Abstract
Objective
To determine whether less invasive endometrial (EM) aspiration biopsy is adequately accurate for evaluating treatment outcomes compared to the dilatation and curettage (D&C) biopsy in early-stage endometrial cancer (EC) patients treated with high dose oral progestin and levonorgestrel intrauterine system (LNG-IUS).
Methods
We conducted a prospective observational study with patients younger than 40 years who were diagnosed with clinical stage IA, The International Federation of Gynecology and Obstetrics grade 1 or 2 endometrioid adenocarcinoma and sought to maintain their fertility. The patients were treated with medroxyprogesterone acetate 500 mg/day and LNG-IUS. Treatment responses were evaluated every 3 months. EM aspiration biopsy was conducted after LNG-IUS removal followed D&C. The tissue samples were histologically compared. The diagnostic concordance rate of the two tests was examined with κ statistics.
Results
Twenty-eight pairs of EM samples were obtained from five patients. The diagnostic concordance rate of D&C and EM aspiration biopsy was 39.3% (κ value=0.26). Of the seven samples diagnosed as normal with D&C, three (42.8%) were diagnosed as normal by using EM aspiration biopsy. Of the eight samples diagnosed with endometrioid adenocarcinoma by using D&C, three (37.5%) were diagnosed with endometrioid adenocarcinoma by using EM aspiration biopsy. Of the 13 complex EM hyperplasia samples diagnosed with the D&C, five (38.5%) were diagnosed with EM hyperplasia by using EM aspiration biopsy. Of the samples obtained through EM aspiration, 46.4% were insufficient for histological evaluation.
Conclusion
To evaluate the treatment responses of patients with early-stage EC treated with high dose oral progestin and LNG-IUS, D&C should be conducted after LNG-IUS removal.
Keywords: Biopsy, Dilatation and Curettage, Endometrial Neoplasms, Levonorgestrel Intrauterine Devices, Progesterone
INTRODUCTION
Endometrial cancer (EC) is the most common gynecological tumor in the United States and the incidence rate has been gradually increasing, accounting for 6% of all female cancer cases in 2014 [1]. EC is more common in postmenopausal women than in premenopausal women. It occurs in 14% of all women and in approximately 4% of women younger than 40 years [2,3]. The importance of fertility sparing treatment is being emphasized in young EC patients. Typical drugs that can be used include systemic progesterone and levonorgestrel intrauterine system (LNG-IUS) [4,5,6,7,8,9,10,11,12,13,14].
As EC shows symptoms including vaginal bleeding in its early stage, it is often detected early and thus has a good prognosis, with a 5-year survival rate of 85% to 91% for stage I patients [15]. Tissue biopsy methods for diagnosing endometrial (EM) lesions include EM aspiration, dilatation and curettage (D&C), and hysteroscopic biopsy. EM aspiration biopsy is an easy, safe, and cost-effective method, and has been reported to be comparable to D&C in diagnosing EM hyperplasia and EC. Accordingly, this technique is widely used on an outpatient basis [16,17]. However, the gold standard follow-up evaluation tool for hormonally treated patients with EM atrophy due to progesterone still remains controversial. Repetitive D&C for evaluating treatment outcomes in early EC may damage the endometrium of patients who seek to preserve their fertility. Therefore, studies should investigate other diagnostic tools that can substitute for D&C, with less invasiveness and less risk of injuring the endometrium. Several studies investigated the accuracy of EM aspiration biopsy conducted without LNG-IUS removal after treating EC with LNG-IUS [9,10,11,12,13,18,19,20]. However, no study has evaluated the accuracy of EM aspiration biopsy after LNG-IUS removal in EC patients treated with high-dose progesterone and LNG-IUS therapy, and whether it can substitute for D&C. This study aimed to compare the accuracy of EM aspiration biopsy conducted after LNG-IUS removal and D&C biopsy in order to evaluate the treatment responses of patients with early EC conservatively treated with high-dose oral progestin and LNG-IUS, and its usefulness.
MATERIALS AND METHODS
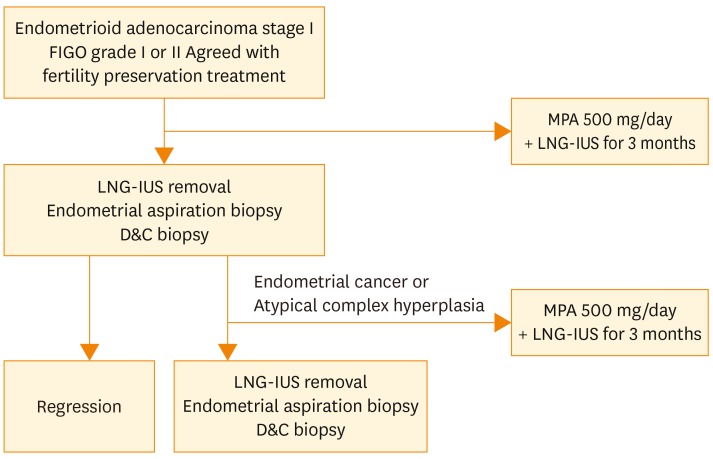
This was a prospective observational study. Patients who underwent conservative treatment upon diagnosis of EC at CHA Gangnam Medical Center, CHA University, Seoul, Korea, between January 2010 and February 2014 were enrolled. The inclusion criteria were as follows: (1) age younger than 40 years; (2) endometrioid adenocarcinoma; (3) histologically confirmed The International Federation of Gynecology and Obstetrics (FIGO) grade 1 or 2; and (4) clinical stage 1A patients without extrauterine spreading of EC or myometrial invasion on magnetic resonance imaging, pelvic examination, or ultrasonography. All initial EC diagnoses were primarily confirmed by using D&C biopsy. All of the patients wanted to preserve their fertility and were treated with high dose oral progestin (medroxyprogesterone acetate [MPA] 500 mg/day) and LNG-IUS. Follow-up evaluations were conducted every 3 months (Fig. 1). For the follow-up tests, in order to collect EM tissue samples, (1) EM aspiration biopsy was conducted by using a pipelle after LNG-IUS removal and (2) D&C biopsy was conducted subsequently. Afterward, the samples collected through the two methods were compared and we evaluated the concordance of the results of EM aspiration and D&C biopsy. Normal endometrium was defined as an EM gland tissue sample without any sign of hyperplasia or cancer that contains sufficient specimen for analysis. All histological evaluations were conducted independently by a gynecological pathologist.
Fig. 1.
Methods of follow-up evaluation on patients. D&C, dilatation and curettage; FIGO, The International Federation of Gynecology and Obstetrics; LNG-IUS, levonorgestrel intrauterine system; MPA, medroxyprogesterone acetate.
All patients were advised with the nature of the treatment and all provided informed consent. All the patients enrolled in the study agreed to participate in the study by providing written consents. The collection and use of samples for this study were approved by the Institutional Review Board of CHA Gangnam Medical Center, CHA University. κ Statistics were used to assess the agreement of the two methods. Interpretation of κ values <0 as indicating no agreement and 0 to 0.20 as slight, 0.21 to 0.40 as fair, 0.41 to 0.60 as moderate, 0.61 to 0.80 as substantial, and 0.81 to 1 as almost good agreement. Values of p<0.05 were considered statistically significant.
RESULTS
From five patients, 28 pairs of EM tissue samples were obtained, with median of 6 tissue biopsies (range, 1 to 8 tissue biopsies) conducted for each patient. The five patients had a median age of 31 years (range, 29 to 35 years) and 0 parity. Of the five patients, three were diagnosed as having FIGO grade 1 disease and the remaining two were diagnosed as having FIGO grade 2 disease. The median body mass index (BMI) of the patients was 22.8 kg/m2 (range, 18.5 to 32.7 kg/m2). One of them had a high BMI, exceeding 30 kg/m2 (32.7 kg/m2) and another was overweight (26.2 kg/m2). The BMI values of the other three patients were within the normal range (range, 18.5 to 22.8 kg/m2). None of the patients complained of adverse events during treatment.
Table 1 compares D&C and EM aspiration biopsy. Of the 28 samples examined by using D&C biopsy, seven samples (25%) had normal results, eight samples (28.6%) were diagnosed with endometrioid adenocarcinoma, and the other 13 samples (46.4%) were diagnosed with complex EM hyperplasia. Of the seven samples diagnosed as normal by using D&C biopsy, three samples also had normal results in the EM aspiration biopsy and four samples contained insufficient materials (diagnostic concordance rate, 42.8%). Of the eight samples diagnosed with endometrioid adenocarcinoma through D&C biopsy, two samples were diagnosed as normal by using EM aspiration biopsy, three samples were diagnosed with endometrioid adenocarcinoma, and three samples contained insufficient materials (diagnostic concordance rate, 37.5%). Of the 13 samples diagnosed as complex EM hyperplasia through D&C, two samples had normal results, five samples were diagnosed with complex EM hyperplasia, and six samples contained insufficient materials when examined by using EM aspiration biopsy (diagnostic concordance rate, 38.5%).
Table 1. Comparison of pathologic results from D&C and endometrial aspiration biopsy.
| D&C biopsy | No. (%) | Endometrial aspiration biopsy | No. | Concordance to D&C (%) |
|---|---|---|---|---|
| Normal | 7 (25.0) | Normal | 3 | 42.8 |
| Insufficient material | 4 | |||
| Endometrioid adenocarcinoma | 8 (28.6) | Endometrioid adenocarcinoma | 3 | 37.5 |
| Normal | 2 | |||
| Insufficient material | 3 | |||
| Complex endometrial hyperplasia | 13 (46.4) | Complex endometrial hyperplasia | 5 | 38.5 |
| Normal | 2 | |||
| Insufficient material | 6 | |||
| Total | 28 (100) | Total aspiration biopsies in concordance | 11 | 39.3 |
κ value, 0.26 (fair); diagnostic concordance, 39.3% (11 out of 28 pairs); p<0.001.
D&C, dilatation and curettage.
Among the 28 pairs of samples, the diagnoses made through D&C and EM aspiration biopsy were concordant in 11 pairs, showing a diagnostic concordance rate of 39.3% and a κ value of 0.26 (p<0.001). This indicates that the results of the two test methods were not in agreement. Of the 11 samples with concordant diagnoses, three samples had normal results, another three samples were diagnosed with EC, and the remaining five samples were diagnosed with complex hyperplasia. The diagnostic concordance rate was 37.5% for EC. Moreover, a high ratio of insufficient materials was observed when EM aspiration biopsy was conducted. Of the 28 samples obtained through EM aspiration biopsy, 13 samples (46.4%) were insufficient. Of the 13 samples, four samples were diagnosed as normal by using D&C, three samples were diagnosed with EC, and six samples were diagnosed with complex hyperplasia. None of the samples obtained through D&C was insufficient for evaluation.
DISCUSSION
EC in young patients, which is related to estrogen or hormonal disorders, including obesity, primipara, polycystic ovarian syndrome, and infertility [4,7,21], is usually detected in its early stage with good cellular differentiation and shows a good prognosis. It rarely invades the extrauterine organs and myometrium [4,21,22,23]. The standard treatment of EC includes total hysterectomy, bilateral salpingo-oophorectomy, peritoneal cytology, and sometimes, lymph node dissection when required [24,25]. However, conservative hormonal therapy can be performed before surgical treatment in young patients diagnosed with clinical stage IA (no evidence of extrauterine spread of disease and myometrial invasion), FIGO grade 1, endometrioid type EM adenocarcinoma who desire to preserve their fertilities [26,27].
Progestin is the most commonly used drug to conservatively treat EC and is available in forms of oral MPA and megestrol acetate. For patients who are contraindicated to receive oral progestin or those with complaints of systemic side effects, LNG-IUS, which works locally in the endometrium, can be used. Recent studies have reported that combination treatment shows better results than single LNG-IUS treatment [8,9,10,11,12,13,18,19]. In particular, Kim et al. [28] conducted a prospective observational study where MPA 500 mg/day and LNG-IUS were used in 16 patients with early-stage EC and reported that complete remission without any particular side effect was observed in 14 of 16 patients. As such, hormonal therapy is advantageous, as it is safe, effective, and can preserve the uterus. However, as it has risks of cancer progression, recurrence, and metastasis, more emphasis is placed on the diagnostic accuracy of follow-up evaluation.
Kim et al. [20] used the combination of high-dose oral progestin and LNG-IUS in patients with early EC and conducted EM aspiration biopsy while the LNG-IUS devices had not been removed yet. For the first time, they compared the biopsy accuracy of these EM aspiration biopsy in situ LNG-IUS and those obtained using D&C biopsy after LNG-IUS removal [20]. The diagnostic concordance rate of the two methods was 32.1%, and the methods showed a low κ value of 0.27. The authors suggested that the low accuracy of EM aspiration biopsy was probably due to (1) LNG-IUS acting as a barrier blocking the appropriate EM aspiration and (2) EM atrophy caused by the combination treatment with high-dose oral progestin and LNG-IUS. In the present study, to overcome the caveat that LNG-IUS may act as a barrier for EM aspiration biopsy, EM aspiration was done after LNG-IUS removal. Our study results also showed a low concordance rate of 39.3% between EM aspiration and D&C biopsy conducted for follow-up evaluation of hormonal therapy and that 46.4% of the samples obtained by using the EM sampling method were insufficient. Van Doorn et al. [29] conducted a prospective cohort study in 913 postmenopausal women with vaginal bleeding. Of these patients, 403 underwent office EM sampling. Sixty-six samples (16.4%) were insufficient. The authors also reported that three patients were diagnosed with EC and one patient was diagnosed with EM atypical hyperplasia when evaluated by using hysteroscopy and D&C biopsy [29]. Furthermore, Clark et al. [30] reported that 20% of samples collected from postmenopausal women through EM aspiration biopsy contained insufficient materials. Other factors that may affect insufficient biopsy results include poor patient compliance, lack of skills in conducting the biopsy, varying pathological interpretation, and EM atrophy. Moreover, adequate sampling is also influenced by EM thickness and hormonal therapy [31,32].
Progestin affects secretory differentiation of EM glands, inhibits cellular differentiation of EM and estrogen receptor functions, promotes apoptosis, and has antiangiogenic effects; thereby, inhibiting the proliferation of endometrium [14]. Combined treatment with high-dose oral progestin and LNG-IUS induces EM atrophy by inhibiting EM proliferation just as in postmenopausal women. In our study, although LNG-IUS was removed, the amounts of the samples were insufficient and the accuracy was low owing to EM atrophy when EM aspiration was conducted. Although EM aspiration biopsy is a convenient method with a low false-positive rate, it is not capable of ruling out EC when used in patients undergoing hormonal therapy [33].
Our study is significant because it is the first study to discover that the low diagnostic accuracy of EM aspiration biopsy when used as a follow-up evaluation method for EC patients who had undergone combination treatment with high-dose oral progestin and LNG-IUS, when compared with D&C, can be attributed to EM atrophy. The limitations of our study include the fact that it was not a randomized trial and that it investigated a limited number of patients. Therefore, more prospective studies need to be conducted. Moreover, further research is necessary to compare the diagnostic accuracy of EM aspiration and D&C biopsy conducted in patients with EM hyperplasia treated with low-dose progestin.
In conclusion, because the accuracy of EM aspiration biopsy was lower than that of D&C when used as a follow-up method for the patients with early-stage EC treated with high-dose oral progestin and LNG-IUS, D&C should be the method of choice.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Creasman WT, Odicino F, Maisonneuve P, Beller U, Benedet JL, Heintz AP, et al. Carcinoma of the corpus uteri. J Epidemiol Biostat. 2001;6:47–86. [PubMed] [Google Scholar]
- 3.Lee NK, Cheung MK, Shin JY, Husain A, Teng NN, Berek JS, et al. Prognostic factors for uterine cancer in reproductive-aged women. Obstet Gynecol. 2007;109:655–662. doi: 10.1097/01.AOG.0000255980.88205.15. [DOI] [PubMed] [Google Scholar]
- 4.Kim YB, Holschneider CH, Ghosh K, Nieberg RK, Montz FJ. Progestin alone as primary treatment of endometrial carcinoma in premenopausal women. Report of seven cases and review of the literature. Cancer. 1997;79:320–327. doi: 10.1002/(sici)1097-0142(19970115)79:2<320::aid-cncr15>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Kaku T, Yoshikawa H, Tsuda H, Sakamoto A, Fukunaga M, Kuwabara Y, et al. Conservative therapy for adenocarcinoma and atypical endometrial hyperplasia of the endometrium in young women: central pathologic review and treatment outcome. Cancer Lett. 2001;167:39–48. doi: 10.1016/s0304-3835(01)00462-1. [DOI] [PubMed] [Google Scholar]
- 6.Gotlieb WH, Beiner ME, Shalmon B, Korach Y, Segal Y, Zmira N, et al. Outcome of fertility-sparing treatment with progestins in young patients with endometrial cancer. Obstet Gynecol. 2003;102:718–725. doi: 10.1016/s0029-7844(03)00667-7. [DOI] [PubMed] [Google Scholar]
- 7.Ushijima K, Yahata H, Yoshikawa H, Konishi I, Yasugi T, Saito T, et al. Multicenter phase II study of fertility-sparing treatment with medroxyprogesterone acetate for endometrial carcinoma and atypical hyperplasia in young women. J Clin Oncol. 2007;25:2798–2803. doi: 10.1200/JCO.2006.08.8344. [DOI] [PubMed] [Google Scholar]
- 8.Montz FJ, Bristow RE, Bovicelli A, Tomacruz R, Kurman RJ. Intrauterine progesterone treatment of early endometrial cancer. Am J Obstet Gynecol. 2002;186:651–657. doi: 10.1067/mob.2002.122130. [DOI] [PubMed] [Google Scholar]
- 9.Giannopoulos T, Butler-Manuel S, Tailor A. Levonorgestrel-releasing intrauterine system (LNG-IUS) as a therapy for endometrial carcinoma. Gynecol Oncol. 2004;95:762–764. doi: 10.1016/j.ygyno.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Dhar KK, NeedhiRajan T, Koslowski M, Woolas RP. Is levonorgestrel intrauterine system effective for treatment of early endometrial cancer? Report of four cases and review of the literature. Gynecol Oncol. 2005;97:924–927. doi: 10.1016/j.ygyno.2004.10.031. [DOI] [PubMed] [Google Scholar]
- 11.Fambrini M, Bargelli G, Peruzzi E, Buccoliero AM, Pieralli A, Andersson KL, et al. Levonorgestrel-releasing intrauterine system alone as primary treatment in young women with early endometrial cancer: case report. J Minim Invasive Gynecol. 2009;16:630–633. doi: 10.1016/j.jmig.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Cade TJ, Quinn MA, Rome RM, Neesham D. Progestogen treatment options for early endometrial cancer. BJOG. 2010;117:879–884. doi: 10.1111/j.1471-0528.2010.02552.x. [DOI] [PubMed] [Google Scholar]
- 13.Minig L, Franchi D, Boveri S, Casadio C, Bocciolone L, Sideri M. Progestin intrauterine device and GnRH analogue for uterus-sparing treatment of endometrial precancers and well-differentiated early endometrial carcinoma in young women. Ann Oncol. 2011;22:643–649. doi: 10.1093/annonc/mdq463. [DOI] [PubMed] [Google Scholar]
- 14.Kim ML, Seong SJ. Clinical applications of levonorgestrel-releasing intrauterine system to gynecologic diseases. Obstet Gynecol Sci. 2013;56:67–75. doi: 10.5468/OGS.2013.56.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trimble EL, Harlan LC, Clegg LX, Stevens JL. Pre-operative imaging, surgery and adjuvant therapy for women diagnosed with cancer of the corpus uteri in community practice in the United States. Gynecol Oncol. 2005;96:741–748. doi: 10.1016/j.ygyno.2004.11.041. [DOI] [PubMed] [Google Scholar]
- 16.Dijkhuizen FP, Mol BW, Brölmann HA, Heintz AP. The accuracy of endometrial sampling in the diagnosis of patients with endometrial carcinoma and hyperplasia: a meta-analysis. Cancer. 2000;89:1765–1772. [PubMed] [Google Scholar]
- 17.Stovall TG, Photopulos GJ, Poston WM, Ling FW, Sandles LG. Pipelle endometrial sampling in patients with known endometrial carcinoma. Obstet Gynecol. 1991;77:954–956. [PubMed] [Google Scholar]
- 18.Pashov AI, Tskhay VB, Ionouchene SV. The combined GnRH-agonist and intrauterine levonorgestrel-releasing system treatment of complicated atypical hyperplasia and endometrial cancer: a pilot study. Gynecol Endocrinol. 2012;28:559–561. doi: 10.3109/09513590.2011.649813. [DOI] [PubMed] [Google Scholar]
- 19.Brown AJ, Westin SN, Broaddus RR, Schmeler K. Progestin intrauterine device in an adolescent with grade 2 endometrial cancer. Obstet Gynecol. 2012;119((2 Pt 2)):423–426. doi: 10.1097/AOG.0b013e318234d97c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim MK, Seong SJ, Song T, Kim ML, Yoon BS, Jun HS, et al. Comparison of dilatation & curettage and endometrial aspiration biopsy accuracy in patients treated with high-dose oral progestin plus levonorgestrel intrauterine system for early-stage endometrial cancer. Gynecol Oncol. 2013;130:470–473. doi: 10.1016/j.ygyno.2013.06.035. [DOI] [PubMed] [Google Scholar]
- 21.Crissman JD, Azoury RS, Barnes AE, Schellhas HF. Endometrial carcinoma in women 40 years of age or younger. Obstet Gynecol. 1981;57:699–704. [PubMed] [Google Scholar]
- 22.Soliman PT, Oh JC, Schmeler KM, Sun CC, Slomovitz BM, Gershenson DM, et al. Risk factors for young premenopausal women with endometrial cancer. Obstet Gynecol. 2005;105:575–580. doi: 10.1097/01.AOG.0000154151.14516.f7. [DOI] [PubMed] [Google Scholar]
- 23.Duska LR, Garrett A, Rueda BR, Haas J, Chang Y, Fuller AF. Endometrial cancer in women 40 years old or younger. Gynecol Oncol. 2001;83:388–393. doi: 10.1006/gyno.2001.6434. [DOI] [PubMed] [Google Scholar]
- 24.Lee JY, Kim K, Lee TS, Kang S, Seong SJ, Kim JW, et al. Controversies in the management of endometrial cancer: a survey of the Korean Gynecologic Oncology Group. J Gynecol Oncol. 2015;26:277–283. doi: 10.3802/jgo.2015.26.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahdi H, Jernigan A, Nutter B, Michener C, Rose PG. Lymph node metastasis and pattern of recurrence in clinically early stage endometrial cancer with positive lymphovascular space invasion. J Gynecol Oncol. 2015;26:208–213. doi: 10.3802/jgo.2015.26.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kesterson JP, Fanning J. Fertility-sparing treatment of endometrial cancer: options, outcomes and pitfalls. J Gynecol Oncol. 2012;23:120–124. doi: 10.3802/jgo.2012.23.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sonoda Y. Surgical treatment for apparent early stage endometrial cancer. Obstet Gynecol Sci. 2014;57:1–10. doi: 10.5468/ogs.2014.57.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim MK, Seong SJ, Kim YS, Song T, Kim ML, Yoon BS, et al. Combined medroxyprogesterone acetate/levonorgestrel-intrauterine system treatment in young women with early-stage endometrial cancer. Am J Obstet Gynecol. 2013;209:358.e1–358.e4. doi: 10.1016/j.ajog.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 29.van Doorn HC, Opmeer BC, Burger CW, Duk MJ, Kooi GS, Mol BW, Dutch Study in Postmenopausal Bleeding (DUPOMEB) Inadequate office endometrial sample requires further evaluation in women with postmenopausal bleeding and abnormal ultrasound results. Int J Gynaecol Obstet. 2007;99:100–104. doi: 10.1016/j.ijgo.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 30.Clark TJ, Mann CH, Shah N, Khan KS, Song F, Gupta JK. Accuracy of outpatient endometrial biopsy in the diagnosis of endometrial cancer: a systematic quantitative review. BJOG. 2002;109:313–321. doi: 10.1111/j.1471-0528.2002.01088.x. [DOI] [PubMed] [Google Scholar]
- 31.Elsandabesee D, Greenwood P. The performance of Pipelle endometrial sampling in a dedicated postmenopausal bleeding clinic. J Obstet Gynaecol. 2005;25:32–34. doi: 10.1080/01443610400025390. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein SR, Nachtigall M, Snyder JR, Nachtigall L. Endometrial assessment by vaginal ultrasonography before endometrial sampling in patients with postmenopausal bleeding. Am J Obstet Gynecol. 1990;163((1 Pt 1)):119–123. doi: 10.1016/s0002-9378(11)90683-8. [DOI] [PubMed] [Google Scholar]
- 33.Park JY, Nam JH. Progestins in the fertility-sparing treatment and retreatment of patients with primary and recurrent endometrial cancer. Oncologist. 2015;20:270–278. doi: 10.1634/theoncologist.2013-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]