazole, with 10–15 mg/kg/die dosage, for at least 1 to 6 months.
Neo-adjuvant treatment is rarely reported.
Conclusions
Subcutaneous localization of hydatid cyst is a rare condition also in endemic areas.
This diagnostic hypothesis could be considered in all subcutaneous localization of masses (6, 43, 44).
The EBM shows absence of treatment protocol for primitive subcutaneous localizations of hydatid disease, not standardized data in pharmacological neo-adjuvant/adjuvant therapy. Could be useful to propose an analytic collection of data with the goal proposed - age, sex, geographic area, anatomic localization, dimensions, clinic presentation, imaging diagnosis with extension of WHO classification for liver disease for uncommon localizations, pre- and post-operative treatment with specification on dosage, duration of administration, follow-up time, recrudescence rate. Could be desirable to create a standardized panel of data collection in order to give a unique guideline in treatment of this rare condition but with possible dangerous complications. The data now available are few and not homogeneous at all. The suggestion to use the WHO classification for hydatid liver disease could be useful in order to give a unique valid classification of the lesions.
References
- 1.Salamone G, Licari L, Randisi B, Di Carlo P, Tutino R, Falco N, Augello G, Raspanti C, Cocorullo G, Gulotta G. A primary subcutaneous hydatid cyst in the thigh A case report. Ann Ital Chir. 2016 Apr 8;:87. pii: S2239253X16024324. [PubMed] [Google Scholar]
- 2.Salamone G, Tutino R, Atzeni J, Licari L, Falco N, Orlando G, Gulotta G. Liver hydatidosis: reasoned indications of surgical treatment. Comparison between conservative and radical techniques. Retrospective study. Ann Ital Chir. 2014;85:422–430. [PubMed] [Google Scholar]
- 3.Eckert J, Deplazes P. Biological, epidemiological, and clinical aspect of Echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17(1):107–35. doi: 10.1128/CMR.17.1.107-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golzari SE, Sokouti M. Pericyst: the outermost layer of hydatid cyst. World J Gastroenterol. 2014 Feb 7;20(5):1377–8. doi: 10.3748/wjg.v20.i5.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Carlo P, Di Vita G, Guadagnino G, Cocorullo G, D’Arpa F, Salamone G, Salvatore B, Gulotta G, Cabibi D. Surgical pathology and the diagnosis of invasive visceral yeast infection: two case reports and literature review. World J Emerg Surg. 2013 Sep 26;8(1):38. doi: 10.1186/1749-7922-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Battyany I, Andrea L, Nagy KK. Subcutaneous hydatid cyst in the popliteal fossa at the site of a previous wasp sting. Diagn Interv Radiol. 2011 Jun;17(2):163–5. doi: 10.4261/1305-3825.DIR.2933-09.1. [DOI] [PubMed] [Google Scholar]
- 7.Sipahioğlu S, Koçarslan S, Zehir S. Primary hydatid cyst in the medial thigh: case report. Eklem Hastalik Cerrahisi. 2014 Dec;25(3):168–72. doi: 10.5606/ehc.2014.36. Turkish. [DOI] [PubMed] [Google Scholar]
- 8.Almadani N, Almutairi B, Alassiri AH. Primary subcutaneous hydatid cyst with palisading granulomatous reaction. Case Rep Pathol. 2013;2013:126541. doi: 10.1155/2013/126541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A, Singal RP, Gupta S, Singal R. Hydatid cyst of thigh diagnosed on ultrasonography - a rare case report. J Med Life. 2012 Jun 12;5(2):196–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Săvulescu F, Iordache II, Hristea R, Dumitru C, Sandru AM, Bălaşa G, Pătruţoiu R, Yazyi M, Iordache C. Primary hydatid cyst with an unusual location-a case report. Chirurgia (Bucur) 2010 May-Jun;105(3):419–22. [PubMed] [Google Scholar]
- 11.Ozkan HS, Sahin B. Primary hydatid disease of subcutaneous tissue in the leg. Clin Exp Dermatol. 2010 Dec;35(8):915–6. doi: 10.1111/j.1365-2230.2010.03843.x. [DOI] [PubMed] [Google Scholar]
- 12.Dirican A, Unal B, Kayaalp C, Kirimlioglu V. Subcutaneous hydatid cysts occurring in the palm and the thigh: two case reports. J Med Case Rep. 2008 Aug 13;2:273. doi: 10.1186/1752-1947-2-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parsak CK, Eray IC, Sakman G, Eray SI, Gumurdurlu D, Akcam T, Parsak CK. Hydatid disease involvement of primary subcutaneous tissue in the posterior proximal thigh--an unusual localization. Int J Dermatol. 2008 Apr;47(4):417–8. doi: 10.1111/j.1365-4632.2008.03387.x. [DOI] [PubMed] [Google Scholar]
- 14.Bagatur AE, Uğur F, Zorer G. Primary giant hydatid cyst in the thigh. Acta Orthop Traumatol Turk. 2002;36(1):72–5. Turkish. [PubMed] [Google Scholar]
- 15.Chevalier X, Rhamouni A, Bretagne S, Martigny J, Larget-Piet B. Hydatid cyst of the subcutaneous tissue without other involvement: MR imaging features. AJR Am J Roentgenol. 1994 Sep;163(3):645–6. doi: 10.2214/ajr.163.3.8079861. [DOI] [PubMed] [Google Scholar]
- 16.Giuffrè G, Tuccari G. Hydatid cyst in soft tissues diagnosed by fine needle aspiration cytology. Cytopathology. 1994 Feb;5(1):55–9. doi: 10.1111/j.1365-2303.1994.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 17.Gürbüz B, Baysal H, Baysal B, Yalman H, Yiğitbaşı MR. Isolated gluteal hydatid cyst. Turkiye Parazitol Derg. 2014;38(1):51–4. doi: 10.5152/tpd.2014.2682. Turkish. [DOI] [PubMed] [Google Scholar]
- 18.Steurer S, Auer H. Primary cystic echinococcosis in the subcutaneous gluteal region - a case report. Wien Klin Wochenschr. 2008;120(19–20 Suppl 4):101–3. doi: 10.1007/s00508-008-1039-9. [DOI] [PubMed] [Google Scholar]
- 19.Daoudi A, Loudiyi WD, Elibrahimi A, Elmrini A, Chakour K, Boutayeb F. Solitary subcutaneous hydatid cyst of gluteal area: an unusual localisation. A case report. Ann Chir Plast Esthet. 2008 Oct;53(5):448–51. doi: 10.1016/j.anplas.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Zangeneh M, Amerion M, Siadat SD, Alijani M. Primary hydatid cyst of the axillary region: a case report. Case Rep Med. 2012;2012:362610. doi: 10.1155/2012/362610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yagmur Y, Akbulut S. Unusual location of hydatid cysts: a case report and literature review. Int Surg. 2012 Jan-Mar;97(1):23–6. doi: 10.9738/CC85.1. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ozsoy M, Keles C, Kahya M, Keles G. Primary echinococcal cyst in the axillary region. J Infect Dev Ctries. 2011 Nov 15;5(11):825–7. doi: 10.3855/jidc.1589. [DOI] [PubMed] [Google Scholar]
- 23.Duman A, Yetişgin A, Tosun A, Ekiz T. Primary Subcutaneous Hydatid Cyst Presenting With Low Back Pain. PM R. 2014 Oct 4; doi: 10.1016/j.pmrj.2014.09.016. pii: S1934-1482(14)01414-2. [DOI] [PubMed] [Google Scholar]
- 24.Demir G, Tekin A, Tekin H. Diagnosis and excision of a primary hydatid cyst localized in the soft tissue. Rev Soc Bras Med Trop. 2014 Jul;47(4):537. doi: 10.1590/0037-8682-0058-2014. [DOI] [PubMed] [Google Scholar]
- 25.Haşlak A, Uysal E. Left lumbar subcutenous hydatid cyst disease: a case report. Turkiye Parazitol Derg. 2014;38(1):55–7. doi: 10.5152/tpd.2014.3113. Turkish. [DOI] [PubMed] [Google Scholar]
- 26.Ay S, Okuş A, Demirgül R, Eryılmaz MA, Atay A. Primary subcutaneous cyst hydatid: presentation of two cases. Turkiye Parazitol Derg. 2013;37(3):219–21. doi: 10.5152/tpd.2013.49. [DOI] [PubMed] [Google Scholar]
- 27.Burgazli KM, Ozdemir CS, Beken Ozdemir E, Mericliler M, Polat ZP. Unusual localization of a primary hydatid cyst: a subcutaneous mass in the paraumbilical region. Eur Rev Med Pharmacol Sci. 2013 Jul;17(13):1766–8. [PubMed] [Google Scholar]
- 28.Vecchio R, Marchese S, Ferla F, Spataro L, Intagliata E. Solitary subcutaneous hydatid cyst: review of the literature and report of a new case in the deltoid region. Parasitol Int. 2013 Dec;62(6):487–93. doi: 10.1016/j.parint.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 29.Jarboui S, Hlel A, Daghfous A, Bakkey MA, Sboui I. Unusual location of primary hydatid cyst: soft tissue mass in the supra-clavicular region of the neck. Case Rep Med. 2012;2012:484638. doi: 10.1155/2012/484638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ousadden A, Elbouhaddouti H, Ibnmajdoub KH, Mazaz K, Aittaleb K. A solitary primary subcutaneous hydatid cyst in the abdominal wall of a 70-year-old woman: a case report. J Med Case Rep. 2011 Jul 2;5:270. doi: 10.1186/1752-1947-5-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sallami S, Ayari K, Oueslati B, Miladi M. Isolated subcutaneous hydatid cyst. Tunis Med. 2011 Mar;89(3):314–5. [PubMed] [Google Scholar]
- 32.Singh S, Khichy S, Singh M, Gill JS. Recurrent solitary hydatid cyst of the subcutaneous tissue. Indian J Surg. 2009 Jun;71(3):162–4. doi: 10.1007/s12262-009-0044-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta R, Mathur SR, Agarwala S, Kaushal S, Srivastav A. Primary soft tissue hydatidosis: aspiration cytological diagnosis in two cases. Diagn Cytopathol. 2008 Dec;36(12):884–6. doi: 10.1002/dc.20936. [DOI] [PubMed] [Google Scholar]
- 34.Bedioui H, Makni A, Nouira K, Mekni A, Daghfous A, Ayadi S, Rebai W, Ksantini R, Chebbi E, Fteriche F, Ammous A, Jouini M, Kacem M, Ben Safta Z. Subcutaneous hydatid cyst. Case report of an exceptional location. Med Trop (Mars) 2007 Apr;67(2):181–2. French. [PubMed] [Google Scholar]
- 35.Safioleas M, Nikiteas N, Stamatakos M, Safioleas C, Manti CH, Revenas C, Safioleas P. Echinococcal cyst of the subcutaneous tissue: a rare case report. Parasitol Int. 2008 Jun;57(2):236–8. doi: 10.1016/j.parint.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 36.Bansal C, Lal N, Jain RC, Srivastava AN, Fatima U. Primary hydatid cyst in the soft tissue of the face: an exceptional occurrence. Indian J Dermatol. 2011 Nov;56(6):768–70. doi: 10.4103/0019-5154.91852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benhammou A, Benbouzid MA, Bencheikh R, Boulaich M, Essakali L, Kzadri M. Hydatid cyst of the neck. B-ENT. 2007;3(4):201–3. [PubMed] [Google Scholar]
- 38.Ok E, Sözüer EM. Solitary subcutaneous hydatid cyst: a case report. Am J Trop Med Hyg. 2000 May;62(5):583–4. doi: 10.4269/ajtmh.2000.62.583. [DOI] [PubMed] [Google Scholar]
- 39.Oztürk S, Devec M, Yildirim S. Hydatid cyst in the soft tissue of the face without any primary. Ann Plast Surg. 2001 Feb;46(2):170–3. doi: 10.1097/00000637-200102000-00016. [DOI] [PubMed] [Google Scholar]
- 40.Teggi A, Lastilla MG, De Rosa F. Therapy of human hydatid disease with mebendazole and albendazole. Antimicrob Agents Chemother. 1993 Aug;37(8):1679–1684. doi: 10.1128/aac.37.8.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caremani M, Lapini L, Tacconi D, Giorni P, Corradini S, Giaccherini R. Sonographic management of complicated cystic echinococcosis. J Ultrasound. 2007 Dec;10(4):179–85. doi: 10.1016/j.jus.2007.09.005. Epub 2007 Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO Informal Working Group on Echinococcosi, et al. Guidelines for treatment of cystic and alveolar echinococcosis in humans. Bull World Health Organ. 1996 [PMC free article] [PubMed] [Google Scholar]
- 43.Bagga PK, Bhargava SK, Aggarwal N, Chander Y. Primary subcutaneous inguinal hydatid cyst: diagnosis by fine needle aspiration cytology. J Clin Diagn Res. 2014 Aug;8(8):FD11–3. doi: 10.7860/JCDR/2014/8692.4744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Memis A, Arkun R, Bilgen I, Ustun EE. Primary soft tissue hydatid disease: report of two cases with MRI characteristics. Eur Radiol. 1999;9(6):1101–3. doi: 10.1007/s003300050798. [DOI] [PubMed] [Google Scholar]