Abstract
Background
There is a high prevalence of non-adherence to immunosuppressants in kidney transplant recipients. Although limited health literacy is common in kidney recipients and is linked to adverse outcomes in other medical populations, its effect on medication adherence in kidney transplant recipients remains poorly understood. The objective was to investigate the effect of lower health literacy on immunosuppressant adherence.
Methods
Kidney recipients who were at least 6 months post-transplant and outpatients of Vancouver General Hospital in B.C., Canada were recruited through invitation letters. A total of 96 recipients completed the Health Literacy Questionnaire, which provides a multifactorial profile of self-reported health literacy and the Transplant Effects Questionnaire-Adherence subscale measuring self-reported immunosuppressant adherence. Hierarchical linear regression was used to analyze the association between health literacy and adherence after controlling for identified risk factors of non-adherence.
Results
Our sample was on average 53 years old, 56% male and 9 years post-transplant. Kidney recipients reported low levels of health literacy on scales measuring active health management and critical appraisal of information and 75% reported non-perfect adherence. Worse adherence was associated with poorer overall health literacy (ΔR2 = 0.08, P = 0.004) and lower scores on six of nine of the health literacy factors.
Conclusions
Poorer health literacy is associated with lower immunosuppressant adherence in adult kidney transplant recipients suggesting the importance of considering a recipient's level of health literacy in research and clinical contexts. Medication adherence interventions can target the six factors of health literacy identified as being risk factors for lower medication adherence.
Keywords: health literacy, medication adherence, immunosuppressant, kidney transplantation, quality of life
Introduction
In the USA there has been a 78% increase in kidney transplantation since 2000 [1], while in Canada the prevalence has more than doubled since 1994 [2]. In Europe the number of kidney transplants rose by 1.6% annually from 2001 [3]. Kidney transplant recipients must be prepared to follow a complex immunosuppressant regimen to prevent decreased organ functioning, graft rejection and graft loss [4–6]. In one literature review, non-adherence to medications was associated with 20 and 16% of late acute rejections and graft losses, respectively, although this was considered an underestimate [7]. Nonetheless, the prevalence of non-adherence in this population is high, with some estimates reporting more than one-third of kidney recipients as non-adherent to immunosuppressant medications [4, 7–9]. Adherence is defined as ‘the extent to which … [taking medication], corresponds with agreed recommendations from a healthcare provider.’ ([10], p.4). Although many risk factors for immunosuppressant non-adherence in kidney recipients have been identified (i.e. younger age, social isolation, higher depressive symptomatology, living transplants, longer time post-transplantation, full-time employment, diabetic status) [7, 11–13] several of these are fixed and not amenable to interventions.
Health literacy is defined as one's ability to access, process and understand health-related information and services in order to make good health decisions [14]. Limited health literacy is a world-wide problem: 60% of Canadians are identified as lacking sufficient health literacy skills [15], 36% of Americans live with limited health literacy [16] and in Europe an estimated 47% of individuals have poor health literacy [17]. Lower health literacy has been linked to worse disease outcomes in a variety of medical groups (e.g. [18–21]). Rates of limited health literacy in kidney disease range from 10 to 40% and have been associated with worse eGFRs in CKD, higher mortality rates in dialysis patients, and higher creatinine levels in transplant recipients and affect whether a patient is listed for or receives a transplant [22–28]. To our knowledge, the effect of limited health literacy on immunosuppressant medication adherence in kidney recipients has not been reported to date.
The World Health Organization (WHO) specifies that the abilities needed for adequate health literacy include both cognitive and social skills [29]. Although this definition places a focus on an individual's personal abilities, adequate health literacy additionally requires the efforts of the healthcare system, educational systems and society [14, 30], suggesting that although patients may present with a fixed cognitive set, modifications geared to facilitate interactions with a complex healthcare system may improve aspects of health literacy.
The objective of the present study was to examine the role of health literacy in immunosuppressant medication adherence in adults with successful kidney allograft functioning after controlling for the effect of other identified risk factors using a novel measure of health literacy that is in accordance with the WHO's definition. To extend previous literature and aid in guiding future interventions, we further explored which aspects of health literacy are risk factors for poorer medication adherence in this illness group.
Materials and methods
Study participants
In this observational study, psychosocial questionnaires were administered by trained research assistants to 96 kidney transplant recipients. Participants were outpatients of Vancouver General Hospital (VGH) in B.C., Canada. Data were collected between January 2011 and May 2014. Eligible participants met the following criteria: (i) ≥19 years; (ii) capable of giving informed consent; (iii) no impairments in vision, hearing, or other sensory or motor functions that might interfere with testing; (iv) English-language fluency and a minimum of sixth-grade education to ensure valid completion of questionnaires; (v) absence of active psychosis, major neurological disease (e.g. dementia) and other current major organ failure; and (vi) minimum 6 months post-transplant with a successful kidney graft and stable kidney functioning (i.e. determined by current eGFR above 14 mL/min/1.73 m2).
Participants were recruited through mailed study invitation letters and follow-up phone calls by trained research assistants. Patients who did not call our laboratory following receipt of the study invitation letter were followed up with phone calls until contact was made. Consecutive patients who met inclusionary criteria were invited to participate in the study session at the Cognitive Aging Laboratory in Simon Fraser University (SFU) or at VGH. Study sessions were independently scheduled with participants during the phone calls and involved meeting one-on-one with a graduate student research assistant to complete the study instruments. All participants received monetary compensation ($30) for their participation. The study was approved by the ethics boards of SFU and the University of British Columbia.
Measures
Clinical measures
For the purpose of characterizing the study population, all participants completed the Health Questionnaire, a self-report questionnaire querying medical history [31, 32]. Additional information (i.e. medications at the time of study, comorbid conditions and transplant history) was collected from participants' medical records at VGH by trained research assistants (Table 1). The most recent laboratory test results including hemoglobin levels (g/L), creatinine levels (µmol/L) and eGFRs (mL/min/1.73 m2) prior to the study session were also collected. Study sessions occurred within 1 month of the laboratory results.
Table 1.
Demographic and clinical characteristics of the study sample
| Participant characteristics | N = 96 |
|---|---|
| Age | 24–81 years, 52.77 ± 12.56 |
| Gender: female | 42 (43.8) |
| Ethnicity | |
| Caucasian | 60 (62.5) |
| Asian | 24 (25) |
| Other | 12 (12.5) |
| Education | 13.97 ± 2.40 |
| Current employment (at least 20 h/week) | 47 (49) |
| eGFR (mL/min/1.73 m2) | 56.62 ± 20.21 |
| Hemoglobin (g/L) | 129.54 ± 16.02 |
| Creatinine (µmol/L) | 119.51 ± 47.71 |
| Smoke cigarettes: yes | 3 (3.1) |
| Hypertension: yes | 69 (71.9) |
| Diabetes mellitus: yes | 23 (24.2) |
| Hypercholesterolemia: yes | 29 (30.5) |
| Heart attack history: yes | 7 (7.4) |
| Antidepressants: yes | 11 (11.6) |
| Benzodiazepines: yes | 7 (7.4) |
| Opiates: yes | 2 (2.1) |
| Lipid-lowering agents: yes | 39 (41.1) |
| Anti-hypertensives: yes | 67 (70.5) |
| Glucose-normalizing medications: yes | 15 (15.8) |
| Calcineurin inhibitor type | |
| Cyclosporine: yes | 9 (9.4) |
| Tacrolimus: yes | 75 (78.1) |
| Transplant history | |
| Time since transplant | 8.81 ± 7.00 |
| Kidney and pancreas transplant | 12 (12.5) |
| Number of kidney transplants | |
| One Transplant | 89 (92.7) |
| Two Transplants | 7 (7.3) |
| Dialysis history | |
| Hemodialysis | 43 (44.8) |
| Peritoneal dialysis | 29 (30.2) |
| Both | 10 (10.4) |
| Time spent on dialysis | 2.54 ± 2.46 |
| Deceased donora | 49 (51) |
| Previously on dialysis | 49 (100) |
| Living donor | 47 (49) |
| Previously on dialysis | 33 (70.2) |
Values for continuous variables are expressed as mean ± SD, categorical variables are number (%).
aDeceased versus living donors previously on dialysis: x2 = 17.09, P < 0.01. Normal ranges of hemoglobin (g/L) are 120–140 g/L for females and 140–160 g/L for males. Normal ranges of creatinine (µmol/L) are 60–110 µmol/L for females and 70–120 µmol/L for males.
Sociodemographic characteristics
Demographic information was collected at the time of the study. Depressive symptomatology was indexed with the total raw score from the Center for Epidemiological Studies Depression Scale (CES-D [33]), which is a 20-item inventory with responses rated on a 4-point Likert-type scale ranging from 0 (rarely) to 3 (most/all of the time). Higher scores indicate a greater number of depressive symptoms, with scores higher than 15/60 suggesting clinically significant depression. Responses to the CES-D have been found to have good reliability for persons with kidney disease (Cronbach's α = 0.87) and to be a valid measure of depressive symptoms in this population [34].
Health literacy measure
We used the Health Literacy Questionnaire (HLQ) [35], which is a self-report measure assessing the skills needed for adequate health literacy encompassing the WHO's definition [29]. The HLQ was validated on large samples of healthcare professionals, patients, community members and policy makers with robust psychometric analysis conducted including confirmatory structural equation modeling and item difficulty to arrive at the 44-item questionnaire with nine psychometrically distinct factors, each with 4–6 items which have acceptable to high reliability (r = 0.77–0.90) (Table 2). While not validated on the kidney disease population specifically, the HLQ has been validated on a general medical population with conditions represented by patients including heart disease and diabetes. Items are rated based on degree of agreement on a 4-point Likert-type scale (1: strongly disagree to 4: strongly agree) or difficulty on a 5-point Likert-type scale (1: cannot do to 5: very easy), such that higher scores indicate better health literacy. We used the HLQ total score, the factor total scores and the factor mean scores for analysis.
Table 2.
Health Literacy Questionnaire Scales
| Scales | Number of items |
|---|---|
| 1. Feeling understood and supported by healthcare providers | 4 |
| 2. Having sufficient information to manage my health | 4 |
| 3. Actively managing my health | 5 |
| 4. Social support for my health | 5 |
| 5. Appraisal of health information | 5 |
| 6. Ability to actively engage with healthcare professionals | 5 |
| 7. Navigating the healthcare system | 6 |
| 8. Ability to find good information | 5 |
| 9. Understanding health information well enough to know what to do | 5 |
Scales 1–5 are rated on a 4-point Likert-type scale (1: strongly disagree to 4: strongly agree) and scales 6–9 are rated on a 5-point Likert-type scales (1: cannot do to 5: very easy).
Medication adherence measure
Medication adherence was measured using the Adherence subscale of the Transplant Effects Questionnaire (TxEQ) [36], which has five distinct and uncorrelated subscales confirmed through factor analysis. The Adherence subscale queries behavioral responses to immunosuppressant medication adherence and comprises five statements rated on a 5-point Likert-type scale (1: strongly agree to 5: strongly disagree) yielding a total score ranging from 5 to 25, with higher scores indicating higher self-reported adherence. Frazier et al. indicated that measurement of non-adherence to medication regimens is improved by treating adherence as a continuous variable, a recommendation fulfilled by the TxEQ [37]. The Adherence subscale total score was used for analyses. The specific items are: ‘Sometimes I think I do not need my anti-rejection medicines;’ ‘Sometimes I forget to take my anti-rejection medicines;’ ‘I find it difficult to adjust to taking my prescribed anti-rejection drug regime;’ ‘When I am too busy I may forget my anti-rejection medicines;’ and ‘Sometimes I do not take my anti-rejection medicines.’ As such, the TxEQ provides insight into the reasons for non-adherence, which facilitates development of an action plan for intervention. The TxEQ was validated on kidney recipients [36]. Previous research has found the TxEQ-Adherence subtest to have adequate internal consistency (Cronbach's α = 0.79) and test–retest reliability (r = 0.77) [36].
Statistical analyses
Prescreening for regression and partial correlational analyses
Based on previous literature demonstrating relationships with either health literacy or adherence [7, 11–15], we examined the association between the following variables using Pearson and point biserial correlations: (i) demographic variables: age, gender, education years, employment status (<20 hours/week versus ≥20), ESL, ethnicity (Caucasian versus other) and marital status; (ii) illness variables: depressive symptoms, time since transplantation, donor type (cadaveric versus living) and diabetes (no diabetes versus current/history of diabetes), eGFR, creatinine and hemoglobin levels; (iii) health literacy variables: the total HLQ variable and HLQ factor total scores; and (iv) TxEQ.
Analyses were conducted using SPSS 20. Hierarchical multiple linear regression was used to model the association of health literacy (HLQ total score) with medication adherence (TxEQ). The relationship between health literacy and self-reported medication adherence was further examined through partial correlations between each HLQ total factor score and TxEQ. Only variables that were associated with either health literacy or TxEQ at an a priori alpha level of P ≤ 0.05 were controlled for in regression and partial correlational analyses.
Power analysis and variable transformation
A priori power analysis revealed that for an alpha level of 0.05 and a statistical power of 0.80 to control for type I and type II errors, respectively, N of 91 would be sufficient to detect a medium effect size with five predictors in the regression model [38]. Transformations were applied to the CES-D (square root transformation; positively skewed) and the TxEQ (reflection and square root transformation; negatively skewed) to meet the criterion of distributional normality required for regression analyses. Results of the correlational and regression analyses are presented using transformed variables.
Results
Study population
Demographic and clinical characteristics of the study sample are shown in Table 1. One-hundred and fifty transplant recipients were contacted for recruitment. Ninety-six met inclusion criteria and participated in the study. Twenty-two declined to participate and 32 did not meet inclusion criteria. Recruitment success rate was ∼64%. This recruitment rate and demographic profile is consistent with that of previous studies assessing various outcomes of kidney transplantation in our lab [31, 32].
Performance on questionnaires
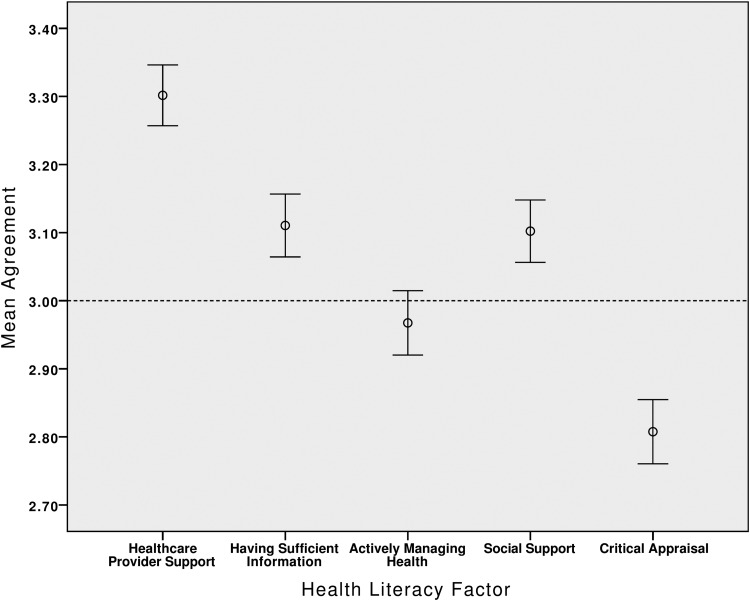
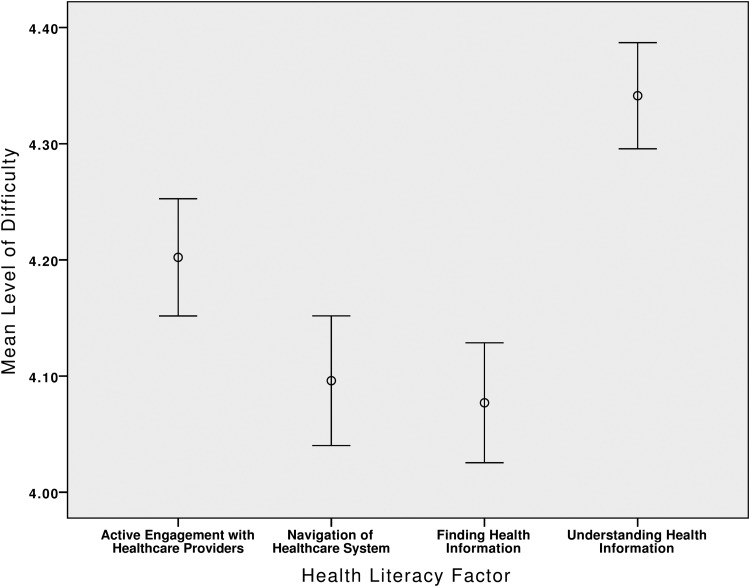
The mean score on the CES-D was 8.58 (SD = 6.95) and 16.7% of participants were classified as having clinically significant symptoms of depression (scores ≥ 16). The mean total HLQ score was 157.69 (SD = 1.60, range = 112–197). Performance on the individual HLQ domains was compared individually for scales 1 through 5 and scales 6 through 9. See Figures 1 and 2 for a profile of strengths and weaknesses across health literacy factors for our sample. On the TxEQ the total score ranged from 13 to 25 (M = 20.89, SD = 3.77), and 74 individuals (75%) achieved a score indicating less than ‘perfect’ self-reported adherence (score <25; <100%). The internal consistency for our sample was adequate (coefficient α = 0.79).
Fig. 1.
Mean degree of agreement (68% confidence interval) to having adequate levels of health literacy across various scales (scales 1–5) of the HLQ. Scale responses range from 1 (strongly disagree) to 4 (strongly disagree). On average, patients were in agreement that they had adequate healthcare provider support, sufficient information and good general social support (mean scores are all above 3 indicating that they are within the ‘Agreement’ range on the Likert-type scale). In contrast, transplant recipients achieved lower mean scores in the domains of actively managing health and critical appraisal of health information (mean scores below 3, i.e. within the ‘Disagreement’ range on the Likert-type scale).
Fig. 2.
Mean degree of difficulty (68% confidence interval) to various tasks comprising four of the health literacy scales (scales 6–9). Scale responses range from 1 (cannot do) to 5 (very easy). Transplant recipients reported high levels of ease for their ability to actively engage with healthcare providers, navigate the healthcare system, find good health information, and read and understand that information (mean scores are all above 4 indicating that they are within the ‘Easy’ range on the Likert-type scale).
Regression and partial correlational analyses: prescreening and results
Younger age (r = −0.22, P < 0.05), male gender (r = −0.34, P < 0.001), higher levels of employment (r = 0.20, P < 0.05) and lower total HLQ levels (r = −0.35, P < 0.001) were each significantly associated with poorer self-reported medication adherence. A higher level of depressive symptoms (r = −0.44, P < 0.001) was significantly associated with poorer performance on the HLQ and all individual factors of the HLQ. Having a spouse (r = 0.28, P < 0.01) was significantly associated with higher general social support on the HLQ. Further, being Caucasian (r = −0.22, P < 0.05) and having lower creatinine levels (r = −0.22, P < 0.05) were each significantly associated with a better ability to critically appraise information on the HLQ. Having English as a first language (r = 0.30, P < 0.01) and a higher eGFR (r = 0.22, P < 0.05) were each associated with a better ability to read and understand health information on the HLQ. None of the transplant history factors were associated with adherence.
After accounting for age, gender, employment status and depressive symptoms, decreased total health literacy was associated with decreased medication adherence (ΔR2 = 0.08, P = 0.004; Table 3). The overall model explained 19% of the variance in adherence (95% CI 0.03–0.31, P = 0.002). Both male gender (β = −0.27, P < 0.01) and lower health literacy (β = −0.31, P < 0.01) were significantly associated with poorer medication adherence in our regression model.
Table 3.
Regression analysis examining the relationship between health literacy and self-reported medication adherence
| Predictor variables | Block 1 | Block 2 | Block 3 | |||||
|---|---|---|---|---|---|---|---|---|
| β | β | β | F | R2 | ΔR2 | P | ΔF | |
| Block 1 | ||||||||
| Age | −0.15 | −0.13 | −0.13 | |||||
| Gender | −0.30** | −0.28** | −0.27** | |||||
| Employment | 0.05 | 0.06 | 0.05 | 4.96** | 0.12 | |||
| Block 2 | ||||||||
| CES-D | 0.12 | −0.02 | 4.09** | 0.12 | 0.01 | 1.42 | ||
| Block 3 | ||||||||
| HLQ | −0.31** | 5.35*** | 0.19 | 0.08 | 0.004 | 8.91** | ||
*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001. CES-D = Center for Epidemiological Studies Depression Scale (transposed); regression analysis with transposed CES-D and TxEQ variables. F-values represent the ANOVA for the full model. F change indicates the contribution of each additional block (i.e. the variable added in Block 2 and Block 3). Degrees of freedom for the F test on the full model = (5, 86). Effect size magnitude: small effect size 0.02 ≤ R2 < 0.15; medium effect size: 0.15 ≤ R2 < 0.35; large effect size: R2 ≥ 0.35.
Six out of the nine factors emerged as [39] significantly correlated with self-reported medication adherence (Table 4). In each case, lower scores on these factors were related to poorer medication adherence.
Table 4.
Partial correlations between HLQ scales and self-reported medication adherence
| Variable | Self-reported medication adherence (TxEQ) |
|---|---|
| 1. General social support | −0.35*** |
| 2. Having sufficient information | −0.33** |
| 3. Reading and understanding health information | −0.29** |
| 4. Navigating healthcare system | −0.28** |
| 5. Active engagement | −0.26* |
| 6. Healthcare provider support | −0.24* |
| 7. Finding good health information | −0.18 |
| 8. Actively managing health | −0.07 |
| 9. Critical appraisal | 0.08 |
*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001. Partial correlations between each of the HLQ total factor scores and self-reported medication adherence (TxEQ) controlling for the effect of age, gender, employment status and depressive symptoms. Variables that were uniquely associated with any one health literacy factor were additionally controlled for. These included: (i) marital status for the General Social Support factor; (ii) creatinine levels and ethnicity for the Critical Appraisal factor; (iii) ESL status and eGFR for the Reading and Understanding Health Information factor. These factors are rank-ordered by effect size magnitude (medium effect size: 0.30 ≤ r < 0.50; small effect size: 0.10 ≤ r < 0.30).
Discussion
We extended previous research by: (i) demonstrating that lower levels of health literacy are linked to poorer medication adherence in adult kidney transplant recipients with successful graft functioning and (ii) identifying specific factors of health literacy that are potential risk factors for poorer medication adherence. Our findings are consistent with that from a recent meta-analysis, which found a significant and positive relationship between health literacy and adherence with a 14% increased risk of non-adherence in those with lower health literacy [39]. Non-adherence rates were 1.33 times greater in those with limited health literacy [39]. A unique aspect of this study is the demonstration of this relationship with the HLQ, which is a contemporary tool compared to those used in previous studies (e.g. TOFHLA, REALM and NVS; [40, 41]). While assessing literacy within a health context, these older measures do not directly address the role of system-level factors in influencing health literacy, nor do they address the social skills embodied within the WHO's contemporary definition [29]. Rather, they focus on select cognitive abilities (i.e. fluency, numeracy) that contribute to health literacy. As such, although these older measures provide a proxy for how patients may interact with medical text and have demonstrated associations with medical outcomes [18–21, 23–27, 42], they do not comprehensively capture the current conceptualization of health literacy. Further, potential for interventions is limited because performance on each of these measures can only provide an indication of an individual's reading level [30, 43].
From a clinical perspective, Ferguson indicates that when evaluating the practical significance of effect sizes, the gravity of the outcome in question as well as the quality of the measurement should be considered [44]. In this case, non-adherence and its associated complications of morbidity and potential mortality [4–6] suggest that the medium effect size observed in the current study is highly significant from a practical perspective. In addition, we used well-validated self-report instruments of health literacy [35] and adherence [36], further adding to the practical significance (i.e. observability in real life) of our findings.
We took into consideration a number of other risk factors that have demonstrated associations with non-adherence and, consistent with past literature [7, 45], found male gender to be associated with lower self-reported immunosuppressant adherence. It is possible that certain personality traits that females tend to endorse more frequently (i.e. conscientiousness) [46] motivate better adherence to medication instructions. As such, the association between gender, personality and adherence warrants further exploration. As our model does not account for all of the variance in adherence, future research should examine the potential contribution of other variables (e.g. cognitive difficulties, personality, self-efficacy).
Practical implications
We were able to identify specific factors of health literacy that demonstrated significant relationships with medication adherence. Out of the nine factors measured by the HLQ, six emerged as important risk factors of medication non-adherence in kidney transplantation. Denhaerynck et al. [7, 45] outline a bias in past literature that examines non-adherence at a patient-specific level and assert that healthcare system predictors are seldom examined, thus limiting the potential for interventions to be targeted beyond the individual. The current findings suggest that health literacy is a potentially modifiable risk factor that can be targeted at both an individual (patient-specific) and organizational (healthcare system) level [35]. Thus, educating healthcare providers in understanding the multifaceted nature of health literacy and in detecting indicators of low health literacy (beyond poor reading ability) may lead to improved outcomes for kidney recipients. Further, the current findings suggest that interventions should target the health literacy domains with the strongest associations with adherence, specifically: (i) accessing and bolstering social support for living with a kidney transplant and (ii) ensuring patients are equipped with sufficient information to manage their health.
Limitations
These results should be considered in light of certain limitations. First, our sample was on average 9 years post-transplantation. While it may be argued that these patients have demonstrated the ability to adhere to transplant requirements given their surviving grafts, we note our sample's reasonable representation of those more recently transplanted and the high prevalence of self-reported non-adherence. The reader is reminded of the risks associated with non-adherence [7, 8] and that non-adherence rates increase with time post-transplantation [47, 48]. Given the study's use of self-report measures, problems with positive impression management may have led to an overestimate of the level of health literacy and adherence. Other means are not without their limitations—for example, when scheduled, participants can easily adjust their pill count to appear more adherent and pharmacy refill records assume that patients refilling in a timely manner are adherent. Electronic monitoring is often undesired by participants due to the bulky nature of bottles and therefore susceptible to ‘pocket dosing’ or technology failure [49]. It is interesting to note that research has demonstrated a higher prevalence of non-adherence as detected through self-report measures in comparison to other means, including electronically monitored levels [7, 9], suggesting that underreporting of non-adherence can be reduced via confidential reporting as used in the current study. Given their ease of administration, cost-effectiveness and sensitivity, self-report measures remain a popular choice for many researchers [7–9, 12, 50]. Having demonstrated the relationship between medication adherence and health literacy, the next step will be to include objective measures of medication adherence to be able to examine health literacy levels across different degrees of non-adherence.
Summary
Our study identified a previously neglected risk factor of medication non-adherence in adult kidney transplant recipients through the use of a comprehensive and contemporary measure of health literacy. Findings that lower health literacy is associated with poorer immunosuppressant adherence suggest that it will be important to consider a recipient's level of health literacy in future research and clinical contexts. These findings additionally highlight the potential role of six HLQ factors in facilitating adherence post-transplantation and can help guide future interventions for immunosuppressant adherence.
Conflict of interest statement
The authors of this manuscript have no conflicts of interest to disclose, and the results of this paper have not been published previously in whole or part, except in abstract form.
Acknowledgements
This study was supported by grants from the Canadian Institutes of Health Research Training Grant in Transplantation to M.N.D. and Astellas Pharma Canada funding to R.J.S. (H11-00446). We are grateful to the staff and participants of the SFU Cognitive Aging Laboratory and the Solid Organ Transplant program at VGH. We are grateful to Dr Allen E. Thornton for providing his statistical expertise.
References
- 1.Saran R, Li Y, Robinson B et al. US Renal Data System 2014 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2015; 66(1 Suppl 1): Svii, S1–S305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Institute for Health Information. Canadian organ replacement register annual report: Treatment of end-stage organ failure in Canada, 2004 to 2013. 2014; (April): 1–129. doi:https://secure.cihi.ca/free_products/2011_CORR_Annua_Report_EN.pdf
- 3.Pippias M, Jager KJ, Kramer A et al. The changing trends and outcomes in renal replacement therapy : data from the ERA-EDTA Registry. Nephrol Dial Transplant 2016; 31: 831–841 [DOI] [PubMed] [Google Scholar]
- 4.Butler JA, Roderick P, Mullee M et al. Frequency and impact of nonadherence to immunosuppressants after renal transplantation: a systematic review. Transplantation 2004; 77: 769–776. http://www.ncbi.nlm.nih.gov/pubmed/15021846 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 5.Fine RN, Becker Y, De Geest S et al. Nonadherence consensus conference summary report. Am J Transplant 2009; 9: 35–41 [DOI] [PubMed] [Google Scholar]
- 6.Pinsky BW, Takemoto SK, Lentine KL et al. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Am J Transplant 2009; 9: 2597–2606 [DOI] [PubMed] [Google Scholar]
- 7.Denhaerynck K, Dobbels F, Cleemput I et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int 2005; 18: 1121–1133 [DOI] [PubMed] [Google Scholar]
- 8.Dew MA, DiMartini AF, De Vito Dabbs A et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation 2007; 83: 858–873 [DOI] [PubMed] [Google Scholar]
- 9.Butler JA, Peveler RC, Roderick P et al. Measuring compliance with drug regimens after renal transplantation: comparison of self-report and clinician rating with electronic monitoring. Transplantation 2004; 77: 786–789. http://www.ncbi.nlm.nih.gov/pubmed/15021850 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Adherence to Long-term Therapies. Geneva, Switzerland: Author, 2003
- 11.Achille MA, Ouellette A, Fournier S et al. Impact of stress, distress and feeling of indebtedness on adherence to immunosuppressants following kidney transplantation. Clin Transplant 2006; 20: 301–306 [DOI] [PubMed] [Google Scholar]
- 12.Gelb SR, Shapiro RJ, Thornton WJL. Predicting medication adherence and employment status following kidney transplant: the relative utility of traditional and everyday cognitive approaches. Neuropsychology 2010; 24: 514–526 [DOI] [PubMed] [Google Scholar]
- 13.Goldfarb-Rumyantzev AS, Wright S, Ragasa R et al. Factors associated with nonadherence to medication in kidney transplant recipients. Nephron Clin Pract 2010; 117: 33–40 [DOI] [PubMed] [Google Scholar]
- 14.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press, 2004 [PubMed] [Google Scholar]
- 15.Canadian Council on Learning. Health Literacy in Canada: A Healthy Understanding. Ottawa, Ontario: Author, 2008.
- 16.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483). U.S. Department of Education. Washington, DC: National Center for Education Statistics, 2006. [Google Scholar]
- 17.HLS-EU Consortium (2012): Comparative Report of Health Literacy in eight EU member states. The European Health Literacy Survey HLS-EU. http://WWW.HEALTH-LITERACY.EU
- 18.Estrada CA, Martin-Hryniewicz M, Peek BT et al. Literacy and numeracy skills and anticoagulation control. Am J Med Sci 2004; 328: 88–93. http://www.ncbi.nlm.nih.gov/pubmed/15311167 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 19.Gazmararian JA, Williams MV, Peel J et al. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003; 51: 267–275 [DOI] [PubMed] [Google Scholar]
- 20.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med 2005; 118: 371–377 [DOI] [PubMed] [Google Scholar]
- 21.Schillinger D, Grumbach K, Piette J et al. Association of health literacy with diabetes outcomes. JAMA 2016; 288: 475–482. http://www.ncbi.nlm.nih.gov/pubmed/12132978 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 22.Devraj R, Borrego M, Vilay AM et al. Relationship between health literacy and kidney function. Nephrology (Carlton) 2015; 20: 360–367 [DOI] [PubMed] [Google Scholar]
- 23.Cavanaugh KL, Wingard RL, Hakim RM et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010; 21: 1979–1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon EJ, Wolf MS. Health literacy skills of kidney transplant recipients. Prog Transplant 2009; 19: 25–34. http://www.ncbi.nlm.nih.gov/pubmed/19341060 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 25.Escobedo W, Weismuller P. Assessing health literacy in renal failure and kidney transplant patients. Prog Transplant 2013; 23: 47–54 [DOI] [PubMed] [Google Scholar]
- 26.Chisholm MA, Fair J, Spivey CA. Health literacy and transplant patients and practitioners. Public Health 2007; 121: 800–803 [DOI] [PubMed] [Google Scholar]
- 27.Kazley AS, Hund JJ, Simpson KN et al. Health literacy and kidney transplant outcomes. Prog Transplant 2015; 25: 85–90 [DOI] [PubMed] [Google Scholar]
- 28.Grubbs V, Gregorich SE, Perez-Stable EJ et al. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 2009; 4: 195–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Health Promotion Glossary. Geneva, Switzerland: Author, 1998 [Google Scholar]
- 30.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med 2006; 21: 878–883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gelb S, Shapiro RJ, Hill A et al. Cognitive outcome following kidney transplantation. Nephrol Dial Transplant 2008; 23: 1032–1038 [DOI] [PubMed] [Google Scholar]
- 32.Thornton WL, Shapiro RJ, Deria S et al. Differential impact of age on verbal memory and executive functioning in chronic kidney disease. J Int Neuropsychol Soc 2007; 13: 344–353 [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401 [Google Scholar]
- 34.Paterson TSE, O'Rourke N, Elmer E et al. The composition and structure of depressive symptomatology in renal disease. Can J Behav Sci Can des Sci du Comport 2011; 43: 318–327 [Google Scholar]
- 35.Osborne RH, Batterham RW, Elsworth GR et al. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013; 13: 658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ziegelmann JP, Griva K, Hankins M et al. The Transplant Effects Questionnaire (TxEQ): the development of a questionnaire for assessing the multidimensional outcome of organ transplantation - example of end stage renal disease (ESRD). Br J Health Psychol 2002; 7(Part 4): 393–408 [DOI] [PubMed] [Google Scholar]
- 37.Frazier PA, Davis-Ali SH, Dahl KE. Correlates of noncompliance among renal transplant recipients. Clin Transplant 1994; 8: 550–557. http://www.ncbi.nlm.nih.gov/pubmed/7865918 (2 April 2016, date last accessed) [PubMed] [Google Scholar]
- 38.Cohen J. A power primer. Psychol Bull 1992; 112: 155–159 [DOI] [PubMed] [Google Scholar]
- 39.Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns 2016; 99: 1079–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Green JA, Mor MK, Shields AM et al. Prevalence and demographic and clinical associations of health literacy in patients on maintenance hemodialysis. Clin J Am Soc Nephrol 2011; 6: 1354–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parker RM, Baker DW, Williams MV et al. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med 1995; 10: 537–541. http://www.ncbi.nlm.nih.gov/pubmed/8576769 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 42.Omachi TA, Sarkar U, Yelin EH et al. Lower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary disease. J Gen Intern Med 2013; 28: 74–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jordan JE, Osborne RH, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J Clin Epidemiol 2011; 64: 366–379 [DOI] [PubMed] [Google Scholar]
- 44.Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract 2009; 40: 532–538 [Google Scholar]
- 45.Denhaerynck K, Steiger J, Bock A et al. Prevalence and risk factors of non-adherence with immunosuppressive medication in kidney transplant patients. Am J Transplant 2007; 7: 108–116 [DOI] [PubMed] [Google Scholar]
- 46.Costa PT, Terracciano A, McCrae RR. Gender differences in personality traits across cultures: robust and surprising findings. J Pers Soc Psychol 2001; 81: 322–331. http://www.ncbi.nlm.nih.gov/pubmed/11519935 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 47.Siegal BR, Greenstein SM. Postrenal transplant compliance from the perspective of African-Americans, Hispanic-Americans, and Anglo-Americans. Adv Ren Replace Ther 1997; 4: 46–54. http://www.ncbi.nlm.nih.gov/pubmed/8996620 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 48.Greenstein S, Siegal B. Odds probabilities of compliance and noncompliance in patients with a functioning renal transplant: a multicenter study. Transplant Proc 1999; 31: 280–281. http://www.ncbi.nlm.nih.gov/pubmed/10083108 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]
- 49.Grant I, Adams KM (eds). Neuropsychological Assessment of Neuropsychiatric and Neuromedical Disorders 3rd ed. New York: Oxford, 2009
- 50.De Geest S, Vanhaecke J. Methodological issues in transplant compliance research. Transplant Proc 1999; 31(4A): 81S–83S. http://www.ncbi.nlm.nih.gov/pubmed/10372057 (2 April 2016, date last accessed) [DOI] [PubMed] [Google Scholar]