Abstract
We describe a case of bilateral cataract surgery in a 56-year-old man following presbyopia laser in situ keratomileusis. The preoperative refraction was −2.00 in the right eye and −0.75 × 105 in the left eye. On the last examination, the uncorrected distance visual acuity was 20/80 that can be corrected to 20/20 in the right eye with a refraction of −2.25 and 20/20 in the left eye, whereas the visual acuity for reading was 20/40 in the right eye and 20/80 in the left eye with a refraction of +2.25. His monovision surgery design of previous cornea surgery was also taken into consideration for the phacoemulsification and posterior chamber intraocular lens (IOL) implantation. Two-step surgery is helpful for predicting an accurate IOL degree.
Keywords: Presbyopia, Phacoemulsification, Laser in situ keratomileusis, Intraocular lens power calculation
Introduction
Laser in situ keratomileusis (LASIK) is a commonly performed refractive surgery of refractive errors. The intraocular lens (IOL) power calculation remains the most difficult part for these kinds of cataract surgery. Although numerous publications and studies have tackled the problem of IOL calculation in eyes after myopic keratorefractive surgery, very few studies have evaluated the IOL power after presbyopia LASIK. We report a case of bilateral cataract surgery following presbyopia LASIK in which the patient had different visual acuity demands for each eye.
Case report
A 56-year-old man presented to the cataract clinic for surgical evaluation and had bilateral presbyopia LASIK for 10 years without any historical data. The preoperative refraction was −2.00 in the right eye and −0.75 × 105 in the left eye, and the corrected distance visual acuity (CDVA) was 20/125 in the right eye and 20/40 in the left eye. Slit lamp examination revealed a clear cornea with posterior capsular opacity and a normal posterior segment in both eyes. The average keratometry (K) of the right eye was 46.62 diopters (D) in keratometer (Topcon, Japan), 46.32 D in corneal topography (Tomey Technology, Waltham, MA), and 46.33D in Scheimpflug imaging (Pentacam, Oculus Optikgeräte GmbH). The average K of left eye was 44.12 D in a partial coherence interferometry (PCI) biometer (IOL master, Zeiss), 43.91 D in corneal topography, and 43.70 D in Scheimpflug imaging. Scheimpflug imaging also revealed K-value of the central 4.5-mm area, which was 46.83 D in the right and 43.65 D in the left eye (Fig. 1). IOL master examination was unavailable for the right eye because of serious lens opacity.
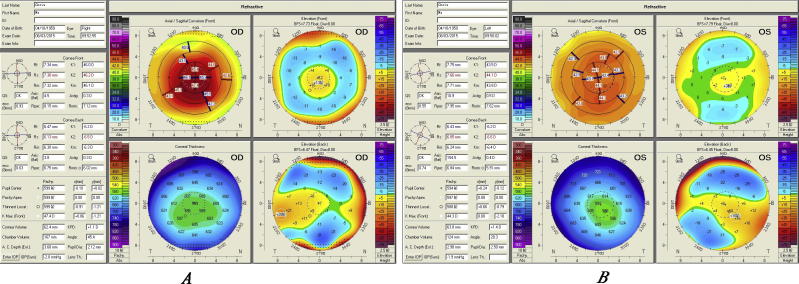
Figure 1.
Preoperative Scheimpflug imaging showing corneal topography after presbyopia LASIK in right eye (A) and left eye (B).
The patient expected his uncorrected visual acuity of the right eye to meet his need for reading and left eye for distance. There was not enough experience for the IOL power calculation following presbyopia LASIK, so a two-step surgery was considered for the right eye: IOL power was calculated after the first step of phacoemulsification, and then IOL implantation. After 3 weeks, the CDVA improved to 20/20 with a refraction of +9.50 D.
IOL power of the right eye was evaluated with following methods: SRK/T formula and Holladay 1 formula incorporated in A-scan with K-value of keratometer before phacoemlsification, SRK/T formula incorporated in IOL master after phacoemlsification, Holladay 1 formula incorporated in IOL master with K value of Scheimpflug imaging after phacoemlsification, IOL calculation online (Haigis-L, Shammes-PHL, Barrett Ture K formula available at ascrs.org) and Mackool algorithm of aphakic refraction technique.1 The IOL (Alcon SN60WF, A = 118.7) power was predicted as follows (Table 1).
Table 1.
Predicted IOL power of right eye calculated with different methods.
| Methods | K-value | Formula | Predicted IOL power (D) | |
|---|---|---|---|---|
| 1 | A-scan software | Keratometer | SRK/T | +18.5 |
| 2 | Holladay 1 | +18.0 | ||
| 3 | IOL master software | Keratometer | SRK/T | +18.5 |
| 4 | Pentacam | Holladay 1 | +17.5 | |
| 5 | iolcalc.ascrs.org | Pentacam | Haigis-L | +17.5 |
| 6 | Shammas-PHL | +16.6 | ||
| 7 | Barrett True K | +16.6 | ||
| 8 | Mackool algorithm | Aphakic Refraction (spherical Equivalent) × 1.75 | +16.5 | |
Considering his demands for reading, Lens of Alcon SN60WF +20.0 D was implanted and the refraction of −2.00 D was kept. After 3 months, the CDVA improved to 20/20 with a refraction of −2.25 D, the reading visual acuity was 20/40, and he felt comfortable when reading (Table 2).
Table 2.
Visual acuity and refractive after IOL implanted of right eye.
| Visit day | UCDVA | Refraction | CDVA | Reading VA | Refraction of reading VA |
|---|---|---|---|---|---|
| 1 d | 20/50 | −0.75/−1.25 × 90 | 20/25 | ||
| 30 d | 20/100 | −2.25 | 20/20 | 20/40 | PLANO |
| 90 d | 20/80 | −2.25 | 20/20 | 20/40 | −0.25 |
UCDVA: uncorrected distance visual acuity; VA: visual acuity.
Note that IOL A-constant of Mackool algorithm is 118.84 for emmetropia or mild myopia. No correction has been done because mild myopia could be achieved by the lower A-constant of 118.7 in contrast to 118.84, which the patient expected.
At the last visit, the refraction of the right eye was –2.25 D after surgery, so the precise IOL degree should be approximately 16.5–17.0 D if emmetropia.2 The aphakic refraction technique, Shammes-PHL, Barrett True K formula has demonstrated to provide an extremely accurate postoperative refractive result. The next was Holladay 1 and Haigis-L formula calculated with K value of Scheimpflug imaging. The discrepancies of other IOL degrees were near 2.00 D, which led to more myopia.
The cataract surgery of the left eye was performed later with the demand of good distance vision acuity. Because it is less possible to hyperopia according to above results, IOL degree (Alcon SN60WF) predicted directly by the Haigis-L(hyperopia) formula within IOL master software was 20.65 D for emmetropia, and then a lens of 21.0D was implanted. After 3 months, the patient obtained a good UCDVA for emmetropia (Table 3).
Table 3.
Visual acuity and refractive after phacoemulsification and IOL implanted of left eye.
| Visit day | UCDVA | Refraction | CDVA | Reading VA | Refraction of reading VA |
|---|---|---|---|---|---|
| 1 d | 20/25 | +0.50 | 20/25 | 20/125 | +2.75 |
| 30 d | 20/20 | PLANO | 20/20 | 20/80 | +2.25 |
| 90 d | 20/20 | +0.25 | 20/20 | 20/80 | +2.25 |
Discussion
Surgical correction of presbyopia is challenges for refractive surgeons. Now PresbyMAX was an effective surgery for the treatment of presbyopia based on the creation of a biaspheric, multifocal corneal surface with central area for near vision correction surrounded by an area calculated for distance, which will decrease the presbyopic symptoms and correct far distance refraction at the same time.3
Monovision is another extended technique for presbyopia. In this case, the monovision surgery design of presbyopia LASIK could be judged from the preoperative refraction: right eye focused for reading (nondominant eye) and left eye focused for distance (dominant eye). This patient has been comfortable with monovision for 10 year; therefore, the same design of cataract surgery should be taken into consideration. Three aspects about accurate IOL power calculation in cataractous eyes underwent hyperopic LASIK are important in the patient, as in other patients underwent myopia LASIK.4
-
1.
Evaluation of the correct post-LASIK K-values: In presbyopia or hyperopia LASIK, the corneal periphery is thinned out to steepen the central cornea. The measured corneal area of the device leads to the error between measured k-reading and actual k-reading. In this case, the K-values of corneal topography and Scheimpflug imaging revealed larger IOL power, which means that the correct K-values needed for accurate IOL power calculations were underestimated after presbyopia LASIK, which agrees with the conclusion of Shammas et al.5 Scheimpflug imaging was more accurate to evaluate the post-presbyopia LASIK corneal changes than topography because K-values of any point can be revealed, including the anterior and posterior corneal surface (Fig. 1). Clinical history method (CHM) is still considered the gold standard to estimate corneal power values after refractive surgery if K-values pre- and post-operation were precisely provided.6, 7 The minimal change in the required corneal power correction is the ratio between the anterior corneal radius and posterior corneal radius after hyperopic LASIK and is not as altered as after myopic LASIK,8, 9 thus, the error of calculated IOL power of a cataractous eye after hyperopic LASIK may be smaller than after myopic LASIK.
-
2.
IOL power calculation formulas: MacLaren et al.10 compared the accuracy of IOL power across different biometry formulae in extreme hyperopia and found the Haigis formula to be the most accurate, followed by the Hoffer Q, Holladay 1, and SRK/T formulae. The Haigis formula overpredicted the lens power required, which would have generated a myopic result. The other formula underpredicted the lens power required and would have generated a hyperopic error caused by the manner in which these formulas internally calculate the estimated lens position (ELP). Haigis-L formula can achieve effective corneal refraction, according to its corrected curve,11 and predict ELP without corneal curvature parameters, which is similar to CHM.12 However, Haigis-L formula is not suitable for an aphakia eye because the anterior chamber depth (ACD) is required. Shammas post-hyperopic LASIK (Shammas-PHL) formula was obtained from the Shammas original formula whether or not the pre-LASIK data are available because the corrected corneal power was calculated by adding the refractive change at the corneal level to the pre-LASIK keratometric readings.5 Barrett True K formula was based on a theoretical model eye in which anterior chamber depth is related to axial length and keratometry, which was found to be more accurate than the other third-generation formulas and maintained its accuracy for different lens styles and for eyes with short, medium, and long axial lengths.13 For this case, the target refraction of emmetropia was reached by Shammas-PHL, Barrett True K and Haigis-L formula with K-value of Scheimpflug imaging because IOL power error caused by K-value or ELP can be partly avoided.
-
3.
Optical biometry measurement: Measurement with ultrasound has been the historical standard for measurement of ocular parameters for IOL calculation, especially for a seriously opacity lens, while PCI-based optical biometry instruments may be more accurate when the fundus could be seen.11 The difference lies in the ocular length, but contributes to a smaller impact compared with K-values. The K-value with a Scheimpflug imaging device involves the anterior and posterior corneal power of the central, and the Central 4.5-mm area was selected according to the pupil diameter. Mackool algorithm was based on aphakic refraction technique derived from previous experiences with secondary IOL implantation,1 need only the refractive result of aphakia, providing an extremely accurate postoperative refraction in eyes having cataracts with IOL implantation surgery after previous myopia LASIK. It also predicted the most correct IOL power in this case involving presbyopia LASIK.
In summary, for accurate IOL calculations after hyperopic or presbyopia keratorefractive surgery, aphakic refraction technique achieved excellent IOL power predictability for the patients who are not willing to change IOL of poor degree and accept two-step surgery. Shammas-PHL, Barrett True K, and Haigis-L(hyperopia) formulae are recommended for one-step surgery, but the patient’s previous ocular refraction and vision demands should be taken into consideration. Further prospectively or retrospectively analyzed studies must be validated in post-presbyopia LASIK eyes, whether or not the pre-LASIK data are available.
Financial disclosure
No author has a financial or proprietary interest in any material or method mentioned.
Conflict of interest
Authors have no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Mackool R.J., Ko W., Mackool R. Intraocular lens power calculation after laser in situ keratomileusis: aphakic refraction technique. J Cataract Refract Surg. 2006;32:435–437. doi: 10.1016/j.jcrs.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 2.Haigis W. Intraocular lens calculation after refractive surgery for myopia: Haigis-L formula. J Cataract Refract Surg. 2008;34:1658–1663. doi: 10.1016/j.jcrs.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 3.Baudu P., Penin F., Arba Mosquera S. Uncorrected binocular performance after biaspheric ablation profile for presbyopic corneal treatment using AMARIS with the PresbyMAX module. Am J Ophthalmol. 2013;155:636–647. doi: 10.1016/j.ajo.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 4.Hodge C., McAlinden C., Lawless M., Chan C., Sutton G., Martin A. Intraocular lens power calculation following laser refractive surgery. Eye Vis (Lond) 2015;2:7. doi: 10.1186/s40662-015-0017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shammas H.J., Shammas M.C., Hill W.E. Intraocular lens power calculation in eyes with previous hyperopic laser in situ keratomileusis. J Cataract Refract Surg. 2013;39:739–744. doi: 10.1016/j.jcrs.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 6.Holladay J.T., Prager T.C., Chandler T.Y., Musgrove K.H., Lewis J.W., Ruiz R.S. A three-part system for refining intraocular lens power calculations. J Cataract Refract Surg. 1988;14:17–24. doi: 10.1016/s0886-3350(88)80059-2. [DOI] [PubMed] [Google Scholar]
- 7.Ladas J.G., Boxer Wachler B.S., Hunkeler J.D., Durrie D.S. Intraocular lens power calculations using corneal topography after photorefractive keratectomy. Am J Ophthalmol. 2001;132:254–255. doi: 10.1016/s0002-9394(01)00894-7. [DOI] [PubMed] [Google Scholar]
- 8.Seitz B., Langenbucher A. Intraocular lens calculations status after corneal refractive surgery. Curr Opin Ophthalmol. 2000;11:35–46. doi: 10.1097/00055735-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Langenbucher A., Haigis W., Seitz B. Difficult lens power calculations. Curr Opin Ophthalmol. 2004;15:1–9. doi: 10.1097/00055735-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 10.MacLaren R.E., Natkunarajah M., Riaz Y., Bourne R.R., Restori M., Allan B.D. Biometry and formula accuracy with intraocular lenses used for cataract surgery in extreme hyperopia. Am J Ophthalmol. 2007;143:920–931. doi: 10.1016/j.ajo.2007.02.043. [DOI] [PubMed] [Google Scholar]
- 11.Haigis W. Challenges and approaches in modern biometry and IOL calculation. Saudi J Ophthalmol. 2012;26:7–12. doi: 10.1016/j.sjopt.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haigis W., Lege B., Miller N., Schneider B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol. 2000;238:765–773. doi: 10.1007/s004170000188. [DOI] [PubMed] [Google Scholar]
- 13.Barrett G.D. An improved universal theoretical formula for intraocular lens power prediction. J Cataract Refract Surg. 1993;19:713–720. doi: 10.1016/s0886-3350(13)80339-2. [DOI] [PubMed] [Google Scholar]