Abstract
Recent empirical findings have suggested the existence of a twist in the Hispanic paradox, in which Mexican and other Hispanic foreign-born migrants living in the United States experience shallower socioeconomic status (SES) health disparities than those in the U.S. population. In this article, we seek to replicate this finding and test conjectures that could explain this new observed phenomenon using objective indicators of adult health by educational attainment in several groups: (1) Mexicanborn individuals living in Mexico and in the United States, (2) U.S.-born Mexican Americans, and (3) non-Hispanic American whites. Our analytical strategy improves upon previous research on three fronts. First, we derive four hypotheses from a general framework that has also been used to explain the standard Hispanic paradox. Second, we study biomarkers rather than self-reported health and related conditions. Third, we use a binational data platform that includes both Mexicans living in Mexico (Mexican National Health and Nutrition Survey 2006) and Mexican migrants to the United States (NHANES 1999–2010). We find steep education gradients among Mexicans living in Mexico’s urban areas in five of six biomarkers of metabolic syndrome (MetS) and in the overall MetS score. Mexican migrants living in the United States experience similar patterns to Mexicans living in Mexico in glucose and obesity biomarkers. These results are inconsistent with previous findings, suggesting that Mexican migrants in the United States experience significantly attenuated health gradients relative to the non-Hispanic white U.S. population. Our empirical evidence also contradicts the idea that SES-health gradients in Mexico are shallower than those in the United States and could be invoked to explain shallower gradients among Mexicans living in the United States.
Keywords: Hispanic paradox, Biomarkers, Socioeconomic status, Mexico
Introduction
The United States is one of the industrialized nations with the highest levels of inequality in the world (United Nations 2012). Its health and mortality levels rank at the very bottom among nations of the Global North (Crimmins et al. 2011; Woolf et al. 2013), with unusually large health and mortality disparities by socioeconomic status (SES) relative to other industrialized countries (Banks et al. 2006).
Against this backdrop, two paradoxes pertaining to Hispanics, now the largest racial/ethnic group in the United States,1 present a conundrum as they challenge established notions of how SES influences health. First, a large and longstanding body of literature has pointed to the fact that Hispanics—particularly the foreign-born—experience consistently lower mortality and have better health in a variety of outcomes relative to non-Hispanic whites in the United States (Markides and Eschbach 2005; Palloni and Arias 2004). This phenomenon is known as the Hispanic health paradox (HHP).
A second, less-documented paradox is that SES disparities within the Hispanic population, and among foreign-born Mexicans in particular, appear to be weaker than those experienced by the U.S. non-Hispanic population (Buttenheim et al. 2010; Goldman et al. 2006; Kimbro et al. 2008; Riosmena and Dennis 2012).
While the evidence for the standard Hispanic paradox is compelling and has withstood ample scrutiny (Elo et al. 2004; Markides and Eschbach 2005; Palloni and Arias 2004; Riosmena et al. 2013), the facts and conjectures about the weak SES-health gradient among foreign-born Hispanic and Mexicans living in the United States are less clear. Recent investigations of contrasts between SES gradients in these two subpopulations are few, include a number of inconsistencies and contradictory findings, and are hampered by important shortcomings. Prior research suggests that weak SES-health gradients among migrants may mirror those in sending countries rather than being the result of the migration experience. Thus, flat gradients among Hispanic and Mexican foreign-born migrants in obesity and smoking may simply reproduce the sending country patterns that lag behind those experienced by the U.S. population (Buttenheim et al. 2010; Riosmena and Dennis 2012). Shallower gradients in self-reported health status or self-reported conditions may be the outcome of self-reports distorted by cultural idiosyncrasies or differential health perceptions by SES (Breen et al. 2010; Goldman et al. 2006; Jurkowski and Johnson 2005; Kimbro et al. 2008). With few exceptions (Crimmins et al. 2005; Turra and Goldman 2007), extant empirical research has yet to document equally weak migrants’ SES gradients in more objective chronic conditions or mortality.
Furthermore, recent empirical research has yet to identify unambiguously and test empirically for mechanisms that either produce different health gradients, however measured, or that blunt them either permanently or temporarily. With the exception of two studies on obesity and smoking (Buttenheim et al. 2010; Riosmena and Dennis 2012), there has been no systematic attempt to empirically identify the mechanisms that shape SES-health gradients. Scarce evidence is available from comparisons of gradients among Mexican migrants residing in the United States and those residing in Mexico, and even less is known about how disparities evolve over time and with duration since migration. These contrasts are the central line of attack for hypotheses verification and constitute the first place to search for explanations.
Finally, very limited information is available on the nature of SES gradients, if any, among the Hispanic and Mexican migrant populations in the United States and those residing abroad. Do they reflect mechanisms that operate after migration takes place, such as differential adaptation to the United States? Are they the product of other postmigration SES-graded processes, such as differential selection in return migration? Or do they truly only reflect conditions that precede migration?
In this article, we extend and improve prior research on health of Hispanic migrants by examining the SES gradients of Mexican immigrants in the United States and of comparable adult populations residing in Mexico. We use biomarkers of chronic health conditions that define the metabolic syndrome (MetS) and a binational perspective based on a data set from the United States and one for Mexico. This article contains three contributions. First, we derive unambiguous hypotheses about health gradients in migrant and nonmigrant populations from an overarching framework employed to account for the standard Hispanic paradox. Second, we use data that enable us to contrast gradients between Mexican migrants living in the United States and the U.S. non-Mexican resident population as well as between Mexican migrants living in the United States and those in Mexico. Third, we focus on objective indicators or biomarkers of health status. Although these data have their own limitations, they provide a sturdier ground on which to anchor inferences about health status of populations rather than conventional self-reported health status and conditions.
Hypotheses
To formulate testable hypotheses, we build on recent research on the standard Hispanic paradox (Palloni and Arias 2004) and consider extensions of those hypotheses. The extensions are needed because we aim to compare gradients in two countries and thus must consider potential migration effects in the places of both origin and destination. Table 1 contains a summary of these hypotheses.2 They are presented in the following subsections.
Table 1.
The Hispanic paradox and its expected link with SES gradients in health
| Hispanic Paradox Explanations | Expected Health Outcome for Mexican Migrants Living in the United States vs. Non-Hispanic Whites |
Expected SES Gradients in Health Outcomes for Immigrants to the United States vs. Nonmigrants in Mexico |
|---|---|---|
| SES-Selective Immigration | Better health |
|
| Negative Return Migration | Better health |
|
| Cultural Adaptation | ||
| Protective Lifestyles | Better health only for those with short duration |
|
| Social Support/Social Networks | Similar health to non-Hispanic whites for longer duration |
|
SES-Selective Immigration
One mechanism that partially accounts for the standard Hispanic paradox is immigration selection, whereby Mexican migrants into the United States are selected for better health (Riosmena et al. 2013; Rubalcava et al. 2008). Health selection among immigrants will influence SES-health gradients observed among migrants living in the United States and those in the country of origin only to the extent that the magnitude of health selection at origin varies by SES. In fact, if there are substantial SES differences in health selection of migrants to the United States, they could produce gradients at destination that are indistinguishable from those that would be generated anyway if the Mexican epidemiological and nutritional transitions lag behind that of the United States.
Were immigration health selection to operate equally among members of different SES in the population of origin, we would observe that gradients among foreign-born migrants living in the United States are similar to those in the country of origin (although their premigration health would differ). The fact that Mexican migrants tend to be either slightly (positively) selected in terms of SES (Chiquiar and Hanson 2005; Feliciano 2005; Orrenius and Zavodny 2005), or (as more recent evidence suggests) slightly negatively selected (Rendall and Parker 2014), would not play a role as long as their SES status does not change after migration. If so, we should observe similar SES-specific health outcomes for immigrants in the United States and nonmigrants in Mexico, and the observed health advantage of immigrants would be a reflection of their (premigration) SES selectivity.
However, if health selection is stronger among lower-SES migrants (Turra and Goldman 2007), the gradient among foreign-born migrants in the United States will be shallower than the one observed in the country of origin and weaker than the one observed in the non-Hispanic white population in the United States. Conversely, the SES-health gradients in Mexico will increase, particularly in places where the outflow of migrants is large and originates disproportionately in the lower-SES population. In contrast, if migration flows into the United States are highly health-selective irrespective of SES, then the SES gradient among Mexican migrants and those abroad will be attenuated.
Health selection of immigrants generates the following expectations:
Hypothesis 1a: It will lead to the standard Hispanic paradox.
Hypothesis1b: If the size of health selection is higher among low-SES migrants than among migrants occupying more privileged SES positions, it will lead to (1) shallower SES gradients among Mexican migrants to the United States than among Mexicans residing in Mexico and (2) a contraction of the difference between gradients among Mexican migrants to the United States and the SES gradient in the nonmigrant U.S. population.
Hypothesis 1c: If the flow of Mexican migrants into the United States represents a sizable fraction of the total adult Mexican population, heavy SES differences in health selection of migrants at the point of migration will flatten the SES gradients in Mexico.
Hypotheses 1a and 1b suggest that shallower SES gradients in Mexico can be expected even in the absence of lags in the Mexican epidemiological transitions (Goldman et al. 2006; Smith and Goldman 2007) because the gradients can plausibly be accounted for the process of Mexican migration itself.
SES Selection of Return Migrants
Return migration to Mexico of older and unhealthier Mexican migrants living in the United States (Palloni and Arias 2004; Riosmena et al. 2013; Turra and Elo 2008) can also influence the SES gradients. As before, the total effect will depend on the strength of return migrants’ health selection by SES. If the relation is weak—for example, if health-selective return migration occurs across the board—then both the gradient among migrants remaining in the United States and those returning to the country of origin will be unchanged. However, if health-selective return migration is heavier among those with low SES, the SES-health gradient among migrants remaining in the United States will be reduced, whereas the one observed abroad will be reinforced. This may indeed lead to the appearance of a shallower SES gradient among Mexican migrants residing in the United States but should sharpen SES gradients in Mexico (in proportion to the size of the return migrant population).
Health selection of return migrants generates the following expectations:
Hypothesis 2a: It partially contributes to the standard Hispanic paradox but mostly at older adult ages (Palloni and Arias 2004; Riosmena et al. 2013; Turra and Elo 2008).
Hypothesis 2b: If the size of health selection among return migrants is higher among low-SES migrants than among migrants occupying more privileged SES positions, it will (1) produce shallower SES gradients among Mexican migrants residing in the United States than among Mexicans residing in Mexico (mostly at older adult ages) and (2) contract the difference between SES-health gradients among Mexican migrants residing in the United States and the SES gradient in the nonmigrant U.S. population (mostly at older ages).
Hypothesis 2c: As a result of Hypothesis 2b, age plays an important role: the force of health selection of return migrants should pivot health gradients to age disparities in gradients of Mexican migrants in the United States. Thus, net of duration of stay (as explained later), it must result in shallower gradients among Mexican older migrants residing in the United States than among their younger counterparts.
Hypothesis 2d: If the outflow of Mexican return migrants represents a sizable fraction of the total older adult population in Mexico, heavy SES differences in health selection of return migrants will sharpen considerably the SES-health gradients in Mexico.
SES-Graded Health Protection and Erosion Mechanisms: Cultural Adaptation
Some of the mechanisms identified earlier refer to processes that take place at or before the time of immigration. They are silent on the role of experiences after individuals migrate and take up residence in the United States. SES-health gradients of migrants residing in the United States may shift over time as a result of their exposure to new residential patterns, insertion into social networks, occupational hazards, and adoption of new behaviors. In large part, these phenomena fall within the territory of research on acculturation or adaptation effects—an area generally given short shrift by research on the Hispanic paradox because data sources that are suitable to assess the Hispanic paradox are unsuitable to deal with acculturation. Although this article is not an exception to this problem, we stretch the empirical evidence as far as it can go and consider the role of duration of residence and language use and their relation to health indicators.
Compelling evidence suggests that Mexican immigrants could experience social conditions with beneficial health influences. In particular, Mexican Americans tend to have strong social networks of support (Viruell-Fuentes et al. 2013), which may buffer them from adversities and could reduce the likelihood of engaging in behaviors with negative health effects. Furthermore, at the outset, Mexican migrants may adhere to behaviors that minimize exposure to health risks. This is particularly true of smoking (Blue and Fenelon 2011) but could conceivably extend to other domains, including alcohol consumption, substance abuse, and unhealthy diets. Conversely, evidence also suggests that the Mexican migrant population in the United States experiences health deterioration over time (Goldman et al. 2014;Riosmena et al. 2013), including some that is unlikely to be driven by acculturative behaviors (Riosmena et al. 2015a).
However, the aforementioned mechanisms are irrelevant unless they operate differentially by SES, which can happen in two ways. First, lower-SES Mexican migrants may gain more from social networks and adhere better to healthy behavioral profiles they brought with them (Cagney et al. 2007), which should flatten SES gradients among migrants residing in the United States relative to SES gradients in the nonmigrant U.S. population but not necessarily when compared with SES gradients in Mexico. Second, if high-SES Mexican migrants to the United States acculturate more rapidly and adopt high-risk behaviors (e.g., diet, smoking, alcohol) more readily than those in low socioeconomic positions, the SES-health gradients among Mexican immigrants should become shallower with longer duration of residence in the United States than both those in the United States and in Mexico. Conversely, if acculturation brings larger net health benefits to high-SES migrants, then SES disparities among Mexican migrants to the United States will increase with duration of residence and could be even larger than those in the country of origin.
Cultural adaptation generates the following expectations:
Hypothesis 3a: Shallower SES gradients are expected among Mexican migrants living in the United States than among those living in Mexico when migrant acculturation is associated with negative health benefits and is faster among high-SES Mexican migrants.
Hypothesis 3b: Shallower SES gradients are expected among Mexican migrants living in the United States than among the nonmigrant U.S. population if low-SES migrants experience advantageous protective effects from social networks and healthy behavioral profiles.
Health Indicators and SES Metric
Why Use the Metabolic Syndrome (MetS) as a Marker of Health Status?
To test the aforementioned hypotheses, we examine biomarkers of the metabolic syndrome (MetS): namely, lipid levels (high triglycerides and low high-density lipoprotein (HDL) cholesterol), high plasma glucose, obesity, waist circumference, and blood pressure (diastolic and systolic) (Table 2).
Table 2.
Definition of the metabolic syndrome and its components
| Health Indicator | Definition |
|---|---|
| Obese | BMI ≥ 30 |
| Triglycerides | ≥150 mg/dL |
| Low-HDL Cholesterol (“good cholesterol”) | <40 mg/dL in men <50 mg/dL in women |
| High Plasma Glucose (“diabetes status”) | ≥100 mg/dL |
| High Blood Pressure or Taking Medications | Systolic ≥130 mmHg Diastolic ≥85 mmHg |
| High Waist Circumference | ≥102 cm in men ≥88 cm in women |
| Metabolic Syndrome (MetS) | ≥3 high-risk factors |
Source: Alberti et al. (2009).
In the absence of an accepted indicator of global health, MetS is the best alternative because it is a strategic measure of epidemiological studies of adult health. MetS comprises indicators that capture dimensions responsible for an increasing toll of ill health and death. Because of substantial heterogeneity among individuals in the stages of metabolic syndrome, the composite measure is always useful as a way to reduce distortions associated with composition by variance of stages in MetS.
Even though the United States and Mexico are at different stages in their health transitions, they share exposure to a number of characteristics that move them toward convergence. Such characteristics include changes in diet and physical activity, which are both behaviors that are partly responsible for shifting the health profiles of populations worldwide. Future prospects of health status and mortality in the United States and elsewhere will depend quite heavily on the trajectory of MetS, as will the nature and magnitude of gradients across groups in the socioeconomic hierarchy. In addition, MetS is a powerful predictor of type 2 diabetes (T2D) and prospective circulatory, heart, and kidney disease, which are the most prominent killers in populations with pervasive metabolic dysfunction. Examining MetS and its components separately may shed light on mechanisms producing gradients because we know that some of them, such as obesity, cholesterol, and T2D, are quite different among immigrants relative to U.S.-born populations (Beltrán-Sánchez et al. 2013; Riosmena et al. 2015b).
A caveat, however, is that few studies have used MetS to study contrasts of health status between migrant and nonmigrant populations;3 to our knowledge, our study is the first to use MetS in a binational study. Precisely because of its novelty, we lack knowledge about the comparability of protocols in order to assess MetS across countries. And although the protocols are standard and should be followed identically everywhere, no study has assessed the degree of cross-country concordance.
Why Use Education as a Marker of SES?
A study of SES gradients among foreign-born migrants is complicated by the fact that the migration experience itself has short- and long-run impacts on SES, rendering measured SES a misleading indicator. In general, when the goal is to compare SES gradients between immigrant populations living in other countries and the populations of origin, using occupation, family income, or an even more stable quantity (such as assets)—all traits that are altered by the act of migration itself—is not advisable. Furthermore, scattered evidence indicates that some of these indicators (e.g., assets, income) are poorly measured among immigrants (Cobb-Clark and Hildebrand 2006). Finally, identifying comparable classes of income (or assets) across different countries is difficult, if not impossible.
A solution to these difficulties is to use an indicator that is less likely to change with the act of migration itself, more easily and better measured, and flexible enough for maximum comparability. Adult educational attainment is perhaps the best indicator available. In addition, schooling appears to discriminate well among groups of individuals on unmeasured traits thought to reflect membership in different social classes or strata, which explains its widespread use in disparate areas (e.g., fertility, mortality, migration, marriage and divorce, family organization). Finally, focusing on schooling as an SES indicator also allows us to compare our findings with those of prior work, which has almost invariably used this indicator.
Data, Measures, and Methods
Data
We use the Mexican National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutrición, ENSANUT) in 2006 for Mexico, as well as six cross-sectional surveys of the National Health and Nutrition Examination Survey (NHANES) from 1999–2000 to 2009–2010 for the United States.
The adult ENSANUT 2006 is a nationally representative sample of the Mexican population aged 20 and older; it includes 45,241 individuals, of whom 11,249 randomly selected individuals provided blood samples. We eliminated 210 people with missing values in education who were, on average, significantly older. We additionally eliminated 2,691 people with missing values in glucose, high-density lipoprotein (HDL) cholesterol, and total cholesterol, thus leaving a sample of 8,348 individuals. Two-tailed t tests show that those with missing biomarker data are significantly older (both among males and females) and, among females only, have significantly lower mean education levels. Additionally, in order to use plasma glucose levels, we restricted the sample to those who fasted more than 8 hours, thus eliminating 755 people. The final analytical sample contains 7,593 individuals, or 69 % of the original subsample with biomarkers. Statistical tests show no significant differences by age or education between the fasting and nonfasting sample.4
The NHANES is a nationally representative and cross-sectional survey. Each of the six cross sections that we use consists of an independent sample of close to 10,000 individuals belonging to about 6,000 households selected using stratified multistage sampling procedures. We pooled six cross sections from 1999–2000 to 2009–2010, including 9,975 individuals aged 20 or older who self-reported as being Mexican foreign-born (n = 1,835), U.S.-born Mexican American (n = 1,233), or U.S.-born non-Hispanic white (n = 6,907). We excluded respondents who fasted fewer than 8 hours (n = 739) and those whose fasting status was unknown (n = 189), leaving a sample of 9,047 eligible individuals (1,674 Mexican foreign-born, 1,107 U.S.-born Mexican American, and 6,266 non-Hispanic white). We additionally restricted the sample to those with complete information on the relevant variables of interest (e.g., glucose, cholesterol, triglycerides, blood pressure, and waist circumference), leading to a final analytic sample of 8,364 people (92.5 % of eligible sample): 1,530 Mexican foreign-born, 1,043 U.S.-born Mexican American, and 5,791 non-Hispanic whites.5
Measures
We examine three sets of health outcomes: individual components of the metabolic syndrome (MetS), the MetS summary index, and anthropometric data for body mass index (BMI). Epidemiologic evidence shows that several cardiometabolic risk factors often co-occur in patients at high risk of cardiovascular disease (CVD), such as abdominal obesity, dyslipidemia, elevated blood pressure, impaired fasting glucose, and insulin resistance (Eckel et al. 2005). Together, these markers define the so-called metabolic syndrome. The MetS identifies individuals at increased risk for CVD, T2D, and all-cause mortality (Ford 2004; Malik et al. 2004). We constructed the MetS using six high-risk factors consistent with the most recent harmonized definition of MetS from 2009 (Table 2) (Alberti et al. 2009). Survey respondents who had three or more of the individual components were defined as having MetS. We created a dichotomous (0/1) variable for each component as well as for the summary index. BMI is estimated as weight divided by height squared, and obesity is defined as a binary variable taking the value of 1 if BMI equals or exceeds 30.
Our model specification uses education as an indicator of SES. Because of large differences in educational attainment between Mexicans and the U.S. population, we use different educational classifications. In ENSANUT, we distinguish three education groups: low education (0 to 6 years), medium education (7–11 years), and those with higher education (completed high school or more). For Mexican foreign-born respondents in NHANES, we use similar educational groups as in ENSANUT based on conditionally imputed educational attainment from the National Health and Interview Survey;6 for U.S.-born Mexican Americans and non-Hispanic whites, we define low education as those without a high school diploma (or GED), medium education as those with a high school diploma or GED, and higher education as those with college or more.
Imputation of exact number of years of education among Mexican migrants interviewed in NHANES is not an ideal strategy for establishing optimal comparability between non-Hispanic whites and Mexican migrants living in the United States. Despite the problems that such a strategy may generate, however, it is highly unlikely to produce systematic biases. First, the imputation is conditional on observed educational class (see footnote 7). Second, using the original education categories (in the absence of imputation) leads to similar results and inferences (Online Resource 1, section B).
Methods
We estimate separate logistic models for all health outcomes. Although we test several specifications, we discuss only two of them. All models control for age using two dummy variables for age groups 20–29 and 50+, with those aged 30–49 as the reference category. When the male and female samples are pooled, we use a dummy variable to control for gender (with males as the reference group). We consider secondary model specifications, adding interaction terms of education with age and gender (Online Resource 1, section C), and also explore models that include duration of residence in the United States (Online Resource 1, section D) as well as language spoken at home (Online Resource 1, section E). Interaction effects and models including duration stretch the data and limit our ability to preserve power in hypotheses testing. However, in some cases, they are useful to gauge potential effects of acculturation differences across SES groups (duration of residence) and return migration of the least healthy (age and sex). We also explore interactions of SES and gender because we expect that migration selectivity (if present) as well as acculturation may be different for men and women. Although we also estimate models controlling for mediating behaviors (smoking, drinking, physical activity, etc.), our substantive results remain unchanged. Thus, we report results from only models without those controls because our interest is to assess the magnitude of the gradient, and not to explain it away.
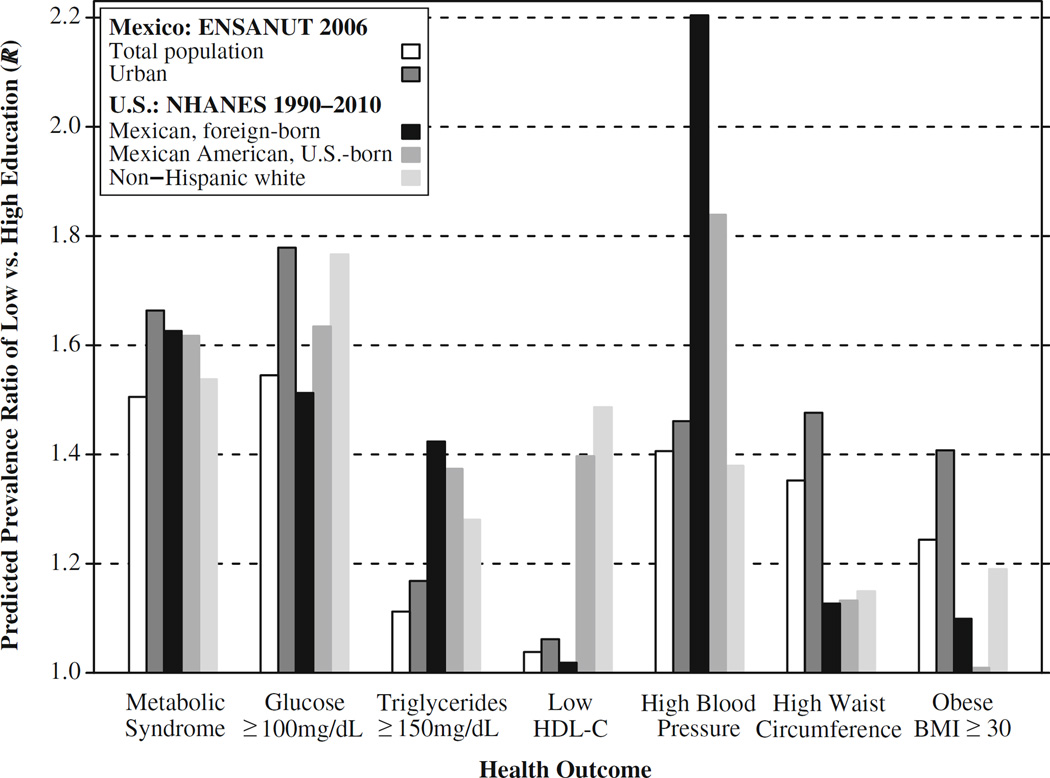
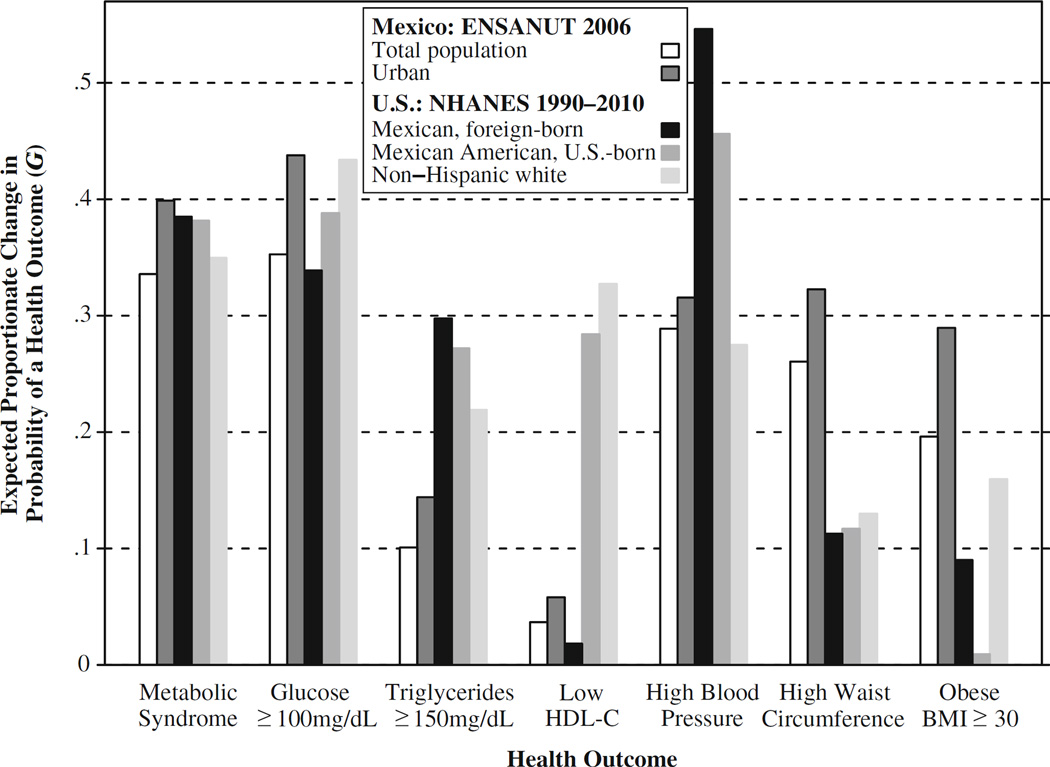
We use three metrics for the size of education health gradients. We first estimate effects of the education dummy variables on the log odds of an outcome. However, comparisons of estimated effects on log odds of prevalence for a health outcome across subsamples are influenced by the size of differentials in the levels of prevalence of the disease in each subsample. To circumvent this problem and to establish consistency with previous research, we propose two additional indicators. First we compute ratios (R) of predicted prevalence of an outcome in the lowest education to the predicted prevalence in the highest education group. These are shown in Fig. 1. Second, to provide a better sense of the implications of the gradients, we compute the expected proportionate change in the probability of having a negative health outcome relative to the maximum change possible induced by shifting educational attainment. This quantity is defined as G = (P(L) – P(M)) / P(L), where P(·) are the predicted probabilities of experiencing the health outcome among males (females) in the age group 30–49, M stands for either medium or high education (depending on which of these two has the minimum value of P(.)), and L stands for the lowest level of education. The steeper the observed education gradient, the closer G should be to a value of 1. Thus, G is the fraction of the total change possible (from P(L) to 0) that could be achieved if everybody in the low-education category experienced the same prevalence as those in the highest.7 A graphic display of these ratios of actual to maximum possible changes is shown in Fig. 2.
Fig. 1.
Predicted prevalence ratio of an outcome in the lowest education to the predicted prevalence in the highest education group (R). Predicted probabilities estimated from models in Table 4. Source: NHANES 1999–2010 and ENSANUT 2006
Fig. 2.
Predicted fraction of the total change possible in each outcome that could be achieved if everybody in the low education category experienced the same prevalence as those in the highest education group. G = (R – 1) / R; estimates of R are shown in Fig. 1. Source: NHANES 1999– 2010 and ENSANUT 2006
Results
Descriptive Statistics
Basic descriptive statistics for key variables in the analyses appear in Table 3. We use the following acronyms: NHW for U.S.-born non-Hispanic whites; MA for U.S.-born Mexican Americans; MFB, Mexicans foreign-born; MxU for Mexicans residing in urban Mexico; MxR for Mexicans residing in rural Mexico; and Mx for Mexicans residing in urban or rural areas.
Table 3.
Sample characteristics of people aged 20 or older in the United States and Mexico: NHANES 1999–2010 and ENSANUT 2006
| Mexico |
United States |
||||
|---|---|---|---|---|---|
| Total Population (Mx) N = 7,593 |
Urban (MxU) N = 4,819 |
Mexican Foreign-born (MFB) N = 1,530 |
U.S.-born Mexican American (MA) N = 1,043 |
Non-Hispanic White (NHW) N = 5,791 |
|
| Female (%) | 62.4 | 62.7 | 50.2 | 55.0 | 50.8 |
| Age (%) | |||||
| 20–29 | 20.9 | 21.4 | 24.3 | 20.6 | 14.4 |
| 30–49 | 47.4 | 47.7 | 41.0 | 29.7 | 30.8 |
| 50+ | 31.7 | 30.9 | 34.6 | 49.7 | 54.8 |
| Education (%) | |||||
| Low | 61.1 | 51.7 | 51.4 | 35.7 | 16.9 |
| Medium | 24.8 | 28.5 | 35.5 | 22.7 | 27.6 |
| High | 14.1 | 19.8 | 13.1 | 41.6 | 55.5 |
| Health Indicators (%) | |||||
| Metabolic syndrome (MetS) | 35.0 | 36.7 | 29.2 | 37.9 | 28.8 |
| High glucose | 21.4 | 23.0 | 22.5 | 27.5 | 21.1 |
| High triglycerides | 27.3 | 28.3 | 41.0 | 41.8 | 34.2 |
| Low-HDL cholesterol | 75.6 | 76.1 | 36.2 | 36.1 | 29.3 |
| High blood pressure | 39.4 | 38.6 | 26.5 | 37.7 | 34.8 |
| High waist circumference | 48.0 | 50.3 | 52.8 | 63.1 | 56.0 |
| Obese | 31.3 | 33.7 | 32.6 | 40.3 | 31.2 |
Notes: Education in Mexico is defined as low (0–6 years), medium (7–11 years), and high (completed high school or more). Education in the United States is defined as low (no high school diploma or GED), medium (high school diploma or GED), and high (college or more). Metabolic syndrome is defined as having three or more high-risk health indicators.
The unweighted unadjusted prevalence of diabetes (high glucose)8 is similar among NHW, MFB, and MxU. Prevalence of high lipid levels (triglycerides) is higher among MFB and MA than among Mx or NHW. Mexicans in Mexico have high prevalence of low HDL cholesterol, almost twice as high as that of any of the other groups. The high prevalence of low HDL cholesterol in Mexico may be due to differences in assay procedures between the surveys, but it is highly unlikely that such discrepancies can distort SES gradients.9
High blood pressure is similar among Mx and MA, but MFB have significantly lower levels (approximately 27 %). Waist circumference and obesity prevalence are highest for MA, while the other three subpopulations are similar. On the whole, NHW and MFB have lower levels of prevalence of cardiometabolic risk (MetS) than the remaining groups, with urban Mexicans experiencing similar levels than among MA. As expected, educational level is highest among NHW, followed by MA and MxU.
Gradients
We first examine the overall MetS index, followed by its components—(1) a diabetes biomarker (glucose), (2) markers of lipids (low levels of HDL cholesterol and high levels of triglycerides), and (3) high blood pressure—all of which are three direct risk factors of cardiovascular disease. We then discuss the markers of adiposity—waist circumference and obese status—both of which are distal yet important risk factors of both diabetes and CVD. We follow this order to highlight first the biomarkers that exert more weight on the toll of ill health and mortality.
The Composite MetS Index
The composite MetS index is not only the most important of our biomarkers but it also summarizes well findings replicated in the literature. First, note in Table 4 and Fig. 1 that the effects of education on the log odds of expressing MetS are similar among MxU and MFB, slightly lower than those prevailing among MA, and about 75 % as high as those of the NHW population. However, the excess gradient among NHW is entirely due to the highest education group.
Table 4.
Coefficient estimates from logistic models associating the metabolic syndrome and its components with sex, age, and education in the United States and Mexico: NHANES 1999–2010 and ENSANUT 2006
| Health Outcome | Mexico: ENSANUT 2006 |
United States: NHANES 1999–2010 |
|||
|---|---|---|---|---|---|
| Total Population (Mx) |
Urban (MxU) | Mexican Foreign- born (MFB) |
U.S.-born Mexican American (MA) |
Non-Hispanic White (NHW) |
|
| MetS | |||||
| Female | 0.72*** | 0.58*** | 0.19 | 0.00 | –0.01 |
| Age 20–29 | –1.20*** | –1.15*** | –0.93*** | –0.59** | –0.76*** |
| Age 50+ | 0.83*** | 0.87*** | 0.98*** | 0.92*** | 0.67*** |
| Medium education | –0.05 | –0.16* | –0.29* | –0.28 | –0.05 |
| Higher education | –0.14 | –0.30** | –0.36 | –0.45** | –0.51*** |
| High Glucose | |||||
| Female | 0.02 | –0.06 | –0.48*** | –0.70*** | –0.59*** |
| Age 20–29 | –1.32*** | –1.37*** | –1.28*** | –0.87** | –1.35*** |
| Age 50+ | 0.89*** | 1.02*** | 1.17*** | 1.23*** | 1.21*** |
| Medium education | –0.06 | –0.12 | –0.27 | –0.50* | –0.15 |
| Higher education | –0.07 | –0.23* | –0.10 | –0.27 | –0.58*** |
| High Triglycerides | |||||
| Female | –0.20*** | –0.26*** | –0.09 | –0.26* | –0.12* |
| Age 20–29 | –0.67*** | –0.72*** | –0.23 | –0.18 | –0.22* |
| Age 50+ | 0.26*** | 0.30*** | 0.23 | 0.50** | 0.17** |
| Medium education | 0.07 | 0.03 | –0.20 | 0.10 | –0.01 |
| Higher education | –0.04 | –0.01 | –0.49** | –0.35* | –0.34*** |
| Low-HDL Cholesterol | |||||
| Female | 0.88*** | 0.80*** | 0.34** | 0.35** | 0.14* |
| Age 20–29 | 0.04 | 0.04 | –0.32* | 0.01 | 0.01 |
| Age 50+ | –0.16* | –0.20* | –0.11 | –0.24 | –0.32*** |
| Medium education | –0.12 | –0.23** | –0.09 | –0.47** | –0.19* |
| Higher education | –0.14 | –0.24* | –0.05 | –0.63*** | –0.63*** |
| High Blood Pressure | |||||
| Female | –0.38*** | –0.40*** | –0.47*** | –0.20 | –0.20*** |
| Age 20–29 | –0.71*** | –0.70*** | –1.26*** | –1.34*** | –0.78*** |
| Age 50+ | 1.05*** | 1.09*** | 1.75*** | 1.43*** | 1.40*** |
| Medium education | –0.10 | –0.07 | –0.37* | –0.07 | 0.14 |
| Higher education | –0.15 | –0.20* | –0.55* | –0.51** | –0.30*** |
| High Waist Circumference | |||||
| Female | 1.91*** | 1.74*** | 1.92*** | 0.93*** | 0.64*** |
| Age 20–29 | –0.88*** | –0.83*** | –0.74*** | –0.24 | –0.59*** |
| Age 50+ | 0.52*** | 0.52*** | 0.53*** | 0.44** | 0.48*** |
| Medium education | 0.01 | –0.15 | –0.15 | 0.03 | –0.08 |
| Higher education | –0.19* | –0.37*** | –0.24 | –0.19 | –0.26*** |
| Obese | |||||
| Female | 0.62*** | 0.54*** | 0.77*** | 0.06 | 0.05 |
| Age 20–29 | –0.66*** | –0.67*** | –0.49** | –0.13 | –0.45*** |
| Age 50+ | –0.10 | –0.14 | 0.17 | –0.20 | 0.00 |
| Medium education | –0.01 | –0.18* | –0.13 | –0.19 | –0.10 |
| Higher education | –0.18* | –0.38*** | –0.10 | –0.07 | –0.24** |
Notes: Education in Mexico is defined as low (0–6 years), medium (7–11 years), and high (completed high school or more). Education in the United States is defined as low (no high school diploma or GED), medium (high school diploma or GED), and high (college or more).
p < .05;
p < .01;
p < .001
As shown in Table 3, the overall level of the MetS is lower among MFB than among MxU (p value = .000) and almost identical to that in NHW (p value = .752), even though MFB education is more unfavorable than among NHW. This confirms the existence of a Hispanic paradox and, jointly with the contrasts of effects of education on predicted prevalence of MetS (Table 4), suggests partial health selection or protection. However, if selection exists at all, its effects are not powerful (or SES-graded) enough to flatten the education health gradient of migrants (Fig. 1). Examination of the values of R, for example, shows that MFB experience SES gradients in MetS that are similar to those of MxU, while MA have SES gradients that more closely resemble those of MFB than those of the NHW population.
Diabetes
Unlike the case of MetS, the prevalence of diabetes (high glucose) among MFB (22.5 %) is very similar to that in MxU (23.0 %, p value = .719) and slightly higher than among NHW (21.1 %, p value = .214) (Table 3). Thus, we see no signs of a Hispanic paradox here. The results in Table 4 show that the pattern of effects on log odds for this indicator is similar to those associated with MetS: comparable gradients in MxU and MFB, higher among MA, and even higher for NHW. Here again, the excess gradients among NHW are almost entirely due to the influence of the highest education group.10
Predicted diabetes prevalence (Fig. 1) shows strong gradients in MxU and NHW. However, MFB manifest a weaker gradient and thus cannot be reflecting gradients in Mexico. Given that diabetes prevalence is similar across the three population groups, this pattern suggests that health selection among MFB may be stronger among those with lower SES than among those with higher SES, or that SES-graded acculturation is at play. This conclusion is also supported by results in Fig. 2, which shows that MFB have the lowest value of G.11
Low HDL Cholesterol and High Triglycerides
Both low HDL cholesterol and high triglyceride biomarkers are predictors of heart disease, but the education gradients they express could not be more different: while low HDL cholesterol is the only indicator that displays no education gradient among MFB, high levels of triglycerides are the indicator with the highest gradient in this group (Table 4)—the opposite of the MxU experience. Predicted prevalence of triglycerides confirms that MFB have the sharpest gradient, while predicted prevalence of low HDL cholesterol shows similar SES gradients for Mx and MFB (Fig. 1). Finally, the prevalence of high triglycerides is much higher among MFB, while Mx have the highest prevalence of low HDL cholesterol (Table 3). We find no traces of a Hispanic paradox in either case.
Hypertension
The pattern of gradients for hypertension is somewhat different. The estimated effects on log odds reveal a strong education gradient in the expected direction among NHW but a substantially higher one among MFB. High blood pressure has scarcely any gradient among Mx, even among MxU. Like in the case of MetS and diabetes, MFB are on average less likely to experience hypertension than NHW and their peers in Mexico (p value = .000, Table 3). In this sense, there is a Hispanic paradox for hypertension that appears jointly with indications of health selection— at least on this indicator. The predicted probability of hypertension for a MFB with the lowest educational attainment is about .36, lower than a comparable MxU (about .45) and lower than among NHW (.41). Conversely, the predicted prevalence of hypertension for the highest education group is lowest among MFB (.16) as contrasted with urban Mx (.31) and NHW (.30). These prevalence rates produce the largest SES gradients in hypertension among MFB (Fig. 1), which is exactly what we would expect if health selection among MFB is stronger among those with lower SES.
BMI and Waist Circumference
Waist circumference is very similar for Mx, MFB, and NHW, but much higher among MA (Table 3). Importantly, the education gradient among MFB does not exist, but it is very sharp among MxU (Table 4). The results for obesity are virtually identical, with stronger SES gradients among MxU.
Age and Gender Interactions
To check the possibility that the effects of SES change with age and/or gender, we estimate models for each health outcome including suitable interaction effects (Online Resource 1, section C). With very few exceptions, the only estimates that are statistically significant are those involving gender in both samples. Gender and SES interactions are negative, statistically significant, and larger (in absolute value) for the highest education group in MxU and among NHW, but not among MFB. Thus, the SES gradients are steeper for females than males in Mexico and among NHW, but not among MFB. This intriguing result suggests a stronger attenuation of the SES gradient among MFB females relative to comparable males. This outcome may be produced partly by stronger health selection among female migrants than among male migrants or, more consistent with the migrant health literature, by more intense acculturation (i.e., experience of its deleterious effects) among females (Gorman et al. 2010).
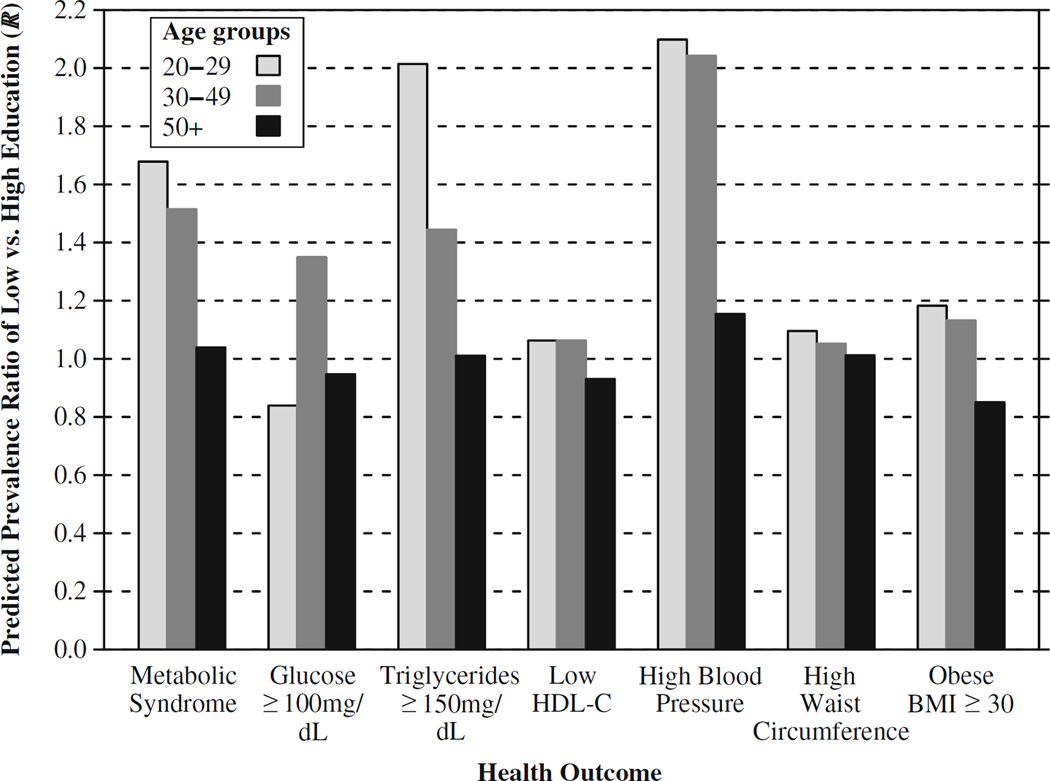
In the set of age and SES interaction terms, one estimate is statistically significant for each population subgroup, except for MFB, for whom no interactions are significant. Thus, the SES gradients previously described for MFB do not seem to differentially operate between younger and older adults. Although this result is inconsistent with the idea that SES gradients among MFB tend to decline with age, we cannot make stronger statements given that the decline is not equally expressed among those aged 50 and older (Fig. 3).
Fig. 3.
Predicted prevalence ratio of an outcome in the lowest education to the predicted prevalence in the highest education group (R) for younger (ages 20–49) and older adults (ages 50+) for Mexican foreign-born living in the United States (MFB). Predicted probabilities estimated from models with age-education interactions (Online Resource 1, section C). Source: NHANES 1999–2010 and ENSANUT 2006
Discussion
Our results are consistent with four inferences: three that are related to the SES gradient and one that is related to the standard variant of Hispanic paradox.
The First Inference
Education gradients are not uniformly shallower among MFB than among their NHW counterparts in the MetS, or in most of its dimensions, at least when contrasting the highest and lowest education groups
Most importantly, this finding applies to the summary indicator MetS, which is a strong predictor of chronic illnesses and adult mortality. Thus, the second paradox of shallower education gradients is tenuous at best. However, the observed outcome itself is relevant because it contradicts Hypotheses 1b and 2b.12
Our results suggest that the steep SES gradients in MetS are not driven by the health condition for which there is no HHP (diabetes) but rather by the health condition for which the HHP is clearest (hypertension).
The Second Inference
Education gradients among MxU in all but one biomarker (high triglycerides) are steep and sometimes steeper than those found in the United States (e.g., high waist circumference and obesity)
Additional estimates for Mexicans living in rural areas (MxR) indicate that they experience much shallower gradients across the board except for waist circumference (Online Resource 1, section F), with similar results for residents in high-migration regions in Mexico (Online Resource 1, section G). Thus, because the bulk of Mexico-U.S. migration does not originate in rural areas, this finding contradicts three hypotheses.
First, this finding goes against the conjecture that shallower or lack of education gradients among MxU could explain shallower gradients among immigrants at destinations (Goldman et al. 2006; Turra and Goldman 2007). Furthermore, the finding is inconsistent with the idea that health gradients in Mexico may be flatter because Mexico lags behind in the epidemiological transition and the effects of a number of risks (obesity, cigarette smoking, etc.) have not yet diffused to lower education groups.
Second, the empirical evidence does not support Hypotheses 1c and 2c. Because most Mexican migrants do not come from rural areas (but rather from small towns that are considered part of urban clusters) (Fussell and Massey 2004; Wong et al. 2006), the effects of their out-migration of flattening of gradients at origin according to Hypothesis 1c should not be important.13
Third, contrary to Hypothesis 2c, we find no age variability in gradients either among MFB or Mx, suggesting that at least one of the expected outcomes of health selection of return migrants is not met. The fact that disparities among MxR are flatter than among MxU is an interesting phenomenon in itself and could be due to lags in epidemiological transition or higher prevalence of behavioral conditions that promote diabetes, hypertension, and obesity among those who are better educated and live in rural areas.14
The Third Inference
Contrary to the acculturation conjecture, we find no significant age variation in the SES gradient anywhere
Age performs double duty in some of our analyses: it is an imperfect proxy for Mexican migrants’ duration of residence in the United States and a better marker to signal the onset of heavier risk of chronic conditions (see Online Resource 1, section C). However, although age may be a strong marker for health risks, it is not the best for duration of residence.
Ascertaining the role of adaptation/acculturation among Hispanic and Mexican migrants in the United States is a tough problem even using a solid measure of duration of residence and has not yet made it to the top of the agenda in the literature on the HHP. To resolve some of the ambiguities imparted by the use of age only, we stretched the data as far as possible with three auxiliary tests: (1) models by duration of residence in the MFB subsample, (2) analysis of language use, and (3) analysis of smoking.
Models by Duration of Residence in the MFB Subsample
We stratify by length of stay in the United States (<5 years, 5–9 years, 10–14 years, 15–19 years, and 20 or more years) (see Online Resource 1, section D), thus effectively separating the roles of age and duration. However, the results shed no more light than the simpler, pooled models. First, the composition of MFB by duration of stay in the United States is skewed toward short durations (34 % with <10 years and 25 % with 10–19 years), with younger migrants accounting for the majority of this group (approximately 50 % aged 20–29 and 36 % aged 30–49), while older adult migrants (ages 50+) account for most of those with 20 or more years of stay in the United States (62 %). Turra and Goldman (2007) found important drops at older ages in the SES gradients for mortality among Hispanics born abroad. This finding prompted them to invoke the idea of selection via return migration (although the finding is also consistent with increasing deleterious effects of assimilation). We find no evidence of such changes at older ages in our data for MFB, but instead we find a hint of increasing deleterious effects of acculturation.
Overall, these results are inconsistent with the existence of shifting gradients as a result of differential acculturation.
Analysis of Language Use
In lieu of duration and age, we also examine the role of language use and its influence on outcomes of interest. Arguably, language use is a better proxy for degree of proximity and access to symbols of the culture in the country of destination and thus reflects better the dimensions of acculturation that matter for health. We estimate additional models using language usage from NHANES for MFB. We use a dummy variable to identify families who speak only Spanish at home (“nonacculturated”) and distinguish them from all other respondents. Results do not suggest significant SES interactions with Spanish language spoken at home, nor do they lead to changes in previous results (see Online Resource 1, section E). Thus, we conclude that, at least when gauged by our indicator of language use, acculturation is not responsible for observed SES gradients among MFB.
Analysis of Smoking
Variability of smoking among migrants offers a unique opportunity to assess a behavior that is both strongly influential for prospective health and mortality and relatively easy (in terms of cost) to adhere to. Smoking prevalence is lower in Mexico than in the United States (Palloni et al. 2015) and appears to account for part of the adult HHP at older ages in the United States (Blue and Fenelon 2011). However, little is known about smoking-SES gradients among MFB in the United States (see Buttenheim et al. 2010; Riosmena and Dennis 2012). Because one of the possible consequences of acculturating is smoking uptake, one would expect that smoking behavior may be responsive to indicators of duration of residence in the United States and/or use of language. If this behavior could be verified, it would place the acculturation conjecture on a solid ground. To assess this possibility, we estimate models for the effects of education, gender, language, and duration of residence on smoking uptake among MFB. A sample of results is shown in Online Resource 1, section H. Briefly, these estimates show no indication of effects of variables other than gender, thus suggesting again that acculturation has limited impact on SES-health gradients among MFB.
The Fourth Inference
The standard Hispanic paradox is not confirmed for some health outcomes and is strongly verified for three key indicators: MetS, hypertension, and waist circumference
All three are predictors of adult mortality associated with cardiovascular disease. We are not the first to find that not all health outcomes behave the same. Just as the standard Hispanic paradox is stronger among older Mexican foreign-born than among other migrant subpopulations, and for mortality more than for other health outcomes, we verify here that it holds for only three of the six health outcomes.
Overall, evidence suggests that immigration health selection may be at play given that MFB have, on average, slightly better health outcomes than their Mexican counterparts. Because of the limited evidence of negative effects of duration of residence in the United States (and of acculturation, more generally), we can infer a weak version of a health selection hypothesis.
Advantages and Shortcomings of this Study
Relative to other studies in this area, ours contains important advantages. First, our research design uses comparable data on both sides of the border, enabling us to rule out the possibility that flatter SES gradients in health among Mexican immigrants are due to inherently low SES-health gradients in Mexico.
Second, we use objective health indicators related to the metabolic syndrome, not self-reported health status or conditions. This tack enables us to rule out the possibility that differences in health screening across individuals of different SES or nativity explain the gradients (or lack thereof) or that they are due to cultural idiosyncrasies.
Third, our results are robust to alternative definitions of education categories. Indeed, when we estimate models using education as reported by MFB in NHANES (instead of imputing their educational attainment), we reach similar conclusions albeit with stronger SES gradients among MFB (see Online Resource 1, section B).
The study has shortcomings. First, it is clear that the SES-health gradients among NHW are mostly due to the contrast between those with high levels of education (college or more) and those without. Even if this contrast also existed among Mexican migrants to the United States, it can hardly be detected because the distribution of migrants by education is heavily concentrated at the bottom. Identifying contrasts requires a much larger sample of migrants.
Second, although we find some evidence of immigrant health selection relative to nonmigrants in Mexico—especially in urban areas—the data available do not permit us to ascertain the exact magnitude of health selection because they do not contain precise information on duration since immigration or on levels of acculturation.
Third, as is the case for many other studies, we cannot state definitively whether our results are mostly due to positive health selection in U.S.-bound migration or negative selection in return migration to Mexico because we lack a comparison group of return migrants in Mexico. The data set that we used for Mexico (ENSANUT 2006) does not include questions related to migration history or family ties to migrants. Future research should address these issues by controlling for duration in the United States, using objective health measures prior to migration for individuals observed in the United States, and featuring comparisons of health outcomes between nonmigrants and return migrants to Mexico.
Summary and Conclusions
We contrast differences in adult health from clinically reported measures by SES observed among Mexican foreign-born living in the United States (MFB) and those living in Mexico. We use comparable data from the NHANES (1999–2010) for the United States and ENSANUT 2006 (Mexican National Health and Nutrition Survey) for Mexico. Although attenuation of SES gradients among Hispanics in the United States has been reported before, we know of no study that has compared such gradients in several important chronic health conditions to those actually experienced by the population of origin (Mexicans living in Mexico). We also use biomarkers (rather than only self-reports) to detect the presence of conditions as we do in this article.
First, our work confirms the “mixed bag” nature of Hispanic health, in which (Mexican immigrants) exhibit a sizable advantage relative to other racial/ethnic groups (e.g., hypertension and, to a much lesser extent, waist circumference), while exhibiting a disadvantage in several others (glucose, low HDL cholesterol, and obesity). These findings are consistent with prior work (e.g., Barquera et al. 2008; Riosmena et al. 2013, 2015b). Future research should explore the reasons behind the discrepancy in obesity and waist circumference, a heretofore-ignored dimension of the HHP.
In addition to these contributions, this article has provided a more in-depth view at a second HHP. Somewhat contrary to prior work showing weak SES gradients on behavioral risk factors and self-reported health assessments, we find that schooling levels—markers of the opportunity structure available to people and their actual social position—provide a portrayal of the negative consequences one might expect of the Mexican and American stratification systems. We find steep SES gradients for Mexicans living in urban areas in all but one biomarker (triglycerides), including the MetS. Although we find lesser gradients among MFB, in some conditions, they are relatively steep in most components and in the MetS.
Having said that, we do find some evidence that Mexican immigrants exhibit somewhat shallower SES gradients among in indicators such as diabetes, low HDL cholesterol, and waist circumference. Because these gradients, for the most part, do not weaken over time spent in the United States, they are unlikely to be driven by return-related attrition or even by differential adaptation to U.S. destinations according to SES. Rather, they could be partly a reflection of differential urban/rural origin across education groups. Mexican immigrants with medium and high levels of education are more likely to originate in urban areas where those with lowest levels of education could disproportionately come from rural areas. Given that rural areas in Mexico are still at earlier stages of the epidemiological transition, the presence of a relatively large group of rural migrants with no education in the United States could partly explain the flatter SES gradients (Beltrán-Sánchez and Crimmins 2013; Beltrán-Sánchez et al. 2011).
We draw two implications for future research: one relating to matters of substance and the other relating to the nature of data that must be brought to bear on the issues examined here. First, a convincing explanation of the standard Hispanic mortality paradox and extensions involving SES gradients must go beyond the conventional accounting of health and mortality disparities by SES and ethnicity. Both problems involve complex relations between health selection, return migration, and (importantly) adaptation to lifestyles in the host nation jointly with individual and collective resilience in the face of adversity. It is hard to believe that a piecemeal approach that separates the standard Hispanic paradox from the one involving gradients will lead to satisfactory results. What we need is a unifying argument that accounts for both phenomena.
Second, convincing empirical tests of these explanations require casting a wider net to include information on outcomes other than mortality and general health. Information on particular chronic conditions, biomarkers, and disability should also be brought into the mix because they may provide leverage to understand intermediate processes. Finally, progress will be slow and difficult in the absence of a binational data set that enables researchers to follow up on health trajectories in places of origin and destination and among those who stay and those who return.
Supplementary Material
Acknowledgments
Beltrán-Sánchez acknowledges support from grants by the National Institute of Child Health and Human Development (R24 HD041022) to the California Center for Population Research at UCLA. Palloni acknowledges support from grants by the National Institute on Aging (R01 G016209 and R37 AG025216) and the Fogarty International Center (FIC) training program (5D43TW001586) to the Center for Demography and Ecology (CDE) and the Center for Demography of Health and Aging (CDHA), University of Wisconsin–Madison. The CDE is funded by NICHD Center Grant 5R24HD04783; CDHA is funded by NIA Center Grant 5P30AG017266. Riosmena acknowledges research, administrative, and computing support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD)–funded University of Colorado Population Center (R24HD066613); from Grant R03HD066061 from the NICHD; and from a Poverty Center Grant awarded to the Center on Poverty and Inequality at Stanford University (Grant Number AE00101) from the U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation, and awarded by Substance Abuse Mental Health Service Administration and a sub-award (H79 AE000101-02S1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the DHHS or NIH. Wong acknowledges support from grants by the National Institute on Aging (R01 AG018016).
Footnotes
Estimates suggest that by 2050, approximately one-third (29 %) of the U.S. population will be Hispanic and approximately one-fifth (19%) will be foreign-born (Passel and Pew Hispanic Center 2005).
Although the standard HHP, as well as the more recently identified “second Hispanic paradox” of shallow SES-health gradients, seemingly apply to the Hispanic foreign-born population other than Mexicans, the strongest supporting empirical evidence comes from data for the Mexican population. In this study, we test hypotheses using data for only Mexican subpopulations.
Exceptions include Beltrán-Sánchez and Crimmins (2013), Beltrán-Sánchez et al. (2013), Crimmins et al. (2007), and Vella et al. (2011).
The ENSANUT 2006 survey sampled approximately 48,000 households, using a stratified multistage sampling procedure representative of the population at the national, urban/rural, and state levels (for further details, see Olaiz-Fernández et al. 2006). This survey collected a series of biomarkers, including blood glucose level, blood pressure, height, and weight (Barquera et al. 2010).
An extensive list of sociodemographic, biomarker, and anthropometric measures, and data protocols in NNAHES are shown elsewhere (CDC and NCHS 2012).
NHANES public data release includes only broad education categories: less than 9th grade; 9th–11th grade, including 12th grade with no diploma; high school graduate or GED equivalent; some college or associate’s degree; and college graduate or above. We use the Mexican foreign-born (MFB) population in the National Health and Interview Survey 1999–2010 to create educational categories that are comparable with those in ENSANUT. We estimated equations for the number of years of education conditional on having less than high school but more than 0 years of schooling, and used these equations to impute a category (1–6 or 7–11) among MFB in NHANES (see Online Resource 1, section A).
Clearly, G = (R – 1) / R.
We use interchangeably the terms diabetes, diabetes mellitus, and T2D to refer to high glucose levels, which is correlated albeit imperfectly with clinical diagnosis of T2D.
NHANES adjusted its HDL values for 1999–2000, 2001–2002, and 2005–2006 to account for >4 % bias relative to quality control samples resulting from changes in assay methodology. No such correction has been applied to the Mexican data. Nonetheless, any adjustment to HDL cholesterol in Mexico would have to be invariant by SES and will not alter SES gradients. Although an adjustment could alter the U.S.-Mexico comparison of levels with levels in the United States among nonmigrants and migrants alike, substantive conclusions regarding SES gradients will remain robust.
Whereas the effects of high education are statistically significant for MxU and NHW, only the effect of the medium educational level is statistically significant among MA.
G represents total change possible in prevalence of diabetes if all of those with low education experience the same prevalence as those with higher education.
Comparing levels in MetS for low-education groups between Mx and MFB shows small differences and therefore weak signs of health selection at the point of migration (results available from authors upon request).
According to the 2006 Mexican National Survey of Population Dynamics, 40 % of migrants to the United States during 2001–2006 left from communities defined as rural (<2,500 inhabitants), and 60 % left from urban areas (Riosmena and Massey 2012). Although some evidence suggests that Mexicans living in large metropolitan areas are less likely to migrate to the United States (Fussell and Massey 2004), this does not necessarily imply that the marginal distribution of migrants according to place of origin is predominantly rural—only that it may be disproportionately so relative to the Mexican rural-urban distribution.
Some evidence suggests that adoption of a Western lifestyle has occurred more rapidly among the better-educated everywhere in Mexico (Beltrán-Sánchez and Crimmins 2013; Beltrán-Sánchez et al. 2011, 2013).
Electronic supplementary material The online version of this article (doi:10.1007/s13524-016-0508-4) contains supplementary material, which is available to authorized users.
References
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA International Association for the Study of Obesity. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- Banks J, Marmot M, Oldfield Z, Smith JP. Disease and disadvantage in the United States and in England. Journal of the American Medical Association. 2006;295:2037–2045. doi: 10.1001/jama.295.17.2037. [DOI] [PubMed] [Google Scholar]
- Barquera S, Campos-Nonato I, Carrion-Rabago C, Villalpando S, Lopez-Ridaura R, Rojas R, Aguilar-Salinas CA. Methodology for the analysis of Type 2 diabetes, metabolic syndrome and cardiovascular disease risk indicators in the ENSANUT 2006. Salud Pública de México. 2010;52(Suppl. 1):S4–S10. doi: 10.1590/s0036-36342010000700003. [DOI] [PubMed] [Google Scholar]
- Barquera S, Durazo-Arvizu RA, Luke A, Cao G, Cooper RS. Hypertension in Mexico and among Mexican Americans: Prevalence and treatment patterns. Journal of Human Hypertension. 2008;22:617–626. doi: 10.1038/jhh.2008.9. [DOI] [PubMed] [Google Scholar]
- Beltrán-Sánchez H, Crimmins EM. Biological risk in the Mexican population at the turn of the 21st century. Journal of Cross-Cultural Gerontology. 2013;28:299–316. doi: 10.1007/s10823-013-9199-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltrán-Sánchez H, Crimmins EM, Teruel GM, Thomas D. Links between childhood and adult social circumstances and obesity and hypertension in the Mexican population. Journal of Aging and Health. 2011;23:1141–1165. doi: 10.1177/0898264311422255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltrán-Sánchez H, Harhay MO, Harhay MM, McElligott S. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999–2010. Journal of the American College of Cardiology. 2013;62:697–703. doi: 10.1016/j.jacc.2013.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blue L, Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: The role of smoking. International Journal of Epidemiology. 2011;40:786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen N, Rao SR, Meissner HI. Immigration, health care access, and recent cancer tests among Mexican-Americans in California. Journal of Immigrant and Minority Health. 2010;12:433–444. doi: 10.1007/s10903-008-9198-3. [DOI] [PubMed] [Google Scholar]
- Buttenheim A, Goldman N, Pebley AR, Wong R, Chung C. Do Mexican immigrants “import” social gradients in health to the US? Social Science & Medicine. 2010;71:1268–1276. doi: 10.1016/j.socscimed.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney KA, Browning CR, Wallace DM. The Latino paradox in neighborhood context: The case of asthma and other respiratory conditions. American Journal of Public Health. 2007;97:919–925. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), & National Center for Health Statistics (NCHS) National health and nutrition examination survey protocol. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Google Scholar]
- Chiquiar D, Hanson GH. International migration, self-selection, and the distribution of wages: Evidence from Mexico and the United States. Journal of Political Economy. 2005;113:239–281. [Google Scholar]
- Cobb-Clark DA, Hildebrand VA. The wealth of Mexican Americans. Journal of Human Resources. 2006;41:841–868. [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. American Journal of Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Preston SH, Cohen B National Research Council. Explaining divergent levels of longevity in high-income countries. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- Crimmins EM, Soldo BJ, Kim JK, Alley DE. Using anthropometric indicators for Mexicans in the United States and Mexico to understand the selection of migrants and the “Hispanic paradox”. Social Biology. 2005;52:164–177. doi: 10.1080/19485565.2005.9989107. [DOI] [PubMed] [Google Scholar]
- Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- Elo IT, Turra CM, Kestenbaum B, Ferguson BR. Mortality among elderly Hispanics in the United States: Past evidence and new results. Demography. 2004;41:109–128. doi: 10.1353/dem.2004.0001. [DOI] [PubMed] [Google Scholar]
- Feliciano C. Educational selectivity in U.S. immigration: How do immigrants compare to those left behind? Demography. 2005;42:131–152. doi: 10.1353/dem.2005.0001. [DOI] [PubMed] [Google Scholar]
- Ford ES. The metabolic syndrome and mortality from cardiovascular disease and all-causes: Findings from the National Health and Nutrition Examination Survey II Mortality Study. Atherosclerosis. 2004;173:309–314. doi: 10.1016/j.atherosclerosis.2003.12.022. [DOI] [PubMed] [Google Scholar]
- Fussell E, Massey DS. The limits to cumulative causation: International migration from Mexican urban areas. Demography. 2004;41:151–171. doi: 10.1353/dem.2004.0003. [DOI] [PubMed] [Google Scholar]
- Goldman N, Kimbro RT, Turra CM, Pebley AR. Socioeconomic gradients in health for white and Mexican-Origin populations. American Journal of Public Health. 2006;96:2186–2193. doi: 10.2105/AJPH.2005.062752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Pebley AR, Creighton MJ, Teruel GM, Rubalcava LN, Chung C. The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography. 2014;51:1159–1173. doi: 10.1007/s13524-014-0304-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman BK, Read JG, Krueger PM. Gender, acculturation, and health among Mexican Americans. Journal of Health and Social Behavior. 2010;51:440–457. doi: 10.1177/0022146510386792. [DOI] [PubMed] [Google Scholar]
- Jurkowski JM, Johnson TP. Acculturation and cardiovascular disease screening practices among Mexican Americans living in Chicago. Ethnicity & Disease. 2005;15:411–417. [PubMed] [Google Scholar]
- Kimbro RT, Bzostek S, Goldman N, Rodriguez G. Race, ethnicity, and the education gradient in health. Health Affairs. 2008;27:361–372. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- Malik S, Wong ND, Franklin SS, Kamath TV, L’Italien GJ, Pio JR, Williams GR. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:1245–1250. doi: 10.1161/01.CIR.0000140677.20606.0E. [DOI] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic paradox. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2005;60(Special Issue 2):S68–S75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernández S, Hernández-Avila M, Sepúlveda-Amor J. Encuesta Nacional de Salud y Nutrición 2006 [2006 National Health and Nutrition Survey 2006] Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública; 2006. [Google Scholar]
- Orrenius PM, Zavodny M. Self-selection among undocumented immigrants from Mexico. Journal of Development Economics. 2005;78:215–240. [Google Scholar]
- Palloni A, Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Palloni A, Novak B, Pinto-Aguirre G. The enduring effects of smoking in Latin America. American Journal of Public Health. 2015;105:1246–1253. doi: 10.2105/AJPH.2014.302420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel JS Pew Hispanic Center. Estimates of the size and characteristics of the undocumented population (Report) Washington, DC: Pew Hispanic Center; 2005. [Google Scholar]
- Rendall MS, Parker SW. Two decades of negative educational selectivity of Mexican migrants to the United States. Population and Development Review. 2014;40:421–446. doi: 10.1111/j.1728-4457.2014.00692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Dennis JA. Importation, SES-selective acculturation, and the weaker SES-health gradients of Mexican immigrants in the United States. Social Science Journal. 2012;49:325–329. doi: 10.1016/j.soscij.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Massey DS. Pathways to El Norte: Origins, destinations, and characteristics of Mexican migrants to the United States. International Migration Review. 2012;46:3–36. doi: 10.1111/j.1747-7379.2012.00879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Everett BG, Rogers RG, Dennis JA. Negative acculturation and nothing more? Cumulative disadvantage and mortality during the immigrant adaptation process among Latinos in the United States. International Migration Review. 2015a;49:443–478. doi: 10.1111/imre.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Root E, Humprey J, Steiner E, Stubbs R. The waning Hispanic health paradox. Pathways, Spring. 2015b Retrieved from http://web.stanford.edu/group/scspi/_media/pdf/pathways/spring_2015/Pathways_Spring_2015_Riosmena_et-al.pdf.
- Riosmena F, Wong R, Palloni A. Migration selection, protection, and acculturation in health: A binational perspective on older adults. Demography. 2013;50:1039–1064. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: New findings from the Mexican Family Life Survey. American Journal of Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Social Science & Medicine. 2007;65:1372–1385. doi: 10.1016/j.socscimed.2007.05.023. [DOI] [PubMed] [Google Scholar]
- Turra CM, Elo IT. The impact of salmon bias on the Hispanic mortality advantage: New evidence from Social Security data. Population Research and Policy Review. 2008;27:515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turra CM, Goldman N. Socioeconomic differences in mortality among U.S. adults: Insights into the Hispanic paradox. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2007;62:S184–S192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- United Nations. Trade and development report, 2012 (UNCTAD report series) New York, NY: United Nations; 2012. [Google Scholar]
- Vella CA, Ontiveros D, Zubia RY, Bader JO. Acculturation and metabolic syndrome risk factors in young Mexican and Mexican-American women. Journal of Immigrant and Minority Health. 2011;13:119–126. doi: 10.1007/s10903-009-9299-7. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Morenoff JD, Williams DR, House JS. Contextualizing nativity status, Latino social ties, and ethnic enclaves: An examination of the “immigrant social ties hypothesis”. Ethnicity & Health. 2013;18:586–609. doi: 10.1080/13557858.2013.814763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong R, Pérez ER, Martiñón LM. Una constante cambiante: La migración de la población Mexicana hacia Estados Unidos de América [A “changing constant”: Mexican Migration to the United States] College Park: University of Maryland, Maryland Population Research Center; 2006. [Google Scholar]
- Woolf SH, Aron LY National Research Council. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.