Abstract
Background
The disease burden associated with stroke by age is not well known.
Aim
To assess the trends in stroke hospitalizations and associated cost among adults aged ≥18 years by age groups in the United States.
Methods
The study population consisted of 2003–2012 adult hospitalizations from the National Inpatient Sample of the Healthcare Cost and Utilization Project. Subarachnoid hemorrhage, intracerebral hemorrhage, and acute ischemic stroke hospitalizations were identified by the principal diagnosis ICD-9-CM code. We estimated national hospitalization rates and inflation-adjusted hospital costs across five consecutive 2-year time intervals, stratified by seven age groups.
Results
Hospitalization rates for subarachnoid hemorrhage decreased significantly from 2003–2004 to 2011–2012 for ages 35–44 (relative percent change (RPC): −23%) and 45–54 (RPC: −22%), respectively. For intracerebral hemorrhage, the rates decreased significantly for ages ≥65 years. Acute ischemic stroke hospitalization rates increased significantly for ages 18–54 and decreased significantly for ages 65–84 years. The average per-hospitalization cost for subarachnoid hemorrhage increased 7–35% among all age groups, except those aged 65–74, and increased 10–29% for intracerabral hemorrhage except those aged 75–84, and increased 6–19% among all ages for acute ischemic stroke, respectively. Overall, the estimated total national cost increased 7% for subarachnoid hemorrhage, 10% for intracerebral hemorrhage, and 18% for acute ischemic stroke from 2003–2004 to 2011–2012.
Conclusions
From 2003 to 2012, subarachnoid hemorrhage and intracerabral hemorrhage stroke hospitalization rates declined across all age groups. While US acute ischemic stroke hospitalizations among ages 65–84 declined significantly, the hospitalization rates increased significantly among ages 18–54. The estimated hospital costs increased across all stroke subtypes during the study period.
Keywords: Hospitalization rate, subarachnoid hemorrhage stroke, intracerebral hemorrhage stroke, acute ischemic stroke, trends
Introduction
Stroke mortality in the United States has decreased from the 4th to 5th leading cause of death; however, stroke continues to be a leading cause of serious long-term disability.1,2 Each year, nearly 800,000 people experience a new or recurrent stroke.2 Of all strokes, an estimated 87% are ischemic, 3% are subarachnoid hemorrhage, and 10% are intracerebral hemorrhage.2
In a previous report, George et al.3 identified an increase in the prevalence of acute ischemic stroke hospitalizations as the principal diagnosis among adolescent and young adults (age 15–44 years) between 1995 and 2008. Although several studies have reported temporal trends in stroke hospitalizations, many of them focused only on those aged ≥65 years, while others examined hospitalizations with either principal or secondary stroke diagnosis for specific age groups.4–6
Limited studies exist on trends in hospital cost associated with acute stroke events by age. In addition to examining the latest temporal trends in stroke hospitalizations, this study is intended to fill this gap and provide estimates on the costs associated with stroke across seven age groups.
Aims
The aim of the present study was to determine the trends in hospitalizations caused by acute stroke by age groups, as well as cost trends associated with those hospitalizations from 2003 to 2012.
Methods
Data sources and study sample
The National Inpatient Sample (NIS) is part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ).7 The NIS is a database of hospital inpatient stays derived from billing data submitted by hospitals to statewide data organizations across the United States. The database captures information on more than 7 million discharges from an average of 1000 hospitals each year, which are weighted to represent over 36 million hospitalizations nationally. All discharges are captured from selected hospitals regardless of payer status.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) was used to identify hospitalizations for subarachnoid hemorrhage (430), intracerebral hemorrhage (431), and acute ischemic stroke (433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, and 436). For each hospitalization, only the principal diagnosis code was used to identify events, which were then assigned to one of three mutually exclusive categories: subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), and acute ischemic stroke (AIS). In the NIS, the principal diagnosis codes are valid at the time of discharge and reflect the condition that is chiefly responsible for the patient’s admission to the hospital.
Statistical methods
The unit of analysis was the hospital discharge. In this analysis, hospital discharge records were included if the patient was 18 years or older at the time of the hospital admission. Patient characteristics included: age, gender, race, first-listed payment source, and discharge disposition. Hospital characteristics included geographic region. The hospital costs were determined by multiplying the total hospital charges by the provided mean cost-to-charge ratios for each hospital. Charges represented what the hospital billed for the case and did not include professional (physician) fees. We combined NIS annual data to create five consecutive 2-year time periods for obtaining the stable estimates between 2003 and 2012. The descriptive statistics and temporal trends were presented for seven age groups: 18–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85 years.
As a result of the redesigning with 2012 data, we used trend weights developed by AHRQ to make estimates comparable for data prior to 2012.8 The rate for the stroke admissions in the United States per 100,000 US population was defined as: (Number of weighted NIS discharges with a principal diagnosis of stroke/ US adult population count from the Census for the same data year)∗100,000.9 We used the personal consumption expenditure (PCE) index for hospital services to adjust costs incurred in earlier years to reflect 2012 US dollars.10 We summarized patient characteristics and calculated the relative percent changes (RPC) in hospitalization rates and average charge per hospitalization over time. We used orthogonal polynomial coefficients (POLYNOMIAL statement in SUDAAN) according to the method of Fisher and Yates (1938) to generate linear contrasts for testing the temporal trends in each age group across five time periods independently. All statistical analyses were conducted using SAS 9.3-callable SUDAAN (Research Triangle Institute, Research Triangle Park, NC) to account for the multistage, disproportionate stratified sampling design.
Because the data are publicly available and do not contain direct personal identifiers, this study was exempted from review by the institutional review board of the Centers for Diseases Control and Prevention.
Results
Subarachnoid hemorrhagic stroke
During the study period, the rates of hospitalizations per 100,000 persons with a principal diagnosis of SAH decreased significantly among persons aged 35 to 44 years (RPC of −23%, Table 1) and 45 to 54 years (RPC of −22%). There were no significant changes among other age groups.
Table 1.
Trends in hospitalization and resource utilization in adults, by the principal diagnosis of SAH, ICH, and AIS by age, NIS 2003–2012
| Principal diagnosis | SAH | ICH | AIS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2003–2004 | 2011–2012* | RPCa | 2003–2004 | 2011–2012* | RPCa | 2003–2004 | 2011–2012* | RPCa | |
| Age 18–34 | |||||||||
| Number of hospitalizations | 3567 | 3411 | 2772 | 2888 | 8275 | 10,178 | |||
| Rates per 100,000 persons | 2.61 | 2.33 | −11% | 2.03 | 1.97 | −3% | 6.05 | 6.95* | 15% |
| Average per-hospitalization costb | $40,509 | $51,509 | 27% | $28,717 | $32,016 | 11% | $14,221 | $15,967 | 10% |
| Age 35–44 | |||||||||
| Number of hospitalizations | 7427 | 5282 | 6056 | 5169 | 25,350 | 28,287 | |||
| Rates per 100,000 persons | 8.44 | 6.51* | −23% | 6.89 | 6.37 | −7% | 28.82 | 34.87* | 21% |
| Average per-hospitalization costb | $45,841 | $55,099 | 20% | $27,383 | $34,928 | 28% | $12,089 | $14,379 | 19% |
| Age 45–54 | |||||||||
| Number of hospitalizations | 13,474 | 11,408 | 15,858 | 16,467 | 82,271 | 102,083 | |||
| Rates per 100,000 persons | 16.34 | 12.82* | −22% | 19.23 | 18.51 | −4% | 99.78 | 114.76* | 15% |
| Average per-hospitalization costb | $46,174 | $55,984 | 21% | $25,241 | $30,086 | 19% | $11,201 | $12,976 | 16% |
| Age 55–64 | |||||||||
| Number of hospitalizations | 10,728 | 11,848 | 19,508 | 22,568 | 167,053 | 202,227 | |||
| Rates per 100,000 persons | 18.72 | 15.46 | −17% | 34.04 | 29.45 | −13% | 291.47 | 263.90 | −9% |
| Average per-hospitalization costb | $49,356 | $53,025 | 7% | $23,852 | $26,774 | 12% | $10,624 | $12,374 | 16% |
| Age 65–74 | |||||||||
| Number of hospitalizations | 6916 | 7386 | 23,094 | 22,487 | 235,742 | 249,585 | |||
| Rates per 100,000 persons | 18.61 | 15.90 | −15% | 62.13 | 48.40* | −22% | 634.25 | 537.17* | −15% |
| Average per-hospitalization costb | $46,528 | $46,734 | 0 | $18,656 | $20,477 | 10% | $10,364 | $11,337 | 9% |
| Age 75–84 | |||||||||
| Number of hospitalizations | 6136 | 6039 | 38,301 | 30,809 | 337,468 | 298,210 | |||
| Rates per 100,000 persons | 23.70 | 22.82 | −4% | 147.96 | 116.44* | −21% | 1303.65 | 1127.09* | −14% |
| Average per-hospitalization costb | $28,928 | $31,271 | 8% | $14.486 | $14,071 | −3% | $10,318 | $10,942 | 6% |
| Age 85+ | |||||||||
| Number of hospitalizations | 2697 | 3163 | 20,294 | 20,913 | 172,992 | 198,904 | |||
| Rates per 100,000 persons | 29.93 | 27.09 | −9% | 225.19 | 179.12* | −20% | 1919.56 | 1703.66 | −11% |
| Average per-hospitalization costb | $16,187 | $21,845 | 35% | $9582 | $12,330 | 29% | $9373 | $10,368 | 11% |
| Total cost in billionsc | 2.18 | 2.34 | 7% | 2.29 | 2.52 | 10% | 10.67 | 12.55 | 18% |
p-value for trend<0.05.
Relative percent change (RPC) for a given variable X is calculated with the following: (X2011-2012 – X2003-2004)/ X2003-2004.
The costs was obtained by using HCUP cost-to-charge ratios multiplying total charges after accounting for inflation using the hospital services component of the Personal Consumption Expenditure index.
Total costs was obtained by number of hospitalizations multiplying average per-hospitalization cost.
After we adjusted for inflation, the average per-hospitalization cost for SAH increased during the study period across all age groups except persons aged 65–74 years (Table 1). The greatest increases were observed among ages ≥85 years (RPC: 35%), ages 18–34 years (RPC: 27%), and ages 45–54 years (RPC: 21%). When we combined the per-hospitalization cost and number of hospitalizations across all age groups, we estimated that the total national costs for hospitalizations with SAH as the principal diagnosis increased from $2.18 billion during 2003–2004 to $2.34 billion during 2011–2012 (RPC: 7%).
The proportion of men did not change across the age groups except among those aged 65–84 years (Table 1 in the online-only data supplement). There were significant increases in SAH hospitalizations among “other” race groups across all age groups except ages 18–34 years and ages ≥85 years. Among the youngest group, hospitalizations among African Americans increased from 20.7% in 2003–2004 to 26.5% in 2011–2012. The regional distribution did not change significantly, where persons were consistently more likely to be from South. The use of Medicaid increased significantly among persons aged 18–64 years while no changes on payer types among persons aged ≥65 years. The in-hospital death rate declined significantly among persons aged ≥45 years. The proportions of SAH hospitalizations transferred to short-term hospitals decreased significantly from 2003 to 2004 to 2011–2012 among ages 18–34 years, 45–54 years, 55–64 years, and 75–84 years respectively while the proportions of those transferred to rehabilitation, nursing or skilled nursing facilities, long-term care facility, or hospice facility increased significantly among the two oldest age group. The average length of stay (in days) was significantly shorter in 2011–2012 as compared to 2003–2004 among those aged ≥55 years.
Intracerebral hemorrhage stroke
During 2003–2012, the rates of hospitalization per 100,000 persons with a principal diagnosis of ICH decreased significantly in the three oldest age groups (RPC of approximately −20%, Table 1). The hospitalization rates remained stable among other age groups over time.
The inflation-adjusted average per-hospitalization cost for ICH increased across all age groups except those aged 75–84 years during the study period. The largest increase was observed among ages ≥85 years (RPC of 29%, Table 1), and ages 35–44 years (RPC of 28%). In 2011–2012, the estimated national cost in ICH hospitalizations totaled $2.52 billion, resulting in a 10% relative percent increase from 2003–2004.
The proportion of men increased among ages 65 to 74 years from 54.5% in 2003–2004 to 56.3% in 2011–2012 (Table 1 in the online-only data supplement). Hospitalization rates among those of “other” race increased significantly among persons aged 35–44 years and 45–54 years. Among those aged 35–64 years there was a significant increase in the use of Medicaid as the primary payer. The in-hospital death rate declined significantly across all age groups and the mean length of stay decreased over time among those aged ≥65 years. The proportions of ICH hospitalizations transferred to rehabilitation, nursing or skilled nursing facilities, long-term care facility, or hospice facility increased significantly from 2003–2004 to 2011–2012 across all age groups except ages 18–34 years.
Acute ischemic stroke
The hospitalization rates per 100,000 persons with a principal diagnosis of AIS increased significantly among persons aged 18–54 years, but decreased significantly among persons aged 65–84 years. The largest increase was observed among ages 35–44 years (RPC: 21%, Table 1) and the relative percent increases were 15% for both ages 18–34 and 45–54. There was no significant change in the hospitalization rate among ages 55–64 and ages ≥85 years, while the hospitalization rates declined significantly among ages 65–74 years (RPC of −15%) and ages 75–84 years (RPC of −14%), respectively.
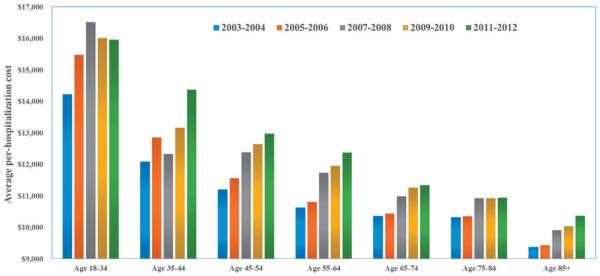
After adjusting for inflation, the average per-hospitalization cost for AIS increased from 6% to 19% across all age groups (Figure 1). The largest increase was observed among ages 35–44 years, with $12,089 per-hospitalization in 2003–2004 and $14,379 per hospitalization in 2011–2012 (RPC: 19%, Table 1). The estimated total cost reached $12.55 billion in 2011–2012 compared to $10.67 billion in 2003–2004 (RPC: 18%).
Figure 1.
Trends in average per-hospitalization cost among AIS by age.
The proportion of men increased significantly from 2003–2004 to 2011–2012 among those aged ≥45 years (Table 1 in the online-only data supplement). Distributions by race and geographic region showed little change over time. Strong trends were seen among proportions of payer types across all age groups. The in-hospital death rate declined significantly across the study period among all age groups except the youngest (18–34 years). The proportions of patients transferred to either short-term hospital or transferred to rehabilitation, nursing or skilled nursing facilities, long-term care facility, or hospice facility increased significantly from 2003–2004 to 2011–2012 among ages 45–74 years. The length of stay among AIS hospitalizations decreased significantly among all age groups, except those aged 55–64 years.
Discussion
Our data provided the latest trends in stroke hospitalizations by age groups from 2003–2004 to 2011–2012. During the study period, we observed an increase in AIS hospitalizations among younger adults (aged 18–34 years (RPC: 15%), 35–44 years (RPC: 21%), and 45–54 years (RPC: 15%)), which was concerning given decreases in older adults. Significant decreases were observed among persons hospitalized with SAH aged 35–54 years. Hospitalization rates for ICH declined significantly only among persons aged ≥ 65 years. The decreases in ICH and AIS hospitalizations among those aged ≥65 years might be attributable, at least in part, to the increased blood pressure control reported in this population,11 but the increases among younger adults was worrisome. On the other hand, the best control of hypertension could have more impact on the incidence of ICH, but not for SAH.
The findings of increasing trends in AIS hospitalization in young adults (18–54 years) were consistent with several studies.3,4 George et al.3 reported significant increases in the prevalence of AIS hospitalizations from 1995–1996 to 2007–2008 among persons aged 15–34 years and 35–44 years, respectively. Towfighi et al.4 identified significant increases in ischemic stroke hospitalizations combining both principal and secondary diagnoses among those aged 35–44 years. In addition, the observations of an increase in the incidence of ischemic stroke in young adults were also reported in several population-based registries.12,13 Our findings indicated continued increases in AIS hospitalizations among these age groups. However, for persons aged 35–44 years hospitalized with ICH, the declining trend from 1995–2008 appeared to have stabilized, based on our results for 2003–2012.
Ovbiagele et al examined stroke hospitalizations in the NIS for combined ischemic and hemorrhagic stroke types among persons aged 35–64 years between 1997 and 2006.4 They found stroke hospitalization rates declined among individuals aged 55–64 years and remained stable among persons aged 45–64 years. Our results identified no significant decline among persons aged 55–64 years with SAH, ICH, or AIS as the principal diagnosis independently. Consistent with other studies,5,6 a significant decline in stroke hospitalizations was observed among persons aged ≥65 years with AIS and ICH. However, hospitalizations for SAH remained stable during 2003–2012 among persons aged ≥65years.
While AIS hospitalizations increased in young adults (18–54 years), the in-hospital deaths remained stable (18–34 years) or decreased (35–44 years and 45–54 years respectively). A recent study using NCHS mortality data reported similar findings.14
The observed increase in total hospitalization costs suggested an increasing economic burden across all stroke types for acute stroke care, but the long-term impact on the economic burden of improved treatment are needed for further study. Our study identified decreasing lengths of stay in most age groups, implying that this was not a factor contributing to the rising perhospitalization cost. Despite a reduction in hospitalizations rates in several age groups, the absolute number of hospitalizations increased among ages 45–64 years, and ages ≥85 years for ICH. The same findings were observed among ages 55–74 years, and ages ≥85 years for AIS. This might explain in part the observed increase in overall stroke costs. In 2011–2012, the estimated total national cost for SAH, ICH, and AIS hospitalizations were $2.34 billion (RPC: 7%), $2.52 billion (RPC: 10%), and $12.55 billion (RPC: 18%), respectively. A recent publication reported the average annual inflation-adjusted Medicare payments for index hospitalizations of ischemic stroke were $8000 in 2005–2006 and $8489 in 2010–2011 (RPC: 6%).6 Our estimates of costs were higher, probably due to the fact that we were unable to make any adjust ments to the cost-to-charge ratios for the non-Medicare population. Medicare uses a system of standardized payments to reimburse hospitals and we were unable to account for potential differences that might exist between payers in the cost-to-charge ratios.
Other studies also reported the increasing cost of stroke care.15,16 Increasing cost likely has several explanations. First, it might be related to the increased use of diagnostic procedures for identification of underlying stroke etiology or co-morbid conditions associated with acute stroke and associated follow-up studies of underlying stroke etiology. Major predictors of hospital cost are length of stay, stroke severity, cardiac disease, and room charges.17 Increased uses of neuro-intensive care units or specialized stroke units, increased use of thrombolytic therapy, and extended cardiac monitoring for identification of atrial fibrillation and carotid imaging are also the potential factors contributing to cost. In our study, we identified the proportions of hospitalizations with AIS transferred to either short-term hospitals or rehabilitation, nursing or skilled nursing facilities, long-term care facility, or hospice facility increased significantly over time. This might be related to the severity or increasing using of advanced stroke care systems. However, in our studies, there was a lack of the clinical information in the dataset to assess these factors. Finally the cost presented in this study did not include the professional (physician) fees, or the cost of rehabilitation or long-term care for the survivors and, therefore, the total medical costs will be higher than those reported in this study.
The strength of this study is that it represents national hospitalizations throughout the United States; however, our findings have limitations. First, any change in coding practices might impact temporal trends in hospitalization rates. The increased use of magnetic resonance imaging and other arterial flow studies for ischemic stroke may lead to an increase in the diagnosis and further treatment planning for these cases. Second, the number of states contributing data to the NIS has increased over years, which could introduce bias in the sample over time. In addition, the estimates of costs might have some variation as compared to the actual cost. Since the cost-to-charge ratios applied in this analysis were unique for each hospital, the lack of information on the differences in payers might affect the estimates. Finally, the unit of the analysis was hospital discharge, not the patient, thus we would not be able to identify repeat hospitalizations in any calendar year.
Conclusions
Our findings demonstrate a significant increase in AIS hospitalizations among persons aged 18–54 years, contributing to an overall 18% relative increase in all stroke hospitalizations in this population. The rates of hospitalization declined significantly for SAH among persons aged 35–54, and for both ICH and AIS among persons aged ≥65. Regardless of trends in stroke hospitalizations, the increasing national hospital cost indicates the rising economic burden of stroke in the health care system, although this might represent improved testing and monitoring to optimize treatment to prevent recurrent strokes. Most importantly, the increased economic burden of stroke is due to both an increase in the per-hospital costs as well as an overall increase in the number of stroke hospitalizations among younger adults. This information has compelling importance for prevention efforts across all age groups, and particularly among adults under age 65.
Supplementary Material
Acknowledgments
Paper is a part of an oral presentation at the 2016 International Stroke Conference, Los Angeles, CA, USA, 17–19 February.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Authors’ contributions
Study conception and design: XT, MGG, CG, and RM
Analysis and interpretation of data: XT, MGG, and CG
Drafting of manuscript: XT and MGG
Critical revision: XT, MGG, CG, and RM
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2010. National Vital Statistics Reports. 2013:61. [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation. 2015;131:e9–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.George MG, Tong X, Kuklina EV, Labarthe DR. Trends in stroke hospitalizations and associated risk factors among children and young adults, 1995–2008. Ann Neurol. 2011;70:713–721. doi: 10.1002/ana.22539. [DOI] [PubMed] [Google Scholar]
- 4.Towfighi A, Markovic D, Ovbiagele B. Recent patterns of sex-specific midlife stroke hospitalization rates in the United States. Stroke. 2011;42:3029–3033. doi: 10.1161/STROKEAHA.111.618454. [DOI] [PubMed] [Google Scholar]
- 5.Fang MC, Perraillon MC, Ghosh K, Culter DM, Rosen AB. Trends in stroke rates, risk, and outcomes in the United States, 1988 to 2008. Am J Med. 2014;127:608–615. doi: 10.1016/j.amjmed.2014.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krumholz HM, Normand ST, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke: 1999–2011. Circulation. 2014;130:966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project . Introduction to the HCUP Nationwide Inpatient Sample (NIS) Agency for Healthcare Research and Quality; Rockville, Maryland: 2012. http://hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2012.pdf. [Google Scholar]
- 8.Healthcare Cost and Utilization Project . Nationwide inpatient sample redesign final report. Agency for Healthcare Research and Quality; Rockville, Maryland: 2014. http://hcup-us.ahrq.gov/db/nation/nis/reports/NISRedesignFinalReport040914.pdf. [Google Scholar]
- 9.Healthcare Cost and Utilization Project . Population Denominator Data for use with the HCUP Databases (Updated with 2012 Population data) Report # 2013–01. Agency for Healthcare Research and Quality; Rockville, Maryland: 2013. http://hcup-us.ahrq.gov/reports/methods/2013_01.pdf. [Google Scholar]
- 10.Bureau of Economic Analysis . Table 2.4.4U. Price Indexes for Personal Consumption Expenditures by Type of Product. U.S. Department of Commerce; Washington, D.C.: 2014. http://www.bea.gov/iTable/iTable.cfm?ReqID=9&step=1#reqid=9&step=3&isuri=1&903=69. [Google Scholar]
- 11.Rosengren A, Giang KW, Lappas G, Jern C, Torén K, Björck Twenty-four-year trends in the incidence of ischemic stroke in Sweden from 1987 to 2010. Stroke. 2013;44:2388–2393. doi: 10.1161/STROKEAHA.113.001170. [DOI] [PubMed] [Google Scholar]
- 12.Béjot Y, Daubail B, Jacquin A, Durier J, Osseby GV, Rouaud O, et al. Trends in the incidence of ischaemic stroke in young adults between 1985 and 2011: The Dijon Stroke Registry. J Neurol Neurosurg Psychiatry. 2014;85:509–513. doi: 10.1136/jnnp-2013-306203. [DOI] [PubMed] [Google Scholar]
- 13.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poisson S, Glidden D, Johnston SC, Fullerton HJ. Deaths from stroke in US young adults, 1989–2009. Neurology. 2014;83:2110–2115. doi: 10.1212/WNL.0000000000001042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cadilhac DA, Carter R, Thrift AG, Dewey HM. Estimating the long-term costs of ischemic and hemorrhagic stroke for Australia. Stroke. 2009;40:915–921. doi: 10.1161/STROKEAHA.108.526905. [DOI] [PubMed] [Google Scholar]
- 16.Brown DL, Boden-Albala B, Langa KM, Lisabeth LD, Fair M, Smith MA, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 17.Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, Hsu CY, et al. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999;30:724–728. doi: 10.1161/01.str.30.4.724. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.