Abstract
Background
Pediatric abdominal pain visits to emergency departments (ED) are common. The objectives of this study are to assess variation in imaging [ultrasound (US) ± computed tomography (CT)] and factors associated with isolated CT use.
Methods
This was a retrospective cohort study of ED visits for pediatric abdominal pain resulting in discharge from 16 regional EDs from 2007–2013. Primary outcome was US or CT imaging. Secondary outcome was isolated CT use. We used multivariable logistic regression to evaluate patient- and hospital-level covariates associated with imaging.
Results
Of the 21,152 visits, imaging was performed in 29.7%, and isolated CT in 13.4% of visits. In multivariable analysis, black patients (OR: 0.4 (95%CI: 0.4, 0.5)) and Medicaid (OR: 0.6 (95%CI: 0.5, 0.7)) had lower odds of advanced imaging compared to white patients and private insurance, respectively. General EDs were less likely to perform imaging (OR: 0.6 (95%CI: 0.5, 0.7)) compared to the pediatric ED; however, for visits with imaging, 3.5% of visits to the pediatric ED compared to 76% of those to general EDs included an isolated CT (P<0.001). Low pediatric volume (OR: 1.8 (95%CI:1.5, 2.2)) and rural (OR:1.8 (95%CI:1.3, 2.5)) EDs had higher odds of isolated CT use, compared to higher pediatric volumes and non-rural EDs, respectively.
Conclusion
There are racial and insurance disparities in imaging for pediatric abdominal pain. General EDs are less likely than pediatric EDs to use imaging, but more likely to use isolated CT. Strategies are needed to minimize disparities and improve the use of “ultrasound-first.”
Keywords: Computed Tomography, Ultrasound, Radiation, Health Disparities, Abdominal Pain
1. Introduction
There are more than one million emergency department (ED) visits for pediatric abdominal pain each year.1 Most pediatric patients presenting to the ED with abdominal pain have benign, self-limiting conditions, however, concern for appendicitis is often the impetus for advanced imaging.2,3 Appendicitis is the most common indication for acute abdominal surgery in pediatrics4 and the second most common cause of malpractice litigation in adolescents.5 Diagnosis of appendicitis can be challenging, and advanced imaging such as ultrasound (US) and computed tomography (CT) may be performed in order to assist with diagnosis. CT is the most accurate imaging modality6; however, there are risks involved with its use, including cost, increased length of stay7 and radiation exposure8. Given the concerns regarding radiation exposure in pediatric patients9,10 and in keeping with the As Low As Reasonably Achievable (“ALARA”) principle11, ultrasound is recommended as first-line imaging for pediatric patients with abdominal complaints.5,12,13
Previous studies suggest disparities in both access to and quality of healthcare for children of different races, ethnicities, and income levels regardless of presenting complaint.14–21 Additionally, there is unexplained variation in care between different hospital types.22,23 An evaluation of practice variation provides opportunities for optimizing resource utilization and quality improvement.24,25 Thus, the objectives of this study were to assess variation in advanced imaging use for pediatric patients with abdominal pain discharged from the ED and, to further assess factors associated with isolated CT use.
2. Methods
2.1 Study Design
We performed a retrospective observational study of visits to 16 EDs within a large, regional, integrated health network from January 1, 2007 through February 28, 2013. The institutional review board at our institution approved the protocol and deemed it exempt from written informed consent.
2.2 Study Setting and Population
The health network studied consists of 15 general EDs and 1 pediatric (academic) ED within a children’s hospital, and represents the largest health system in the region. Not all hospitals contributed data for the entire time period, depending on their adoption of the electronic medical record. We included visits by patients less than 19 years of age presenting with abdominal pain and discharged from the ED. Relevant visits were identified by electronic chart review by a single reviewer from a list of all chief complaints during the time period indicating abdominal pain such as: “abdominal” or “stomach ache”, “pain” or “cramps”, “rule-out appendicitis,” and “epigastric,” “right upper quadrant,” “left upper quadrant,” “right lower quadrant,” or “left lower quadrant pain.” We excluded pregnancy- and trauma-related visits, as defined by a chief complaint or a primary International Classification of Diseases, Ninth Revision, Clinical modification (ICD-9-CM) diagnosis code related to pregnancy (640–649.4, V22, V23, V61.3–V61.9, V72.4, 633, 651, 659, and 779.6) or trauma (860–869, 902, 908.4, 958.93, and 959.12).
2.3 Study Protocol
We included the following patient-level variables: age, sex, race/ethnicity, and primary insurance. Race/ethnicity and primary insurance information are recorded in the electronic medical record by registration personnel upon ED arrival. We included those comorbidities hypothesized to be associated with the decision to perform advanced imaging as defined via ICD-9-CM coding (Crohn’s disease-DX555, Ulcerative Colitis-DX556, transplant history-DXV42, and post-operative status-DXV45 or DXV58). We report primary discharge diagnoses except when the primary diagnosis was abdominal pain (not otherwise specified); in those cases we used the 2nd–4th diagnoses codes, when included, to further specify the discharge diagnosis. We evaluated the following ED-level covariates: ED type (pediatric vs. general), ED academic status, pediatric visit volume for non-pediatric institutions, and location (large urban, small urban or rural). An academic ED was defined as one in which emergency medicine residents rotated. We calculated the mean annual pediatric visit volume for each general ED and then defined those EDs as high volume if their mean annual volume was above the median for all EDs in the study. We categorized hospital location by metropolitan statistical area size (large urban, more than 1 million persons; small urban, 1 million to 100,000 persons; rural, less than 100,000 persons or nonmetropolitan statistical area).
2.4 Measurements
The primary outcome was advanced imaging use, defined as abdominal CT, abdominal US, and/or pelvic US performed during the ED visit as extracted from billed radiology procedures during that visit. The secondary outcome, among patients who had advanced imaging use, was isolated CT use (i.e. CT without having had an US).
2.5 Data Analysis
We used descriptive statistics to summarize patient, visit, and ED demographics as well as to report the frequency of imaging use. We compared proportions using the chi-squared test. Across the study period, approximately 14% of patients had multiple ED visits during the study period. Due to the potentially correlated nature of multiple visits by the same patient, we considered using a generalized estimating equations approach, which can help to deal with correlated data. We performed multivariable modeling with a generalized estimating equations model, as well as logistic regression, to evaluate the association of patient and ED covariates on imaging use. The differences between these two types of models were small (i.e. <10% difference in odds ratios (ORs) and 95% confidence intervals (CIs) without changes in statistical significance); therefore, we report the simpler logistic regression model, which treats each visit as an independent observation.26
We constructed models for two distinct outcomes. In the first model, the dependent variable was any advanced imaging (vs. no advanced imaging) use among all EDs. To evaluate factors associated with the outcome of advanced imaging, we included candidate covariates determined a priori to be associated with advanced imaging, either through previous work or scientific plausibility.17–19,27 Candidate covariates achieving p-values less than 0.2 on univariate analysis were included in multivariable models. Next, we sought to evaluate factors associated with isolated CT use (versus US ±CT), among those who received any advanced imaging. For this outcome, we further stratified the analysis by general EDs and pediatric ED given the differences in CT use.2,17,18 There were only 8 visits by patients < 3 years that involved an isolated CT in the general EDs and no such visits in the pediatric ED, therefore, we excluded the 285 visits by patients < 3 years from the analysis of this second outcome.
We report results as odds ratios with 95% confidence intervals (CI) and considered two-sided p-values less than 0.05 to be statistically significant. We used SPSS version 23 (IBM Corp, Armonk, NY) for all statistical analyses.
3. Results
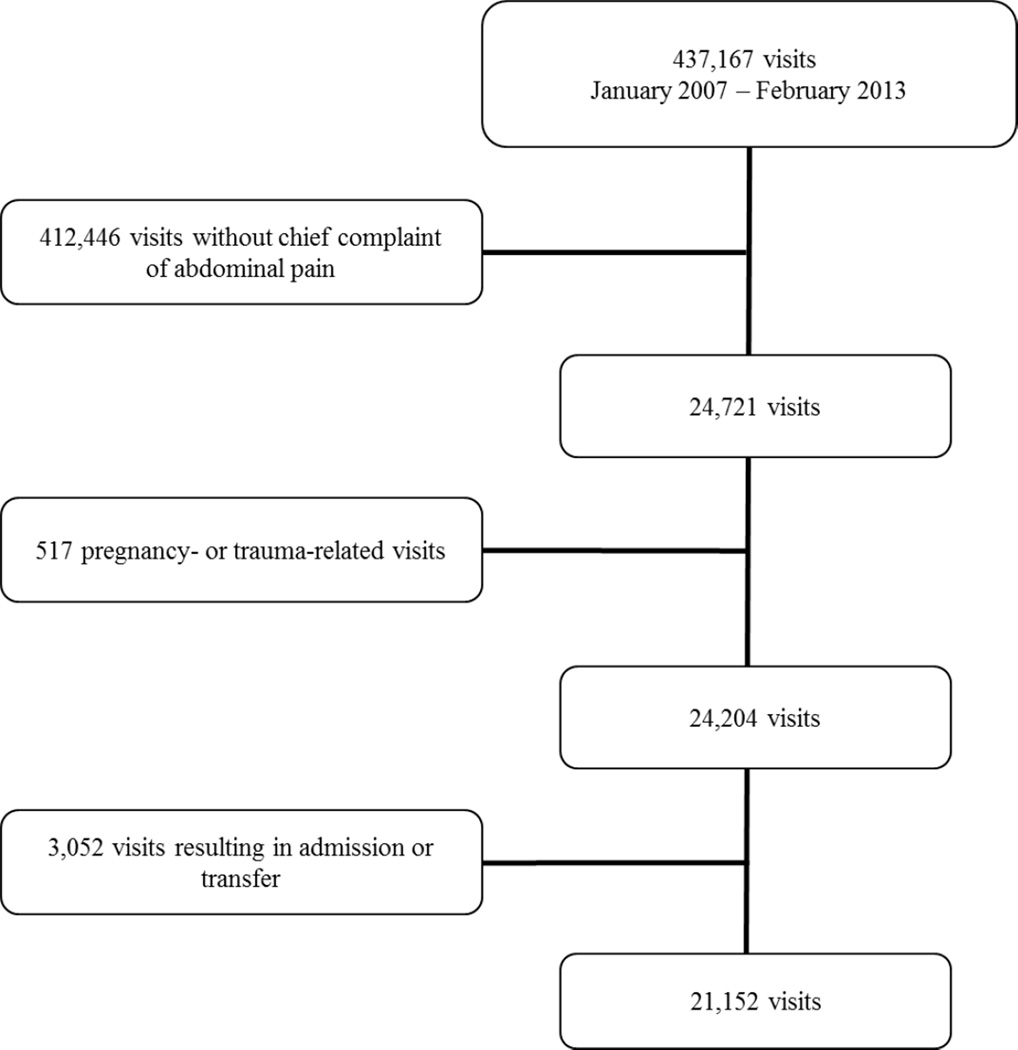
Of the 437,167 pediatric visits to EDs during the study period, 173,756 visits (39.7%) were to the pediatric ED. After excluding for pregnancy or trauma, 5.7% (24,204) of these visits were for abdominal pain, of which, 87.4% resulted in discharge from the ED (Figure 1). The final cohort included 21,152 visits by 17,540 patients. Of these, 8,715 visits (41.2%) and 7,426 patients (42.3%) were to the pediatric ED (Table 1). The median age of all patients in the cohort was 12.3 years (interquartile range: 7.0–16.7 years). Most patients were female (61.3%), white/non-Hispanic (71.3%), and privately insured (58.5%) (Table 1). The most common discharge diagnoses were abdominal pain (not otherwise specified) (24.0%) followed by constipation (15.7%), urinary tract infection (6.2%), and nausea/vomiting (6.2%).
Figure.
Flow Diagram of Study Cohort
Table 1.
Patient and visit characteristics.
| All EDs n (%) |
General EDs n (%) |
Pediatric ED n (%) |
|
|---|---|---|---|
| Patient Characteristics | (N=17,540 patients) | (N=10,114 patients) | (N=7,426 patients) |
| Age | |||
| < 3 years | 1,042 (5.9) | 362 (3.6) | 680 (9.2) |
| 3–11 years | 7,485 (42.7) | 3257 (32.2) | 4228 (56.9) |
| 12–18 years | 9,013 (51.4) | 6495 (64.2) | 2518 (33.9) |
| Sex: Female | 10,749 (61.3) | 6,670 (65.9) | 4079 (54.9) |
| Race | |||
| White/non-Hispanic | 12,498 (71.3) | 6,989 (69.1) | 5509 (74.2) |
| Black | 4,396 (25.1) | 2,731 (27.0) | 1665 (22.4) |
| Other | 646 (3.7) | 394 (3.9) | 252 (3.4) |
| Insurance | |||
| Private | 10,255 (58.5) | 5,350 (52.9) | 4905 |
| Medicaid | 6,421 (36.6) | 4,083 (40.4) | 2338 |
| Self-pay | 842 (4.8) | 663 (6.6) | 179 |
| Missing | 22 (0.13) | 18 (0.18) | 4 (0.05) |
| Comorbidity† | 176 (1.0) | 88 (0.9) | 88 (1.2) |
| Visit Characteristics | (N=21,152 visits) | (N=12,437 visits) | (N=8,715 visits) |
| Academic ED | 10,948 (51.8) | 2,233 (18.0) | N/A |
| Pediatric Volume | |||
| Low | 6,607 (53.1) | 6,607 (53.1) | N/A |
| High | 5,830 (46.9) | 5,830 (46.9) | N/A |
| Metropolitan location | |||
| Large Urban | 17,189 (81.3) | 8,474 (68.1) | N/A |
| Small Urban | 2,524 (11.9) | 2,524 (20.3) | N/A |
| Rural | 1,439 (6.8) | 1,439 (11.6) | N/A |
| Repeat Visits | 517 (2.4) | 239 (1.9) | 278 (3.2) |
| Discharge Diagnosis | |||
| Abdominal pain, not otherwise specified | 5073 (24.0) | 2941 (23.6) | 2132 (24.5) |
| Constipation | 3311 (15.7) | 1004 (8.1) | 2307 (26.7) |
| Urinary tract infection | 1307 (6.2) | 1026 (8.2) | 281 (3.2) |
| Nausea/vomiting | 1310 (6.2) | 750 (6.0) | 560 (6.4) |
| Diarrhea | 1138 (5.4) | 286 (2.3) | 852 (9.8) |
| Gastroenteritis | 854 (4.0) | 801 (6.4) | 53 (0.6) |
| Viral infection | 626 (3.0) | 409 (3.3) | 217 (2.5) |
| Menstrual /female genital organ-related | 603 (2.9) | 552 (4.4) | 51 (0.6) |
| Acute gastritis | 572 (2.7) | 399 (3.2) | 173 (2.0) |
| Ovarian pathology | 417 (2.0) | 359 (2.9) | 58 (0.7) |
| Pelvic inflammatory disease/ cervicitis/vaginitis |
413 (2.0) | 374 (3.0) | 39 (0.4) |
| Fever | 405 (1.9) | 231 (1.9) | 174 (2.0) |
| Pharyngitis | 387 (1.8) | 267 (2.1) | 120 (1.4) |
| Gastroesophageal reflux | 347 (1.6) | 174 (1.4) | 173 (2.0) |
| Upper respiratory infection | 308 (1.5) | 246 (2.0) | 62 (0.7) |
| Other* | 2141 (10.1) | 916 (7.4) | 1225 (14.1) |
| Missing | 273 (1.3) | 106 (0.9) | 167 (1.9) |
Comorbidities include Crohn’s Disease, Ulcerative Colitis, transplant history and post-operative status.
“Other” diagnoses are those responsible for <1% of the visit cohort for all EDs and include but are not limited to: headache, otitis media, renal stone, pneumonia, chest pain, dehydration, and functional digestive disorders.
Not Applicable = NA
3.1 Advanced Imaging
Of the 21,152 visits for abdominal pain resulting in discharge, 29.7% (n=6,273) included advanced imaging. Isolated CT was performed in 13.4% of visits (n=2,842). US was performed in 16.2% of visits (n=3,431) and of those, 11.3% (n=389) included both an US and CT. Among the 12,437 visits for abdominal pain to general EDs, 29.2% (n=3,635) included advanced imaging. Isolated CT was performed in 22.2% of visits (n=2,759). US was performed in 7.0% of visits (n=876) to general EDs and of those, 22.9% (n=201) included both an US and CT. In multivariable analysis (Table 2), visits by Black and other minority patients and those without private insurance had lower odds of receiving advanced imaging compared to White/non-Hispanic patients. Visits to academic EDs were at lower odds of including advanced imaging compared to non-academic EDs, as were those to general EDs compared to pediatric EDs.
Table 2.
Factors associated with any advanced imaging among visits to all EDs
| All EDs (n=21,152) |
|||
|---|---|---|---|
| Characteristics | Advanced Imaging (n=6,273) |
Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio† (95%CI) |
| Age | |||
| <3 yrs | 285 (4.5%) | Reference | Reference |
| 3–11 yrs | 1,768 (28.2%) | 0.7 (0.6–0.9) | 0.6 (0.5–0.8) |
| 12–18 yrs | 4,220 (67.3%) | 1.6 (1.4–1.9) | 1.8 (1.5–2.1) |
| Gender | |||
| Female | 4,099 (65.3%) | Reference | Reference |
| Male | 2,174 (34.7%) | 0.9 (0.8–1.0) | 1.0 (0.9–1.1) |
| Race | |||
| White/non-Hispanic | 5,094 (81.2%) | Reference | Reference |
| Black | 1,002 (16.0%) | 0.4 (0.3–0.5) | 0.4 (0.4–0.5) |
| Other | 177 (2.8%) | 0.6 (0.5–0.8) | 0.7 (0.5–0.9) |
| Insurance^ | |||
| Private | 4,258 (67.9%) | Reference | Reference |
| Medicaid | 1,773 (28.3%) | 0.5 (0.4–0.6) | 0.6 (0.5–0.7) |
| Self-Pay | 232 (3.7%) | 0.5 (0.4–0.7) | 0.6 (0.5–0.7) |
| Comorbidity | |||
| No | 6,182 (98.5%) | Reference | Reference |
| Yes | 91 (1.5%) | 1.4 (1.0–1.9) | 1.1 (0.8–1.5) |
| Repeat Visit | |||
| No | 6,076 (96.9%) | Reference | --- |
| Yes | 197 (3.1%) | 1.5 (1.2–1.8) | --- |
| Academic Hospital | |||
| No | 3,127 (50.0%) | Reference | Reference |
| Yes | 3,146 (50.2%) | 0.9 (0.8–1.0) | 0.7 (0.6–0.8) |
| Hospital Type | |||
| Pediatric | 2,638 (42.1%) | Reference | Reference |
| General | 3,635 (57.9%) | 0.9 (0.8–1.1) | 0.6 (0.5–0.7) |
| Pediatric Volume* | |||
| High | 1,698 (46.7%) | Reference | --- |
| Low | 1,937 (53.3%) | 1.0 (0.9–1.1) | --- |
| Location | |||
| Large Urban | 5,056 (80.1%) | Reference | --- |
| Small Urban | 779 (12.4%) | 1.0 (0.9–1.2) | --- |
| Rural | 438 (7.0%) | 1.0 (0.9–1.2) | --- |
Adjusted Odds Ratio listed only for factors significant on univariate analysis (p<0.2).
Insurance information was missing for 10 visits with advanced imaging.
Pediatric volume number and percentages for general EDs only (advanced imaging N=3635) as there is only 1 pediatric ED
3.2 Isolated CT imaging
Evaluating the subset of visits with advanced imaging, 3.5% of those to the pediatric ED compared to 76% of those at general EDs included an isolated CT (P<0.001). Visits by adolescents had higher odds of receiving an isolated CT at the pediatric ED compared to patients aged 3–11 years old. By contrast, adolescents had lower odds of receiving an isolated CT at general EDs compared to patients aged 3–11 years old (Table 3). Among general EDs, those with the lowest pediatric volumes and those classified as rural had higher odds of receiving an isolated CT, compared to higher pediatric volumes and non-rural location, respectively.
Table 3.
Factors associated with CT use, alone, among visits with advanced imaging to the pediatric ED and general EDs.
| Pediatric ED (N=2,367) |
General EDs (N=3,621) |
|||||
|---|---|---|---|---|---|---|
| Patient Characteristics |
CT (N=83) n(%) |
Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio† (95%CI) |
CT (N=2,751)‡ n(%) |
Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio† (95%CI) |
| Age√ | ||||||
| 3–11 yrs | 24 (28.9) | Reference | Reference | 543 (19.7) | Reference | Reference |
| 12–18 yrs | 59 (71.1) | 2.3 (1.4–3.8) | 2.9 (1.7–4.9) | 2,208 (80.3) | 0.5 (0.3–0.6) | 0.7 (0.5–0.9) |
| Gender | ||||||
| Female | 45 (54.2) | Reference | Reference | 1,773 (64.4) | Reference | Reference |
| Male | 38(45.8) | 1.4 (0.9–2.2) | 1.9 (1.1–3.0) | 978 (35.6) | 3.1 (2.5–3.9) | 2.9 (2.3–3.6) |
| Race | ||||||
| White/non-Hispanic | 75 (90.4) | Reference | Reference | 2,233 (81.2 | Reference | Reference |
| Black | 6 (7.2) | 0.4 (0.1–1.1) | 0.5 (0.2–1.2) | 441 (16.0 | 0.8 (0.6–1.0) | 0.9 (0.7–1.2) |
| Other | 2 (2.4) | 0.8 (0.1–3.2) | 1.0 (0.2–4.2) | 77 (2.8 | 1.1 (0.6–1.8) | 1.2 (0.7–2.0) |
| Insurance^ | ||||||
| Private | 69 (83.1) | Reference | Reference | 1,750 (63.6 | Reference | Reference |
| Medicaid | 12 (14.5) | 0.6 (0.2–1.1) | 0.6 (0.3–1.2) | 860 (31.3 | 1.0 (0.8–1.3) | 1.1 (0.9–1.4) |
| Self-Pay | 1 (1.2) | 0.9 (0.1–6.9) | 1.2 (0.1–9.0) | 137 (5.0 | 0.7 (0.5–1.0) | 0.8 (0.5–1.2) |
| Comorbidity | ||||||
| No | 75 (90.4) | Reference | Reference | 2,711 (98.5 | Reference | NA |
| Yes | 8 (9.6) | 7.8 (3.4–17.5) | 7.8 (3.2–18.6) | 40 (1.5) | 1.3 (0.6–2.6) | NA |
| Repeat Visit | ||||||
| No | 71 (85.5) | Reference | Reference | 2,692 (97.9) | Reference | Reference |
| Yes | 12 (14.5) | 3.9 (2.0–7.5) | 4.3 (2.1–8.6) | 59 (2.1) | 0.7 (0.4–1.1) | 0.7 (0.4–1.2) |
| Academic Hospital* | ||||||
| No | NA | NA | NA | 2,369 (86.1) | Reference | NA |
| Yes | NA | NA | NA | 382 (13.9) | 1.0 (0.7–1.2) | NA |
| Pediatric Volume* | ||||||
| High | NA | NA | NA | 1,391 (50.6) | Reference | Reference |
| Low | NA | NA | NA | 1,360 (49.4) | 0.5 (0.4–0.7) | 1.8 (1.5–2.2) |
| Location* | ||||||
| Large Urban | NA | NA | NA | 1,789 (65.0) | Reference | Reference |
| Small Urban | NA | NA | NA | 643 (23.4) | 1.7 (1.3–2.2) | 1.2 (0.9–1.6) |
| Rural | NA | NA | NA | 319 (11.6) | 1.0 (0.7–1.3) | 1.8 (1.3–2.5) |
Adjusted Odds Ratio listed only for factors significant on univariate analysis (p<0.2).
N excludes the 8 visits by patients <3 years who only received CT. Additionally, there were no visits by patients <3 years who only received a CT at the pediatric ED.
Given the small number of children <3 years with CT imaging, this age group (N=285) could not be included in these regression models
Insurance information was missing for 5 visits (1 at the pediatric ED, 4 at the general EDs) with isolated CT use
Academic hospital status, pediatric volume number and percentages are for general EDs only as there is only 1 pediatric ED which is academic, has 100% pediatric volume, and is located in a large urban area.
NA = Not applicable
4. Discussion
Our regional, multicenter ED study of pediatric visits for abdominal pain demonstrates variation in ED advanced imaging utilization across patient race/ethnicity, insurance status, and ED type. Specifically, we found that minority patients and those not privately insured were less likely to receive advanced imaging for abdominal pain. Previous studies through 2009 regarding imaging disparities for pediatric abdominal pain vary in their findings, with some indicating racial and insurance disparities,2,17 and others in conflict with these results.3 Our data support those of other national studies and provide the most recent evidence to date.2,17
The reasons for such variation in advanced imaging are likely multifactorial and due to patient and parent/guardian factors, system-level factors, as well as provider biases. For example, there may be stronger parental preference for advanced imaging among White, non-Hispanic parental/guardians. A study by Natale, et al,19 demonstrated parental anxiety/request for neuroimaging was more common for these patients. Similarly, in a survey of adult ED patients, white and privately insured patients preferred their acute problem was definitively diagnosed, such as with CT, even at the expense of more radiation.28 Patients with private insurance may initially seek care at a primary care facility and be referred to the ED specifically for further evaluation with advanced imaging, making it difficult for ED physicians to avoid imaging. Numerous studies29–34 have elucidated physician implicit pro-White bias, which contributes to racial inequities in healthcare and may have played a role in provider imaging decisions in our study.
Interestingly, our study found general EDs had 40% lower odds of advanced imaging compared to the pediatric ED. This may be due to the around-the-clock diagnostic ultrasound services available at the pediatric ED. Further, the ease of obtaining this imaging modality may lower the provider-ordering threshold.35 Although general EDs were less likely to perform advanced imaging, in cases where advanced imaging was utilized, we found these EDs were much more likely to perform an isolated CT. These findings may be the result of system-level factors that hinder or even preclude the use of an “ultrasound first” approach. Specifically, US is operator-dependent, with appendiceal visualization rates varying widely from 22%–98%36–40 and given that the majority of examinations in general EDs are performed on adult patients, it is possible that there is less accuracy and more technician discomfort with pediatric exams which would effect physician ordering practices. This notion is supported by our findings that adolescents treated at general EDs are less likely to have a CT as the primary imaging modality compared to younger patients. Our finding of higher odds of isolated CT imaging at low pediatric volume EDs further supports this notion. US availability, which may vary across hospitals35, is also likely a factor in our study. In particular, rural hospitals may not have the ability to obtain US imaging around-the-clock, and this may explain why these facilities were more likely to use CT as the primary imaging modality.
Physician-level factors likely also played a role in our findings. CT has superior accuracy compared to US and a preference for CT may indicate risk (of misdiagnosis) aversion by general emergency physicians.41 In addition, physicians may not be willing (or able) to tolerate the potential increase in lengths of stay associated with equivocal US results, in which the appendix is not visualized. In these cases, depending on the pre-test probability, physicians might order another imaging test (CT), a surgical consultation, and/or admission or transfer for observation, all of which would contribute to length of stay.
In adult patients with abdominal pain, CT is often used to evaluate for the many concerning etiologies42, however, with the exception of trauma, CT is uncommonly needed as the primary modality in the evaluation of pediatric patients.11,12 Hence, “Ultrasound First” is the recommended approach for the evaluation of pediatric patients with abdominal pain.5,12,43,44 Regardless of the reasons our data suggest that pediatric patients with abdominal pain are being evaluated in general EDs in much the same fashion as adults and given their increased radiosensitivity45, indicates a need for improvement in the radiologic evaluation of these patients.46
Mechanisms to optimize imaging strategies and decisions for pediatric patients deserve further evaluation and scrutiny. The limitations of US, such as availability and operator-dependence, deserve attention at the individual facility level and emergency physicians should advocate for improved US services for pediatric patients, as appropriate. Standardized clinical practice guidelines have been shown to reduce CT use while maintaining diagnostic accuracy.35,43,44 Several studies have investigated the use of non- and less-radiating alternatives to traditional CT imaging for pediatric appendicitis. For example, a recent study evaluated the use of MRI compared to CT after an equivocal US result and showed no difference in time to surgery, negative appendectomy rate, perforation, or length of stay.47 However, the availability of MRI use in this scenario is a limitation for many EDs. Several other studies evaluated the use of a focused right lower quadrant CT in lieu of or following an equivocal US, but have had conflicting results in the sensitivity and specificity of the focused right lower quadrant CT.48–52A final approach is in cases when decisions regarding transfer to a pediatric center have been made regardless of imaging findings (i.e. for pain management, hydration, parent/guardian request). In these cases it may be appropriate to forgo imaging and transfer to a pediatric center in order to perform advanced imaging studies.
Our study has certain limitations. First, our study used administrative data and therefore lacked clinical variables, such as measures of severity of illness. However, we limited our population to those visits resulting in discharge in order to assess a more homogenous, lower acuity population of patients with abdominal pain. Nonetheless, there may have been unmeasured confounders related to the decision to obtain imaging. The imaging data did not specify the exact indication for the radiologic test, and in some cases, the CT (or US) performed at the time of the visit may have been the more appropriate test. Our study, however, was not designed to evaluate appropriateness of imaging; rather, we sought to explore variation in resource utilization across EDs. Additionally, visits with both US and CT imaging were not included in the isolated CT group; however, it is possible that the US was done to evaluate for ovarian pathology, specifically, and the CT to evaluate for appendicitis, which would be inconsistent with an “ultrasound-first” approach to the evaluation of appendicitis. This scenario would result in our underestimating actual CT practices. Also, given the retrospective nature of the data extraction, previous visits to facilities outside of the 16 ED network may not be reported. Finally, this study was performed within a single, regional health system, and the results may not generalize to all EDs. However, our study includes 14 different EDs, which serve a large catchment area.
5. Conclusions
There are racial/ethnic and insurance disparities in advanced imaging use for pediatric visits for abdominal pain. General EDs are less likely than pediatric EDs to use advanced imaging overall, however, are more reliant on CT rather than US when imaging is utilized. Our findings highlight the need for increased attention to current ED imaging practices in an effort to reduce disparities in care and improve the use of “ultrasound first” in the evaluation of pediatric patients with abdominal pain.
Acknowledgments
Funding Sources: This work was supported by the National Institutes of Health through [Grant Number UL1TR000005].
Abbreviations
- CT
Computed Tomography
- CI
Confidence Interval
- ED
Emergency Department
- OR
Odds ratio
- US
Ultrasound
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Financial relationships: All authors have no financial relationships relevant to this article to disclose.
conflicts of interest: Authors have no conflicts of interest to disclose.
References
- 1.Prevention CfDCa. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. [Accessed December 17, 2015];2015 [Google Scholar]
- 2.Hryhorczuk AL, Mannix RC, Taylor GA. Pediatric abdominal pain: use of imaging in the emergency department in the United States from 1999 to 2007. Radiology. 2012;263(3):778–785. doi: 10.1148/radiol.12111726. [DOI] [PubMed] [Google Scholar]
- 3.Caperell K, Pitetti R, Cross KP. Race and acute abdominal pain in a pediatric emergency department. Pediatrics. 2013;131(6):1098–1106. doi: 10.1542/peds.2012-3672. [DOI] [PubMed] [Google Scholar]
- 4.Guthery SL, Hutchings C, Dean JM, Hoff C. National estimates of hospital utilization by children with gastrointestinal disorders: analysis of the 1997 kids' inpatient database. J Pediatr. 2004;144(5):589–594. doi: 10.1016/j.jpeds.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 5.Howell JM, Eddy OL, Lukens TW, et al. Clinical policy: Critical issues in the evaluation and management of emergency department patients with suspected appendicitis. Ann Emerg Med. 2010;55(1):71–116. doi: 10.1016/j.annemergmed.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 6.van Randen A, Laméris W, van Es HW, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011;21(7):1535–1545. doi: 10.1007/s00330-011-2087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kocher KE, Meurer WJ, Desmond JS, Nallamothu BK. Effect of testing and treatment on emergency department length of stay using a national database. Acad Emerg Med. 2012;19(5):525–534. doi: 10.1111/j.1553-2712.2012.01353.x. [DOI] [PubMed] [Google Scholar]
- 8.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 9.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Commission USNR. ALARA. [Accessed September 14, 2015];2015 http://www.nrc.gov/reading-rm/basic-ref/glossary/alara.html.
- 12.Radiology ACo. Appropriateness Criteria: Right Lower Quadrant Pain, Suspected Appendicitis. [Accessed December 17, 2015];2015 http://www.acr.org/~/media/7425a3e08975451eab571a316db4ca1b.pdf. [Google Scholar]
- 13.Antevil JL, Rivera L, Langenberg BJ, Hahm G, Favata MA, Brown CV. Computed tomographybased clinical diagnostic pathway for acute appendicitis: prospective validation. J Am Coll Surg. 2006;203(6):849–856. doi: 10.1016/j.jamcollsurg.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 14.Couchman GR, Forjuoh SN, Rajab MH, Phillips CD, Yu J. Nonclinical factors associated with primary care physicians' ordering patterns of magnetic resonance imaging/computed tomography for headache. Acad Radiol. 2004;11(7):735–740. doi: 10.1016/j.acra.2004.03.050. [DOI] [PubMed] [Google Scholar]
- 15.Richardson LD, Babcock Irvin C, Tamayo-Sarver JH. Racial and ethnic disparities in the clinical practice of emergency medicine. Acad Emerg Med. 2003;10(11):1184–1188. doi: 10.1111/j.1553-2712.2003.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 16.Wall SP, Ha ES, Habicht ME, et al. Impact of patient race on receiving head CT during blunt head injury evaluation. Acad Emerg Med. 2005;12(9):862–868. doi: 10.1197/j.aem.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Fahimi J, Herring A, Harries A, Gonzales R, Alter H. Computed tomography use among children presenting to emergency departments with abdominal pain. Pediatrics. 2012;130(5):e1069–e1075. doi: 10.1542/peds.2012-0739. [DOI] [PubMed] [Google Scholar]
- 18.Mannix R, Bourgeois FT, Schutzman SA, Bernstein A, Lee LK. Neuroimaging for pediatric head trauma: do patient and hospital characteristics influence who gets imaged? Acad Emerg Med. 2010;17(7):694–700. doi: 10.1111/j.1553-2712.2010.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Natale JE, Joseph JG, Rogers AJ, et al. Cranial computed tomography use among children with minor blunt head trauma: association with race/ethnicity. Arch Pediatr Adolesc Med. 2012;166(8):732–737. doi: 10.1001/archpediatrics.2012.307. [DOI] [PubMed] [Google Scholar]
- 20.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3):e310–e315. doi: 10.1542/peds.2004-1541. [DOI] [PubMed] [Google Scholar]
- 21.Payne NR, Puumala SE. Racial disparities in ordering laboratory and radiology tests for pediatric patients in the emergency department. Pediatr Emerg Care. 2013;29(5):598–606. doi: 10.1097/PEC.0b013e31828e6489. [DOI] [PubMed] [Google Scholar]
- 22.Hartman M, Watson RS, Linde-Zwirble W, et al. Pediatric traumatic brain injury is inconsistently regionalized in the United States. Pediatrics. 2008;122(1):e172–e180. doi: 10.1542/peds.2007-3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wennberg J, Gittelsohn A. Variations in medical care among small areas. Sci Am. 1982;246(4):120–134. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- 24.Fung V, Schmittdiel JA, Fireman B, et al. Meaningful variation in performance: a systematic literature review. Med Care. 2010;48(2):140–148. doi: 10.1097/MLR.0b013e3181bd4dc3. [DOI] [PubMed] [Google Scholar]
- 25.Selby JV, Schmittdiel JA, Lee J, et al. Meaningful variation in performance: what does variation in quality tell us about improving quality? Med Care. 2010;48(2):133–139. doi: 10.1097/MLR.0b013e3181c15a6e. [DOI] [PubMed] [Google Scholar]
- 26.Liang K-Y, Zeger S. Longitudinal Data Analysis Using Generalized Linear Models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 27.Johnson TJ, Weaver MD, Borrero S, et al. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. 2013;132(4):e851–e858. doi: 10.1542/peds.2012-3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takakuwa KM, Estepa AT, Shofer FS. Knowledge and attitudes of emergency department patients regarding radiation risk of CT: Effects of age, sex, race, education, insurance, body mass index, pain, and seriousness of illness. AJR Am J Roentgenol. 2010;195(5):1151–1158. doi: 10.2214/AJR.09.3847. [DOI] [PubMed] [Google Scholar]
- 29.Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102(5):988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 32.White-Means S, Zhiyong Dong, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009;66(4):436–455. doi: 10.1177/1077558709333995. [DOI] [PubMed] [Google Scholar]
- 33.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burr A, Renaud EJ, Manno M, et al. Glowing in the dark: time of day as a determinant of radiographic imaging in the evaluation of abdominal pain in children. J Pediatr Surg. 2011;46(1):188–191. doi: 10.1016/j.jpedsurg.2010.09.088. [DOI] [PubMed] [Google Scholar]
- 36.Raval MV, Deans KJ, Rangel SJ, Kelleher KJ, Moss RL. Factors associated with imaging modality choice in children with appendicitis. J Surg Res. 2012;177(1):131–136. doi: 10.1016/j.jss.2012.03.044. [DOI] [PubMed] [Google Scholar]
- 37.Garcia Peña BM, Mandl KD, Kraus SJ, et al. Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA. 1999;282(11):1041–1046. doi: 10.1001/jama.282.11.1041. [DOI] [PubMed] [Google Scholar]
- 38.Estey A, Poonai N, Lim R. Appendix not seen: the predictive value of secondary inflammatory sonographic signs. Pediatr Emerg Care. 2013;29(4):435–439. doi: 10.1097/PEC.0b013e318289e8d5. [DOI] [PubMed] [Google Scholar]
- 39.Ross MJ, Liu H, Netherton SJ, et al. Outcomes of children with suspected appendicitis and incompletely visualized appendix on ultrasound. Acad Emerg Med. 2014;21(5):538–542. doi: 10.1111/acem.12377. [DOI] [PubMed] [Google Scholar]
- 40.Cohen B, Bowling J, Midulla P, et al. The non-diagnostic ultrasound in appendicitis: is a nonvisualized appendix the same as a negative study? J Pediatr Surg. 2015;50(6):923–927. doi: 10.1016/j.jpedsurg.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 41.Pines JM, Hollander JE, Isserman JA, et al. The association between physician risk tolerance and imaging use in abdominal pain. Am J Emerg Med. 2009;27(5):552–557. doi: 10.1016/j.ajem.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 42.Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology. 2012;265(3):733–742. doi: 10.1148/radiol.12120614. [DOI] [PubMed] [Google Scholar]
- 43.Townsend BA. Ultrasound as an alternative to computed tomography for pediatric imaging. N C Med J. 2014;75(2):128–129. doi: 10.18043/ncm.75.2.128. [DOI] [PubMed] [Google Scholar]
- 44.Wan MJ, Krahn M, Ungar WJ, et al. Acute appendicitis in young children: cost-effectiveness of US versus CT in diagnosis--a Markov decision analytic model. Radiology. 2009;250(2):378–386. doi: 10.1148/radiol.2502080100. [DOI] [PubMed] [Google Scholar]
- 45.Brody AS, Frush DP, Huda W, Brent RL. Radiology AAoPSo. Radiation risk to children from computed tomography. Pediatrics. 2007;120(3):677–682. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 46.Frush K. Why and when to use CT in children: perspective of a pediatric emergency medicine physician. Pediatr Radiol. 2014;44(Suppl 3):409–413. doi: 10.1007/s00247-014-3122-x. [DOI] [PubMed] [Google Scholar]
- 47.Aspelund G, Fingeret A, Gross E, et al. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics. 2014;133(4):586–593. doi: 10.1542/peds.2013-2128. [DOI] [PubMed] [Google Scholar]
- 48.Akhtar W, Ali S, Arshad M, Ali FN, Nadeem N. Focused abdominal CT scan for acute appendicitis in children: can it help in need? J Pak Med Assoc. 2011;61(5):474–476. [PubMed] [Google Scholar]
- 49.Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Raptopoulos V. Right lower quadrant pain and suspected appendicitis: nonfocused appendiceal CT--review of 100 cases. Radiology. 2000;217(1):159–163. doi: 10.1148/radiology.217.1.r00oc34159. [DOI] [PubMed] [Google Scholar]
- 50.Rao PM, Rhea JT, Novelline RA, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology. 1997;202(1):139–144. doi: 10.1148/radiology.202.1.8988203. [DOI] [PubMed] [Google Scholar]
- 51.Rhea JT, Rao PM, Novelline RA, McCabe CJ. A focused appendiceal CT technique to reduce the cost of caring for patients with clinically suspected appendicitis. AJR Am J Roentgenol. 1997;169(1):113–118. doi: 10.2214/ajr.169.1.9207509. [DOI] [PubMed] [Google Scholar]
- 52.Fefferman NR, Roche KJ, Pinkney LP, Ambrosino MM, Genieser NB. Suspected appendicitis in children: focused CT technique for evaluation. Radiology. 2001;220(3):691–695. doi: 10.1148/radiol.2203001826. [DOI] [PubMed] [Google Scholar]