Abstract
Introduction
Individuals with chronic conditions often experience exacerbation of those conditions and have specialized medical needs after a disaster. Less is known about the level of disaster preparedness of this particular population and the extent to which being prepared might have an impact on the risk of disease exacerbation. The purpose of this study was to examine the association between self-reported asthma, cardiovascular disease, and diabetes and levels of household disaster preparedness.
Methods
Data were analyzed from 14 US states participating in the 2006–2010 Behavioral Risk Factor Surveillance System (BRFSS), a large state-based telephone survey. Chi-square statistics and adjusted prevalence ratios were calculated.
Results
After adjusting for sociodemographic characteristics, as compared to those without each condition, persons with cardiovascular disease (aPR =1.09; 95% CI, 1.01–1.17) and diabetes (aPR =1.13; 95% CI, 1.05–1.22) were slightly more likely to have an evacuation plan and individuals with diabetes (aPR =1.04; 95% CI, 1.02–1.05) and asthma (aPR =1.02; 95% CI, 1.01–1.04) were slightly more likely to have a 3-day supply of prescription medication. There were no statistically significant differences in the prevalence for all other preparedness measures (3-day supply of food and water, working radio and flashlight, willingness to leave during a mandatory evacuation) between those with and those without each chronic condition.
Conclusion
Despite the increased morbidity and mortality associated with chronic conditions, persons with diabetes, cardiovascular disease, and asthma were generally not more prepared for natural or man-made disasters than those without each chronic condition.
Keywords: asthma, cardiovascular disease, diabetes, household preparedness
Introduction
In the past decade, there were 178 recorded natural disasters (eg, earthquakes, drought, and epidemics) and 32 man-made disasters (eg, industrial accidents) in the United States.1 Individuals with chronic health conditions are a population of particular concern to consider in overall disaster planning efforts. Between 41% and 77% of evacuees from previous incidents have had at least one chronic condition, such as heart disease, hypertension, diabetes, or asthma;2–5 this population continues to grow and is estimated to include 157 million Americans by 2020.6 A substantial portion of all medical care delivered during the response and recovery phases of an incident is provided to individuals experiencing exacerbations of underlying diseases.7–9 One study found that chronic diseases and related conditions accounted for 24.3% of illness-related visits to emergency treatment facilities in New Orleans post-Hurricane Katrina, with diabetes mellitus, respiratory complaints, and cardiovascular disease (CVD) being among the most common pre-existing chronic conditions.8
Few studies have examined factors that may influence individual or household preparedness for disasters. Existing studies suggest associations between lower levels of disaster readiness and younger age, lower household income, and mental illness.10–11 One study found that individuals with one, two, or three or more chronic diseases were less likely to have multiple components of preparedness (ie, an evacuation plan; 3-day supply of water, food, and medication; and working radio and flashlight) than individuals without chronic conditions.12 Notably, this study did not explore differences by type of chronic condition. Another study used a summary score (sum of all preparedness components) to evaluate preparedness and found that individuals with asthma were no more likely to be prepared, and individuals with CVD and diabetes were more likely to be prepared, than individuals without these conditions.10 However, differences by specific preparedness components were not explored. Whether differences in preparedness indicators exist among individuals with specific chronic conditions is unknown. Thus, this study examined the association between specific self-reported household preparedness components and three chronic conditions (CVD, diabetes, and asthma).
Methods
Behavioral Risk Factor Surveillance System (BRFSS) data collected from 2006 through 2010 were used for this study. The BRFSS is a state-based surveillance system operated by state health departments in collaboration with the United States (US) Centers for Disease Control and Prevention (CDC). The objective of the BRFSS is to collect uniform, state-specific data on preventive health practices and risk behaviors linked to chronic diseases, injuries, and preventable infectious diseases in the adult population. Trained interviewers collect data from a standardized questionnaire on a monthly basis using an independent probability sample of households with landline telephones in the non-institutionalized US adult population. The BRFSS questionnaire consists of three parts: 1) core questions asked in all 50 states, the District of Columbia (DC), Puerto Rico, Guam, and the U.S. Virgin Islands; 2) supplemental modules, which are a series of questions on specific topics (eg, adult asthma history, intimate partner violence, mental health) that a state can choose to include in its survey; and 3) questions added by the states individually. All BRFSS questionnaires, data, and reports are available online.13
General Preparedness Module Questions
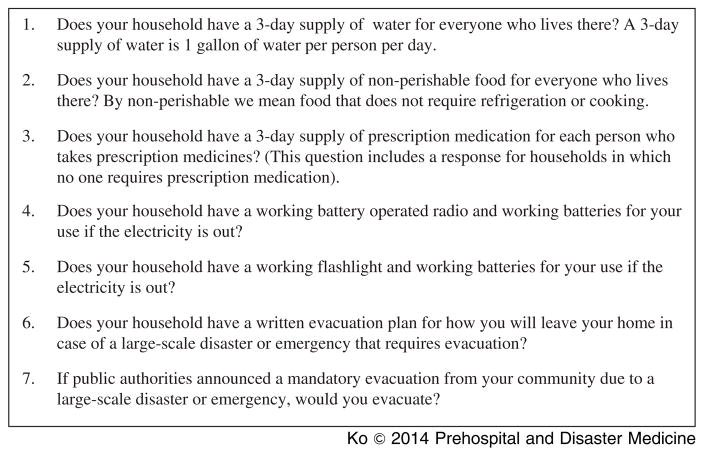
The General Preparedness module was included in the BRFSS in select states from 2006 through 2010. Preparedness data were available for Connecticut, Montana, Nevada, and Tennessee in 2006; Delaware, Louisiana, Maryland, Nebraska, and New Hampshire in 2007; Georgia, Montana, Nebraska, New York, and Pennsylvania in 2008; Mississippi in 2009; and Montana and North Carolina in 2010. Overall household disaster preparedness, as defined by the BRFSS questionnaire, included the following seven criteria: having a 3-day supply of food, water, and prescription medications; having a working battery-powered radio and a working battery-powered flashlight; having an evacuation plan; and expressing a willingness to evacuate from the community when instructed to do so by public health authorities (Figure 1).
Figure 1.
Selected BRFSS Disaster Preparedness Module questions
Chronic Disease Questions
Chronic disease questions were included in the core module from 2006 through 2010. The following three questions assessed CVD status: “Has a doctor, nurse, or other health professional EVER told you that you had any of the following? 1. ‘…heart attack, also called a myocardial infarction?’ 2. ‘…angina or coronary heart disease?’ and 3. ‘…a stroke?”‘ Individuals were considered to have CVD if they responded “Yes” to any of the above questions. Individuals who responded “No” to all three items were considered not to have CVD.
Diagnosed diabetes status was assessed using one question: “Have you ever been told by a doctor that you have diabetes?” Individuals who said “yes” were considered to have diabetes. Individuals who responded, “Yes, but only during pregnancy,” “No,” or “Pre-diabetes or borderline diabetes,” were considered not to have diagnosed diabetes.
Asthma was assessed using two yes/no questions: “Have you ever been told by a doctor, nurse, or other health professional that you had asthma?”, and “Do you still have asthma?” Individuals who responded “Yes” to both questions were considered to have asthma. People who were never diagnosed with asthma and persons who had been previously diagnosed but who no longer had asthma were considered not to have asthma.
Statistical Analysis
A univariate analysis was conducted to explore the characteristics of the entire sample, including sociodemographics, preparedness, and chronic disease (CVD, diabetes, asthma) status. A bivariate analysis was used to explore the relationships between each of the sociodemographic variables and chronic disease status; a second bivariate analysis was carried out to explore the relationship between chronic disease status and each household disaster preparedness item. Significance was assessed using a chi-square test. Finally, the association between chronic disease status and each household disaster preparedness item was adjusted for a set of covariates using logistic regression.
Covariates of interest included age in years (18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75+), gender, race/ethnicity (white non-Hispanics, black non-Hispanics, Hispanics, other non-Hispanics), education (less than 12 years, 12 years, greater than 12 years), marital status (currently married, previous married, and never married), and employment status (currently employed, unemployed, retired, unable to work, homemaker/student). Health care coverage (yes, no) at the time of survey, defined as having health insurance, prepaid plans such as Health Maintenance Organizations (HMOs), or government plans such as Medicare, was also examined. All analyses were weighted to reflect the complex survey design, resulting in weighted percentages, confidence intervals, and adjusted prevalence ratios. The unweighted and weighted sample size, response rate, and cooperation rate for each state in each year is reported in Table 1. Significance was assessed using an alpha level of .05. All analyses were conducted using SAS callable SUDAAN (Research Triangle, release 9.2, Research Triangle Park, North Carolina USA).
Table 1.
States Participating in the BRFSS General Preparedness Module 2006–2010 by Year, United States
| Year/State | Unweighted (n) | Weighted (n) | Response Ratea % | Cooperation Rateb % |
|---|---|---|---|---|
| 2006 | ||||
| * Connecticut | 4,842 | 2,697,438 | 44.3 | 74.0 |
| Montana | 6,059 | 727,026 | 54.8 | 72.5 |
| Nevada | 3,591 | 1,825,459 | 50.1 | 80.2 |
| Tennessee | 4,416 | 4,583,404 | 56.7 | 81.3 |
| 2007 | ||||
| Delaware | 3,991 | 663,748 | 43.2 | 70.4 |
| Louisiana | 6,684 | 3,249,264 | 41.0 | 60.1 |
| * Maryland | 4,403 | 4,265,213 | 31.4 | 57.8 |
| * Nebraska | 5,514 | 1,338,549 | 65.4 | 80.0 |
| New Hampshire | 5,990 | 1,027,463 | 37.7 | 64.0 |
| 2008 | ||||
| Georgia | 5,716 | 7,163,610 | 55.1 | 85.8 |
| Montana | 6,846 | 738,769 | 48.3 | 69.4 |
| * Nebraska | 5,373 | 13,333,476 | 65.5 | 80.2 |
| * New York | 3,989 | 1,484,027 | 40.0 | 63.4 |
| * Pennsylvania | 6,603 | 9,696,488 | 45.6 | 66.7 |
| 2009 | ||||
| Mississippi | 11,194 | 2,170,140 | 49.3 | 70.9 |
| 2010 | ||||
| Montana | 7,304 | 760,685 | 65.4 | 80.6 |
| North Carolina | 12,139 | 7,174,410 | 41.1 | 64.5 |
Split sample.
Percent of completed interviews of all eligible individuals.
Percentage of eligible individuals who were contacted and completed the survey.
For this study combined data collected from 104,654 individuals from 14 states who completed the General Prepared-ness module from 2006 through 2010 was used.
Results
Overall Population
The majority of individuals in this BRFSS sample were female (51.8%), white non-Hispanic (74.3%), 25–54 years of age (58.4%), had greater than 12 years of education (60.6%), were currently employed (61.1%), were currently married (60.6%), and had health care coverage at the time of survey (86.4%) (Table 2). More than three-fourths of individuals reported having ready, household access to the following: a 3-day supply of food (82.9%); a 3-day supply of prescription medication for each member of the household who required medication (89.7%); a working battery-powered radio (77.7%); and a working battery-powered flashlight (94.8%). The majority of respondents also reported a willingness to comply with mandatory evacuation orders (94.9%). Slightly more than half (53.6%) of individuals reported that their household had a 3-day supply of water and even fewer (21.1%) reported having an evacuation plan. Only 25.3% of individuals assessed themselves as being well prepared, 55.5% felt somewhat prepared, and 19.1% felt not prepared at all for a large-scale disaster or emergency.
Table 2.
Characteristics of Individuals in Study Sample, BRFSS, United States, 2006–2010 (N =104,654)
| Characteristic | % (95% CI) |
|---|---|
| Sex | |
| Male | 48.2 (47.5–48.8) |
| Female | 51.8 (51.2–52.5) |
| Race | |
| White non-Hispanic | 74.3 (73.7–75.0) |
| Black non-Hispanic | 14.0 (13.5–14.4) |
| Hispanic | 6.5 (6.1–6.9) |
| Other non-Hispanica | 5.2 (4.9–5.5) |
| Age | |
| 18–24 | 9.9 (9.4–10.5) |
| 25–34 | 17.8 (17.2–18.4) |
| 35–44 | 21.4 (20.8–22.0) |
| 45–54 | 19.2 (18.8–19.7) |
| 55–64 | 14.5 (14.1–14.8) |
| 65–74 | 9.0 (8.7–9.3) |
| 75+ | 8.2 (8.0–8.5) |
| Education | |
| Less than 12 years | 9.3 (8.9–9.7) |
| 12 years | 30.1 (29.5–30.7) |
| Greater than 12 years | 60.6 (60.0–61.3) |
| Employment Status | |
| Currently employed | 61.1 (60.4–61.7) |
| Unemployed | 5.8 (5.5–6.2) |
| Retired | 16.3 (15.9–16.6) |
| Unable to work | 5.6 (5.3–5.9) |
| Housewife/student | 11.3 (10.9–11.8) |
| Marital Status | |
| Currently married | 60.6 (60.0–61.3) |
| Previously marriedb | 17.7 (17.3–18.1) |
| Never marriedc | 21.7 (21.1–22.4) |
| Health Care Coverage | |
| Yes | 86.4 (85.9–86.9) |
| No | 13.6 (13.1–14.1) |
| Preparedness Measures | |
| 3-day supply of food | 82.9 (82.4–83.5) |
| 3-day supply of water | 53.6 (52.9–54.3) |
| 3-day supply of prescription meds | 89.7 (89.2–90.1) |
| Working radio and batteries | 77.7 (77.2–78.3) |
| Working flashlight and batteries | 94.8 (94.4–95.1) |
| Evacuation plan | 21.1 (20.6–21.7) |
| Leave if mandatory evacuation | 94.9 (94.6–95.2) |
| Self-assessment of Preparedness | |
| Well prepared | 25.3 (24.8–25.9) |
| Somewhat prepared | 55.5 (54.9–56.2) |
| Not prepared at all | 19.1 (18.6–19.7) |
| Chronic Conditions | |
| Cardiovascular disease | 8.2 (7.9–8.5) |
| Diabetes | 8.7 (8.4–9.0) |
| Asthma | 8.5 (8.2–8.9) |
Asian, non-Hispanic; Native Hawaiian/Pacific Islander, non-Hispanic; American Indian/Alaska Native, non-Hispanic; other race, non-Hispanic; multi-race, non-Hispanic.
Previously married includes those divorced, widowed, or separated.
Never married includes those never married or member of unmarried couple.
Cardiovascular Disease
Approximately 8.2% of respondents had CVD (Table 2). Males were more likely to have CVD as were white non-Hispanics, individuals aged 55 years or older, individuals with less than 12 years of education, those unable to work or retired, and those who were previously married (Table 3). Approximately 91.0% of adults with CVD had health insurance coverage at the time of the survey. Individuals with CVD were more likely than those without to report that their household had a 3-day supply of food (85.9% versus 82.7%), a 3-day supply of water (60.9% versus 52.9%), a 3-day supply of prescription medication (94.4% versus 89.2%), and an evacuation plan (26.6% versus 20.7%). They were, however, less likely than those without CVD to indicate that they would leave their community if there was a mandatory evacuation (93.8% versus 95.0%) (Table 4). After adjusting for socio-demographic characteristics, all associations between prepared-ness and CVD status were attenuated and no longer significant except for having an evacuation plan (adjusted prevalence ratio, aPR =1.09; 95% CI, 1.01–1.17).
Table 3.
Sociodemographic Characteristics of the Study Sample by Type of Chronic Disease, BRFSS, United States, 2006–2010 (N =104,654)
| Demographic Characteristic | Cardiovascular Disease | Diabetes | Asthma | |||
|---|---|---|---|---|---|---|
| Yes % (95% CI) | Chi-square P Value | Yes % (95% CI) | Chi-square P Value | Yes % (95% CI) | Chi-square P Value | |
| Sex | ||||||
| Male | 9.4 (8.9–9.9) | < .0001 | 9.1 (8.6–9.6) | .0242 | 6.6 (6.0–7.1) | < .0001 |
| Female | 7.0 (6.7–7.3) | < .0001 | 8.4 (8.0–8.7) | .0242 | 10.4 (9.9–10.9) | < .0001 |
| Race | ||||||
| White non-Hispanic | 8.6 (8.3–8.9) | < .0001 | 8.1 (7.8–8.4) | < .0001 | 8.3 (7.9–8.7) | .0839 |
| Black non-Hispanic | 7.8 (7.1–8.6) | < .0001 | 12.2 (11.3–13.3) | < .0001 | 9.6 (8.5–10.8) | .0839 |
| Hispanic | 5.2 (4.1–6.6) | < .0001 | 6.6 (5.3–8.0) | < .0001 | 7.7 (6.0–9.8) | .0839 |
| Other non-Hispanica | 6.3 (5.3–7.5) | < .0001 | 10.6 (8.7–12.8) | < .0001 | 9.9 (8.1–12.2) | .0839 |
| Age | ||||||
| 18–24 | 0.4 (0.2–0.7) | < .0001 | 0.6 (0.3–1.1) | < .0001 | 9.4 (7.8–11.3) | .2870 |
| 25–34 | 1.4 (1.0–1.9) | < .0001 | 2.1 (1.7–2.7) | < .0001 | 8.6 (7.6–9.8) | .2870 |
| 35–44 | 2.5 (2.0–3.0) | < .0001 | 4.8 (4.1–5.6) | < .0001 | 8.4 (7.5–9.3) | .2870 |
| 45–54 | 6.4 (5.8–7.0) | < .0001 | 8.6 (7.9–9.3) | < .0001 | 8.4 (7.7–9.1) | .2870 |
| 55–64 | 12.9 (12.1–13.8) | < .0001 | 15.4 (14.5–16.3) | < .0001 | 9.1 (8.4–9.9) | .2870 |
| 65–74 | 20.7 (19.6–22.0) | 20.4 (19.3–21.6) | 8.4 (7.6–9.2) | |||
| 75+ | 29.5 (28.0–31.0) | 18.7 (17.4–20.0) | 7.7 (6.9–8.5) | |||
| Education | ||||||
| Less than 12 years | 16.1 (14.8–17.5) | < .0001 | 15.1 (13.9–16.5) | < .0001 | 12.2 (11.0–13.6) | < .0001 |
| 12 years | 9.3 (8.7–9.8) | < .0001 | 9.9 (9.3–10.5) | < .0001 | 8.1 (7.4–8.8) | < .0001 |
| Greater than 12 years | 6.4 (6.1–6.7) | < .0001 | 7.2 (6.8–7.6) | < .0001 | 8.2 (7.7–8.7) | < .0001 |
| Employment Status | ||||||
| Currently employed | 3.6 (3.3–3.9) | < .0001 | 5.0 (4.7–5.4) | < .0001 | 7.2 (6.7–7.7) | < .0001 |
| Unemployed | 5.5 (4.5–6.6) | < .0001 | 6.5 (5.3–7.9) | < .0001 | 11.7 (9.7–14.0) | < .0001 |
| Retired | 23.4 (22.4–24.3) | < .0001 | 19.8 (18.9–20.7) | < .0001 | 7.5 (6.9–8.1) | < .0001 |
| Unable to work | 26.2 (24.3–28.3) | < .0001 | 25.2 (23.3–27.3) | < .0001 | 22.2 (20.2–24.3) | < .0001 |
| Housewife/student | 3.9 (3.4–4.6) | < .0001 | 5.5 (4.7–6.4) | < .0001 | 9.2 (8.0–10.5) | < .0001 |
| Marital Status | ||||||
| Currently married | 7.7 (7.4–8.1) | < .0001 | 8.7 (8.3–9.1) | < .0001 | 7.4 (7.0–7.8) | < .0001 |
| Previously marriedb | 16.2 (15.4–17.1) | < .0001 | 14.4 (13.7–15.2) | < .0001 | 10.5 (9.7–11.2) | < .0001 |
| Never marriedc | 2.9 (2.5–3.4) | < .0001 | 4.2 (3.7–4.7) | < .0001 | 10.2 (9.2–11.4) | < .0001 |
| Health care Coverage | ||||||
| Yes | 91.0 (89.7–92.1) | < .0001 | 90.8 (89.6–91.8) | < .0001 | 87.2 (85.5–88.6) | < .0001 |
| No | 9.0 (7.9–10.3) | < .0001 | 9.3 (8.3–10.4) | < .0001 | 12.8 (11.4–14.5) | < .0001 |
Asian, non-Hispanic; Native Hawaiian/Pacific Islander, non-Hispanic; American Indian/Alaska Native, non-Hispanic; other race, non-Hispanic; multirace, non-Hispanic
Previously married includes those divorced, widowed, or separated
Never married includes those never married or member of unmarried couple
Table 4.
Unadjusted Prevalence and Adjusteda Prevalence Ratio of Preparedness Measures by Chronic Conditions, BRFSS, United States, 2006–2010 (N =104,654)
| Preparedness Measures | Cardiovascular Disease | Diabetes | Asthma | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| 3-day Supply of Food | ||||||
| % (95% CI) | 85.9 (84.5–87.1)* | 82.7 (82.1–83.3) | 84.0 (82.5–85.5) | 82.8 (82.2–83.4) | 81.1 (79.0–83.1) | 83.1 (82.6–83.7) |
| APR (95% CI) | 1.00 (0.98–1.02) | referent | 0.98 (0.96–1.01) | referent | 0.99 (0.97–1.01) | referent |
| 3-day Supply of Water | ||||||
| % (95% CI) | 60.9 (59.1–62.7)* | 52.9 (52.2–53.7) | 60.1 (58.2–61.9)* | 53.0 (52.2–53.7) | 53.8 (51.4–56.1) | 53.6 (52.9–54.3) |
| APR (95% CI) | 1.02 (0.99–1.07) | referent | 1.03 (0.99–1.07) | referent | 1.02 (0.97–1.07) | referent |
| 3-day Supply of Medication | ||||||
| % (95% CI) | 94.4 (93.5–95.2)* | 89.2 (88.6–89.7) | 94.7 (93.8–95.5)* | 89.1 (88.6–89.6) | 91.4 (89.7–92.8)* | 89.6 (89.1–90.1) |
| APR (95% CI) | 1.02 (1.00–1.03) | referent | 1.04 (1.02–1.05)* | referent | 1.02 (1.01–1.04)* | referent |
| Working Radio | ||||||
| % (95% CI) | 76.5 (75.0–78.0) | 77.9 (77.3–78.6) | 78.3 (76.8–79.7) | 77.7 (77.1–78.3) | 75.8 (73.7–77.8) | 77.9 (77.3–78.5) |
| APR (95% CI) | 0.99 (0.97–1.01) | referent | 1.02 (1.00–1.04) | referent | 1.00 (0.97–1.02) | referent |
| Working Flashlight | ||||||
| % (95% CI) | 94.1 (93.2–94.9) | 94.9 (94.5–95.2) | 94.7 (93.8–95.4) | 94.8 (94.4–95.1) | 93.0 (91.8–94.1)* | 94.9 (94.6–95.3) |
| APR (95% CI) | 0.99 (0.98–1.00) | referent | 1.00 (0.99–1.01) | referent | 0.99 (0.98–1.00) | referent |
| Evacuation Plan | ||||||
| % (95% CI) | 26.6 (25.0–28.2)* | 20.7 (20.1–21.2) | 27.0 (25.4–28.8)* | 20.6 (20.0–21.1) | 22.1 (20.4–23.9) | 21.0 (20.5–21.6) |
| APR (95% CI) | 1.09 (1.01–1.17)* | referent | 1.13 (1.05–1.22)* | referent | 1.03 (0.95–1.12) | referent |
| Leave if Mandatory Evacuation | ||||||
| % (95% CI) | 93.8 (92.9–94.7)* | 95.0 (94.7–95.3) | 94.2 (93.2–95.1) | 95.0 (94.6–95.3) | 93.7 (92.1–94.9) | 95.1 (94.7–95.4) |
| APR (95% CI) | 1.00 (0.99–1.01) | referent | 1.00 (0.99–1.01) | referent | 0.98 (0.96–1.00) | referent |
Significant at P <.05.
Adjusted for: gender, race/ethnicity, age group, education, employment status, marital status, and health care coverage.
Diabetes
Approximately 8.7% of respondents had diagnosed diabetes (Table 2). Males, black non-Hispanics, individuals aged 55 years or older, individuals with less than 12 years of education, those unable to work or retired, and individuals who were previously married were more likely to have diagnosed diabetes (Table 3). Approximately 90.8% of adults with diagnosed diabetes had health care coverage at the time of the survey. Compared to individuals without diagnosed diabetes, those with diabetes were more likely to report that their household had a 3-day supply of water (60.1% versus 53.0%), a 3-day supply of prescription medication (94.7% versus 89.1%), and an evacuation plan (27.0% versus 20.6%) (Table 4). After adjusting for socio-demographic characteristics, the differences remained significant for having a 3-day supply of prescription medication (aPR =1.04; 95% CI, 1.02–1.05) and an evacuation plan (aPR =1.13; 95% CI, 1.05–1.22).
Asthma
Approximately 8.5% of respondents had asthma at the time of the survey (Table 2). Females, individuals with less than 12 years of education, individuals unable to work, and those previously married or never married were more likely to have asthma (Table 3). Approximately 87.2% of adults with asthma had health care coverage at the time of the survey. Individuals with asthma were more likely than those without asthma to report that their household had 3-day supply of medication (91.4% versus 89.6%; chi-square Wald-F P value =.0311) and less likely to have a working battery-powered flashlight (93.0% versus 94.9%) (Table 4). After adjusting for sociodemographic characteristics, having a 3-day supply of medication (aPR =1.02, 95% CI, 1.01–1.04) remained significant.
Discussion
To the authors’ knowledge, this is the first study to examine the association between specific chronic illnesses and household preparedness items. This study found that, after adjusting for covariates, individuals with CVD, diagnosed diabetes, and asthma were generally no more likely to have a 3-day supply of food or water than those without these conditions. Adequate nutrition is important for any individual in the hours and days after a disaster due to increase stress and physical demands. For those with underlying chronic health conditions, limited access to food, water, shelter, power, and medical facilities may have more dire consequences, often leading to exacerbation of their underlying condition.14–16 The American Diabetes Association (ADA) recommended that waterproof and insulated disaster kits not only include medication and medical supplies, such as glucose testing strips and antibiotic ointments, but also prepackaged snacks.17
This study also found that, after adjusting for covariates, individuals with diagnosed diabetes and asthma were slightly more likely, but individuals with CVD were no more likely, to have a 3-day supply of medication than individuals without these conditions. Previous incidents have demonstrated that post-disaster continuity of care, especially continuation of daily medication for persons with chronic illnesses, is vital.18 One study found that approximately 7.2% of health care visits at emergency treatment facilities after Hurricane Katrina were for medication refills.8 Another study of Hurricane Katrina evacuees found that 38% of medication doses dispensed by federal relief teams and 73% of doses dispensed by retail pharmacies were for management of chronic conditions, with cardiovascular medications being the most common.19 Medication availability may attenuate the risk of disease exacerbation and complications that individuals with chronic diseases often experience post disaster. Individuals with diabetes often experience post-disaster complications ranging from the more mild (poor glycemic control) to the more severe (diabetic ketoacidosis, comas, tissue infections, stroke, and brain hemorrhages).14,20–22 Even with more mild complications, the effect may be long lasting. In some cases, poor glycemic control continued among diabetic patients receiving care from a state-funded medical center in New Orleans up to 16 months post-Hurricane Katrina.15 Emergency preparedness knowledge, such as the importance of an evacuation kit with an appropriate medication supply, should be included in patient and provider discussions regarding the patient’s self-management skills for their chronic conditions.
In this study, the majority of individuals with CVD had health care coverage; yet, they were no more likely to have a 3-day supply of medication after adjusting for health care coverage. Numerous agencies, including the Federal Emergency Management Agency (FEMA), the American Medical Association, and the American Red Cross have issued guidelines and support for individuals with chronic conditions to maintain an emergency reserve of medications and other supplies; 23–25 however, the amount of reserve medication recommended in these guidelines is inconsistent. Unfortunately, insurance policies often hinder the ability of an individual to prepare adequately and obtain emergency medication and supplies by authorizing 30–60 day quantities only.26 In a California study, insurance policies on average, only allowed prescription refills through a retail pharmacy after 70%–75% of the medication had been used.27 Moreover, only two out of nine insurers presented a “replacement” option for one annual extra medication supply with authorization and additional copayment.27 Depending on the timing of a disaster, individuals may not be able to secure additional or replacement medication under these policies. In other words, if a disaster occurs when individuals only have a few days of medication left and have not yet refilled their medications, they may have difficulties obtaining them after a disaster due to infrastructure obstacles.21 The resulting influx of individuals with chronic conditions into the medical system and emergency rooms for their refill needs as well as treatment for exacerbation of their conditions has been well documented in the literature.8,14,18–22 Efforts to increase accessibility to emergency supplies of medication for individuals should be explored.
Existing literature indicates that, in general, minority populations and lower income individuals and families are often the most negatively impacted by disasters.10,11,28 The importance of engaging extended family and social networks into preparedness planning efforts warrants further exploration.29 A possible contributing factor may be that chronic conditions are more prevalent among Black and Hispanic populations,30–31 as observed with this study’s sample of individuals with diabetes and asthma. In another detailed analysis of BRFSS data, Hispanics were significantly less likely than all other race/ethnicities to have a 3-day supply of food, a 3-day supply of medication, and a working battery-operated radio.11
Limitations
There are several limitations to this study. First, BRFSS data are self reported; thus, chronic diseases were not adjudicated. Second, preparedness may be overestimated due to a social desirability bias. Third, results from this study may not be generalizable as the General Preparedness module was only administered in 14 states and across different years. Fourth, the BRFSS sampling frame only includes individuals living in households with landlines. Finally, the response rate for the 14 states included in this study was low (range: 31.4% to 65.5%); however, post-stratification weights were used to reduce the impact of non-response.32
Conclusion and Recommendations
Results from this study lead to a few public health implications:
Mobilization of educational materials to health care providers, including physicians and pharmacists through their professional organizations, is necessary to ensure that patients receive emergency preparedness knowledge for their chronic conditions as standard of care. A module on emergency preparedness in self-management education programs for people with chronic conditions should be included. Such information can also be used by health departments to target outreach efforts and risk communication messages to affected populations.
Partnerships should be established between preparedness organizations and chronic disease organizations (such as advocacy groups and providers) to address the needs of these populations to improve community resiliency and community recovery. In fact, the National Standards for State and Local Planning encourage these types of partnerships when building public health preparedness capabilities.33
To increase the availability of an emergency supply of medication, in addition to a patients’ standard supply, partnerships should be built with multiple sectors such as health insurance companies, medication distribution agents, and manufacturers.
Considerable education campaigns and efforts should be directed to the minority population, due to the high prevalence of chronic disease and often low household preparedness levels.
Despite the increased morbidity and mortality associated with chronic conditions at times of disasters, persons with diabetes, cardiovascular disease, and asthma were generally not more prepared for natural or man-made disasters than those without each chronic condition.
Abbreviations
- ADA
American Diabetes Association
- aPR
adjusted prevalence ratio
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CVD
cardiovascular disease
- FEMA
Federal Emergency Management Agency
Footnotes
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1.Center for Research on the Epidemiology of Disasters. [Accessed March 6, 2013];EM-DAT: The International Disaster Database. http://www.emdat.be/result-country-profile?disgroup=natural&country=usa&period=2004$2013.
- 2.Vest JR, Valadez AM. Health conditions and risk factors of sheltered persons displaced by Hurricane Katrina. Prehosp Disaster Med. 2006;21(2):55–58. doi: 10.1017/s1049023x00003356. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed March 6, 2013];The Washington Post/Kaiser Family Foundation/Harvard University Survey Project Survey of Huricane Katrina Evacuees. 2005 http://www.kff.org/newsmedia/upload/7401.pdf.
- 4.Chan EY, Kim J. Chronic health needs immediately after natural disasters in middle-income countries: the case of the 2008 Sichuan, China earthquake. Eur J Emerg Med. 2011;18(2):111–114. doi: 10.1097/MEJ.0b013e32833dba19. [DOI] [PubMed] [Google Scholar]
- 5.Kolwaite A. Preparing for Functional Needs While Sheltering During a Disaster -Kentucky, 2011. Paper presented at: 61st Epidemic Intelligence Service Conference; April 16–20, 2012; Atlanta, Georgia USA. [Google Scholar]
- 6.Partnership for Solutions. [Accessed March 6, 2013];Chronic Conditions: Making the Case for Ongoing Care. http://www.policyarchive.org/handle/10207/21756.
- 7.Delfino RJ, Brummel S, Wu J, et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med. 2009;66(3):189–197. doi: 10.1136/oem.2008.041376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma AJ, Weiss EC, Young SL, et al. Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Med Public Health Prep. 2008;2(1):27–32. doi: 10.1097/DMP.0b013e31816452f0. [DOI] [PubMed] [Google Scholar]
- 9.Guha-Sapir D, van Panhuis WG, Lagoutte J. Short communication: patterns of chronic and acute diseases after natural disasters - a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami. Trop Med Int Health. 2007;12(11):1338–1341. doi: 10.1111/j.1365-3156.2007.01932.x. [DOI] [PubMed] [Google Scholar]
- 10.Ablah E, Konda K, Kelley CL. Factors predicting individual emergency preparedness: a multi-state analysis of 2006 BRFSS data. Biosecur Bioterror. 2009;7(3):317–330. doi: 10.1089/bsp.2009.0022. [DOI] [PubMed] [Google Scholar]
- 11.DeBastiani SD, Strine TW. Household Preparedness for Public Health Emergencies -14 States, 2006–2010. MMWR. 2012;61(36) [PubMed] [Google Scholar]
- 12.Bethel JW, Foreman AN, Burke SC. Disaster preparedness among medically vulnerable populations. Amer J Prev Med. 2011;40(2):139–143. doi: 10.1016/j.amepre.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Centers for Disease Control and Prevention. [Accessed July 3, 2013];Behavioral Risk Factor Surveillance System (BRFSS) http://www.cdc.gov/brfss/
- 14.Miller AC, Arquilla B. Chronic diseases and natural hazards: impact of disasters on diabetic, renal, and cardiac patients. Prehosp Disaster Med. 2008;23(2):185–194. doi: 10.1017/s1049023x00005835. [DOI] [PubMed] [Google Scholar]
- 15.Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mokdad AH, Mensah GA, Posner SF, et al. When chronic conditions become acute: prevention and control of chronic diseases and adverse health outcomes during natural disasters. Prev Chronic Dis. 2005;2(special issue):A04. [PMC free article] [PubMed] [Google Scholar]
- 17.American Diabetes Association. American diabetes association statement on emergency and disaster preparedness: a report of the disaster response task force. Diabetes Care. 2007;30(9):2395–2398. doi: 10.2337/dc07-9926. [DOI] [PubMed] [Google Scholar]
- 18.Arrieta MI, Foreman RD, Crook ED, Icenogle ML. Insuring continuity of care for chronic disease patients after a disaster: key preparedness elements. Am J Med Sci. 2008;336(2):128–133. doi: 10.1097/MAJ.0b013e318180f209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jhung MA, Shehab N, et al. Chronic Disease and Disasters. Medication demands of Hurricane Katrina evacuees. Am J Prev Med. 2007;33(3):207–210. doi: 10.1016/j.amepre.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 20.Inui A, Kitaoka H, Majima M, et al. Effect of the Kobe earthquake on stress and glycemic control in patients with diabetes mellitus. Arch Intern Med. 1998;158(3):274–278. doi: 10.1001/archinte.158.3.274. [DOI] [PubMed] [Google Scholar]
- 21.Cefalu WT, Smith SR, Blonde L, Fonseca V. The Hurricane Katrina aftermath and its impact on diabetes care: observations from “ground zero”: lessons in disaster preparedness of people with diabetes. Diabetes Care. 2006;29(1):158–160. doi: 10.2337/diacare.29.1.158. [DOI] [PubMed] [Google Scholar]
- 22.Salman S, Sengul AM, Salman F, et al. Influence of earthquake on the quality of life of patients with type 1 diabetes. Psychiatry Clin Neurosci. 2001;55(2):165. doi: 10.1046/j.1440-1819.2001.00807.x. [DOI] [PubMed] [Google Scholar]
- 23.Federal Emergency Management Agency. [Accessed March 6, 2013];Are you Ready? An In-depth Guide to Citizen Preparedness. http://www.ready.gov/are-you-ready-guide.
- 24.American Medical Association. [Accessed March 6, 2013];Personal medication supply in times of disaster. 2008 http://www.medicalnewstoday.com/articles/111921.php.
- 25.American Red Cross. [Accessed January 18, 2013];Preparedness Kit Contents. 2009 http://arcbrcr.org/
- 26.Allweiss P, Albright A. Diabetes, disasters, and decisions. Diabetes Management. 2011;1(4):369–377. [Google Scholar]
- 27.Carameli K, Eisenman DP, Blevins J, d’Angona B, Glik DC. Planning for chronic disease medications in disaster: perspectives from patients, physicians, pharmacists, and insurers. Disaster Med Public Health Prep. 2010;4:E1–E9. doi: 10.1001/dmp.2010.46. [DOI] [PubMed] [Google Scholar]
- 28.Andrulis DP, Siddiqui NJ, Gantner JL. Preparing racially and ethnically diverse communities for public health emergencies. Health Aff (Millwood) 2007;26(5):1269–1279. doi: 10.1377/hlthaff.26.5.1269. [DOI] [PubMed] [Google Scholar]
- 29.Eisenman DP, Cordasco KM, Asch S, Golden JF, Glik D. Disaster planning and risk communication with vulnerable communities: lessons from Hurricane Katrina. Am J Public Health. 2007;97(S1):S109–S115. doi: 10.2105/AJPH.2005.084335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update a report from the American heart association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National Health Statistics Reports. 2011;(32):1–14. [PubMed] [Google Scholar]
- 32.U.S. Centers for Disease Control and Prevention. [Accessed March 6, 2013];Behavioral Risk Factor Surveillance System Survey Data Documentation. 2006 http://www.cdc.gov/brfss/technical_infodata/surveydata/2006.htm.
- 33.U.S. Centers for Disease Control and Prevention. [Accessed March 8, 2013];Public Health Preparedness Capabilities: National Standards for State and Local Planning. 2011 www.cdc.gov/phpr/capabilities.