Abstract
Research on multiple health behaviours is increasing but little is known about parental behaviours and how they covary. Our study investigates cigarette smoking, alcohol intake, fruit and vegetable (F&V) consumption and physical activity among mothers and co-resident partners in England. Using the UK Household Longitudinal Study, we examined (i) clustering of health behaviours using observed-expected ratios and latent class analysis (ii) socio-demographic correlates of the derived latent classes and (iii) intra-couple concordance of individual health behaviours and their latent classes. We identified five latent classes for mothers and partners: Never smoked drinkers (28% of mothers; 29% of partners), Abstainers (25%; 17%), Drinkers and ex-smokers (19%; 26%), Unhealthy low frequency drinkers (18%; 16%) and Unhealthiest behaviour group (11%; 12%). These had distinctive social profiles. Never smoked drinkers were more likely than those in other groups to be white and socially advantaged: married, older, and with higher educational qualifications and incomes. Abstainers were non-smokers who never or occasionally drank, and were disproportionately drawn from ethnic minority groups and middle/lower income families. Drinkers and ex-smokers were the most physically active group and were more likely to be socially advantaged. Unhealthy low frequency drinkers were more likely to be disadvantaged and have a limiting long-standing illness. The Unhealthiest behaviour group had the highest proportion of smokers, heavy smokers and binge drinkers and the lowest F&V intake and physical activity levels. They were largely white and socially disadvantaged: younger, non-married and with lower educational levels. Mothers and their partners typically shared the same risk behaviours, and 44 per cent of partners and mothers belonged to the same latent class. Our findings point to the potential for a broadening of research and policy perspectives, from separate behaviours to combinations of behaviours, and from individuals to the domestic units and communities of which they are part.
Keywords: Cigarette smoking, Alcohol consumption, Physical activity, Diet, Latent class analysis, Social inequalities
Highlights
-
•
Little is known about the multiple health behaviours of couples with children.
-
•
Mothers and partners belong to five similar health behaviour groups (latent classes).
-
•
Mothers and partners were more likely than not to belong to the same class
-
•
The largest class – never smokers who drank frequently – were socially advantaged.
-
•
Those with the unhealthiest behaviours were more likely to be white and disadvantaged.
1. Introduction
Four behaviours – cigarette smoking, high alcohol intake, poor diet and physical inactivity – underlie the chronic diseases (cardiovascular disease, cancer, lung disease and type-2 diabetes) responsible for 70% of premature deaths in Europe (WHO, 2011, WHO, 2014). These behaviours have both separate and synergistic effects on health (Khaw et al., 2008, Kvaavik et al., 2010, Martin-Diener et al., 2014, WHO, 2008). Social disadvantage increases the risk of smoking, poor diet and physical inactivity; evidence for high alcohol intake is less consistent (Bloomfield et al., 2006, Stringhini et al., 2010). the four behaviours are a major focus of public health policies, with governments advising the public not to smoke and providing recommendations on minimum levels of physical activity and fruit and vegetables (F&V) intake and maximum thresholds for alcohol consumption.1
While much of the evidence focuses on single health behaviours, there is increasing appreciation that these behaviours are not independent (McAloney et al., 2014, Noble et al., 2015a, Prochaska et al., 2008). Earlier studies have investigated the co-occurrence of behaviours by establishing the prevalence of different risk behaviour combinations and/or by summing the number of risk behaviours reported by each study participant into a risk score. However, these approaches have limitations (McAloney et al., 2014; Noble et al., 2015a). Establishing that behaviours co-occur does not establish whether their co-occurrence differs from what would be expected given the prevalence of each behaviour, and risk scores do not indicate which behaviours contribute to an individual's score.
Studies are therefore increasingly going beyond co-occurrence and risk scores to examine inter-relationships between health behaviours. Recent reviews have identified two main analytical approaches: examining differences between observed and expected combinations of behaviour and interrogating underlying patterns across the behaviours (McAloney et al., 2014; Noble et al., 2015a). The first approach led the way in the analysis of multiple risk behaviours (McAloney et al., 2014). It uses dichotomous measures of behaviours and observed and expected (O/E) ratios to provide a simple summary measure of whether combinations of behaviours occurs more (or less) often than would be expected if the behaviours were independent.
Relying on more advanced statistical techniques, the second approach offers a number of analytic advantages. It moves beyond observed combinations of behaviour, to identify latent (or unobservable) types either of participants based on their behaviours (e.g. latent class analysis) or of behaviours (e.g. factor analysis) (Hofstetter, Dusseldorp, van Empelen & Paulussen, 2014). Latent class analysis (LCA) is increasingly used to investigate inter-relationships between behaviours (Mawditt et al., 2016, McAloney et al., 2014; Noble et al., 2015a). It identifies mutually exclusive behavioural clusters to which study participants are assigned on the basis of their probability of membership. While some studies use single dichotomous measures of behaviour based on adherence to national public health guidelines (e.g. de Vries et al., 2008), the methods allow a broader set of measures of the relevant behaviours to be included, for example, smoker/ex-smoker/never smoker. In addition, by identifying underlying relationships between behaviours, a potentially large number of behavioural combinations can be reduced to a smaller number of behavioural classes (McAloney et al., 2014, Muthén, 2001). The socio-demographic profile of the resultant classes can also be described, for example by regression analyses to predict class membership (Cleveland et al., 2010, Evans-Polce et al., 2016, Robinson, 2012).
However, while evidence on multiple risk behaviours is accumulating, there are important gaps. Despite the policy emphasis on settings-based approaches to health promotion (Poland et al., 2009, WHO, 2013), we found no studies investigating intra-household associations in multiple risk behaviours. In addition, most studies focus on the general population, together with a few studies of younger adults, older people and patient populations (e.g. people with hypertension, cancer survivors) (King et al., 2015, McAloney et al., 2014; Noble et al., 2015a). Neither of the reviews of multiple health behaviours studies included studies of parents or reported measures that enabled identification of parents, e.g. presence of dependent children in the household (King et al., 2015, McAloney et al., 2014; Noble et al., 2015a). A citation search of the reviews identified a further five studies of clustering of the four behaviours covered here (Bryant et al., 2013, Filippidis et al., 2015, Kritsotakis et al., 2016, Mawditt et al., 2016, Morris et al., 2016). Again, none provided information on parental health behaviours.
As this suggests, little is known about parental health behaviours and how they covary. Yet parents caring for dependent children represent a large sub-group of the population. In the UK, they represent 31% of all adults (Office of National Statistics (ONS, 2014). Over a third of UK married couples (38%) and cohabiting couples (41%) are caring for dependent children in the family, and 75% of children are living in two-parent households (ONS, 2015). Childhood and adolescence are formative periods for the development of health behaviours which persist into adulthood (Ebrahim et al., 2004, Jefferis et al., 2004, Schooling and Kuh, 2002) and parents are an important influence on the behaviours of their children (Brown and Ogden, 2004, Edwardson and Gorely, 2010, Gilman et al., 2009, Pearson et al., 2009, Van Der Vorst et al., 2005).
Our study investigates patterns of smoking, alcohol intake, F&V consumption and physical inactivity among co-resident parents caring for dependent children in England. Within the UK's devolved structure, England's health policy has a particularly strong emphasis on health behaviours (Graham, 2009, Smith and Collin, 2013) and the study funder's remit is to provide evidence to inform this policy. We include measures based on government recommendations (‘health risk behaviours’) along with a fuller range of measures of the four behaviours. Looking separately at mothers and partners, we examine (i) inter-relationships between heath behaviours using observed-expected ratios and LCA and (ii) the socio-demographic correlates of the latent classes. Focusing on mother-partner pairs, we examine (iii) intra-couple concordance of health risk behaviours and class membership. Because ‘class’ is commonly used to refer to an individual's socioeconomic background, we use ‘group’ and ‘latent class’ when referring to the classes derived from the LCA.
2. Design and methods
2.1. The study population
The UK Household Longitudinal Study (UKHLS) is a panel study of individuals from c28,000 UK households and an ethnic minority boost sample of around 4000 households. Study participants were first surveyed in 2009/10 and are followed up each year (Buck and McFall, 2011, ISER and NatCen Social Research, 2012). In 2010/11 (wave 2), the UKHLS included questions on the four health behaviours.
We defined mothers as adult non-pregnant women (aged 16 years and over) who lived in England and had a child <16 years living with them at the time of the interview whom they reported to be their natural, step, foster, or adoptive child. A small proportion (3.3%) of mothers was excluded because they were pregnant. Partners were the co-resident partners of mothers. Almost all (99.6%) of the partners were male and most (78%) were married to the mother. Further sample details are given in Supplementary Appendix A1.
2.2. Questions on health behaviour
The main interview included questions on smoking, F&V consumption and physical activity; alcohol consumption was part of a separate self-completion questionnaire (details in Supplementary Appendix A2). A high proportion of responses were missing for alcohol consumption among minority ethnic groups; imputed values were therefore derived from median values matched for ethnic and religious group, marital status and country of birth (see Appendix A2).
Behavioural measures included ones aligned to government recommendations for smoking, single-occasion alcohol intake (consuming more than twice the recommended daily limit, with separate limits set for men and women) and F&V consumption; for physical activity, we derived a measure that approximated to the recommendation (see Box 1). These binary measures (meeting/not meeting the relevant recommendation) were used for investigating clustering using observed-expected ratios; for the LCA, additional categories and a wider range of behaviour measures were used (see Box 2). In addition to current smoking behaviour, age of smoking initiation was used in the LCAs because early smoking initiation is associated with difficulty quitting and longer term use, as well as with heavier smoking (Breslau et al., 1993, Lando et al., 1999).
Box 1. Measures of health risk behaviours used in the analyses (in italics) aligned to government recommendations (in bold).
Smoking recommendation: do not smoke.
Smokes ≥1 cigarette a day.
Alcohol consumption recommendation: on most days do not drink more than 2-3 units (women) or 3-4 units (men) of alcohol a day and on no days drink more than 6 units (women) or 8 units (men).
Consumed more than twice the daily recommended units of alcohol on their heaviest drinking day in the past week (‘binge’ drinking): >6 units (women) or >8 units (men).
Fruit and vegetable consumption recommendation: eat at least 5 portions of fruit and/or vegetables a day.
Consumed <5 portions of fruit and vegetables on average per day.
Physical activity recommendation: engage in at least 150 minutes a week of moderate to vigorous intensity physical activity per week in bouts of 10 minutes or more, or engage in at least 75 minutes a week of vigorous intensity physical activity or an equivalent of the two.
Did not engage in
-
•
30 minutes or more of brisk or fast walking 20 times in the past four weeks
-
•
or moderate to vigorous activity more than 3 days a week
-
•
or did not engage in a combination of these activities (i.e. 30 minutes or more brisk or fast walking for 4 days a week and 1 day or more a week moderate to vigorous sports activity).
(For further information on government guidelines, see Department of Health, 2003, Department of Health, 2005, Department of Health, 2011, Department of Health, 2013a, Department of Health, 2013b)
Box 2. Behavioural measures used in the LCA.
-
•
Smoking status (6 categories incl. non-smoker, ex-regular smoker & average current daily cigarette consumption).
-
•
Age started smoking (5 categories).
-
•
Drinking frequency (9 categories).
-
•
Number of alcoholic units consumed on the heaviest day in the past 7 days (8 categories).
-
•
Fruit and vegetable portions consumed per day (4 categories)
-
•
Number of days walking briskly or fast paced in the past 4 weeks (7 categories).
-
•
Frequency of participation in moderate to vigorous sporting activities over the last 12 months (7 categories).
2.3. Analysis techniques
Analyses were conducted in Stata with the exception of the LCA which was conducted using latentGOLD software version 4.5 (Vermunt & Magidson, 2008). Adjustments were made for the survey's complex survey design and differential non-response (Knies, 2014); all results refer to weighted estimates (further details on weighting are given in Appendix A3).
With the exception of intra-couple concordance, analyses were conducted separately for mothers and partners. Clustering was investigated using both O/E ratios and LCA. Analyses based on O/E ratios included mothers and their partners with data (self-reported responses or imputed values) for the four behaviours (mothers: unweighted n=2538; partners: unweighted n=2538). O/E ratios were calculated for each risk behaviour combination, for example not meeting recommendations for F&V and physical activity but meeting the smoking and alcohol intake recommendations. Values >1 and <1 indicated clustering; statistical significance was based on 95% confidence intervals.
The LCA included respondents with data for the full range of behavioural measures (Box 2) (mothers: unweighted n=3397; partners: unweighted n=2554). All mothers and partners who answered the behaviour questions were included. With no definitive method of determining the optimal number of classes, we considered measures of fit (Akaike's Information Criterion and the Bayesian Information Criterion), the misclassification rate, the percentage of cases in each class with a low probability of class membership, class stability across successive class solutions and the interpretability of the resulting classes (Nylund et al., 2007, Weich et al., 2011). Further information is provided in the Supplementary Appendix A4. We attached particular importance to the interpretability of the resulting classes when determining the final number of classes. Individuals were allocated to a class on the basis of their probability of membership (Clark & Muthén, 2009)
The socio-demographic correlates of each LCA class were determined using stepwise logistic regression, with class membership as the dependent variable and socio-demographic factors as predictors (details in Appendix). We included socio-demographic factors predictive of multiple health behaviours among adults (Conry et al., 2011; Noble et al., 2015a; Poortinga, 2007), together with those reported in studies of parental health behaviours (Bartley et al., 2004, Robinson et al., 2004, Schoon and Parsons, 2003). We included: age, domestic relationships (marital status, number of children, age of youngest child), socioeconomic circumstances (education, household income), employment status, ethnic background and health status (limiting long-standing illness). The social profile of each class was determined by producing predicted probabilities of belonging to a class for socio-demographic factors that remained significant predictors in regression models. The small number of black African and Arabs were combined with Indian, Pakistani and Bangladeshi groups; the majority of this combined group were from South Asia.
Analyses of intra-couple concordance included couples where both mother and partner had data for the relevant behavioural measures: 2538 couples for concordance in the couple's risk behaviours and 2361 couples for concordance in their latent classes. Logistic regression was used to determine significant associations between mothers’ and partners’ latent classes.
3. Results
3.1. Multiple health risk behaviours: prevalence and clustering using O/E ratios
The majority of mothers and partners did not meet the recommendations for F&V consumption (mothers: 80%; partners: 86%) and physical activity (77%; 72%). A larger proportion of partners (32%) than mothers (22%) reported alcohol intakes in the previous seven days that exceeded binge drinking thresholds; a larger proportion of partners (24%) than mothers (19%) were also smokers. Partners had more risk behaviours than mothers: 78% had two or more risk behaviours compared to 74% of mothers. A smaller proportion of partners than mothers (3% vs 5%) reported no risk behaviours and a higher proportion (7% vs 4%) reported all four risk behaviours.
The most commonly-occurring combination of risk behaviours was not meeting the recommended levels of F&V consumption and physical activity. However, there was no evidence of clustering. Clustering was apparent for having all four, and having no, risk behaviours. Drinking risk without any other risk behaviour was also more common than expected. In addition, there were four behavioural combinations that occurred less frequently than expected: smoking risk only; F&V and smoking risk; physical activity and smoking risk; and F&V, physical activity and drinking risk. Details are provided in supplementary Table S1.
3.2. Multiple health behaviours: identifying latent classes
For both mothers and their partners, the LCA indicated that a 5-class solution was optimal. The 5-class solutions were also very similar for both mothers and partners (Table 1, Table 2) and are summarised below.
Table 1.
Latent classes: mothers.
| Behaviours | Classes |
|||||
|---|---|---|---|---|---|---|
| Never-smoked drinkers | Abstainers | Unhealthiest | Drinkers & ex-smokers | Unhealthy low frequency drinkers | All | |
| % | % | % | % | % | % | |
| Group size | 28 | 25 | 11 | 19 | 18 | 100 |
| Smoking status | ||||||
| non-smoker | 88 | 94 | 48 | |||
| past experimenters | 12 | 6 | 5 | |||
| Ex-regular smoker | 33 | 82 | 51 | 28 | ||
| Current smoker – light | 12 | 15 | 14 | 7 | ||
| Current smoker – moderate | 41 | 2 | 23 | 9 | ||
| current smoker – heavy | 15 | 0 | 12 | 4 | ||
| Age started smoking | ||||||
| Never smoked/not regular smoker | 100 | 100 | 53 | |||
| Under 16 | 56 | 29 | 45 | 20 | ||
| 16–18 | 34 | 46 | 39 | 19 | ||
| 19–24 | 8 | 21 | 13 | 7 | ||
| 25+ | 1 | 4 | 3 | 1 | ||
| Drinking frequency | ||||||
| Almost everyday | 5 | 0 | 10 | 7 | 4 | |
| 5/6 days per week | 7 | 5 | 10 | 4 | ||
| 3/4 days per week | 20 | 17 | 28 | 13 | ||
| Once or twice a week | 42 | 5 | 45 | 32 | 4 | 24 |
| Once or twice a month | 19 | 13 | 17 | 16 | 20 | 17 |
| Every couple of months | 6 | 15 | 5 | 3 | 27 | 12 |
| Once or twice a year | 0 | 20 | 1 | 2 | 31 | 11 |
| Have not had a drink in last year | 9 | 7 | 4 | |||
| Did not answer question | 37 | 1 | 10 | 11 | ||
| Number of units on heaviest drinking day | ||||||
| Did not drink in past week | 1 | 96 | 1 | 2 | 91 | 41 |
| Up to and including 2 | 24 | 3 | 5 | 13 | 7 | 12 |
| Over 2 and up to (& including) 3 | 5 | 3 | 2 | 1 | 2 | |
| Over 3 and up to (& including) 4 | 24 | 14 | 21 | 1 | 12 | |
| Over 4 and up to (& including) 5 | 3 | 1 | 6 | 1 | 2 | |
| Over 5 and up to (&including) 6 | 18 | 18 | 18 | 10 | ||
| Over 6 and up to (& including) 8 | 12 | 19 | 16 | 9 | ||
| Over 8 | 13 | 34 | 27 | 12 | ||
| Fruit and vegetable portions per day | ||||||
| 5 or more portions | 24 | 19 | 6 | 34 | 13 | 21 |
| 3 or 4 portions | 43 | 35 | 16 | 39 | 26 | 34 |
| 1 or 2 portions | 8 | 15 | 19 | 7 | 13 | 12 |
| none | 24 | 31 | 59 | 20 | 48 | 33 |
| Not meeting F&V recommendations | 75.8 | 81.3 | 94.1 | 66.1 | 86.6 | 79.2 |
| Number of days brisk or fast paced walking in past 4 weeks | ||||||
| None | 59 | 74 | 85 | 51 | 74 | 67 |
| 1–4days | 11 | 6 | 5 | 12 | 9 | 9 |
| 5–9 days | 7 | 5 | 3 | 9 | 4 | 6 |
| 10–14 days | 6 | 3 | 2 | 8 | 3 | 5 |
| 15–19 days | 3 | 1 | 3 | 1 | 2 | |
| 20–24 days | 6 | 6 | 3 | 4 | 4 | 5 |
| 25–29 days | 9 | 5 | 2 | 13 | 5 | 7 |
| Frequency of participation in moderate activity | ||||||
| no moderate activities | 13 | 43 | 42 | 6 | 40 | 27 |
| three or more times a week | 17 | 12 | 4 | 24 | 8 | 13 |
| at least once a week | 27 | 15 | 6 | 28 | 13 | 18 |
| at least once a month | 20 | 12 | 13 | 21 | 16 | 16 |
| at least 3 or 4 times a year | 16 | 12 | 22 | 12 | 14 | 15 |
| twice in last 12 months | 5 | 4 | 10 | 5 | 5 | 6 |
| once in last 12 months | 3 | 3 | 3 | 4 | 3 | 3 |
| Not meeting physical activity recommendations | 71.3 | 80.4 | 90.7 | 65.1 | 84.6 | 76.7 |
| Unweighted Bases | 880 | 1118 | 301 | 567 | 531 | 3397 |
| Weighted Bases | 867 | 771 | 330 | 582 | 565 | 3115 |
Table 2.
Latent classes: partners.
| Behaviour | Classes |
|||||
|---|---|---|---|---|---|---|
| Never-smoked, drinkers | Abstainers | Unhealthiest | Drinkers & ex-smokers | Unhealthy low frequency drinkers | All | |
| % | % | % | % | % | % | |
| Group size | 29 | 17 | 12 | 26 | 16 | 100 |
| Smoking status | ||||||
| non-smoker | 83 | 92 | 39 | |||
| past experimenters | 17 | 8 | 6 | |||
| Ex-regular smoker | 14 | 73 | 45 | 28 | ||
| Current smoker – light | 1 | 21 | 14 | 8 | ||
| Current smoker – moderate | 43 | 6 | 25 | 11 | ||
| current smoker – heavy | 42 | 17 | 8 | |||
| Age started smoking | ||||||
| Never smoked/not regular smoker | 100 | 100 | 46 | |||
| Under 16 | 60 | 30 | 44 | 22 | ||
| 16–18 | 33 | 44 | 35 | 21 | ||
| 19–24 | 7 | 20 | 14 | 8 | ||
| 25+ | 5 | 7 | 2 | |||
| Drinking frequency | ||||||
| Almost everyday | 8 | 26 | 11 | 9 | ||
| 5/6 days per week | 7 | 7 | 12 | 3 | 7 | |
| 3/4 days per week | 29 | 18 | 29 | 18 | ||
| Once or twice a week | 45 | 8 | 34 | 33 | 9 | 29 |
| Once or twice a month | 10 | 21 | 10 | 13 | 27 | 15 |
| Every couple of months | 1 | 20 | 4 | 1 | 21 | 8 |
| Once or twice a year | 0 | 15 | 1 | 18 | 5 | |
| Have not had a drink in last year | 7 | 7 | 2 | |||
| Did not answer question | 29 | 0 | 15 | 7 | ||
| Number of units on heaviest drinking day | ||||||
| Did not drink in past week | 1 | 86 | 0 | 86 | 28 | |
| Up to and including 2 | 11 | 8 | 8 | 10 | 8 | |
| Over 2 and up to (& including) 3 | 1 | 1 | 0 | 1 | 0 | 1 |
| Over 3 and up to (& including) 4 | 17 | 3 | 5 | 13 | 2 | 10 |
| Over 4 and up to (& including 5 | 2 | 1 | 0 | 1 | ||
| Over 5 and up to (&including 6) | 16 | 1 | 10 | 12 | 1 | 9 |
| Over 6 and up to (& including 8) | 16 | 15 | 17 | 11 | ||
| Over 8 | 37 | 1 | 69 | 47 | 32 | |
| Fruit and vegetable portions per day | ||||||
| 5 or more portions | 20 | 12 | 2 | 17 | 8 | 14 |
| 3 or 4 portions | 30 | 27 | 14 | 29 | 17 | 25 |
| 1 or 2 portions | 12 | 16 | 12 | 16 | 18 | 15 |
| none | 38 | 45 | 73 | 38 | 57 | 46 |
| Not meeting F&V recommendations | 79.9 | 88.0 | 97.9 | 83.0 | 91.6 | 86.0 |
| Number of days brisk or fast paced walking in past 4 weeks | ||||||
| None | 51 | 70 | 67 | 54 | 63 | 59 |
| 1–4days | 16 | 11 | 12 | 14 | 12 | 14 |
| 5–9 days | 11 | 4 | 4 | 6 | 8 | 7 |
| 10–14 days | 6 | 4 | 3 | 6 | 4 | 5 |
| 15–19 days | 3 | 1 | 3 | 3 | 1 | 2 |
| 20–24 days | 5 | 4 | 5 | 6 | 1 | 5 |
| 25–29 days | 9 | 7 | 5 | 10 | 10 | 8 |
| Frequency of participation in moderate+ sporting activity | ||||||
| no moderate activities | 11 | 33 | 39 | 6 | 32 | 20 |
| three or more times a week | 19 | 14 | 9 | 25 | 13 | 17 |
| at least once a week | 27 | 19 | 15 | 25 | 17 | 22 |
| at least once a month | 20 | 16 | 10 | 23 | 14 | 18 |
| at least 3 or 4 times a year | 16 | 12 | 16 | 16 | 17 | 16 |
| twice in last 12 months | 4 | 3 | 7 | 3 | 5 | 4 |
| once in last 12 months | 2 | 2 | 4 | 3 | 2 | 3 |
| Not meeting physical activity recommendations | 70.5 | 75.9 | 81.3 | 65.1 | 79.3 | 72.6 |
| Unweighted Bases | 706 | 531 | 265 | 617 | 435 | 2554 |
| Weighted Bases | 750 | 425 | 313 | 677 | 405 | 2570 |
Never-smoked drinkers were the largest group among both mothers (28%) and partners (29%). The group 'were never regular smokers' is more accurate because some had experimented. They frequently consumed alcohol (74% of mothers and 89% of partners drank more than once a week), and a sizeable minority binge drank (25% of mothers and 37% of partners), but drank fewer units than other groups who engaged in binge drinking. They were above average consumers of F&V (but 76% of mothers and 80% of partners consumed less than 5 portions a day) and engaged in average physical activity compared to other mothers and partners (71% of mothers and partners did not meet the recommended levels).
Abstainers were the second largest group among mothers (25%) and a smaller proportion (17%) of partners. It also consisted of non-smokers but, unlike the Never-smoked drinkers, they were occasional or non-drinkers. None of the mothers and 1% of partners had drunk more than twice the recommended level per day in the previous week. They had average F&V intake (81% of mothers and 88% of partners did not meet the recommendations) and engaged in slightly below average physical activity (80% and 76% respectively did not meet the recommendation).
Unhealthiest behaviour group represented a similar proportion of mothers (11%) and partners (12%). It contained the highest proportion of current smokers (67%; 86%) and heavy (≥20 a day) smokers (15%; 42%); many started smoking before the age of 16. The group also had the highest proportion of binge drinkers (53%; 69%). They had the lowest F&V intake of any group. Nearly all (94%; 98%) did not meet the recommendation; most (59%; 73%) did not eat any F&V. The group also had the lowest participation in physical activity (91%; 81%). With the exception of physical activity, partners had less healthy lifestyles than mothers in this group.
Drinkers and ex-smokers but the most physically active with high F&V consumption represented 19% of mothers and was the second largest group among partners (26%). It consisted mainly of ex-smokers (81%; 73%) along with some current light or moderate smokers (19%; 27%), and had a lower proportion that started smoking before the age of 16 than other groups with current or ex-smokers. The group contained frequent drinkers and a high proportion that exceeded the binge drinking threshold (44%; 64%). However, the group had the one of the highest intake of F&V, but most (66%; 83%) still did not meet the recommendation. It had the most frequent participation in physical activity and the lowest proportion of any group (65%; 65%) did not meet the physical activity recommendation. Partners had unhealthier behaviours than mothers, except for physical activity.
Unhealthy low frequency drinkers contained a similar proportion of mothers (18%) and partners (16%). It consisted of occasional or non-drinkers, and none had exceeded the binge drinking threshold. However, the group was unhealthy in relation to the other three health behaviours. Large proportions (49%; 56%) were current smokers. They were low F&V consumers; 87% of mothers and 92% of partners consumed less than 5 portions a day. They were also low participators in physical activity; 87% and 92% respectively did not reach the recommended level.
3.3. Social patterning of latent classes
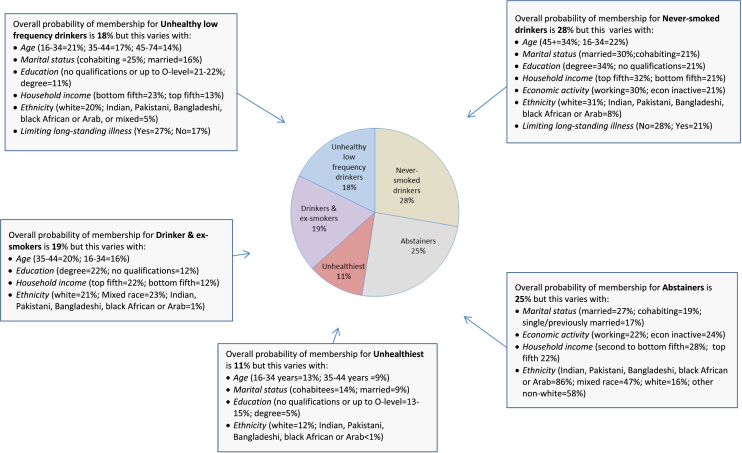
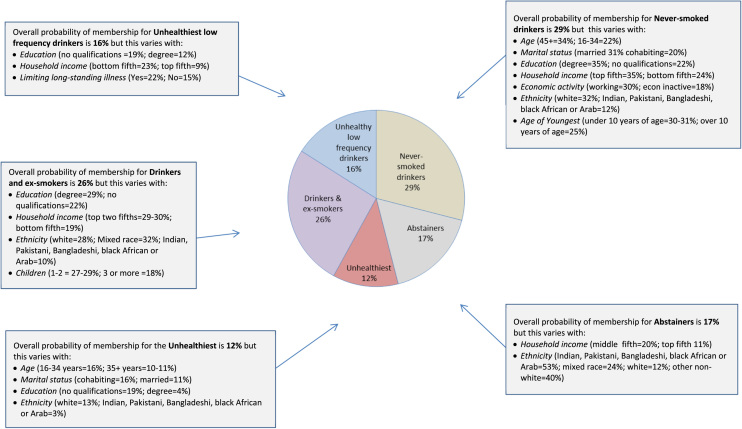
The sociodemographic characteristics of the five latent classes are summarised below (patterns are for both mothers and partners unless noted otherwise) and in Fig. 1 (mothers) and Fig. 2 (partners). Details of the regression models, estimated odds of class membership and the class profiles by sociodemographic factors are given in Tables S2–S7.
Fig. 1.
Social patterning of mothers' latent classes.
Fig. 2.
Social patterning of partners' latent classes.
Never smoked drinkers were more likely than those in other groups to be older, married, employed, with higher educational qualifications and higher incomes. They were more likely to be white and less likely to be from a minority ethnic background (Indian, Pakistani, Bangladeshi, black African or Arab). In addition, mothers were less likely to have a limiting long-standing illness.
Abstainers were less likely than those in other groups to be white and more likely to be Indian, Pakistani, Bangladeshi, black African/Arab, mixed race and other non-white; they were also more likely to live in middle income households. In addition, mothers were more likely to be married.
Those in the unhealthiest behaviour group were more likely to be white younger, not married and with lower educational qualifications. Mothers, were likely to be in the household income quintile and were unlikely to be Indian, Pakistani, Bangladeshi, black African/Arab.
Drinkers and ex-smokers were lowest likely to have higher educational qualifications and household incomes that lifted them out of the lowest two income quintiles. Mothers in particular were unlikely to be Indian, Pakistani, Bangladeshi, black African or Arab. Mothers were additionally more likely to be older (35–44), cohabitees and less likely to have a limiting long-standing illness. Partners were additionally more likely to have one or two children rather than three or more.
Unhealthy low frequency drinkers were more likely to have no/low educational qualifications, live in a lower-income household and have a limiting long-standing illness. In addition, mothers were less likely to be married and to be Indian, Pakistani, Bangladeshi, black African or Arab and more likely to be younger.
3.4. Intra-couple concordance of health risk behaviours and latent class membership
There was a high degree of concordance among couples in their health risk behaviours; the observed associations were all significantly different (p<0.001) from what would be expected if the behaviours of a mother and her partner were independent of each other. Concordance ranged from 83% for smoking to 66% for low physical activity (Table 3). In 13% of families, both parents were smokers. In 13% of families, both partners exceeded the threshold for binge drinking. In 72% of couples, neither parent met the ‘5 a day’ recommendation for F&V intake; in 58% of couples, neither met the physical activity recommendations.
Table 3.
Single risk behaviours of mothers and their partners.
| Behaviours |
Mothers |
Total (%) | ||
|---|---|---|---|---|
| No Risk (%) | Risk (%) | |||
| Smoking | Non-smoker | Smoker | ||
| Partners | Non-smoker | 70 | 6 | 76 |
| smoker | 11 | 13 | 24 | |
| Total | 81 | 19 | 100 | |
| Binge drank in last 7 days | Below binge levels | Binge drank | ||
| Partners | Below binge levels | 59 | 9 | 68 |
| Binge drank | 19 | 13 | 32 | |
| Total | 78 | 22 | 100 | |
| Fruit and vegetable portions per day | 5 or more a day | Less than 5 a day | ||
| Partners | 5 or more a day | 6 | 7 | 14 |
| Less than 5 a day | 14 | 72 | 86 | |
| Total | 20 | 80 | 100 | |
| Walking fast or briskly 5 days/week or moderate+ activity 3 days/ week | High physical activity | Low physical activity | ||
| Partners | High PA | 8 | 20 | 28 |
| Low PA | 15 | 58 | 72 | |
| Total | 23 | 77 | 100 | |
p<0.001 for all four cross-tabulations.
In 44% of couples, the mother and her partner belonged to the same latent class (sum of the shaded diagonals in Table 4). In the logistic regression analyses, there were significant associations (p<0.001) between the behavioural classes to which mothers their partners belonged: they were between three and six times more likely to be members of the same group than not. Odds of belonging to the same latent class were the highest when couples were both Abstainers (6.66; 95%CI 5.19, 8.54) or both allocated to the Unhealthiest class (6.59; 95%CI 4.763, 9.16). Out of the 25 possible class combinations, the largest group of couples (15.1%) were both Never-smoked drinkers (Table 4); they were the largest latent class among mothers (28%) and partners (29%) and had a high odds of living with a partner who was also a Never-smoked drinker (OR=4.60; 95%CI 3.71, 5.69). The odds of Unhealthy low frequency drinkers living together was 4.44 (95%CI 3.39, 5.81) and of Drinkers and ex-smokers living together was 3.30 (95%CI 2.56, 4.25).
Table 4.
Latent classes of mothers and their partners.
| Mother's latent class |
total | ||||||
|---|---|---|---|---|---|---|---|
| Never-smoked drinkers | Abstainers | Unhealthy Low freq drinkers (LFD) | Unhealthiest | Drinkers & ex-smokers | |||
| Partner's latent class | Never-smoked, drinkers | 15.1% | 6.1% | 1.9% | 1.5% | 5.5% | 30.2% |
| Abstainers | 2.0% | 9.6% | 3.0% | 0.5% | 1.0% | 16.1% | |
| Unhealthy LFD | 1.7% | 4.8% | 6.6% | 1.3% | 1.4% | 15.8% | |
| Unhealthiest | 1.6% | 1.1% | 3.3% | 4.1% | 1.8% | 11.9% | |
| Drinkers & ex-smokers | 7.2% | 3.2% | 3.6% | 3.3% | 8.7% | 26.0% | |
| Total | 27.5% | 24.8% | 18.4% | 10.8% | 18.4% | 100% | |
p<0.001 overall for chi2 cross-tabulation.
4. Discussion
Focusing on parents, we examined the inter-relationships and social patterning of the four health behaviours that contribute most to chronic disease. As far as we are aware, ours is the first study to focus on this key population group.
We based our study on the UK's largest nationally-representative household survey. We exploited three features of the UKHLS: the inclusion of questions on health behaviours in the 2010/11 survey, its household structure and its rich social data. Its range of behavioural questions enabled us to derive measures of risk behaviours based on government guidelines along with a wider set of measures of the four behaviours. Its household structure permitted analysis of intra-couple concordance in risk behaviours and behavioural classes and its rich social data meant we could investigate the patterning of behavioural classes by multiple dimensions of social background and identity.
Using O/E-based analyses, we found clustering at both ends of the risk continuum: not meeting recommendations for any behaviour and meeting all the recommendations occurred more than would be expected if the behaviours were independent. In studies of the general population, a similar clustering has been found (Berrigan et al., 2003, Laaksonen et al., 2001, Poortinga, 2007, Schuit et al., 2002). However, as in other studies, only a small proportion fell into these outlier groups: 8% of mothers and 10% of partners. For over 70% of mothers and partners, risk behaviours combined in ways that did not differ significantly from the patterns expected based on their separate prevalence.
Using a wider range of behavioural measures, the latent class analyses enabled us to identify five latent classes to which mothers and partners could be allocated. The behavioural classes were independently estimated for mothers and partners but were similar for both, adding confidence to our analysis.
Like the O/E-based approach, the LCA pointed to a high-risk group (Unhealthiest behaviour group). This group contained the highest proportion of smokers, heavy smokers, binge drinkers and those both failing to meet the recommendation for F&V and consuming no F&V. It also contained the lowest proportion meeting the physical activity recommendation. Other studies have suggested that addictive behaviours like smoking and alcohol consumption cluster (de Vries et al., 2008) and that smoking has the strongest and most consistent associations with other risk behaviours (Berrigan et al., 2003, Laaksonen et al., 2001, Poortinga, 2007, Schuit et al., 2002). However, our latent classes included ones in which smoking was associated with occasional and low alcohol intake (Unhealthy low frequency drinkers) and conversely never smoking was part of a lifestyle that included frequent drinking (Never smoked drinkers). The group least likely to either smoke or to drink was the Abstainers. While their lifestyles were health-promoting with respect to these behaviours, other groups had higher levels of F&V consumption and physical activity, including the Drinkers and ex-smokers. As these patterns suggest, health behaviours combine in more varied ways than characterisations of ‘high risk’ and ‘low risk’ groups may suggest.
With respect to the social patterning, socioeconomic background has long been known to be a predictor of multiple health behaviours. Our study additionally highlighted the importance of ethnic background. With the exception of partners who were Unhealthy low frequency drinkers, both social factors influenced the probability of belonging to a latent class. Thus, never smoking and frequent drinking was associated with multiple advantages: being white, older, more highly educated and better-off. Conversely, the combination of never smoking and never drinking (Abstainers) was more strongly associated with being from a minority ethnic group and living in a low to middle-income household. Indeed the overwhelming majority of parents from minority ethnic groups fell into this group. Other UK studies have pointed to healthier behaviours among minority ethnic groups (Lawder et al., 2010); however in our study, Abstainers had average F&V intake and below average levels of physical activity. The latent class occupied by a high proportion of drinkers and ex-smokers again had a distinctive social profile: more socio-economically advantaged and less likely to belong to a minority ethnic group. Parents with the most health-damaging lifestyles (heavy smoking, binge drinking, diets with little or no F&V, and low levels of physical activity) were most likely to be white and socially disadvantaged.
With respect to intra-couple concordance, mothers and partners often had risk behaviours in common. This meant that children in most families were growing up with parents who were both non-smokers; however, in 1 in 8 families, both were smokers. Similarly, in most families neither parent reported drinking at levels that met the threshold for binge drinking. However, in 1 in 8 families, both parents were binge drinkers. In a larger proportion (over half) of households, neither parent met the physical activity guidelines; in over 70%, neither parent met the dietary recommendations. Because the analyses were cross-sectional, we were unable to examine whether an individual's health behaviours influence those of their partner's, e.g. whether a smoker quits smoking when in a cohabiting relationship with a non-smoker.
We also found significant associations in the latent classes to which mothers and their partners belonged: mothers and partners were much more likely than not to be members of the same behaviour group. Couples where both partners were Never-smoked drinkers made up the largest group of couple combinations. This suggests that, in around 1 in 7 two-parent families, never smoking but frequent alcohol consumption by both parents is a common pattern; in this group, a sizeable minority (1 in 4 mothers and over 1 in 3 partners) also binge drank. As noted above, parents in this group are likely to enjoy a range of social and material advantages. This can be contrasted with the Abstainer couples, who represented 1 in 10 of couples. Compared to other groups, these non-smoking and low/non-drinking families are characterised by their greater socio-economic disadvantage (higher rates of unemployment and economic inactivity and middle to lower incomes).
Some limitations of our study should be noted. The UKHLS included a restricted range of health behaviour questions from which to derive proxies for current (2010/11) recommendations (Box 1). For alcohol consumption, our focus was restricted to binge drinking in the previous week; we were unable to consider government guidelines on weekly consumption. It should also be noted that the binge drinking recommendation has been revised by the UK government; in 2016, the threshold for men was lowered to match the one for women (Department of Health, 2016). In addition, like most studies of health behaviours, our study is based on self-reported data which are less reliable than objective measures (Celis-Morales et al., 2012). In addition, questions on three of the behaviours were asked as part of the interviewer-administered component; such questions are more susceptible to response bias (Tipping et al., 2010). Alcohol intake was recorded in a confidential self-completion questionnaire, potentially reducing social desirability bias (Tipping et al., 2010). However, parents from minority ethnic groups tended not to answer the alcohol questions, requiring data imputation.
Focused on couples, our study excluded lone parent families, the large majority of which were female-headed. Rerunning the analyses of partnered mothers to include all mothers left the results for all analyses substantively unchanged.
Finally, there is a diversity of approaches to latent class analysis, including approaches to the inclusion of covariates. Results can be difficult to compare across studies because they are highly dependent on the measures and methods of analysis (Berrigan et al., 2003, de Vries et al., 2008, McAloney et al., 2014; Noble et al., 2015a; Noble et al., 2015b). The allocation of individuals to a class is based on their having the highest probability of being in it for their given behaviour profile, but the behaviours of those allocated to the same class can vary between individuals.
5. Conclusion
While there is increasing research on multiple risk behaviours, little attention has been given to parental behaviours and how they covary. Our study focused on mothers and co-resident partners, the domestic unit in which the majority of children are brought up, and investigated the four health behaviours that contribute most to chronic disease and premature mortality. We uncovered five distinctive behavioural groups. By predicting membership of these groups on the basis of socio-economic and ethnic background, we could identify the ways in which patterns of health behaviour were differentiated by social position.
Such evidence offers insights for public health policies informed by social determinants of health perspectives, where both behavioural factors and social circumstances are identified as shaping people's health (Marmot, Allen, Bell, Bloomer & Goldblatt, 2012). It suggests that these perspectives could be used in differentiated ways for different sub-groups. For example, parents with the most health-damaging lifestyles (heavy smoking, binge drinking, diets with little or no F&V, and low levels of physical activity) were most likely to be white and socially disadvantaged. Policies that address the wider determinants of their social disadvantage – over their life course and through the early years of their children's lives – are therefore likely to be essential if their lifestyles are to improve. However, in our study the largest group of mothers and partners were not socially disadvantaged. The never smokers who drank frequently (and failed to meet recommendations for diet and physical activity) were characterised by their multiple social advantages. They were more likely to be white, well-educated, married and well-off. In this group, policies tackling wider determinants like low educational attainment and low income would be unlikely to be accompanied by improvements in their lifestyle. Instead, information-based approaches explicitly targeted at the lifestyles of advantaged families may offer a more effective approach.
If future studies identify similar combinations and social patterning of multiple health behaviours, our findings would support a shift in public health research and policy from individual health behaviours to combinations of behaviours, as well as from individuals to the domestic units and communities of which they are part.
Ethical statement
The paper is based on secondary analysis of data that was subject to ethical review at the point of collection. The dataset was accessed via assigned End User Licence.
Acknowledgements
The study was supported by the funding from the Public Health Research Consortium (PHRC) http://phrc.lshtm.ac.uk/. The PHRC is funded by the Department of Health (DH) Policy Research Programme. Views expressed in the paper are those of the authors and not necessarily those of the DH. We thank Kareena McAloney, Christos Byron and Julia Hall for their contribution to the study.
Footnotes
Examples include Australia (e.g. physical activity: http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines#apaadult; diet http://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating; alcohol intake http://www.alcohol.gov.au/internet/alcohol/publishing.nsf/Content/guide-adult), USA (physical activity http://health.gov/paguidelines/pdf/paguide.pdf; diet http://health.gov/dietaryguidelines/2015/guidelines/; alcohol intake http://health.gov/dietaryguidelines/2015/guidelines/appendix-9/ and smoking http://smokefree.gov/); Department of Health, 2003, Department of Health, 2005, Department of Health, 2011, Department of Health, 2013a, Department of Health, 2013b.
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2016.10.011.
Appendix A. Supplementary material
Supplementary material
References
- Bartley M., Kelly Y., Schoon I., Hope S. Parent health. In: Dex S., Joshi H., editors. Millennium Cohort Study first survey: A user’s guide to initial findings. Centre for Longitudinal Studies, Institute of Education, University of London; London: 2004. [Google Scholar]
- Berrigan D., Dodd K., Troiano R.P., Krebs-Smith S.M., Barbash R.B. Patterns of health behavior in U.S. adults. Preventive Medicine. 2003;36 doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- Bloomfield K., Grittner U., Kramer S., Gmel G. Social inequalities in alcohol consumption and alcohol-related problems in the study countries of the EU concerted action ‘Gender, Culture and Alcohol Problems: A Multi-national Study’. Alcohol and Alcoholism. 2006;41(1):i26–i36. doi: 10.1093/alcalc/agl073. [DOI] [PubMed] [Google Scholar]
- Brown R., Ogden J. Children's eating attitudes and behaviour: A study of the modelling and control theories of parental influence. Health Education Research. 2004;19(3):261–271. doi: 10.1093/her/cyg040. [DOI] [PubMed] [Google Scholar]
- Breslau N., Fenn N., Peterson E.L. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug and alcohol dependence. 1993;33(2):129–137. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- Bryant J., Bonevski B., Paul C.L., Lecathelinais C.L. A cross-sectional survey of health risk behaviour clusters among a sample of socially disadvantaged Australian welfare recipients. Australian and New Zealand Journal of Public Health. 2013;37(2):118–123. doi: 10.1111/1753-6405.12028. [DOI] [PubMed] [Google Scholar]
- Buck N., McFall S. Understanding society: Design overview. Longitudinal and Life Course Studies. 2011;3(1):5–17. [Google Scholar]
- Celis-Morales C.A., Perez-Bravo F., Ibañez L., Salas C., Bailey M.E.S., Gill J.M.R. Objective vs. self-reported physical activity and sedentary time: Effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7(5):e36345. doi: 10.1371/journal.pone.0036345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, S. & Muthén, B. (2009). Relating latent class analysis results to variables not included in the analysis. 〈https://www.statmodel.com/download/relatinglca.pdf〉.
- Cleveland M.J., Collins L.M., Lanza S.T., Greenberg M.T., Feinberg M.E. Does individual risk moderate the effect of contextual-level protective factors? A latent class analysis of substance use. Journal of Prevention Intervention in the Community. 2010;38(3):213–228. doi: 10.1080/10852352.2010.486299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conry M.C., Morgan K., Curry P., McGee H., Harrington J., Ward M., Shelley E. The clustering of health behaviours in Ireland and their relationship with mental health, self-rated health and quality of life. BMC Public Health. 2011;2011(11):692. doi: 10.1186/1471-2458-11-692. 〈http://www.biomedcentral.com/1471-2458/11/692〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries H., van ‘t Riet J., Spigt M., Metsemakers J., van den Akker M., Vermunt J.K., Kremers S. Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Preventive medicine. 2008;46(3):203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Department of Health (2003). 5 A DAY. Available at: 〈http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publichealth/Healthimprovement/FiveADay/index.htm〉.
- Department of Health (2005). Binge drinking and public health. Available at: 〈http://www.parliament.uk/documents/post/postpn244.pdf〉.
- Department of Health (2011). Physical activity guidelines for adults (16-64 years) Fact sheet 4. Available at: 〈https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213740/dh_128145.pdf〉.
- Department of Health (2013a). Reducing smoking. [Online]. Available at: 〈https://www.gov.uk/government/policies/reducing-smoking〉.
- Department of Health (2013b). Reducing harmful drinking. [Online]. Available at: 〈https://www.gov.uk/government/policies/reducing-harmful-drinking〉.
- Department of Health (2016). UK Chief Medical Officers' alcohol guidelines review summary of the proposed new guidelines. 〈https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/489795/summary.pdf〉.
- Ebrahim S., Montaner D., Lawlor D.A. Clustering of risk factors and social class in childhood and adulthood in British women's heart and health study: Cross sectional analysis. BMJ. 2004;328(7444):861. doi: 10.1136/bmj.38034.702836.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwardson C.L., Gorely T. Parental influences on different types and intensities of physical activity in youth: A systematic review. Psychology of Sport and Exercise. 2010;11(6):522–535. [Google Scholar]
- Evans-Polce R., Lanza S., Maggs J. Heterogeneity of alcohol, tobacco, and other substance use behaviors in U.S. college students: A latent class analysis. Addictive Behaviors. 2016;53:80–85. doi: 10.1016/j.addbeh.2015.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filippidis F.T., Agaku I.T., Vardavas C.I. Geographic variation and socio-demographic determinants of the co-occurrence of risky health behaviours in 27 European Union member states. Journal of Public Health. 2015 doi: 10.1093/pubmed/fdv061. [DOI] [PubMed] [Google Scholar]
- Gilman S.E., Rende R., Boergers J., Abrams D.B., Buka S.L., Clark M.A., Niaura R.S. Parental smoking and adolescent smoking initiation: An intergenerational perspective on tobacco control. Pediatrics. 2009;123(2):e274–e281. doi: 10.1542/peds.2008-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham H. Health inequalities, social determinants and public health policy. Policy Politics. 2009;37(4):463–479. [Google Scholar]
- Hofstetter H., Dusseldorp E., van Empelen P., Paulussen T.W.G.M. A primer on the use of cluster analysis or factor analysis to assess co-occurrence of risk behaviors. Preventive medicine. 2014;67:141–146. doi: 10.1016/j.ypmed.2014.07.007. [DOI] [PubMed] [Google Scholar]
- ISER, & NatCen Social Research (2012). Understanding society: Findings 2012. Retrieved from 〈https://www.understandingsociety.ac.uk/research/publications/findings/2012〉.
- Jefferis B.J.M.H., Power C., Graham H., Manor O. Effects of childhood socioeconomic circumstances on persistent smoking. American Journal of Public Health. 2004;94(2):279–285. doi: 10.2105/ajph.94.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khaw K.-T., Wareham N., Bingham S., Welch A., Luben R., Day N. Combined Impact of health behaviours and mortality in men and women: The EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, K., Meader, N., Wright, K., Graham, H., Petticrew, M., Power, C., Sowden, A. (2015). Multiple risk behaviours and interventions to reduce multiple risk behaviours – what do we know? Retrieved from 〈http://phrc.lshtm.ac.uk/papers/PHRC_002_Final_Report.pdf〉
- Knies G., editor. Understanding Society-The UK Household Longitudinal Study: Waves 1–4, User Manual. University of Essex; Colchester, UK: 2014. [Google Scholar]
- Kritsotakis G., Psarrou M., Vassilaki M., Androulaki Z., Philalithis A.E. Gender differences in the prevalence and clustering of multiple health risk behaviours in young adults. Journal of Advanced Nursing. 2016 doi: 10.1111/jan.12981. [DOI] [PubMed] [Google Scholar]
- Kvaavik E., Batty G.D., Ursin G., Huxley R., Gale C.R. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom health and lifestyle survey. Archives of Internal Medicine. 2010;170(8):711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- Laaksonen M., Prättälä R., Karisto A. Patterns of unhealthy behaviour in Finland. European Journal Public Health. 2001;11 doi: 10.1093/eurpub/11.3.294. [DOI] [PubMed] [Google Scholar]
- Lando H.A., Thai D.T., Murray D.M., Robinson L.A., Jeffery R.W., Sherwood N.E., Hennrikus D.J. Age of initiation, smoking patterns, and risk in a population of working adults. Preventive medicine. 1999;29(6):590–598. doi: 10.1006/pmed.1999.0590. [DOI] [PubMed] [Google Scholar]
- Lawder R., Harding O., Stockton D., Fischbacher C., Brewster D.H., Chalmers J., Conway D.I. Is the Scottish population living dangerously? Prevalence of multiple risk factors: The Scottish Health Survey 2003. BMC Public Health. 2010;10:1–13. doi: 10.1186/1471-2458-10-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M., Allen J., Bell R., Bloomer E., Goldblatt P. WHO European review of social determinants of health and the health divide. Lancet. 2012;380(9846):1011–1029. doi: 10.1016/S0140-6736(12)61228-8. [DOI] [PubMed] [Google Scholar]
- Martin-Diener E., Meyer J., Braun J., Tarnutzer S., Faeh D., Rohrmann S., Martin B.W. The combined effect on survival of four main behavioural risk factors for non-communicable diseases. Preventive Medicine. 2014;65:148–152. doi: 10.1016/j.ypmed.2014.05.023. [DOI] [PubMed] [Google Scholar]
- Mawditt C., Sacker A., Britton A., Kelly Y., Cable N. The clustering of health-related behaviours in a British population sample: Testing for cohort differences. Preventive Medicine. 2016;88:95–107. doi: 10.1016/j.ypmed.2016.03.003. [DOI] [PubMed] [Google Scholar]
- McAloney K., Graham H., Law C., Platt L., Wardle H., Hall J. Fruit and vegetable consumption and sports participation among UK Youth. International Journal of Public Health. 2014;59(1):117–121. doi: 10.1007/s00038-013-0523-9. [DOI] [PubMed] [Google Scholar]
- Morris L.J., D’Este C., Sargent-Cox K., Anstey K.J. Concurrent lifestyle risk factors: Clusters and determinants in an Australian sample. Preventive medicine. 2016;84:1–5. doi: 10.1016/j.ypmed.2015.12.009. [DOI] [PubMed] [Google Scholar]
- Muthén B.O. Latent variable mixture modeling. In: Marcoulides G.A., Schumacker R.E., editors. New developments and techniques in structural equation modeling. Lawrence Erlbaum Assocıates; London: 2001. pp. 1–33. [Google Scholar]
- Noble N., Paul C., Turon H., Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Preventive Medicine. 2015;81:16–41. doi: 10.1016/j.ypmed.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Noble N.E., Paul C.L., Turner N., Blunden S.V., Oldmeadow C., Turon H.E. A cross-sectional survey and latent class analysis of the prevalence and clustering of health risk factors among people attending an Aboriginal Community Controlled Health Service. BMC Public Health. 2015;15(1):1–9. doi: 10.1186/s12889-015-2015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. [Google Scholar]
- Office for National Statistics (ONS) (2014). Households and Household Composition in England and Wales, 2001-11. 〈http://www.ons.gov.uk/ons/dcp171776_361923.pdf〉 Accessed 28.10.14.
- Office for National Statistics (ONS) (2015). Statistical bulletin: Families and Households: 2015. 〈http://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/families/bulletins/familiesandhouseholds/2015-11-05#families〉.
- Pearson N., Biddle S.J., Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutrition. 2009;12(02):267–283. doi: 10.1017/S1368980008002589. [DOI] [PubMed] [Google Scholar]
- Poland B., Krupa G., McCall D. Settings for health promotion: An analytic framework to guide intervention design and implementation. Health Promotion Practice. 2009;10(4):505–516. doi: 10.1177/1524839909341025. [DOI] [PubMed] [Google Scholar]
- Poortinga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Preventive Med. 2007;44:124–128. doi: 10.1016/j.ypmed.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Prochaska J.J., Spring B., Nigg C.R. Multiple health behavior change research: An introduction and overview. Preventive medicine. 2008;46(3):181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson S.M., Crozier S.R., Borland S.E., Hammond J., Barker D.J.P., Inskip H.M. Impact of educational attainment on the quality of young women's diets. European Journal of Clinical Nutrition. 2004;58(8):1174–1184. doi: 10.1038/sj.ejcn.1601946. [DOI] [PubMed] [Google Scholar]
- Robinson C. Healthy foundation segmentation. In: Mindell C., editor. Health survey for England 2011. Health and Social Care Information Centre (HSCIC); London: 2012. [Google Scholar]
- Schooling M., Kuh D. A life course perspective on women's health behaviours (Ch. 13) In: Kuh D., Hardy R., editors. A life course approach to women's health. Oxford University Press; Oxford: 2002. [Google Scholar]
- Schoon I., Parsons S. Lifestyle and health-related behaviour. In: Ferri E., Bynner J., Wadsworth M., editors. Changing Britain, changing lives: Three generations at the turn of the century. Institute of Education; London: 2003. [Google Scholar]
- Schuit A.J., van Loon A.J.M., Tijhuis M., Ocke M.C. Clustering of lifestyle risk factors in a general adult population. Preventive Medicine. 2002;35 doi: 10.1006/pmed.2002.1064. [DOI] [PubMed] [Google Scholar]
- Smith K.E., Collin J. Scotland and the public health politics of independence. British Medical Journal. 2013;347 doi: 10.1136/bmj.f7595. [DOI] [PubMed] [Google Scholar]
- Stringhini S., Sabia S., Shipley M. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tipping S., Hope S., Pickering K., Erens B., Roth M.A., Mindell J.S. The effect of mode and context on survey results: Analysis of data from the Health Survey for England 2006 and the Boost Survey for London. BMC Medical Research methodology. 2010;10(1):1–8. doi: 10.1186/1471-2288-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Vorst H., Engels R.C.M.E., Meeus W., Deković M., Van Leeuwe J. The role of alcohol-specific socialization in adolescents' drinking behaviour. Addiction. 2005;100(10):1464–1476. doi: 10.1111/j.1360-0443.2005.01193.x. [DOI] [PubMed] [Google Scholar]
- Vermunt, J., & Magidson, J. (2008). Latent GOLD 4.5. Retrieved from 〈http://www.statisticalinnovations.com/〉.
- Weich S., McBride O., Hussey D., Exeter D., Brugha T., McManus S. Latent class analysis of co-morbidity in the Adult Psychiatric Morbidity Survey in England 2007: Implications for DSM-5 and ICD-11. Psychological Medicine. 2011;41(10):2201–2212. doi: 10.1017/S0033291711000249. [DOI] [PubMed] [Google Scholar]
- WHO (2008). Global Burden of Disease: 2004 Update. Geneva.
- WHO (2011). Global status report on noncommunicable diseases 2010. Switzerland.
- WHO (2013). Healthy Settings. From 〈http://www.who.int/healthy_settings/en/〉.
- WHO (2014). Global status report on noncommunicable diseases 2014. Retrieved from 〈http://www.who.int/nmh/publications/ncd-status-report-2014/en/〉.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material