Abstract
Introduction
Troponins are known to be released in response to cardiac damage and therefore are the biomarkers of choice for the early diagnosis of acute myocardial infarction (AMI), improving outcome in patients presenting with chest pain. However, false results can occur due to interference from other substances in the blood.
Case
A 52-year-old male with a past medical history of alcohol abuse, hypertension, and coronary artery bypass graft at age 34 with normal stress test 2 years before presented to the emergency department (ED) complaining of 1 day of non-exertional chest pain with radiation to the neck and left arm. His troponin was elevated to 5 ng/mL in two samples drawn 12 h apart, with normal CK-MB. Renal function was normal. Electrocardiogram (ECG) showed normal sinus rhythm with no ST elevations or depressions. He underwent cardiac catheterization which showed no obstructive lesions. Five years later, he returned to the ED with abdominal pain and shortness of breath. Troponin was elevated and showed no signs of downtrend on repeat every 6 h. ECG was unchanged from 5 years before. He was discharged with a follow-up cardiac computed tomography (CT). Troponin was measured on the day of his scan and remained elevated; he was asymptomatic. Cardiac CT showed unremarkable coronaries and bypass grafts. Given persistently positive troponin in the setting of minimal to no symptoms, he was thought to have falsely elevated troponins. Centrifugation and 2:1 dilution of the sample resulted in the same general value, respectively. Rheumatoid factor and heterophile antibodies were negative. When his blood sample was sent to a different hospital utilizing a three-site immunoassay method, the value was found zero.
Discussion
Cardiac troponins (cTn) are structural proteins unique to the heart, not expressed outside of cardiac tissue and have high sensitivity and specificity for myocardial damage. Therefore, it is the test of choice for the diagnosis of AMI. When an increased troponin value is encountered in the absence of myocardial infarction, other etiologies should be explored, including vasculitis, drug abuse, myocarditis, pulmonary embolism, sepsis, and renal failure. If the clinical picture is not consistent with the elevated lab value, it is necessary to think of other causes, including false-positive results. The prevalence of this type of interference is likely to worsen in the future because of the emergence of immunotherapy in the treatment of a wide range of conditions and the use of radiolabeled antibodies in diagnosis using immunoscintigraphic procedures. Therefore, it is important to consider this as part of the differential.
Keywords: troponin, myocardial infarction, false immunoassay, false positive, CK-MB, two-site immunoasay, three-site immunoassay, chest pain
Acute myocardial infarction (AMI) is a major cause of death and disability. Approximately 15 million patients per year in the United States and Europe present to the emergency department (ED) with chest pain or other symptoms suggestive of AMI (1). Cardiac troponins (cTn) are structural proteins unique to the heart, not expressed outside of cardiac tissue. They have high sensitivity and specificity for myocardial damage and, therefore, are the test of choice for the diagnosis of AMI (1, 2). When an increased cTn value is encountered in the absence of AMI, a careful search for other possible etiologies including vasculitis, drug abuse, myocarditis, pulmonary embolism, sepsis, renal failure, etc., should be undertaken (3). However, one of the overlooked reasons of elevated troponin, although rare, is false-positive troponin. A case is presented below.
Case
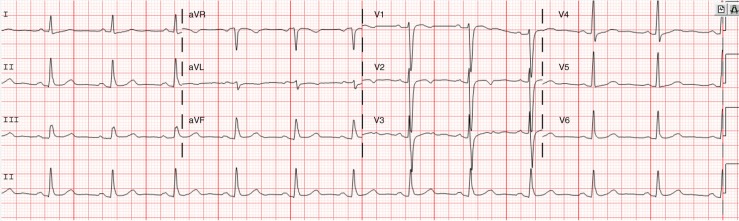
A 52-year-old male with a past medical history of alcohol abuse, hypertension, and coronary artery bypass graft (CABG) at age 34 due to previous myocardial infarction (MI) and status postnormal stress test from 2 years before presented to the ED with 1 day of chest pain that began while watching television. He described the pain as different from his previous MI, less intense, not crushing in nature, rated 6 out of 10, with radiation to the neck and down the left arm. Each episode lasted 3 to 5 min throughout the day. He also complained of diaphoresis, but denied shortness of breath, dizziness, palpitations, nausea or vomiting. He endorsed running the day before with no chest pain and an exercise tolerance of 8–9 blocks, which had been unchanged for the past year. In the ED, initial troponin measured was 5.04 ng/mL, with repeat troponin 12 h later found at 4.72 ng/mL. CK-MB and renal function were normal. Electrocardiogram (ECG) showed normal sinus rhythm (NSR) but no significant ST elevations or depressions with some T-wave changes (Fig. 1).
Fig. 1.
NSR with dynamic changes in T-waves in V1 and V2 when comparing two ECGs.
Echocardiogram showed mild tricuspid regurgitation, with normal left ventricular contractility, global left ventricular ejection fraction of 65%, and trivial pericardial effusion. Given the troponin elevation and patient history, he underwent cardiac catheterization, which revealed mild diffuse disease with patent left internal mammary artery to left anterior descending artery (LAD). He was deemed to have non-obstructive coronary artery disease (CAD).
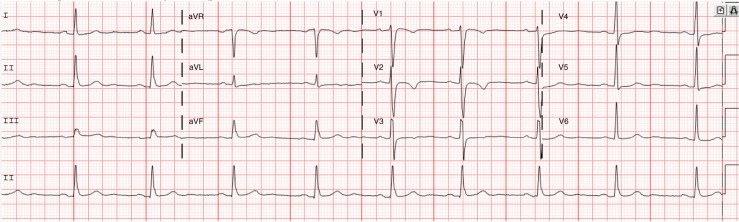
Five years later, he presented to the ED at another hospital with severe lower abdominal pain that began around 5 am, described as gas pain with shortness of breath. Motrin did not alleviate the pain, so he presented to the ED. On further questioning, he denied any chest pain, nausea, vomiting, palpitations, dizziness, fever, or diarrhea and reported unlimited exercise tolerance. Troponin was trended every 6 h and was as follows: 4.75 ng/mL, 4.29 ng/mL, 3.98 ng/mL, 4.43 ng/mL, and 4.59 ng/mL. Creatinine in this admission remained at baseline. ECG remained unchanged from 5 years before (Fig. 2).
Fig. 2.
Repeat ECG after second emergency department visit.
He was transferred to our hospital for catheterization capabilities, and his troponin continued to be trended. They remained elevated in the same range. Given stably elevated levels of troponin without any signs of downtrending, the thought was that the patient had falsely elevated troponin. Therefore, catheterization was deferred, and he was discharged with a cardiac computed tomography (CT) follow-up a few days later. Troponin was measured the day of his cardiac CT and was elevated to 5.72 ng/mL; he was asymptomatic. Cardiac CT revealed mild diffuse disease with patent grafts, similar to the catheterization 5 years before.
The concept of falsely elevated troponin was further investigated. The integrity of the assay is tested daily by the lab and was deemed to be correct. The patient's sample was first diluted 2:1 with repeat value of 6.13 ng/mL. The sample was centrifuged to remove any interfering substances, and the supernatant was measured; the value still remained elevated. The next theory was that there must be an antibody to the assay; therefore, the patient's blood sample was tested for rheumatoid factor and heterophile antibody, the two most common causes of false-positive immunoassay; both were found negative. The patient's blood sample was sent to a different hospital that utilizes a three-site immunoassay method for troponin and was returned negative. Therefore, the patient has an interfering substance to the immunoassay used at our facility.
Discussion
The sequence located between amino acid residues 30 and 110 of cardiac troponin I (cTnI) is the most stable region of the cTnI and, therefore, the area most often targeted for antibody detection for immunoassays. Immunoassays work via an antibody–antigen reaction through weak hydrogen bonds and van der Waals forces (4). There have been two mechanisms proposed for this reaction: the ‘lock and key’ model (where there is no change in the structure of the antibody when it binds to the antigen) and the ‘induced fit model’ (in which both the antigen and antibody change their conformation on binding) (5). Our facility uses the Access AccuTnI + 3TM assay, a two-site immunoenzymatic assay, which has a ‘capture’ antibody and a ‘signal’ antibody for quantification. False-positive results occur when these antibodies cross-react with other structurally related molecules. The quantity of labeled antibody linked determines the degree of positive assay response (4). False positives can also occur when plasma cells create endogenous antibodies that can bind to different epitopes involved in the antigen/analyte causing interference. This, interestingly, can occur in up to 30–40% of the population. It may be of importance to note that autoantibodies to cTn were found in 3–6% of healthy control subjects, blood donors, and hospitalized patients with or without a history of cardiac disease (5).
If a false-positive result is clinically suspected, there are several confirmatory measures. First, measurement of surrogate parameters, that is, creatinine kinase, CK-MB, and myoglobin, should be performed to see whether they are elevated (4). If these tests are within the normal range, as in our patient, further investigation would be warranted as this raises the suspicion of false positivity. To further prove false-positive results, serial dilutions can be done as the value is expected to decrease based on the dilution – that is to say, 2:1 dilution should halve the value. In a patient with falsely elevated troponin, dilution often fails to change the value since it is due to the interference. In fact, there may be a paradoxiical linearity with progressive dilution – the higher the dilution, the higher the troponin level (5). In our patient, the troponin level increased from 5 ng/mL to 6.15 ng/mL with a 2:1 dilution. No other dilutions were done unfortunately. The false-positive test can be remeasured after a month, as the interference can be transient depending on the nature of interference (i.e., infection or immunization). However, this is impractical if the patient is suspected of having AMI. In this case, the suspicion was low given the trend of the troponin, and more importantly, the patient's troponin remained elevated several days post discharge with no accompanying symptoms.
Interference can be permanent in some patients. It arises from various activities such as keeping pets, ingesting animal antigens, and blood transfusions. Interference may also be present in patients with an autoimmune disease, particularly in those who use monoclonal antibody immunotherapy such as those used in rheumatoid arthritis (RA). It may also be present in patients with hematological malignancies and solid tumors (5). Our patient was both RA antibody negative and heterophile antibody negative. Reanalysis after the removal of immunoglobulin antibodies via polyethylene glycol (PEG) precipitation can be done to verify the same; however, it was not possible at our institution. To verify that there is antibody interference, the blood sample was sent to another hospital and was tested using a different assay system, Advia Centaur XP TnI-Ultra assayTM. This system is a three-site sandwich immunoassay involving three different determinants, which provide higher sensitivity than two-site assays (6). The patient's troponin was found negative. Therefore, it appeared that our patient had falsely elevated troponin.
Conclusion
When an increased troponin value is encountered in the absence of MI, other etiologies should be explored, including vasculitis, drug abuse, myocarditis, pulmonary embolism, sepsis, and renal failure (1). Falsely elevated troponin should also be considered when data do not corroborate with clinical presentation. Our patient had persistently elevated troponin with no symptoms and therefore had an antibody to the two-site immunoassay used by the hospital. His value was found zero when a three-site immunoassay was utilized. False values can occur due to interferences from heterophile antibodies or human autoantibodies that mimic troponin, that minimic troponin, by linking the capture antibody to detection antibody. Dilution of the samples often fails to cause changes in the values. Addition of PEG will cause precipitation of the autoantibodies, reducing inference in the assay, which can make the diagnosis (4). The prevalence of this type of interference is likely to worsen in the future due to the emergence of immunotherapy in the treatment of a wide range of conditions, along with the use of radiolabeled antibodies in diagnostic immunoscintigraphic procedures (5). Therefore, this differential is important to keep in mind.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.White HD. Pathobiology of troponin elevations: Do elevations occur with myocardial ischemia as well as necrosis? J Am Coll Cardiol. 2011;57:2406–8. doi: 10.1016/j.jacc.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Adams JE, 3rd, Bodor GS, Dávila-Román VG, Delmez JA, Apple FS, Ladenson JH, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993;88:101–6. doi: 10.1161/01.cir.88.1.101. [DOI] [PubMed] [Google Scholar]
- 3.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–67. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 4.Boscato LM, Stuart MC. Incidence and specificity of interference in two-site immunoassays. Clin Chem. 1986;32:1491–5. [PubMed] [Google Scholar]
- 5.Ismail AA. Identifying and reducing potentially wrong immunoassay results even when plausible and ‘not-unreasonable’. Adv Clin Chem. 2014;66:241–94. doi: 10.1016/b978-0-12-801401-1.00007-4. [DOI] [PubMed] [Google Scholar]
- 6.Nomura M, Imai M, Takahashi K, Kumakura T, Tachibana K, Aoyagi S, et al. Three-site sandwich radioimmunoassay with monoclonal antibodies for a sensitive determination of human alpha-fetoprotein. J Immunol Methods. 1983;58:293–300. doi: 10.1016/0022-1759(83)90357-5. [DOI] [PubMed] [Google Scholar]