Abstract
Background
PRK is a refractive surgery that reshapes the corneal surface by excimer laser photoablation to correct refractive errors. The effect of increased ultraviolet (UV) exposure on promoting post-PRK corneal haze has been reported in the literature; however, information is lacking regarding the effect of ambient UV exposure on physician practice patterns. The aim of this study was to evaluate the effect of ophthalmologists’ practice location on their reported practice patterns to prevent post-PRK corneal haze.
Methods
A cross-sectional observational study was conducted through an online survey sent to ophthalmologists performing PRK. The survey recorded the primary city of practice from which the two independent variables, latitude and average annual sunshine days, were determined. It also measured the frequency of use of postoperative preventive interventions (dependent variables) which are as follows: intraoperative Mitomycin-C, oral vitamin C, sunglasses, topical corticosteroids, topical cyclosporine, oral tetracyclines and amniotic membrane graft.
Results
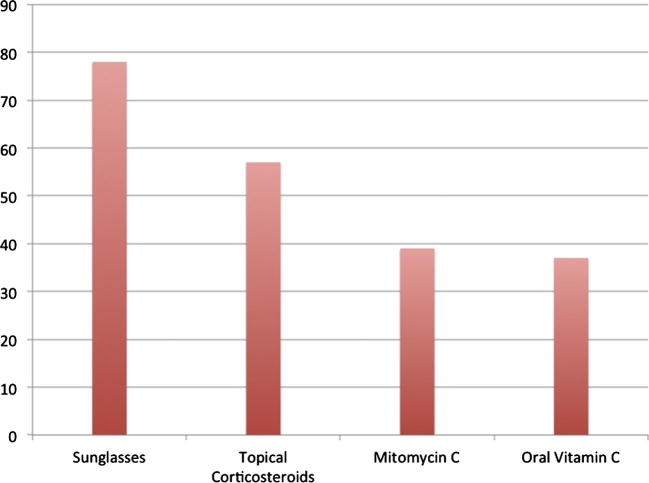
Fifty-one ophthalmologists completed the survey. Practice locations’ mean latitude was 36.4 degrees north, and average sunshine days annually accounted for 60% of year days. There was no significant relation between latitude/average annual sunshine days and usual post-PRK prophylactic treatments (P > 0.05). The commonest protective maneuvers were sunglasses (78%), prolonged topical corticosteroids (57%), Mitomycin-C (39%) and oral vitamin C (37%).
Conclusion
We found no significant difference in ophthalmologists’ practice patterns to prevent post-PRK corneal haze in relation to practice location latitude and average sunshine days. Moreover, the results demonstrated that the most widely used postoperative measures to prevent post-PRK haze are sunglasses, Mitomycin-C, topical corticosteroids, and oral Vitamin C.
Abbreviations: PRK, photorefractive keratectomy; UV, ultraviolet; IRB, Institutional Review Board
Keywords: Photorefractive keratectomy, Refractive surgery, Corneal haze, UV, Mitomycin
Introduction
Photorefractive Keratectomy (PRK) is a common refractive surgery that reshapes the corneal surface by excimer laser photoablation, aiming to effectively correct refractive errors while maintaining optimal corneal health and visual acuity. One of the major postoperative complications of this procedure is corneal haze that can jeopardize the quality of vision, especially during the initial postoperative months.1
Clinical and laboratory research into this issue has been performed in an attempt to determine the factors that contribute to the development of corneal haze, and how best to prevent it. Several modifying factors were introduced and are being used in clinical practice to improve post-PRK corneal transparency such as intraoperative application of mitomycin-C, in addition to the usual topical postoperative regimen including antibiotics, corticosteroids, non-steroidal anti-inflammatory drugs and oral vitamin C.2 Despite the introduction of these prophylactic treatments, a proportion of patients still develop corneal haze. Risk factors that increase the incidence and severity of corneal haze include high degrees of refractive errors and environmental factors such as ultraviolet (UV) light exposure.3 Several studies evaluated the correlation between the development of post-PRK corneal haze and increased exposure to UV light.3, 4 Nagy and colleagues4 conducted an experimental animal study to assess the clinical and microscopic effects of UV-B light exposure on photokeratectomized rabbit eyes. The authors compared photokeratectomized rabbit eyes with and without additional postoperative UV-B irradiation, and concluded that high UV-B exposure should be avoided during early healing phase. The authors proposed that it exerts an augmenting effect as it clinically aggravates corneal haze with prolongation of the stromal healing response microscopically. Additionally, Stojanovic and Nitter3 reported that the risk of late onset corneal haze (LOCH), haze occurring 4–12 months post-PRK, is higher in areas with more UV exposure and thus, encouraged wearing protective sunglasses in the first year after surgery. Taken together all these experimental and clinical studies provide solid evidence regarding the enhancing effect that UV light exposure has on the development of corneal haze after PRK. However, data correlating practice location as a surrogate for UV light exposure and practice patterns is still lacking in the literature. To the best of our knowledge, this study is the first to evaluate the relationship between location of performing PRK and ophthalmologists’ clinical practice patterns to prevent postoperative corneal haze. We hypothesized that clinical practice patterns to prevent post-PRK corneal haze are influenced by location of practice, justified by the fact that UV light exposure varies from one location to another.
Methods
This is a cross-sectional observational study conducted through an online survey sent to ophthalmologists performing PRK in different countries worldwide via the Cornea Society ListServ (Keranet) and the American Society of Cataract and Refractive Surgery ListServ. The survey recorded the primary city of practice from which the two independent variables, latitude and average annual sunshine days, were determined using Google search engine. The survey also measured the frequency of use of common postoperative preventive interventions (dependent variables) which are as follows: intraoperative Mitomycin-C, oral vitamin C, sunglasses, topical corticosteroids, topical cyclosporine, oral tetracyclines and amniotic membrane graft. Responses that did not include location of practice were not included in the analysis.
SPSS version 22.0 was used for data analysis. Descriptive statistics were calculated for all the options for each question for the latitude and average days of sunshine. If there were an adequate number of responses for each of the 3 options for a question then the Kruskal Wallis test was used to compare the latitude and average days of sunshine among them. If any option was chosen less than 5 times, it was merged with the next option and compared with the third option using Mann Whitney test. For example, for Intraoperative Mitomycin C, “Never or almost never” was selected only 2 times; it was merged with the next option “sometimes or in certain cases” and compared with “always or almost always”. Level of statistical significance was 0.05.
This survey was performed in adherence to the tenets of the Declaration of Helsinki. The Institutional Review Board of King Khaled Eye Specialist Hospital approved the survey, and potential respondents were informed that the anonymous composite results would be used for research. As the participants are all physicians that voluntarily responded to an email survey and were submitting information in an anonymous fashion, the IRB felt that obtaining local IRB ethics approval for each participant’s location would actually increase the risk of breach of privacy, and therefore was not indicated. The data set with location of practice was not submitted with the manuscript, as this could also jeopardize the privacy of the respondents.
Results
Fifty-one ophthalmologists responded to the survey. Table 1 details the descriptive data for latitude and average days of sunshine in the reported practice locations. Table 2 describes the data relating the two independent variables, practice location latitude and average annual sunshine days, to the frequency of usage of listed interventions to prevent post-PRK corneal haze. The most prevalent protective measure post-PRK was wearing sunglasses for UV protection, advised by more than three quarters (78.4%) of participating ophthalmologists “always or almost always”. Topical corticosteroid application after the first postoperative month was the second most common intervention recommended by more than half of the participants. Intraoperative Mitomycin-C accounted for the 3rd most commonly used protective intervention where less than 5% never/almost never used it. Less popular interventions included oral vitamin C, topical cyclosporine, oral tetracyclines and rarely amniotic membrane graft. Fig. 1 represents the relative frequencies of reported usage of these common protective measures.
Table 1.
Descriptive data for latitude and average days of sunshine.
| N | Mean | Median | Standard deviation | Minimum | Maximum | |
|---|---|---|---|---|---|---|
| Latitude | 51 | 36.4170 | 37.3000 | 8.83299 | 6.23 | 59.95 |
| Average days of sunshine per year | 51 | 218.5882 | 214.0000 | 38.18176 | 133.00 | 300.00 |
Table 2.
Descriptive data for postoperative interventions to prevent corneal haze in relation to the independent variables, latitude and average sunshine days.
| Frequency | Percent | Latitude |
Average sunshine days |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Median | P value | Min | Max | Median | p value | |||
| Intraoperative Mitomycin C | ||||||||||
| Never, sometimes or in certain cases | 26 | 47.1 | 19.92 | 59.95 | 39.73 | 152 | 265 | 211 | ||
| Always or almost always | 25 | 39.22 | 6.23 | 51.97 | 36.02 | 0.391 | 133 | 300 | 217 | 0.177 |
| Oral Vitamin C | ||||||||||
| Never or almost never | 19 | 41.2 | 6.23 | 47.62 | 35.23 | 152 | 292 | 214 | ||
| Sometimes or in certain cases | 7 | 13.7 | 17.37 | 51.97 | 39.73 | 0.677 | 133 | 300 | 214 | |
| Always or almost always | 18 | 37.3 | 19.92 | 59.95 | 38.69 | 160 | 281 | 206 | 0.92 | |
| Ultraviolet protection (e.g. sunglasses) | ||||||||||
| Never or almost never | 5 | 9.8 | 26.37 | 42.27 | 36.02 | 178 | 292 | 265 | ||
| Sometimes or in certain cases | 4 | 9.8 | 25.78 | 51.97 | 39.97 | 133 | 249 | 200 | ||
| Always or almost always | 35 | 78.4 | 6.23 | 59.95 | 36.00 | 0.692 | 152 | 300 | 214 | 0.189 |
| Topical corticosteroids beyond initial one month post-operative period | ||||||||||
| Never or Almost never | 9 | 19.6 | 19.92 | 59.95 | 36.02 | 196 | 292 | 214 | ||
| Sometimes or in certain cases | 9 | 17.6 | 25.78 | 46.88 | 34.00 | 167 | 284 | 197 | ||
| Always or almost always | 26 | 56.9 | 6.23 | 51.97 | 39.68 | 0.752 | 133 | 300 | 214 | 0.489 |
| Topical cyclosporine (e.g. Restasis) | ||||||||||
| Never or almost never | 28 | 54.9 | 6.2 | 59.9 | 38.19 | 133 | 300 | 214 | ||
| Sometimes or in certain cases | 17 | 33.3 | 5.5 | 45.70 | 31.40 | 0.381 | 167 | 284 | 208 | 0.338 |
| (or) always or almost always | ||||||||||
| Amniotic membrane graft | ||||||||||
| Never or almost never | 43 | 88.2 | 6.23 | 59.95 | 36.02 | 133 | 300 | 214 | ||
| Sometimes or in certain cases | 1 | 2 | n/a | n/a | ||||||
| Oral tetracycline, doxycycline or minocycline | ||||||||||
| Never or almost never | 35 | 68.6 | 6.23 | 59.95 | 36.02 | 152 | 300 | 214 | ||
| Sometimes or in certain cases | 10 | 19.6 | 32.47 | 51.97 | 39.58 | 0.375 | 133 | 284 | 199 | 0.332 |
| (or) always or almost always | ||||||||||
Figure 1.
The most commonly used treatments to prevent the development of corneal haze post-PRK, reported as % of respondents using “Always or almost always”.
Discussion
The augmenting effect of UV irradiation on corneal haze development was presented in several previous studies.2, 3, 4 This study investigated the impact of practice location on practice patterns to prevent post-PRK corneal haze and found no significant influence, although more than 50% of year days were sunny on average in practice cities. This could be attributed in part to the limited sample size in our study, which could be underpowered to find an association of smaller magnitude. In addition, one of the weaknesses of any survey is the non-random selection of ophthalmologists responding to the online survey. Variations in individual patient UV exposure, due to patient demographics and lifestyle or occupational factors, also cannot be controlled in a survey such as this. An additional uncontrolled variable is the surgeons’ indication for MMC (such as patient age, depth of ablation, or other factors) or application technique.
Mitomycin-C and corticosteroids were among the most commonly prescribed prophylactic treatments. Previously conducted experimental and clinical studies affirmed the success of Mitomycin-C in preventing haze occurrence.5, 6, 7, 8 It is noteworthy that only 2 respondents (4%) reported “Never or almost never” using intraoperative mitomycin. Nien and colleagues ascertained the efficacy of corticosteroids in reducing short-term post-PRK haze when its use was compared to cyclosporine.7 Therefore, we propose that the currently used methods of preventing corneal haze is effective, such that additional measures are not typically required, even in environments with higher UV exposure. Hence, the effectiveness of current surgical techniques and postoperative regimens could explain why practice location with greater UV exposure was not associated with an alteration in practice patterns.
Conclusion
In spite of the relation between UV light exposure and development of corneal haze, in this study we found no significant variance in ophthalmologists’ practice patterns to prevent post-PRK corneal haze based on practice location latitude and average days of sunshine. Moreover, the results demonstrated that the most widely used postoperative preventive measures are sunglasses, mitomycin-C, topical corticosteroids, and vitamin C. Oral tetracyclines and amniotic membrane grafts are being used infrequently. It remains to be determined which interventions are necessary and which are superfluous, to avoid unnecessary medications or lifestyle modifications. Such studies may still be best performed with consideration given to the ambient UV exposure, but a prospective randomized controlled trial will be required to definitively determine the effect of environmental UV irradiation upon any particular PRK regimen.
Conflict of interest
The Authors have no relevant financial or non-financial conflict of interest to disclose.
Author’s contributions
DUS participated in design of the study, interpretation of data, and revision of final manuscript. EMS participated in collection and interpretation of data and writing of the manuscript. Both authors approved the final manuscript.
Acknowledgements
The authors wish to thank Michael Wagoner D.O., the members of KeraNet (the Cornea Society ListServ) and the American Society of Cataract and Refractive Surgery ListServ for their participation. This data was presented in part at the European Society of Ophthalmology meeting, Vienna, June 2015.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Eman M. Al-Sharif, Email: eman.sharif@hotmail.com.
Donald U. Stone, Email: dstone@kkesh.med.sa.
References
- 1.Van de Pol C., Soya K., Hwang D.G. Objective assessment of transient corneal haze and its relation to visual performance after photorefractive keratectomy. Am J Ophthalmol. 2001;132:204–210. doi: 10.1016/s0002-9394(01)01003-0. [DOI] [PubMed] [Google Scholar]
- 2.Parekh P., Davis E. Prevention and treatment of haze. IOC. 2008;48:29–40. doi: 10.1097/IIO.0b013e31815f1ef2. [DOI] [PubMed] [Google Scholar]
- 3.Stojanovic A., Nitter T.A. Correlation between ultraviolet radiation level and the incidence of late-onset corneal haze after photorefractive keratectomy. J Cataract Refract Surg. 2001;27:404–410. doi: 10.1016/s0886-3350(00)00742-2. [DOI] [PubMed] [Google Scholar]
- 4.Nagy Z.Z., Hiscott P., Seitz B., Schlötzer-Schrehardt U., Süveges I., Naumann G.O. Clinical and morphological response to UV-B irradiation after excimer laser photorefractive keratectomy. Surv Ophthalmol. 1997;42(Suppl 1):S64–76. doi: 10.1016/s0039-6257(97)80028-8. [DOI] [PubMed] [Google Scholar]
- 5.Carones F., Vigo L., Scandola E., Vacchini L. Evaluation of the prophylactic use of mitomycin-C to inhibit haze formation after photorefractive keratectomy. J Cataract Refract Surg. 2002;28:2088–2095. doi: 10.1016/s0886-3350(02)01701-7. [DOI] [PubMed] [Google Scholar]
- 6.Shalaby A., Kaye G.B., Gimbel H.V. Mitomycin C in photorefractive keratectomy. J Refract Surg. 2009;25:S93–97. doi: 10.3928/1081597X-20090115-03. [DOI] [PubMed] [Google Scholar]
- 7.Nien C.J., Flynn K.J., Chang M., Brown D., Jester J.V. Reducing peak corneal haze after photorefractive keratectomy in rabbits: prednisolone acetate 1.00% versus cyclosporine A 0.05% J Cataract Refract Surg. 2011;37:937–944. doi: 10.1016/j.jcrs.2010.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vetrugno M., Maino A., Quaranta G.M., Cardia L. The effect of early steroid treatment after PRK on clinical and refractive outcomes. Acta Ophthalmol Scand. 2001;79:23–27. doi: 10.1034/j.1600-0420.2001.079001023.x. [DOI] [PubMed] [Google Scholar]