Abstract
Objective:
Cone-beam computed tomography (CBCT) has been proposed in surgical planning of lower third molar extraction. The aim of the present study was to assess the reliability of CBCT in defining third molar root morphology and its spatial relationships with the inferior alveolar nerve (IAN).
Materials and Methods:
Intraoperative and radiographic variables of 74 lower third molars were retrospectively analyzed. Intraoperative variables included IAN exposure, number of roots, root morphology of extracted third molars, and presence/absence of IAN impression on the root surface. Radiographic variables included presence/absence of the cortex separating IAN from the third molar roots on CBCT examination, number of roots and root morphology on both orthopantomography (OPG) and CBCT. The statistical association between variables was evaluated using the Fisher's exact test.
Results:
In all cases of intraoperative IAN exposure, the cortex appeared discontinuous on CBCT images. All cases, in which the cortical bone was continuous on CBCT images, showed no association with nerve exposure. In all cases in which nerve impression was identified on the root surface, the IAN cortex showed interruptions on CBCT images. No nerve impression was identified in any of the cases, in which the cortex appeared continuous on CBCT images. CBCT also highlighted accessory roots and apical anomalies/curvatures, not visible on the OPG.
Conclusions:
CBCT seems to provide reliable and accurate information about the third molar root morphology and its relationship with the IAN.
Keywords: Cortical interruption, nerve impression, tooth root
INTRODUCTION
The incidence of injury to the inferior alveolar nerve (IAN) after lower third molar removal has been reported to range from 0.26% to 8.4%[1] although values higher than 35%[2] have also been documented in cases where an intimate relationship between the tooth and the nerve was present.
Orthopantomography (OPG) is recommended as the first choice conventional radiographic examination for preliminary risk assessment of IAN damage since it is easy to perform and due to its low biological and economic costs. However, OPG is a two-dimensional examination which cannot provide reliable information on the actual anatomical relationship between the third molar and the IAN.[3,4,5,6,7,8] Actually, although several OPG markers have been proposed as risk indicators of a close anatomical relationship between teeth and the IAN, and therefore, as risk indicators of nerve damage, their absence does not exclude that nerve damage may result in the presence of a simple and limited radiographic superimposition on OPG.[1,9,10,11]
On the contrary, computed tomography (CT) and cone-beam CT (CBCT) allow to obtain precise knowledge of all third molar anatomical and topographical variables which is essential for proper surgical planning to minimize accidents and complications and provide the patient with clear information about the inherent risks.[10,11,12,13,14,15,16]
An ideal radiographic evaluation should provide accurate information about the morphology of the tooth which is to be extracted in relation to the degree of root formation, the number of roots, and the presence of apical anomalies. It should provide accurate information regarding the characteristics of the surrounding bone and the relationship with the neighboring anatomical structures.
When performing any preoperative radiographic examination, one should always take into account the principle “as low as reasonably achievable,” according to which the X-ray procedures with lower radiation doses should be followed.[10,12,17] Therefore, CT and CBCT should not be considered the radiographic methods of choice in surgical planning of lower third molar extraction; however, they should be reserved only for cases in which OPG reveals the presence of third molar topographic/anatomic variables which may influence the surgical approach.[10,11,15]
With regard to the risk of IAN injury, recent guidelines conclude that when conventional radiology highlights a direct relationship between the third molar and the nerve, CT or CBCT should be performed to obtain a thorough evaluation of the three-dimensional anatomical and topographical characteristics of the tooth to be removed.[10,11] Therefore, even the slightest superimposition between the third molar and IAN, also in the absence of specific risk markers at OPG among those proposed in the literature, is an indication for a second level radio-diagnostic in-depth analysis.[1,9,10,11]
In several studies, CT cross-sectional reconstruction was used to assess a possible cortical presence to separate the third molar from the IAN although the predictive value of this factor in IAN injury is still debated. Some authors[18,19,20,21,22] believe that IAN intraoperative exposure is an important risk factor in nerve damage, thus the absence of IAN cortical bone is considered a risk factor as well. Other studies[11,23] do not consider such factors as predictive or as conditions which can significantly influence the risk of nerve injury, but rather as simple highly indicative parameters of a close spatial tooth-IAN relationship.
To define the role of CBCT in planning third molar removal, the present study was carried out with the purpose to assess the accuracy of CBCT, comparing radiographic findings with intraoperative ones. In addition, OPG and CBCT evaluations of root morphology were also compared.
MATERIALS AND METHODS
Preoperative CBCT examinations of 74 previously extracted impacted mandibular third molars were reviewed. In all cases, CBCT was performed due to the third molar superimposition with the IAN on previous OPG images. All examinations were independently examined by all authors.
OPG was performed with a Sirona OrthoPhos XG Plus Machine (The Dental Company, New York, USA), with direct digitalization and the following data: Rotation time 14.1 s, 62–73 kV, 1–15 mA.
CBCT was performed with a NewTom VGi Dental X-ray Machine (QR, Verona, Italy) and the following technical data: Field of view 12 × 8, kV 110, exposure time 5.3 s, total mA 64.68, delivered dose 7.7 mGy, cross-sections 1 mm mesiodistally spaced.
For each third molar, the following variables were examined.
Radiographic variables: Cortical presence/absence to separate the IAN from the third molar roots on CBCT examination; number of roots and root morphology on both OPG and CBCT.
Intraoperative variables from patient clinical charts: IAN exposure, number of roots and root morphology of extracted third molars, and presence/absence of IAN impression on the root surface.
To test the accuracy of CBCT in identifying any interruption of IAN canal cortical bone, with consequent possible nerve exposure, the statistical association between the binary variable (present/absent) “IAN cortical interruption,” assessed on CBCT, and each of two other binary variables (yes/no), “IAN intraoperative exposure” and “IAN impression on the root surface,” were verified using the Fischer's exact test. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of CBCT were also evaluated.
The present study is part of a protocol which was approved by the Local Ethical Committee with the protocol number 987/12.
RESULTS
The 74 radiographic examinations of the present study involved mandibular third molars extracted in 63 patients, of which 23 were male (36.5%) and 40 were female (63.5%), with a mean age of 24.7 ± 6.5 years (range: 16–57 years).
Interruptions of IAN canal cortical bone on CBCT were found in 49/74 cases [66.21%; Figures 1 and 2], while intraoperative IAN exposure occurred in 31/74 cases (41.89%) and IAN root impression was found in 28/74 cases (37.84%).
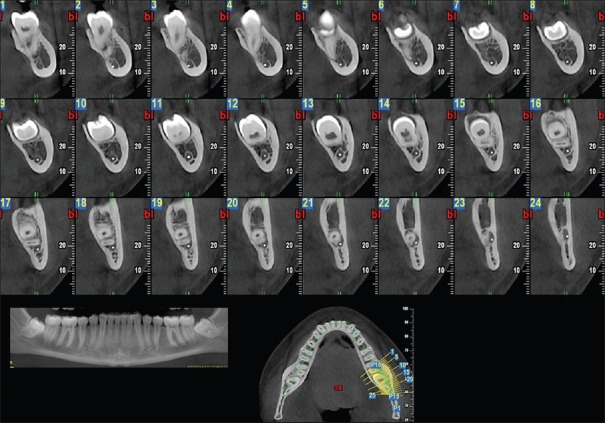
Figure 1.
Cone-beam computed tomography: 1 mm mesiodistally spaced cross-sections at the level of the lower right third molar which is vertically positioned. The third molar roots overlap the inferior alveolar nerve and the canal cortical bone does not show any discontinuity (sections 13 and 14)
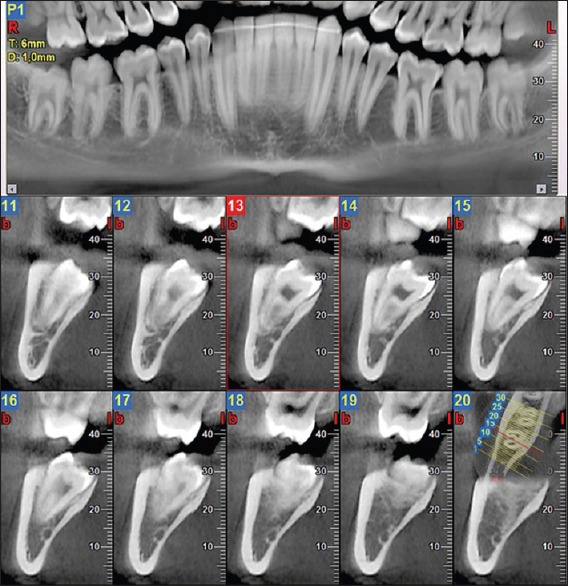
Figure 2.
Cone-beam computed tomography: 1 mm mesiodistally spaced cross-sections at the level of the lower left third molar which is mesially inclined. The third molar roots lap the inferior alveolar nerve and the canal cortical bone appears interrupted for a few millimeters (sections 18–23)
In all cases of intraoperative IAN exposure, the cortex was interrupted on CBCT images (P < 0.01), although in 18/49 cases (36.73%), the interruption was not associated with intraoperative nerve exposure. All cases, in which the cortical bone was continuous on CBCT images, showed no association with nerve exposure.
In all cases in which IAN impression was identified on the root surface of the extracted tooth, the IAN cortical was interrupted on CBCT images. In 21/49 cases (42.86%) in which the CBTC indicated a cortical interruption with direct root-nerve contact, no impression was identified on the tooth root after extraction. IAN root impression was not identified in any of the cases, in which the cortex appeared continuous on CBCT images.
A highly significant statistical correlation, therefore, exists between “IAN cortical interruption” and each of the two variables “IAN intraoperative exposure” and “IAN impression on the root surface.”
CBCT was able to predict a direct contact between the third molar root and IAN with a 75.67% accuracy (sensitivity: 100%; specificity: 58.14%; PPV: 63.27%; NPV: 100%; P < 0.01).
High sensitivity and high NPV also exclude that an IAN impression is found on the root surface of the extracted tooth in the case of continuous IAN cortical bone on CBCT images (sensitivity: 100%; specificity: 54.35%; PPV: 57.14%; NPV: 100%; accuracy: 71.62%; P < 0.01).
As for the assessment of apical curvatures, in ten cases OPG revealed distal curvatures, also verified on CBCT images and at postoperative evaluation of the extracted tooth. A buccal curvature was found in four molars, ipsilateral to the IAN in one case and associated with a distal curvature in three cases. Lingual apical curvatures were postsurgically identified in five cases. None of them were preliminarily recognized on OPG. Two of them were not detected even at CBCT. With regard to the number of roots, CBCT allowed the identification of accessory roots, unrecognizable on the OPG, in four cases.
DISCUSSION
The present study showed a strong association between intraoperative IAN exposure and interruptions of IAN cortex on CBCT images. Actually, although CBCT allowed to identify all cases of intraoperative nerve exposure, the IAN was not clinically visible in some cases in which the cortical bone appeared interrupted on CBCT. The lack of intraoperative IAN exposure may be related to different factors such as the small size of the cortical bone defect and its position in relation to the presence of undercuts or interradicular bone septa able to interfere with the surgical inspection.
Susarla et al.[18] found that a defect size lower than 3 mm on the CT is correlated to a low probability of intraoperative IAN exposure while other authors[13,24] found that IAN exposure is less likely when it runs lingually to the root or interradicularly. Therefore, the fact that the IAN cortex appears interrupted on CT images does not necessarily imply that the IAN is clinically visible. On the other hand, the presence of a cortex which separates the IAN from the third molar root seems to completely exclude the possibility of intraoperative nerve exposure (sensitivity 100%, specificity: 58.14%; PPV: 63.27%; NPV: 100%; accuracy: 75.67%; P < 0.01). This result is similar to that of Matzen and Wenzel[11] and seems somewhat different from that obtained by Susarla et al.[18] who reported an albeit relatively low possibility (5/80 cases) of intraoperative IAN exposure, even in the presence of a continuous cortex on the CT images. This discrepancy might be a consequence of different types of CT machines and settings, as well as of different surgical techniques or possible cortical or interradicular septa fractures during the third molar luxation. Although the IAN cortex was interrupted on CT images in all cases in which an impression on root surface was found, interruptions were also detected in the absence of the corresponding IAN impression on the root. Therefore, in the presence of a close anatomical proximity, as revealed by the lack of cortical integrity on CT, it is plausible that an IAN impression is not always found on the root surface, while an intact cortex on CT appears to completely exclude any possibility of IAN impression on the root. The latter can be also considered indicative of a close spatial relationship between root and nerve although its absence does not rule out a proximity (sensitivity: 100%; specificity: 54.35%; PPV: 57.14%; NPV 100%; accuracy: 71.62%; P < 0.01). The absence of an IAN impression in the cases where the CBCT showed an interrupted cortex could be related to morphological root factors such as the presence of curvatures or apical tapering which follow the shape of the IAN canal itself, without leaving any visible trace. Some authors also showed that the IAN impression on the root was more frequently associated to the lingual position of the nerve to the root.[14,24]
The previous studies[11,15,23] support the findings of the present study in that CBCT also identified accessory roots and apical anomalies/curvatures, not visible on OPG.
CONCLUSION
CBCT imaging seems to provide accurate information about the third molar root morphology and its relationship with the IAN since it allows to identify all cases in which the IAN is exposed and all cases in which an IAN impression is present on the root surface. All this information is crucial for efficient surgical planning and for providing patients with appropriate information about the surgical risks. However, cortical interruptions on CBCT, although strongly indicative of a close spatial relationship with the third molar root, neither necessarily imply that the IAN will be exposed during the third molar extraction nor imply that an impression will be present on the tooth root surface; hence, cortical interruptions cannot be taken into account when predicting IAN damage during the third molar surgery.
All authors contributed substantially to this work.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: An literature review of prospective studies. Int J Oral Maxillofac Surg. 2011;40:1–10. doi: 10.1016/j.ijom.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Jhamb A, Dolas RS, Pandilwar PK, Mohanty S. Comparative efficacy of spiral computed tomography and orthopantomography in preoperative detection of relation of inferior alveolar neurovascular bundle to the impacted mandibular third molar. J Oral Maxillofac Surg. 2009;67:58–66. doi: 10.1016/j.joms.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Szalma J, Lempel E, Jeges S, Szabó G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: Retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:294–302. doi: 10.1016/j.tripleo.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 4.Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:377–83. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]
- 5.Blaeser BF, August MA, Donoff RB, Kaban LB, Dodson TB. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg. 2003;61:417–21. doi: 10.1053/joms.2003.50088. [DOI] [PubMed] [Google Scholar]
- 6.Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63:3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 7.Gomes AC, Vasconcelos BC, Silva ED, Caldas Ade F, Jr, Pita Neto IC. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg. 2008;66:256–9. doi: 10.1016/j.joms.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Atieh MA. Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg. 2010;68:74–82. doi: 10.1016/j.joms.2009.04.074. [DOI] [PubMed] [Google Scholar]
- 9.Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20–5. doi: 10.1016/0266-4356(90)90005-6. [DOI] [PubMed] [Google Scholar]
- 10.Guidelines on CBCT for Dental and Maxillofacial Radiology. SEDENTEXCT Project. [Last accessed on 2016 May]. Available from: http://www.sedentexct.eu/files/radiation_protection_172.pdf .
- 11.Matzen LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: A review – Based on a hierarchical model of evidence. Dentomaxillofac Radiol. 2015;44:20140189. doi: 10.1259/dmfr.20140189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Vlijmen OJ, et al. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: A pilot study. Int J Oral Maxillofac Surg. 2011;40:834–9. doi: 10.1016/j.ijom.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 13.Maegawa H, Sano K, Kitagawa Y, Ogasawara T, Miyauchi K, Sekine J, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:639–46. doi: 10.1016/s1079-2104(03)00356-1. [DOI] [PubMed] [Google Scholar]
- 14.Ohman A, Kivijärvi K, Blombäck U, Flygare L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac Radiol. 2006;35:30–5. doi: 10.1259/dmfr/58068337. [DOI] [PubMed] [Google Scholar]
- 15.Suomalainen A, Ventä I, Mattila M, Turtola L, Vehmas T, Peltola JS. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:276–84. doi: 10.1016/j.tripleo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Park JB, Kim N, Park S, Ko Y. Evaluation of number of roots and root anatomy of permanent mandibular third molars in a Korean population, using cone-beam computed tomography. Eur J Dent. 2013;7:296–301. doi: 10.4103/1305-7456.115413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991;21:1–201. [PubMed] [Google Scholar]
- 18.Susarla SM, Sidhu HK, Avery LL, Dodson TB. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg. 2010;68:1296–303. doi: 10.1016/j.joms.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 19.Ueda M, Nakamori K, Shiratori K, Igarashi T, Sasaki T, Anbo N, et al. Clinical significance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral Maxillofac Surg. 2012;70:514–20. doi: 10.1016/j.joms.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 20.Nakamori K, Tomihara K, Noguchi M. Clinical significance of computed tomography assessment for third molar surgery. World J Radiol. 2014;6:417–23. doi: 10.4329/wjr.v6.i7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park W, Choi JW, Kim JY, Kim BC, Kim HJ, Lee SH. Cortical integrity of the inferior alveolar canal as a predictor of paresthesia after third-molar extraction. J Am Dent Assoc. 2010;141:271–8. doi: 10.14219/jada.archive.2010.0160. [DOI] [PubMed] [Google Scholar]
- 22.Nakayama K, Nonoyama M, Takaki Y, Kagawa T, Yuasa K, Izumi K, et al. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg. 2009;67:2587–91. doi: 10.1016/j.joms.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 23.Guerrero ME, Botetano R, Beltran J, Horner K, Jacobs R. Can preoperative imaging help to predict postoperative outcome after wisdom tooth removal. A randomized controlled trial using panoramic radiography versus cone-beam CT? Clin Oral Investig. 2014;18:335–42. doi: 10.1007/s00784-013-0971-x. [DOI] [PubMed] [Google Scholar]
- 24.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Bergé SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg. 2009;38:964–71. doi: 10.1016/j.ijom.2009.06.007. [DOI] [PubMed] [Google Scholar]