Abstract
Introduction
Gender-related differences in type B aortic dissection (TBAD) presentation and outcomes are not well understood. The objective of this study is to assess the impact of gender on short-term outcomes in patients with TBAD.
Methods
Patients with TBAD were identified from National Inpatient Sample datasets from 2009–2012 according to previously published methods. The primary outcomes of interest were in-hospital mortality and major complications (renal, cardiac, pulmonary, paraplegia, and stroke-related) between men and women. An inverse propensity-weighted regression was used to balance comorbid and clinical presentation differences. Subgroup analyses were performed on those undergoing endovascular (TEVAR) and open repair, and for elderly patients over the age of 70.
Results
We identified 9855 patients with TBAD; females were fewer (43.6%, n=4293), and presented at a later age (69.8±15.5 vs. 62.8±15.6, p<0.001). Females had more comorbidities (median Elixhauser 4 [IQR 2–5] vs. 3 [IQR 2–5], p<0.001), and were more often managed non-operatively (87.4% vs. 81.8%, p<0.001) compared to males. For those undergoing intervention, 58% (n=903) had open repair and TEVAR rates were higher in females compared to males (45.6% vs. 40.0%, p<0.001). Unadjusted mortality rates did not differ significantly by gender (male: 11.6% vs. female: 10.7%). In an adjusted propensity-weighted regression, gender did not significantly affect in-hospital mortality or stroke rates, but females were less likely to have acute renal failure during their hospitalization and more likely to experience cardiac events when undergoing open repair. Elderly females were also less likely to experience acute renal failure but had higher odds of cardiac events regardless of intervention compared to elderly men.
Conclusions
In comparison to men, females with TBAD presented at a later age, were more likely to undergo TEVAR, sustain a perioperative cardiac event with open surgery, and less likely to experience acute renal complications overall. Elderly females were additionally more likely to sustain a cardiac event regardless of operative status. Future studies should attempt to identify anatomic and epidemiologic reasons for these differences.
1. INTRODUCTION
Aortic dissection is an uncommon, emergent condition that is often life-threatening, with thoracic aortic dissection accounting for an estimated incidence of 5–10 cases per million people per year1–3. Emergent surgical reconstruction is the treatment of choice for ascending aortic dissection (TAAD) involving the aortic root, ascending aorta, and aortic arch, but the management of type B dissection (TBAD) involving the descending thoracic aorta distal to the left subclavian artery continues to evolve. Although gender differences in presentation and risk have been demonstrated for other cardiovascular health conditions4,5, the disparities between males and females for patients presenting with TBAD have not been extensively explored6. The objective of this study is to analyze differences between male and female patients with TBAD in presentation and in-hospital outcomes using a large national database.
2. METHODS
Data was obtained from the 2009–2012 National Inpatient Sample (NIS) datasets. The NIS is a research dataset curated and provided by the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project7. The dataset consists of a 20% sample of discharge-level inpatient admissions nationally; from 2009–2011 consisting of all discharges from a 20% sample of hospitals collected nationally, then in 2012 changing to a 20% sample of all nationwide discharges. The NIS provides sampling weights that can be used to reconstruct national population estimates for trend analysis in addition to analysis as a stand-alone cohort. Coding of diagnoses and procedures uses the International Classification of Diseases, Ninth Revision, Clinical Modification system (ICD-9-CM). This retrospective study of national, de-identified administrative data was approved by the university institutional review board prior to data collection and analysis.
Patients carrying a diagnosis of TBAD were identified using ICD-9-CM coding according to published methods for NIS data as initially described by Sachs and colleagues and utilized in several subsequent studies8–10. Comorbid conditions were identified using the Elixhauser comorbidity index11. Those undergoing treatment with endovascular repair or open repair were also identified according to the same methods; patients not receiving either were classified as non-operative.
The primary comparison groups were separated by gender. The primary outcome was in-hospital mortality. Secondary outcomes included acute renal failure, acute cardiac event, acute respiratory failure, acute stroke, and acute paraplegia experienced during the hospitalization identified according to previously published methods8. In order to account for any differences between the male and female cohorts, propensity methods were used to balance comorbid and procedural characteristics. A logistic model was fit on gender to derive a propensity score over a range of clinically important factors, and was then applied as an inverse probability of treatment weight in order to compare the male and female cohorts. Primary and secondary adjusted analyses were performed using logistic regression on the weighted cohorts with a robust variance estimator.
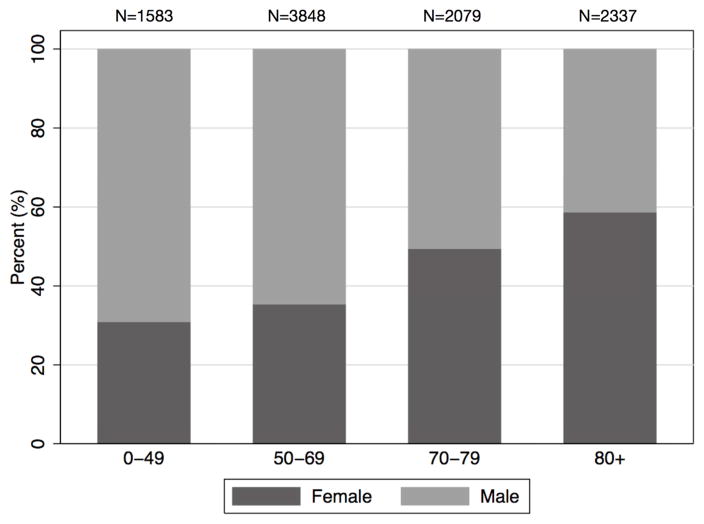
Three subgroup analyses comparing outcomes between men and women were performed: one for those undergoing TEVAR, one for those undergoing open repair, and one for elderly patients over the age of 70. This age cutoff was selected due to the marked differences in gender makeup on either side of this cut-point (Figure 1), as well as previous usage in several abdominal aortic aneurysm studies12. Subgroup analyses were performed in an analogous fashion to the primary outcome analysis, comparing male to female gender using inverse propensity weighting.
Figure 1. Gender Makeup by Decade of Age.
Percentage of gender by decade of age.
Statistical analysis was performed using Stata SE 13.1 (StataCorp, College Station, TX). Student t-, Fisher exact, chi square, Wilcoxon rank-sum, and Kruskal-Wallis tests were used where appropriate for unadjusted comparisons. Normality was assessed qualitatively for all factors. Balance between the weighted cohorts was assessed using standardized differences. Trends in repair and sex over time were estimated using sampling weights provided by Healthcare Cost and Utilization Project 7.
3. RESULTS
We identified 9855 patients over the four-year period presenting with a diagnosis of acute type B dissection. The average age was 65.9±16 years. The majority of patients received non-operative, medical management (n=8300, 84.2%); 9.2% (n=902) underwent an open repair and 6.6% (n=652) received TEVAR.
There were 5555 male (57.4%) and 4293 female patients (43.6%) in the unadjusted sex-stratified cohorts. Females tended to be older and had higher rates of congestive heart failure, chronic pulmonary disease, diabetes, and other chronic comorbid conditions (Table 1). Male patients were more likely to undergo an intervention, endovascular or open surgical repair (male: 18.2%, female 12.6%; P<0.001). In both cohorts, a higher rate of patients received open repair compared to TEVAR (Table 1). When stratifying by decade of age, the percentage of females presenting with TBAD increased with each age category, with a smaller female representation in the younger age groups but with females making up a majority of patients greater than 70 years of age (Figure 1).
Table 1.
Baseline Characteristics
| Total N (%) |
Male N (%) |
Female N (%) |
P | |
|---|---|---|---|---|
| N=985 | N=555 | N=4293 | ||
| Age, mean ± SD | 65.9 ± 15.9 | 62.8 ± 15.6 | 69.8 ± 15.5 | <0.001 |
| Shock | 459 (4.7) | 274 (4.9) | 185 (4.3) | 0.2 |
| Cancer | 407 (4.1) | 231 (4.2) | 176 (4.1) | 0.9 |
| Heart Failure | 1869 (19.0) | 993 (17.9) | 875 (20.4) | 0.002 |
| Peripheral Vascular Disease | 5602 (56.8) | 3125 (56.3) | 2476 (57.7) | 0.2 |
| Hypertension | 7792 (79.1) | 4385 (78.9) | 3401 (79.2) | 0.7 |
| Chronic Pulmonary Disease | 2314 (23.5) | 1189 (21.4) | 1125 (26.2) | <0.001 |
| Diabetes | 1593 (16.2) | 821 (14.8) | 772 (18.0) | <0.001 |
| Renal Insufficiency | 2164 (22.0) | 1311 (23.6) | 853 (19.9) | <0.001 |
| Rheumatologic Disorder | 328 (3.3) | 82 (1.5) | 246 (5.7) | <0.001 |
| Coagulopathy | 839 (8.5) | 542 (9.8) | 297 (6.9) | <0.001 |
| Intervention | ||||
| Nonoperative Management | 8300 (84.2) | 4542 (81.8) | 3751 (87.4) | <0.001 |
| TEVAR | 652 (6.6) | 405 (7.3) | 247 (5.8) | |
| Open Repair | 903 (9.2) | 608 (10.9) | 295 (6.9) |
All values mean ± SD or N (%)
In the unadjusted analysis, 11.1% (n=1092) of patients died while in-hospital. Females had a significantly higher rate of cardiac events, but lower rates of acute renal failure, paraplegia, and stroke (Table 2). In the TEVAR subgroup, females were less likely to have acute renal failure (Female: 14.6%, n=36; Male: 30.6%, n=124; P<0.001) and trended toward lower rates of acute pulmonary complications (Female: 21.9%, n=54; Male: 27.9%, n=113; P=0.09) and lower mortality (Female: 7.3%, n=18; Male: 11.4%, n=46; P=0.09). In the open repair subgroup, females were also less likely to have acute renal complications (Female: 28.8%, n=85; Male: 38.0%, n=231; P=0.01) but had higher rates of cardiac events (Female: 23.1%, n=68; Male: 16.4%, n=100; P=0.02) without any difference for in-hospital mortality.
Table 2.
Unadjusted Outcomes
| Total | Male | Female | P | |
|---|---|---|---|---|
| N=9855 | N=5555 | N=4293 | ||
| In-Hospital Mortality | 1092 (11.1) | 594 (10.7) | 498 (11.6) | 0.2 |
| Acute Renal Failure | 1996 (20.3) | 1323 (23.8) | 672 (15.7) | <0.001 |
| Cardiac Event | 1107 (11.2) | 580 (10.4) | 527 (12.3) | 0.004 |
| Paraplegia | 134 (1.4) | 96 (1.7) | 38 (0.9) | <0.001 |
| Acute Respiratory Failure | 1865 (18.9) | 1049 (18.9) | 816 (19.0) | 0.9 |
| Acute Stroke | 75 (0.8) | 53 (1.0) | 22 (0.5) | 0.01 |
| Length of Stay (d) | 5 (2,9) | 5 (2, 9) | 5 (2, 8) | <0.001 |
| Disposition | ||||
| Mortality | 1092 (11.1) | 594 (10.7) | 498 (11.6) | |
| Discharged Home | 6107 (62.0) | 3538 (63.7) | 2563 (59.7) | |
| Transfer to Acute Care | 839 (8.5) | 523 (9.4) | 316 (7.4) | <0.001 |
| Transfer to Skilled Facility | 1814 (18.4) | 898 (16.2) | 915 (21.3) |
All values are N (%) or median (IQR)
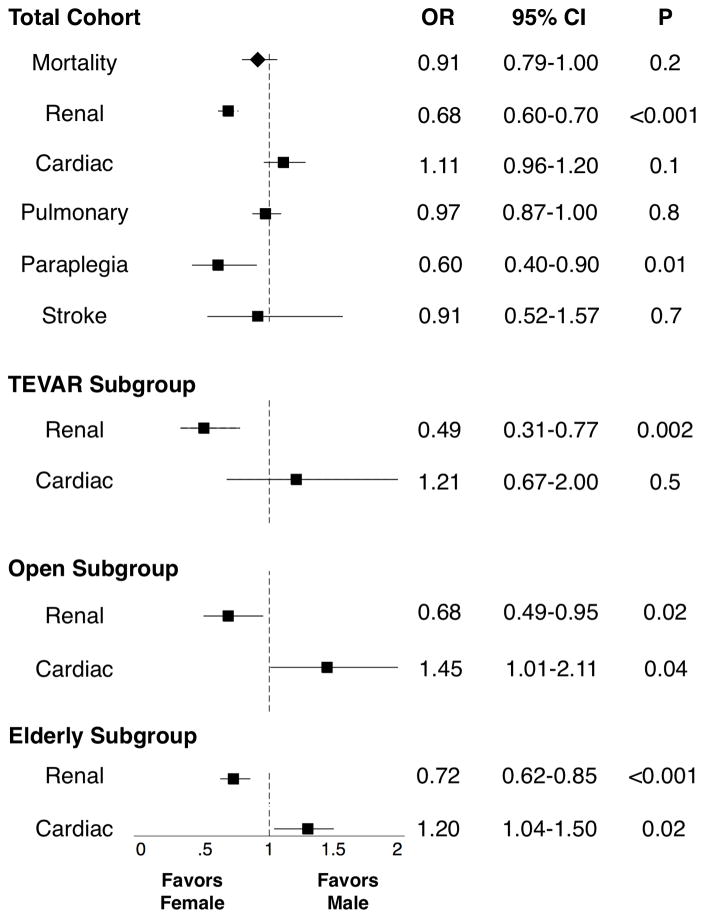
After propensity weighting, analysis of the total cohort showed that females had lower odds of renal complications and paraplegia (Figure 1), but no difference for in-hospital mortality. Females had lower odds of acute renal failure for both TEVAR and open repair, but had higher odds of cardiac events in the open surgery group. Neither intervention subgroup demonstrated any gender differences for in-hospital mortality. Females in the elderly subgroup similarly showed lower odds of acute renal failure without significantly different mortality, but with higher odds of cardiac events regardless of operative status (Figure 2).
Figure 2. Total Cohort.
Propensity-weighted outcomes of in-hospital mortality and adverse events by analysis group OR: odds ratio. CI: confidence interval
4. DISCUSSION
The management of acute type B dissection is controversial due to a lack of consensus on disease management. Progression of the disease as well as evolving treatment paradigms have seen endovascular repair replace open surgery as the preferred treatment for complicated TBAD, but treatment specifics of TEVAR and medical management, as well as long-term outcomes, remain unclear3,13–15. Although management patterns have fluctuated over the past ten years, TBAD remains a morbid condition not only in the acute phase, but also in the chronic phase due to the risk of progression to aneurysmal degeneration, rupture, and even death16,17, Differences in overall characteristics and outcomes between males and females have not been well studied in the TBAD population, in contrast to the well-documented gender differences in those with thoracic aortic aneurysm18,19.
Our study showed substantial differences in baseline characteristics between males and females presenting with acute TBAD. Overall, females made up less than half of the presenting population. In our unadjusted cohorts, females tended to be older and generally more chronically ill, with higher rates of diabetes, and chronic pulmonary, heart failure, and rheumatologic conditions compared to men. These differences have not been well studied; the only large-scale comparison of baseline characteristics between men and women was carried out by IRAD investigators in 20046. Women made up a substantially smaller cohort in their study (32.1%) and did not differ substantially from men in the type of comorbidity, although similarly to our study, females tended to present at an older age. Direct comparison of IRAD results to our data is also difficult due to the inclusion of Type A dissection patients in the IRAD cohort, making up more than half of the total cohort. Based on our results, practitioners can expect women presenting with acute type B dissection to be generally older and with more comorbidities than males.
A relatively small number of patients underwent intervention in our study cohort. Women especially were likely to receive non-operative therapy compared to men, and of those that did undergo operation, were more likely to receive TEVAR. Although it is difficult to comment on the reasoning for operative decision making in the absence of disease-specific data, the increased tendency for intervention in males compared to females is highly significant and may reflect the increased age, comorbidity of the female cohort or symptoms on presentation. This same finding was demonstrated in the IRAD cohort, with 72% of TBAD patients receiving medical management, 18% undergoing operative repair, and 10% receiving endovascular therapy. The IRAD data also showed a higher percentage of medical management in women compared to men. This was mainly driven by the higher rate of open repair in men, the generalizability of which may be limited by the subsequent meteoric rise in usage of TEVAR for TBAD9,15,20.
In the unadjusted study cohorts, females had a lower rate of acute renal failure but a higher rate of cardiac events. When divided into subgroups by intervention performed, females had higher adjusted rates of cardiac events in the open repair group but uniformly had less acute renal complications for both TEVAR and open repair. This is not reflected in the previous IRAD study, which showed no difference in in-hospital complications or mortality for females and males with TBAD; however, the IRAD female cohort did demonstrate a higher rate of imaging findings consistent with impending rupture6, which are not documented covariates in our study and may contribute to an overall increase in adverse outcomes with a large sample. The female IRAD cohort also was noted to have a longer time from onset to presentation, with this delay in diagnosis or treatment potentially contributing to increased adverse outcomes after intervention due to progression of disease.
After a propensity weighted analysis was performed to adjust for baseline characteristics which may have contributed to differences in the unadjusted outcomes, the female cohort was found to have lower odds of acute renal failure and paraplegia and no significant difference for in-hospital mortality. In propensity-weighted subgroup analysis, the results observed in the unadjusted analysis persisted: both open and TEVAR groups had lower odds of acute renal failure in females, but open repair carried significantly higher odds of a cardiac event in women. Additionally, elderly female patients maintained both the lower odds of acute renal failure as well as higher odds of cardiac events overall. The IRAD study also did not reflect any significant differences between females and males for acute renal failure or cardiac events, both in the overall cohort or in intervention subgroups, but the analysis was also adjusted only for age, type of dissection, and hypertension, the sample size of TBAD compared to TAAD was small, and age stratification was not performed. However, in the general cardiovascular literature, population-based studies have reported increased risk for ischemic heart disease for post-menopausal women compared to men of similar age4,5.
The gender differences resulting in acute renal complications and paraplegia are difficult to identify using this dataset and may result from an unmeasured covariate, such as anatomic differences in the location or spread of the dissection, or other disease or progression of disease-specific characteristics such as degree of false-lumen thrombosis. Further study of large cohorts are necessary in order to determine the anatomic or disease-specific reasons for these differences that persist despite adjustment for age and comorbid or clinical conditions.
Analysis using administrative discharge databases, such as the NIS, has several limitations. All analysis is retrospective, and validity of all coding for diagnoses and procedures are not verifiable. In addition, the data are not longitudinally linked and do not contain any disease or procedure-specific information, nor do they contain time-course information about diagnoses or hospital course. In particular, we were unable to determine with a high degree of accuracy whether the presentation of dissection was complicated by malperfusion. Alpha correction for multiple comparisons was not utilized in this study, as the outcomes studied were intended for exploratory analysis rather than for purposes of causal inference. Despite these limitations, we believe that this study provides a broad overview of gender differences in a large national dataset of patients presenting with acute TBAD and may be informative for further study.
5. CONCLUSIONS
This review of a large, administrative database has shown that compared to males, females with TBAD present at a later age and have more comorbid conditions. Despite these differences, there was no gender-based impact on in-hospital mortality after propensity-weighted adjustment for age and clinical and comorbid conditions. However, females were more likely to sustain a perioperative cardiac event during open aortic surgical repair for TBAD and were less likely to experience acute renal failure. Elderly females were also less likely to experience acute renal failure but at the expense of higher odds of cardiac events, regardless of operative status. Future TBAD studies should attempt to identify anatomic and epidemiologic reasons for these gender differences.
Acknowledgments
This study was funded in part by grant 2T32HL098036-06 from the National Institutes of Health.
Footnotes
Presented at the plenary session of the 2016 annual winter meeting of the Vascular and Endovascular Surgery Society.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903. doi: 10.1001/jama.283.7.897. [DOI] [PubMed] [Google Scholar]
- 2.White RA, Miller DC, Criado FJ, et al. Report on the results of thoracic endovascular aortic repair for acute, complicated, type B aortic dissection at 30 days and 1 year from a multidisciplinary subcommittee of the Society for Vascular Surgery Outcomes Committee. J Vasc Surg. 2011;53(4):1082–1090. doi: 10.1016/j.jvs.2010.11.124. [DOI] [PubMed] [Google Scholar]
- 3.Singh M, Hager E, Avgerinos E, Genovese E, Mapara K, Makaroun M. Choosing the correct treatment for acute aortic type B dissection. J Cardiovasc Surg (Torino) 2015;56(2):217–229. [PubMed] [Google Scholar]
- 4.Ostadal B, Ostadal P. Sex-based differences in cardiac ischaemic injury and protection: therapeutic implications. Br J Pharmacol. 2014;171(3):541–554. doi: 10.1111/bph.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gutierrez-Chico JL, Mehilli J. Gender differences in cardiovascular therapy: focus on antithrombotic therapy and percutaneous coronary intervention. Drugs. 2013;73(17):1921–1933. doi: 10.1007/s40265-013-0135-y. [DOI] [PubMed] [Google Scholar]
- 6.Nienaber Ca, Fattori R, Mehta RH, et al. Gender-related differences in acute aortic dissection. Circulation. 2004;109(24):3014–3021. doi: 10.1161/01.CIR.0000130644.78677.2C. [DOI] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project (HCUP) Rockville M: HCUP National Inpatient Sample (NIS); www.hcup-us.ahrq.gov/nisoverview.jsp. Published 2012. [Google Scholar]
- 8.Sachs T, Pomposelli F, Hagberg R, et al. Open and endovascular repair of type B aortic dissection in the Nationwide Inpatient Sample. J Vasc Surg. 2010;52(4):860–866. doi: 10.1016/j.jvs.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Shah TR, Rockman CB, Adelman MA, Maldonado TS, Veith FJ, Mussa FF. Nationwide Comparative Impact of Thoracic Endovascular Aortic Repair of Acute Uncomplicated Type B Aortic Dissections. Vasc Endovascular Surg. 2014;48(3):230–233. doi: 10.1177/1538574413518122. [DOI] [PubMed] [Google Scholar]
- 10.Brunt ME, Egorova NN, Moskowitz AJ. Propensity score-matched analysis of open surgical and endovascular repair for type B aortic dissection. Int J Vasc Med. 2011;2011(2008) doi: 10.1155/2011/364046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity Measures for Use with Administrative Data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Kontopodis N, Antoniou SA, Georgakarakos E, Ioannou CV. Endovascular vs Open Aneurysm Repair in the Young: Systematic Review and Meta-analysis. J Endovasc Ther. 2015;22(6):897–904. doi: 10.1177/1526602815606937. [DOI] [PubMed] [Google Scholar]
- 13.Fattori R, Cao P, De Rango P, et al. Interdisciplinary expert consensus document on management of type B aortic dissection. J Am Coll Cardiol. 2013;61(16):1661–1678. doi: 10.1016/j.jacc.2012.11.072. [DOI] [PubMed] [Google Scholar]
- 14.Nienaber CA, Kische S, Rousseau H, et al. Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ Cardiovasc Interv. 2013;6(4):407–416. doi: 10.1161/CIRCINTERVENTIONS.113.000463. [DOI] [PubMed] [Google Scholar]
- 15.Pape LA, Awais M, Woznicki EM, et al. Presentation, Diagnosis, and Outcomes of Acute Aortic Dissection: 17-Year Trends From the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66(4):350–358. doi: 10.1016/j.jacc.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 16.Fattori R, Montgomery D, Lovato L, et al. Survival after endovascular therapy in patients with type b aortic DISSECTION: A report from the international registry of acute aortic dissection (IRAD) JACC Cardiovasc Interv. 2013;6(8):876–882. doi: 10.1016/j.jcin.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Tolenaar JL, Froehlich W, Jonker FHW, et al. Predicting In-Hospital Mortality in Acute Type B Aortic Dissection: Evidence From International Registry of Acute Aortic Dissection. Circulation. 2014;130(11_suppl_1):S45–S50. doi: 10.1161/CIRCULATIONAHA.113.007117. [DOI] [PubMed] [Google Scholar]
- 18.Jackson BM, Woo EY, Bavaria JE, Fairman RM. Gender analysis of the pivotal results of the Medtronic Talent Thoracic Stent Graft System (VALOR) trial. J Vasc Surg. 2011;54(2):358–363. 363.e1. doi: 10.1016/j.jvs.2010.12.064. [DOI] [PubMed] [Google Scholar]
- 19.Kasirajan K, Morasch MD, Makaroun MS. Sex-based outcomes after endovascular repair of thoracic aortic aneurysms. J Vasc Surg. 2011;54(3):669–676. doi: 10.1016/j.jvs.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Jones DW, Goodney PP, Nolan BW, et al. National trends in utilization, mortality, and survival after repair of type B aortic dissection in the Medicare population. J Vasc Surg. 2014;60(1):11–19. e1. doi: 10.1016/j.jvs.2013.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]