Abstract
The Medical Informatics Network Tool (MINT) is a software system that supports the management of care for chronic illness. It is designed to improve clinical information, facilitate teamwork, and allow management of health care quality. MINT includes a browser interface for entry and organization of data and preparation of real-time reports. It includes personal computer–based applications that interact with clinicians. MINT is being used in a project to improve the treatment of schizophrenia. At each patient visit, a nurse briefly assesses symptoms, side effects, and other key problems and enters this information into MINT. When the physician subsequently opens the patient's electronic medical record, a window appears with the assessment information, a messaging interface, and access to treatment guidelines. Clinicians and managers receive reports regarding the quality of patients' treatment. To date, MINT has been used with more than 165 patients and 29 psychiatrists and has supported practices that are consistent with improvements in the quality of care.
Schizophrenia is a chronic brain disorder that occurs in about 1% of the population and manifests as symptoms of psychosis and disorganized thinking. It accounts for 10% of all permanently disabled people and 3,200 premature deaths annually in the United States.1 During the past two decades, there have been dramatic advances in the treatment of schizophrenia. New medications can improve symptoms and quality of life while causing fewer unpleasant side effects. Structured psychosocial treatments allow severely ill people to live successfully in the community and markedly improve their functioning. Unfortunately, the majority of people with schizophrenia are not receiving appropriate care.2 While state governments spend approximately $16 billion per year on public mental health services for adults, outcomes under typical care are much worse than in state-of-the-art care. Quality problems are prevalent nationally in provider organizations, including the Department of Veterans Affairs (VA).
To address this problem, the VA Health Services Research and Development service and Quality Enhancement Research Initiative (QUERI) have funded a number of projects, including Enhancing Quality Utilization in Psychosis (EQUIP).3,4 The EQUIP project is implementing and evaluating a collaborative care model designed to improve the quality of care for schizophrenia. Collaborative care models reorganize practice and typically involve changing the division of labor and responsibility, adopting new care protocols, and becoming more responsive to patients' needs.5 In a number of chronic medical illnesses and depression, researchers have demonstrated that collaborative care improves health care processes and patient outcomes by keeping ill patients in care and ensuring the provision of appropriate medication and psychosocial services.6,7 In EQUIP, established collaborative care principles have been applied to the treatment of schizophrenia and are being evaluated in a randomized, controlled trial.
A central component of EQUIP is the Medical Informatics Network Tool (MINT), a software system that was developed to support both the EQUIP care model and research evaluation. MINT supports care model implementation by helping clinicians collect, manage, and utilize patient-specific and scientific information in real time. It facilitates communication among members of the clinical team and provides reports that are used to manage care. MINT supports the research evaluation by maintaining data on all enrolled patients, their contact information, and dates for follow-up interviews. The EQUIP project, supported by MINT, is ongoing at the mental health clinics of two large VA medical centers in Southern California: the Long Beach Healthcare System and the Greater Los Angeles Healthcare System at Sepulveda. This paper describes the objectives, architecture, and functions of MINT and the utilization and performance of the system. Future applications are discussed.
Background
Key Problems with Care for Schizophrenia
Appropriate treatment for schizophrenia has been defined in a number of national treatment guidelines.8,9,10 Researchers have compared usual treatment at public clinics with appropriate care and found large differences.2 Severely ill patients drop out of treatment at a high rate, often unnoticed by busy clinicians.11 Symptoms, side effects, and other problems are often not accurately assessed and medications not appropriately changed.12 Family members and other caregivers are usually not in contact with clinicians or not provided support or education. Although optimal treatment is team based, clinicians at typical clinics are often very busy and have difficulty coordinating care. Overall, there is a pressing need to improve information about the patient and to use it to focus care.
At mental health clinics, the clinical information that is typically available has been of limited use in improving care. Most clinics do not have patient registries that include clinical information. Handwritten medical records can be illegible, incomplete, difficult to access from more than one site, and poorly organized. This makes it difficult for clinicians and managers to assess and ensure the quality of care.13 Most clinicians lack training in structured assessment tools, and accurate clinical assessment is often not a routine part of care.14 Centralized clinic databases typically contain only basic patient data from infrequent assessments.
Although care management strategies can improve patient outcomes, they are not being widely used in mental health. Researchers have found that physician feedback, disease registries, clinical guidelines, and patient and caregiver education can improve care and outcomes in a number of chronic diseases.15 The treatment of schizophrenia, like other chronic diseases, requires the accurate collection and use of both patient-specific and scientific information. This integration is particularly important given the complexity of the treatment regimens for schizophrenia and the seriousness of the risks faced by this population, such as victimization, substance abuse, and untreated medical disorders.
Using Clinical Information to Improve Care
Wagner and colleagues16 emphasize the importance of providing greater access to clinical information for all members of the health care team when managing chronic conditions. There must be ongoing clinical assessment combined with access to needed treatments. In schizophrenia, accurate assessment of the severity of symptoms (e.g., hallucinations) and medication side effects, e.g., akathisia (motor restlessness), requires specific training. Although psychiatrists may lack the time and incentive to conduct ongoing assessments, master's degree–level clinicians can accurately assess symptoms and side effects using structured instruments.17 Ensuring access to needed treatments requires both that the treatments be available and that clinicians make use of them. The availability of treatments can be improved by providing policy makers and managers with information regarding unmet patient needs. Clinicians can be encouraged to make use of available treatments by providing them with real-time data regarding patients' unmet treatment needs and by providing feedback when care is not appropriate.
The use of informatics systems to carry out these functions has been shown to improve care and reduce errors in a number of chronic medical disorders.18,19,20,21 There are several types of effective informatics systems.22 Computer-based clinical decision support systems (CDSS) match individual patient information to a knowledge base for the purposes of assessment and making recommendations for clinical decision making. A review of research on CDSS found that two-thirds of studies reported benefits in physician performance and six of 14 studies reported improvements in patient outcomes.19 These studies involved a wide variety of targets (medication dosing, diagnosis, preventive care), diseases (asthma, hypertension, cancer, diabetes, AIDS), and medical services (mammograms, nursing care, vaccinations). Electronic medical records (EMRs) are electronic stores of notes, laboratory test results, patient problems, medications, and demographic data. They have been shown to improve preventive care and adherence to clinical guidelines and to reduce errors in ordering medications and tests in primary and specialty care.23,24,25,26,27 Clinical reminders have been found to increase adherence to clinical guidelines, especially in preventive care.19,20,28 Disease registries gather, organize, and provide access to condition-specific information for a panel of patients. Registries manage only selected information in a structured format, which differentiates them from more comprehensive systems such as EMRs. Disease registries are increasingly used for medical disorders such as diabetes, asthma, congestive heart failure, and depression.15 They are believed to be a critical component of interventions that improve care and patient outcomes in chronic illness.29 For example, a disease registry for diabetes could include laboratory test results on glucose (HgbA1c) and lipid levels, blood pressure measurements, and dates of recent eye examinations. Care for a population of patients can then be improved by identifying and contacting patients who are doing poorly or who have not received necessary services. Also, services can be reorganized when pervasive clinical problems are identified.
Since the late 1990s, the VA has had a fully electronic medical record called the Computerized Patient Record System (CPRS) and has had success using reminder systems in some chronic diseases.30 In primary care clinics, VA researchers have experimented with decision support software for hypertension31 and depression (Edmund Chaney, personal communication). However, in mental health specialty care, there has been less progress. It has become apparent that current medical records do not contain reliable information on critical clinical domains such as psychotic symptoms, medication side effects, and functioning.14 In the VA, there has been routine collection of data in just two domains: (1) tardive dyskinesia, a side effect of antipsychotic medication, and (2) global assessment of functioning (GAF), a measure that attempts to simultaneously rate interpersonal, vocational, and symptomatic functioning. The usefulness of these data has been limited since tardive dyskinesia rarely occurs with current medications and the GAF is only reliable when administered by highly trained staff.32 As a result, quality assessment has usually been based only on utilization data, such as medication dose, that are indirectly related to patient outcomes.33 Indeed, the Mental Health QUERI has come to the conclusion that the major barrier to integrating research findings into practice is a lack of routine outcome data to inform quality measurement.34
Design Objectives
MINT was developed to support both implementation of collaborative care and the research study of this implementation. Design objectives for support of collaborative care included facilitating entry of key clinical data elements and access to this information by the treatment team in real time. Clinical information was to be provided to psychiatrists during their visit with the patient, since this is when it has maximum effect. Psychiatrists were to have one-click access to targeted treatment guidelines and an interface to efficiently communicate with other members of the treatment team. They were to receive feedback regarding the extent to which they are compliant with treatment guidelines, in comparison with other psychiatrists at the clinic. Clinicians were to monitor patients' appointments and identify patients with inadequate follow-up. Finally, project staff required information regarding the frequency of patient assessments and the extent to which clinicians use the feedback information. All data had to be kept secure from unauthorized access, and the system was required to meet stringent VA information security requirements.
Design objectives for MINT support of the research evaluation included management of patient and clinician enrollment and contact information, follow-up contacts, and research assessments. EQUIP includes an independent research team that performs quantitative and qualitative assessments on an ongoing basis throughout the project. All patients undergo a structured interview by research staff at baseline and at approximately 6 and 15 months. Given the large number of patients and clinicians enrolled at multiple sites, an efficient information management interface was desired. It was also desirable to integrate the research data with care management information regarding patients, so data would not have to be entered multiple times. However, research staff had to be kept blind regarding whether particular patients and psychiatrists were in the intervention group to avoid biasing the assessments.
System Description
MINT consists of two major components: (1) a secure server accessible via the Internet using a standard Web browser interface, and (2) compiled applications running on personal computers (PCs) that interact with the clinician and the VA EMR. The server is on the Intranet inside the VA firewall, and access is restricted to authorized users. Data are maintained in a password-protected relational database. Web pages are programmed in hypertext and Active Server Page software and provide for user, clinician, and patient enrollment; entry and editing of data; report generation; secure messaging among the team; and editing of guidelines. Each user is assigned an access level (read-only, clinician, research team, quality manager, local administrator, or system administrator) that determines the functions that they can use. Compiled Visual Basic applications run on the clinicians' PCs. A pop-up application runs in the background and is the primary point of clinician access to MINT. An enroller application is used by project staff to enroll new clinicians and patients into the project's database. Both the pop-up and enroller communicate with the project server using Windows Socket protocols. MINT is compatible with Windows NT®, 2000, and XP and uses the high-speed local area networks of the VA.
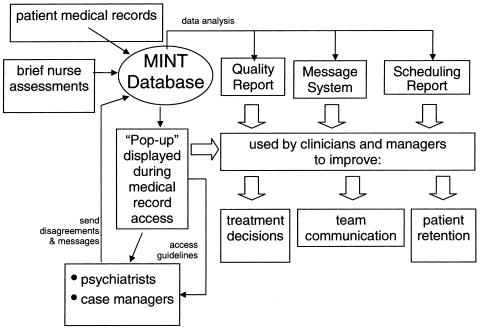
▶ shows a schematic diagram of the overall system architecture and data flows. Data enter the MINT database from brief assessments of patients, from patients' medical records, and from project staff. MINT analyzes the data, displays them using the pop-up, creates a variety of reports for Web viewing or printing, and runs a secure messaging system. Clinicians can use the pop-up to access treatment guidelines, send and receive messages, and disagree with brief assessments.
Figure 1.
Schematic diagram of MINT functions.
User Services
Patient and Clinician Enrollment
All psychiatrists at the Sepulveda and Long Beach mental health clinics were recruited for EQUIP. All enrolled, except one, for a total of 48 psychiatrists. Patients were eligible for the study if they had a visit during a six-month period before study initiation, a second visit during the first six months of the study, and a diagnosis of schizophrenia or schizoaffective disorder. Across both clinics, 292 patients are currently enrolled. Half the psychiatrists at each site were randomized, along with their patients, to the collaborative care model. The rest remained with care as usual.
MINT is active only for patients and clinicians who are enrolled in EQUIP. This is accomplished starting with an enroller application that records the unique personal identification numbers (PINs) that the EMR (CPRS) uses to identify patients and clinicians. After each clinician gives informed consent to enroll in the study, a project staff member runs the enroller application on a PC. The clinician logs into the CPRS, causing the CPRS application to generate window messages that include his or her PIN. This PIN is read by the enroller, and his or her name and PIN are entered into the MINT database. To enroll a patient, a project staff member runs the enroller application, opens the CPRS, and chooses the medical record for that patient. When this happens, CPRS messages a unique patient PIN. The enroller checks that the patient is not already in the database; confirms the patient's identity with the user; and enters the patient's name, social security number, date of birth, height, and PIN into the MINT database. Within the MINT database, each clinician and patient is assigned to collaborative care or care as usual.
Entry of Brief Assessments
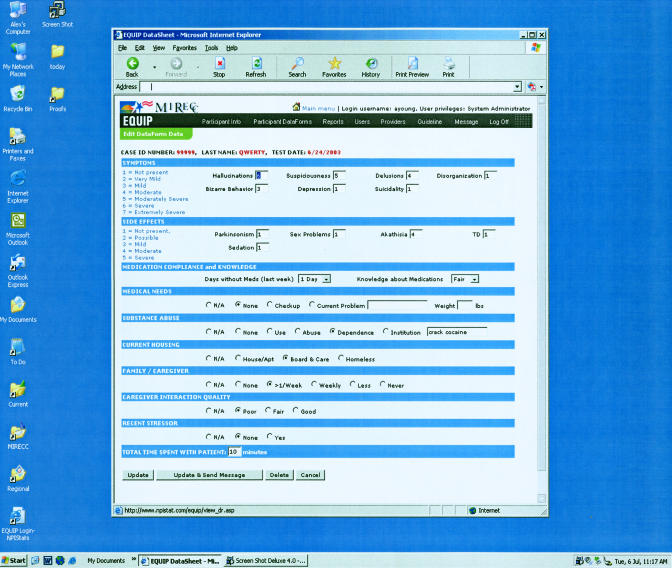
The Institute of Medicine35 has asserted that “patient-specific clinical information” is critical to improving care. To collect this information, MINT houses a brief assessment module that is administered by a trained clinician (typically a nurse) before each psychiatrist visit. These “psychiatric vital signs” assess the following domains using established clinical scales: (1) patients' symptoms, including hallucinations, suspiciousness, delusions, disorganization, bizarre behavior, depression, and suicidality, as measured by the Brief Psychiatric Rating Scale36; (2) medication side effects, including akathisia,37 tardive dyskinesia,38 parkinsonism,39 sedation, sexual dysfunction, and weight gain; (3) medication compliance, measured as the number of days of compliance during the past week; (4) medical problems, including chronic conditions and body mass index (BMI) as a measure of overweight40; (5) substance abuse based on the Clinician Rating Scale41; (6) housing status; (7) family/caregiver contact frequency and problems; and (9) the presence of recent stressors. The assessment of these items averages about 10 minutes and is usually conducted when the patient is waiting to meet with his or her clinician. When patients are severely ill or miss appointments, telephone assessments are performed. Assessment data are directly entered into a page on the MINT Web site (▶). When desirable, staff use a secure wireless interface to access the Web site from a notebook computer.
Figure 2.
Web site page for entering a brief assessment.
Feedback to Psychiatrists
It has been suggested that providing patient-level clinical information to health care professionals can aid in the identification of previously unknown health problems, improve chronic disease management, and enhance communication between patients and clinicians.42 Although the evidence that clinician feedback improves the care process and outcomes is mixed for a variety of diseases, the evidence for mental health information is stronger.43 Studies that have not shown an effect on care have concluded that clinical information needs to be provided in the context of a comprehensive disease management program.43,44
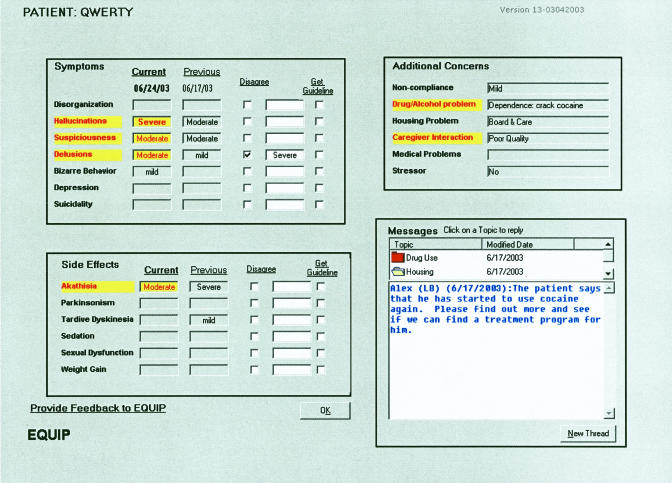
MINT provides clinical data to psychiatrists during the clinical encounter, the time that it is most likely to be used. When an enrolled psychiatrist accesses an enrolled patient's CPRS record, the pop-up application detects that both PINs are in the MINT database. If the patient is assigned to collaborative care, a window is then displayed in front of the CPRS chart. The pop-up window contains the ratings from the current and previous brief assessments (▶). Severe problems are highlighted using a warning color. Clinicians can disagree with an item's rating by checking a box and entering their assessment. There is a “guideline” box next to each symptom and side effect item. When checked, a brief guideline synopsis is displayed with links to Web sites that contain the full version of guidelines. When the clinician is done reviewing the pop-up, he or she clicks “OK” to return to the patient's CPRS chart. The pop-up can be redisplayed at any time during the encounter.
Figure 3.
Pop-up screen seen by psychiatrists.
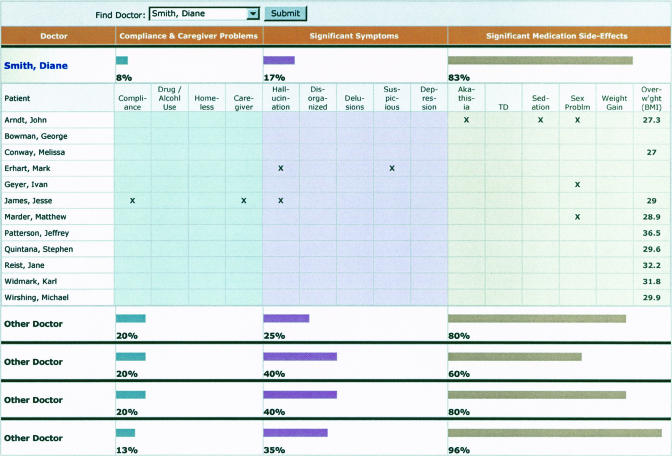
In addition to providing information via the pop-up window, MINT uses its Web site to generate reports about the quality of care for specific patients. Psychiatrists log into the Web system, and view an “action item report” that lists active clinical problems for all their enrolled patients (▶). Problems are presented in three domains: (1) treatment compliance and related issues, (2) symptoms, and (3) medication side effects. When a patient has a severe problem, it is indicated with an X. Psychiatrists do not see patient-level data for other psychiatrists' practices. However, they do see summary statistics for their caseload and for the caseloads of other psychiatrists at their clinic. These consist of numerical and graphic representations of the proportion of a psychiatrist's patients that have a problem in each domain. Psychiatrists can use this feedback to compare their performance with that of other psychiatrists.
Figure 4.
Web site report on problems with the quality of patient care.
Messaging Among the Clinical Team
Effective care for chronic disease, and especially schizophrenia, often requires a team of clinicians with differing skills.45 An important characteristic of successful team care is strong communication among team members.46 MINT supports this communication. After entering the brief assessment data, the nurse can enter a text message. This message appears in the pop-up when the psychiatrist next sees that patient. The psychiatrist can respond to the message or start a new message topic. Messages have proven to be especially useful when there is a chronic medical issue, significant stressor, distress with family or caregivers, or a topic requiring further elaboration or a response from the psychiatrist. In addition to viewing messages in the pop-up, any enrolled team member can log into the MINT Web site and view a message report that lists all new messages that have not yet been read. There is also the option to respond to any message.
Management of Quality
Quality oversight is facilitated by using a patient registry, by brief assessment data, and by identifying patients who are not receiving needed services. A registry of patients and clinicians is maintained using the Web interface. This registry maintains patient contact information, whether consent has been obtained for caregiver contact, any caregiver contact information, the patient's primary psychiatrist, and the date of the last contact with the patient. For each patient in the registry, brief assessment data are available. These data focus on key clinical problems for which there are evidence-based treatments that substantially improve outcomes. Guidelines, including the Schizophrenia PORT, were used to determine which clinical problems to include. For example, psychotic symptoms and medication side effects are major targets of evidence-based care. Similarly, items assess family interaction and discord so that additional family education and support can be provided when necessary.
Brief assessment data are displayed by the pop-up. They are also used to generate reports for clinical managers regarding care quality. These reports are identical to the action item report provided to individual psychiatrists, except that they contain patient-level information for all the psychiatrists at the clinic. The reports can be used to identify psychiatrists who could benefit from extra support or resources to manage particular clinical problems. It also identifies pervasive patient problems at the clinic.
MINT is also used to identify patients who are using too few or no necessary services. For example, the MINT Web site produces an “appointment report” that lists scheduled appointments for all patients. This is used to monitor receipt of services, identify when necessary follow-up has not been arranged, and identify opportunities to locate difficult-to-find patients. Data for this appointment report are automatically drawn on a nightly basis from VA medical record databases.
Project Management
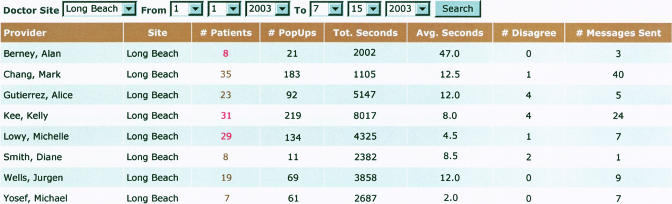
The MINT Web site is used to manage information security, treatment guidelines, and implementation of the EQUIP care model. Project administrators use the Web site to manage access privileges for individual users and to modify and update the treatment guidelines that are retrieved from the pop-up. Management staff use the site to monitor progress with care model implementation. A “brief assessment report” lists the number of assessments that have been entered by each clinician during a given date range. In addition, a “clinician feedback report” lists for each psychiatrist information on his or her pop-up viewing during a given date range (▶). Data presented include the number of pop-ups that the psychiatrist viewed, the names of patients whose data were viewed, and the date of the most recent assessment for each patient. This feature allows staff to identify when psychiatrists have received patient information. The report also presents the number of seconds that the psychiatrist viewed each pop-up, the number of messages that he or she has sent, and the number of times he or she disagreed with the brief assessments. Management staff use this feature to monitor how much attention individual psychiatrists are paying to the information presented to them.
Figure 5.
Web site report regarding psychiatrists' use of the pop-up.
Status Report
MINT began operation at Long Beach in January 2003 and at Sepulveda in April 2003. At 14 months, MINT is managing data for 165 intervention patients. It is being used by two nurse quality managers who conduct brief assessments and manage the study sites. It is used by 29 psychiatrists who are receiving the EQUIP intervention. MINT is also managing research enrollment for an additional comparison group of 19 psychiatrists and 127 patients that is continuing with usual care.
As shown in the ▶, clinicians have entered 1,223 brief assessments and 1,100 messages into the database. The pop-up has been displayed to psychiatrists 2,201 times. Psychiatrists often view the pop-up more than once while treating a patient. The window appears when they first open the medical record at the start of the visit. They sometimes choose to recall the pop-up again during the visit. If they write a patient note at a later time in the day, it will appear again. Psychiatrists have disagreed with 49 of the nurses' brief assessments and have written 78 messages back to other clinicians. The median time that psychiatrists have spent viewing each pop-up has been 7 seconds. Twenty-five percent of viewings are less than 3 seconds and 75% are less than 17 seconds. As psychiatrists have become accustomed to the interface, the median viewing duration has decreased gradually from 11 seconds during the first month to 4 seconds during month 14. The number of messages sent by psychiatrists has increased gradually over this time.
Table 1.
Use of MINT Service during Months 1 through 14 of Care Model Implementation*
| Implementation Month/Year |
Site Total |
Project Total |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Service | Site | 1/03 | 2/03 | 3/03 | 4/03 | 5/03 | 6/03 | 7/03 | 8/03 | 9/03 | 10/03 | 11/03 | 12/03 | 1/04 | 2/04 | ||
| Entry of brief assessments | LB | 56 | 42 | 47 | 48 | 41 | 58 | 41 | 39 | 44 | 47 | 35 | 45 | 44 | 45 | 632 | 1,223 |
| Sep | 28 | 53 | 67 | 54 | 53 | 59 | 64 | 48 | 58 | 51 | 56 | 591 | |||||
| Entry of messages by clinicians | LB | 45 | 32 | 38 | 25 | 34 | 35 | 41 | 42 | 54 | 52 | 18 | 33 | 34 | 39 | 522 | 1,100 |
| Sep | 26 | 52 | 63 | 53 | 53 | 67 | 72 | 42 | 44 | 49 | 57 | 578 | |||||
| Feedback to psychiatrists (pop-up) | LB | 26 | 67 | 26 | 129 | 106 | 74 | 92 | 64 | 47 | 92 | 73 | 158 | 70 | 42 | 1,066 | 2,201 |
| Sep | 15 | 73 | 134 | 105 | 143 | 130 | 147 | 61 | 62 | 105 | 160 | 1,135 | |||||
| Disagreement by psychiatrists | LB | 0 | 6 | 0 | 0 | 1 | 2 | 0 | 6 | 5 | 4 | 6 | 3 | 4 | 3 | 40 | 49 |
| Sep | 0 | 3 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 9 | |||||
| Entry of messages by psychiatrists | LB | 1 | 2 | 1 | 9 | 2 | 13 | 12 | 4 | 4 | 6 | 6 | 2 | 6 | 2 | 70 | 78 |
| Sep | 0 | 0 | 1 | 2 | 0 | 2 | 3 | 0 | 0 | 0 | 0 | 8 | |||||
LB = the Long Beach Healthcare System; Sep = the Greater Los Angeles Healthcare System at Sepulveda.
MINT was used with 11 psychiatrists and 84 patients at Long Beach and 18 psychiatrists and 81 patients at Sepulveda.
Clinician and psychiatrist use of the pop-up, messaging system, and reports has remained steady throughout implementation. During implementation, users have made numerous suggestions regarding improving the interfaces. Feedback has ranged from adjustments in visual aspects of the pop-up (e.g., increase font sizes) to addition of new features (e.g., add a “to do list” of urgent problems to be addressed). Changes have been made based on user feedback. An iterative process of quality enhancement appears to have promoted active participation and motivation of those using the system.
Nine months after implementation of MINT, a sample (53%) of intervention clinicians were interviewed by an independent researcher regarding human factors characteristics, use, usability, and usefulness of the informatics system. The interview included established informatics questionnaires47 plus qualitative items regarding MINT components and the impact of MINT on treatment.
With regard to the collaborative care model, the majority of psychiatrists found the informatics system intuitive and easy to use and believed that it provided relevant clinical information in a visually appealing format. Although some psychiatrists viewed the pop-up only quickly due to time constraints, virtually all stated that they learned important new information about their patients, especially related to the patients' social circumstances. Most stated that the assessment data reminded them to discuss side effects and medical problems with their patients. Some psychiatrists specifically stated that there was a better level of patient care due to the additional information. One psychiatrist pointed out that the assessments were especially helpful with patients whose clinical stability varies. Psychiatrists acknowledged that they rarely accessed the treatment guidelines, and a few stated that they should use the guidelines more. The messaging system was used mostly by nurse quality managers to communicate information to psychiatrists. Overall, psychiatrists stated that MINT provided them with specific information that they used to improve their treatment decision making.
Nurse quality managers report that MINT has made it possible to proactively monitor the care of a population of chronically ill patients. Assertive outreach has been made to patients who have missed appointments or who have had inadequate follow-up given the severity of their illness. There have been anecdotal reports from clinicians and nurses that communication has been enhanced among the clinicians regarding the care of individual patients, facilitating teamwork and provision of appropriate services.
MINT has also been very helpful to staff who manage the clinical and research components of the EQUIP project. With several clinicians and hundreds of patients enrolled in the project, staff have reported that MINT has been invaluable in ensuring that participants have research follow-up interviews on time and that problems with implementation of the intervention can be quickly identified and resolved.
With regard to improving care, MINT Web site reports indicated that there was a severe, pervasive problem with overweight at both clinics. At the Sepulveda and Long Beach clinics, 74% of people with schizophrenia were overweight (BMI >25) and 40% were obese (BMI >30). This is even worse than the general U.S. adult population, in which about 65% of people are overweight and 31% are obese.48 Acting on these MINT data, clinic managers identified resources for counseling regarding nutrition and exercise. Since this time, 73% of the patients who are overweight have received individual and/or group wellness counseling, often under a standardized protocol. Additionally, psychiatrists have been alerted to address weight problems in their medication treatment. Guideline-concordant approaches to this include changing to a medication with less weight gain liability, or adding medications that can reduce weight gain.
MINT Web site reports have also indicated that many patients have severe, persistent psychotic symptoms, despite trials of numerous medications. Clozapine is a medication that is substantially more effective for these patients, but its use requires regular blood monitoring. Specific organizational structures need to be in place to check these blood tests and dispense medication refills, yet these are lacking at many clinics. The implementation of MINT raised awareness of these barriers. A centralized clozapine clinic was created at Sepulveda and referral procedures for clozapine at Long Beach were improved. In total, 43 patients have been referred for clozapine and two have been switched to this medication.
Additionally, MINT Web site reports identified that many patients with ongoing clinical problems (severe psychotic symptoms, noncompliance, or family stress) have family contact at least once per week. The majority of these patients consented to the clinical team contacting their family. All patients who gave consent were offered a family intervention, resulting in 67 referrals. Twelve have received family or caregiver counseling, three families refused any intervention once contacted, and two families were provided with education and information regarding community resources.
Discussion
MINT is designed to improve the quality of care at the patient, clinician, and practice levels. At the patient level, MINT identifies specific problems that need to be addressed, such as psychosis or homelessness. At the clinician level, MINT identifies when psychiatrists should consider new strategies for dealing with problems in their panel of patients. At the practice level, MINT identifies pervasive problems that require changes in the organization of care.
Data from the research evaluation indicate that the MINT informatics system is well received and provides clinical information that has been used to improve treatment decisions. Results indicate that the information provided in the pop-up prompts clinicians to assess side effects and physical problems and not just symptoms. Although psychiatrists were still spending the same amount of time with patients (20-minute sessions), it is possible that this time was used more effectively given the additional clinical information provided by MINT. Referrals for weight management, clozapine use, and family services have increased substantially and may lead to improved patient outcomes. Organizational changes have occurred that have improved access to care.
MINT has a variety of potential uses in psychiatric disorders and other chronic medical illnesses. It should be useful in large, multisite efforts to improve the quality of care. Potential applications also include situations in which feedback to clinicians is desired during the treatment visit or key clinical data need to be managed over time. MINT is easy to incorporate into usual practice at busy clinics and is readily adaptable to local needs. The user interface is intuitive and easy to use. In EQUIP, very brief training was sufficient for almost all users. Dissemination should be affordable, particularly within the VA given that it has a standardized national EMR. Further modifications will be required for clinics working with paper charts. Whatever the local medical record situation, the vast majority of our health care organizations share a pressing need for improved clinical information. This is especially true in mental health, where substantial progress in improving care will require that improved information systems are integrated into day-to-day clinical operations.
Supported by the Department of Veterans Affairs through the Health Services Research & Development Service (RCD 00-033 and CPI 99-383) and the Desert Pacific Mental Illness Research, Education and Clinical Center (MIRECC) and by the NIMH UCLA-RAND Center for Research on Quality in Managed Care (MH 068639).
The authors thank Sun Hwang, Qing Chen, Kuo-Chung Shih, Daniel Mezzacapo, Michelle Briggs, Donna Bean, Christopher Reist, Kirk McNagny, Christopher Kessler, EQUIP clinicians, and the Long Beach and Greater Los Angeles VA Information Resource Management Services for their contributions to the project.
Any opinions expressed are only those of the authors and do not necessarily represent the views of any affiliated institutions.
References
- 1.Young AS, Magnabosco JL. Services for adults with mental illness. In: Levin BL, Petrila J, Hennessy KD, (eds). Mental Health Services: A Public Health Perspective. 2nd ed. New York, NY: Oxford University Press; 2004, pp 177–208.
- 2.Lehman AF. Quality of care in mental health: the case of schizophrenia. Health Aff (Millwood). 1999;18(5):52–65. [DOI] [PubMed] [Google Scholar]
- 3.McQueen L, Mittman BS, Demakis JG. Overview of the Veterans Health Administration (VHA) Quality Enhancement Research Initiative (QUERI). J Am Med Inform Assoc. 2004;11:339–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young AS, Mintz J, Cohen AN. Clinical computing: using information systems to improve care for persons with schizophrenia. Psychiatr Serv. 2004;55:253–5. [DOI] [PubMed] [Google Scholar]
- 5.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102. [DOI] [PubMed] [Google Scholar]
- 6.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–20. [DOI] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288:1909–14. [DOI] [PubMed] [Google Scholar]
- 8.Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull. 2004 (in press). [DOI] [PubMed]
- 9.Veterans Health Administration. Clinical Guideline for Management of Persons with Psychoses, Version 1.0. Washington, DC: Department of Veterans Affairs; 1997.
- 10.American Psychiatric Association. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 suppl):1–56. [PubMed] [Google Scholar]
- 11.Young AS, Grusky O, Jordan D, Belin TR. Routine outcome monitoring in a public mental health system: the impact of patients who leave care. Psychiatr Serv. 2000;51:85–91. [DOI] [PubMed] [Google Scholar]
- 12.Young AS, Sullivan G, Burnam MA, Brook RH. Measuring the quality of outpatient treatment for schizophrenia. Arch Gen Psychiatry. 1998;55:611–7. [DOI] [PubMed] [Google Scholar]
- 13.Dick RS, Steen EB, Detmer DE, (eds). The Computer-Based Patient Record: An Essential Technology for Health Care, Revised Edition. Washington, DC: National Academies Press, 1997. [PubMed]
- 14.Cradock J, Young AS, Sullivan G. The accuracy of medical record documentation in schizophrenia. J Behav Health Serv Res. 2001;28:456–65. [DOI] [PubMed] [Google Scholar]
- 15.Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289:434–41. [DOI] [PubMed] [Google Scholar]
- 16.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 17.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “the drift busters”. Int J Methods Psychiatr Res. 1993;3:221–44. [Google Scholar]
- 18.Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. The clinical value of computerized information services. A review of 98 randomized clinical trials. Arch Fam Med. 1996;5:271–8. [DOI] [PubMed] [Google Scholar]
- 19.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998;280:1339–46. [DOI] [PubMed] [Google Scholar]
- 20.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3:399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lobach DF, Hammond WE. Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am J Med. 1997;102:89–98. [DOI] [PubMed] [Google Scholar]
- 22.Hersh WR. Medical informatics: improving health care through information. JAMA. 2002;288:1955–8. [DOI] [PubMed] [Google Scholar]
- 23.Rollman BL, Hanusa BH, Gilbert T, Lowe HJ, Kapoor WN, Schulberg HC. The electronic medical record. A randomized trial of its impact on primary care physicians' initial management of major depression. Arch Intern Med. 2001;161:189–97. [DOI] [PubMed] [Google Scholar]
- 24.Garrett LE Jr, Hammond WE, Stead WW. The effects of computerized medical records on provider efficiency and quality of care. Methods Inf Med. 1986;25:151–7. [PubMed] [Google Scholar]
- 25.Rissover J. Six electronic medical record systems. Med Software Rev. 1997:1–8.
- 26.Safran C, Rind DM, Davis RB, et al. Guidelines for management of HIV infection with computer-based patient's record. Lancet. 1995;346(8971):341–6. [DOI] [PubMed] [Google Scholar]
- 27.Young DW. Improving the consistency with which investigations are requested. Med Inform (Lond). 1981;6:13–7. [DOI] [PubMed] [Google Scholar]
- 28.Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. The clinical value of computerized information services: A review of 98 randomized clinical trials. Arch Fam Med. 1996;5:271–8. [DOI] [PubMed] [Google Scholar]
- 29.Metzger J. Using Computerized Disease Registries in Chronic Disease Care. Oakland, CA: California Healthcare Foundation,, 2004.
- 30.Cannon DS, Allen SN. A comparison of the effects of computer and manual reminders on compliance with a mental health clinical practice guideline. J Am Med Inform Assoc. 2000;7:196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goldstein MK, Hoffman BB, Coleman RW, et al. Patient safety in guideline-based decision support for hypertension management: ATHENA DSS. J Am Med Inform Assoc. 2002;9(6 suppl):S11–6. [PMC free article] [PubMed] [Google Scholar]
- 32.Roy-Byrne P, Dagadakis C, Unutzer J, Ries R. Evidence for limited validity of the revised global assessment of functioning scale. Psychiatr Serv. 1996;47:864–6. [DOI] [PubMed] [Google Scholar]
- 33.Young AS. Dosages and outcomes. Psychiatr Serv. 2003;54:1547. [DOI] [PubMed] [Google Scholar]
- 34.Veterans Health Administration. Quality Enhancement Research Initiative: Mental Health QUERI Strategic Plan. Available at: http://www.mentalhealth.med.va.gov/mhg/exec-summary.shtml. Accessed July 6, 2004.
- 35.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2001. [PubMed]
- 36.Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green MF, Shaner A. Brief Psychiatric Rating Scale (BPRS) expanded version (4.0): scales, anchor points and administration manual. Int J Methods Psychiatr Res. 1993;3:227–43. [Google Scholar]
- 37.Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–6. [DOI] [PubMed] [Google Scholar]
- 38.Marsden CD, Schachter M. Assessment of extrapyramidal disorders. Br J Clin Pharmacol. 1981;11:129–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–9. [DOI] [PubMed] [Google Scholar]
- 40.National Institues of Health (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. From National Institutes of Health (US). Available at: http://www.nhlbi.nih.gov/guidelines/obesity/ob_home.htm. Accessed Mar 30, 2004.
- 41.Mueser KT, Drake RE, Clark RE, McHugo GJ, Mercer-McFadden C, Ackerson TH. Toolkit: evaluating substance abuse in persons with severe mental illness. From The Human Services Research Institute. Available at: http://www.mentalhealth.org/cmhs/CommunitySupport/research/toolkits/pn6ch2.asp. Accessed Mar 30, 2004.
- 42.Deyo RA, Carter WB. Strategies for improving and expanding the application of health status measures in clinical settings. A researcher-developer viewpoint. Med Care. 1992;30:MS176–86, discussion, MS196–209. [DOI] [PubMed] [Google Scholar]
- 43.Espallargues M, Valderas JM, Alonso J. Provision of feedback on perceived health status to health care professionals: a systematic review of its impact. Med Care. 2000;38:175. [DOI] [PubMed] [Google Scholar]
- 44.Fihn SD, McDonell MB, Diehr P, et al. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004; 116(4):241–8. [DOI] [PubMed] [Google Scholar]
- 45.Young AS, Forquer SL, Tran A, Starzynski M, Shatkin J. Identifying clinical competencies that support rehabilitation and empowerment in individuals with severe mental illness. J Behav Health Serv Res. 2000;27(3):321–33. [DOI] [PubMed] [Google Scholar]
- 46.Liberman RP, Hilty DM, Drake RE, Tsang HW. Requirements for multidisciplinary teamwork in psychiatric rehabilitation. Psychiatr Serv. 2001;52:1331–42. [DOI] [PubMed] [Google Scholar]
- 47.Lewis JR. IBM computer usability satisfaction questionnaires: psychometric evaluation and instructions for use. Int J Hum Comput Interact. 1995;7:57–78. [Google Scholar]
- 48.National Center for Health Statistics. Health, United States, 2002. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2002.