Abstract
Objectives:
The objective of this study is to assess the knowledge and practice of dentists from Jordan, regarding prevention of infective endocarditis (IE) in dental practice.
Materials and Methods:
A sample of Jordanian dentists was interviewed regarding their IE knowledge and practice using a validated and pretested survey instrument.
Results:
Most of the dentists have encountered a patient with IE who needed prophylactic antibiotic (PA) and have prescribed antibiotics to prevent IE. Jordanian dentists’ approach to patients in need for PA varied between the National Institute for Health and Clinical Excellence recommendations and the American Heart Association to a lesser degree, but still a relatively high percent (39%) did not know any guidelines to follow although 74% have encountered patients who needed endocarditis prophylaxis. Patients with prosthetic heart valve were ranked on top of medical conditions that required PA (87.4%), and most dentists (94.5%) thought that dental extractions need PA followed by periodontal surgery (88.2%).
Conclusion:
There is a lack of consistency in the knowledge and practice of Jordanian dentists with regard to IE. There is a need to take actions to improve dentist's knowledge regarding this topic.
Keywords: Antibiotic choice, antibiotic prophylaxis, dental procedures, dentist's knowledge, infective endocarditis
INTRODUCTION
Infective endocarditis (IE), which is a life-threatening infection of the endocardium or heart valves, is usually associated with cardiac defects, congenital, or acquired.[1] Oral cavity, with more than 600 microbiological species have been recorded in the human mouth, is also home to microbial communities with multiple effects in human health and disease.[2] Various dental procedures have been linked to the occurrence of IE. Nevertheless, there seems to be a dilemma about which dental procedures and under what circumstances significant risk occurs.[3] Several guidelines regarding IE prevention are available globally including, British Society for Antimicrobial Chemotherapy guidelines (BSAC) on 2006, National Institute for Health and Clinical Excellence guidelines (NICE) on 2008, European Society of Cardiology guidelines on 2009, the Australian guidelines, and the American Heart Association guidelines (AHA) on 2007; most of these guidelines recommended a more restrictive use of prophylaxis for IE.[4,5,6,7] The BSAC guidelines reduced cardiac conditions in which prophylaxis indicated to the presence of prosthetic valves, a history of IE, and some congenital heart diseases.[8] AHA guidelines added another indication, valvulopathy in cardiac transplant recipients.[9] NICE guidelines did not recommend any prophylaxis to patients for IE prevention regardless their risk.[10]
The data about epidemiology of IE in Jordan are scarce, mostly due to the absence of nationwide studies in this regard. Similarly, little is known about the practice of general dental practitioners in Jordan, regarding prevention of IE and their compliance with international guidelines of IE prophylaxis.
The aim of this study was to assess the knowledge and practice of dentists from Jordan, regarding prevention of IE in dental practice.
MATERIALS AND METHODS
This cross-sectional study was approved by the Faculty of Dentistry Research and Ethics Committee in accordance with the World Medical Declaration of Helsinki. Ethical protocol number (12/2015).
A total of 210 dentists were approached to participate in the study, and 127 agreed to participate. A survey instrument was used to interview participants. The survey instrument included questions about demographic data, knowledge about risk factors of IE, and predisposing dental procedures and their current practice of prescribing antibiotics to at-risk patients [Appendix 1].
Statistical analysis performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics used to describe our study sample. To examine differences between groups, Chi-square test, one-way ANOVA, Student's t-test, and Spearman's rho test were used. Results with P < 0.05 considered statistically significant.
RESULTS
The sample was composed of 52.8% males and 47.2% females. Mean age was 33.5 years (range 22–65 years) with 1–40 years of experience (mean 9 years) [Table 1].
Table 1.
Demographic characteristics of participating dentists
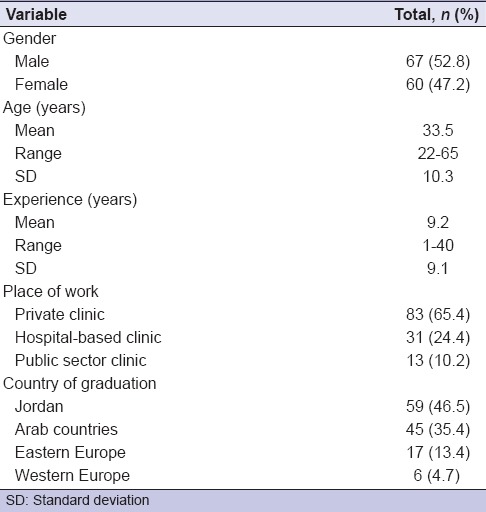
As shown in Table 1, most of the respondents were working in private clinics and graduated from Jordanian universities.
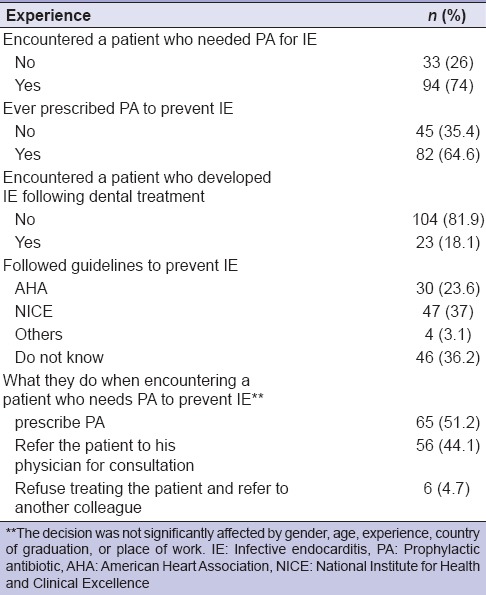
Most of the dentists have encountered a patient with IE who needed prophylactic antibiotic (PA) and have prescribed PA to prevent IE, 37% were following the NICE guidelines, and 23.6% were following AHA guidelines. Majority of the respondents (51%) have prescribed PA when encountering suspected patient to prevent IE, 44% have referred, and only 4.7% have refused to treat these patients [Table 2].
Table 2.
Experience with infective endocarditis
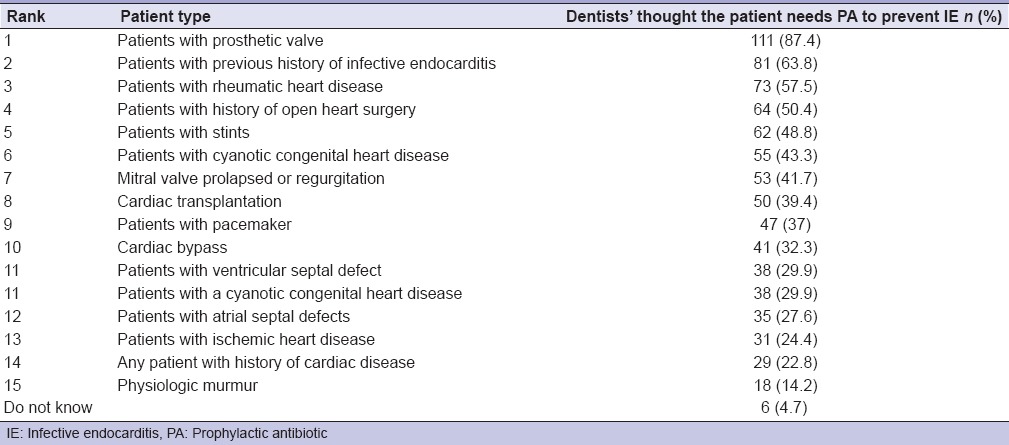
Patients with prosthetic heart valve were ranked on top of medical conditions that required PA (87.4%), and then patients with the previous history of IE, followed by patients with rheumatic heart disease (57.5), the least record was for patients having physiologic murmurs [Table 3].
Table 3.
Patients who need prophylactic antibiotics to prevent infective endocarditis
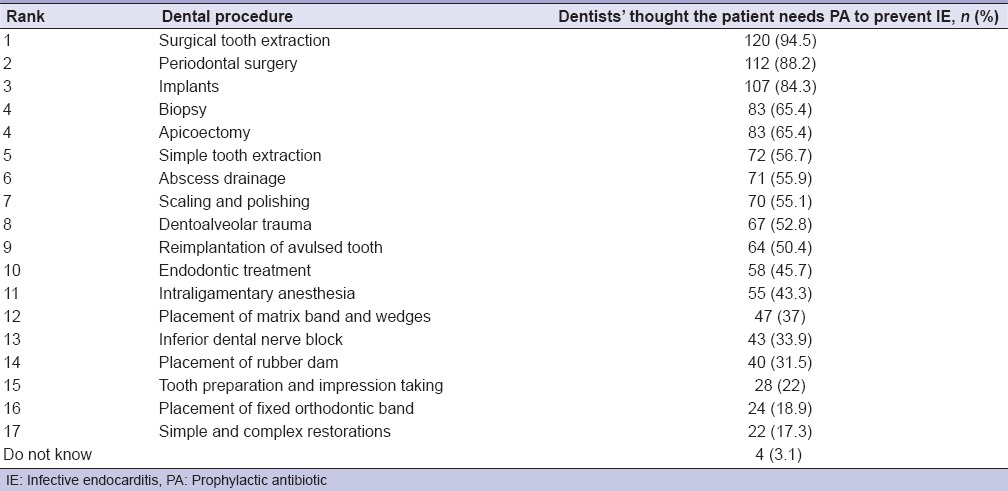
Regarding dental procedures which needed PA [Table 4], most dentists (87.4%) thought that dental extractions need PA, followed by periodontal surgery (88.2%); however, only 17.3% thought that PA is needed for simple tooth restorations.
Table 4.
Procedures that require the administration of prophylactic antibiotics to prevent infective endocarditis
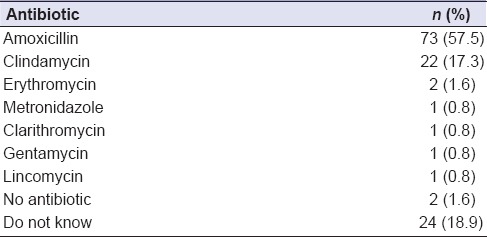
Amoxicillin was the antibiotic of choice for 57.5% of dentists to prevent IE, 17.3% prescribed clindamycin; a minority have prescribed lincomycin, metronidazole, gentamicin, and clarithromycin. Around 19% of dentists did not know which antibiotic to prescribe [Table 5].
Table 5.
Antibiotics prescribed for prevention of infective endocarditis before dental procedures
DISCUSSION
Dental procedures, especially the invasive ones, are being blamed for causing IE.[1,3,4] We aimed in this study to assess the knowledge and practice of dentists in Jordan, regarding prevention of IE in dental practice.
Although the NICE recommended the restriction of antibiotic prophylaxis (AP) use to very few predefined circumstances,[8] more than 50% of Jordanian dentists still prescribe PA widely to prevent IE.
Jordanian dentists' approach patients in need for PA varied between the NICE recommendations and the AHA to a lesser degree, but still a relatively high percent (39%) did not know any guidelines to follow although 74% have encountered patients who needed PA to prevent IE.
Only 37% of the respondents followed the NICE guidelines compared with a similar study in London, in which 95% of participants were aware of the NICE guidelines and 77% of them were compliant with those guidelines.[11]
This controversy, over the PA prescription for the different dental procedure, is a critical issue among dentists worldwide, which is affected by both the new guidelines and the IE incidence.[12]
Prosthetic heart valves and preexisting structural abnormality of the heart are major risk factors for IE,[13] a fact which is well appreciated by 87% of Jordanian dentists; comparable results were reported by an Iranian study.[11] While 14.2% of Jordanian dentists prescribe PA for cases of physiologic murmurs, 87.2% of their Iranian counterparts prescribe PA for this condition. This might be due to the variations of the universal recommendations or due to lack of knowledge regarding the clinical condition.
Dental procedures that needed PA, due to invasive nature and the risk of bacteremia were extractions and periodontal surgery; majority of Jordanian dentists agree with this fact.[12,14,15]
While Amoxicillin was the drug of choice as PA for 57.5% of respondents in this study, it was the drug of choice for 89% of Nigerian dentists.[16] In contrast, most general dentists in Japan prescribe cephams followed by Penicillin.[17]
Giving PA is not without harm although it is crucial in certain specific circumstances. Antimicrobial resistance is an emerging issue that must be dealt with to decelerate its progression. PA aim only to prevent IE due to viridans streptococci, and in its best case scenario can prevent up to 10% of all cases of IE.[18] Based on these statistics, it is not feasible to give PA to every cardiac patient, and it is worth to adhere with the guidelines to prevent IE in the specific patients, the PA target, without adding on antimicrobial resistance.
It has been reported that all observational studies such as cross-sectional surveys are prone to limitation and bias.[19] In this study, the number of participants is limited as a big number of dentists refused to participate; it may be due to their inadequate knowledge about this issue. Moreover, most dentists still prescribe PA in most cardiac patients although it is not recommended anymore in the majority of them; this discrepancy might be due to lack of update on their knowledge about the guidelines.
CONCLUSION
Although the issue of AP to prevent IE is controversial and no general consensus exists, a large proportion of dentists still do not follow any guidelines. The majority of dentists encountered a patient who needs PA so that the level of knowledge and practice need to be upgraded in Jordan.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIX 1: QUESTIONNAIRE
Age:
Gender:
Country of graduation:
Years of practice:
Place of practice: Private clinics, hospital-based clinic, public sector clinic
Have you encountered a patient who needed prophylactic antibiotics to prevent infective endocarditis?
Yes no
Have you ever prescribed prophylactic antibiotics to prevent infective endocarditis to your patients?
Yes no
Have you ever encountered a patient who developed infective endocarditis following dental treatment?
Yes no
Which guidelines regarding prevention of infective endocarditis do you follow in your practice?
AHA NICE others I do not know
If you encounter a patient who needs prophylactic antibiotics to prevent infective endocarditis
I prescribe the prophylactic antibiotics
Refer the patient to his physician for consultation
Refuse treating the patient and refer him to another colleague.
Which of the following patients would need prophylactic antibiotics to prevent infective endocarditis?
Patients with prosthetic valve
Patients with stents
Patients with history of open heart surgery
Patients with ischemic heart disease
Patients with ventricular septal defect
Patients with atrial septal defects
Patients with rheumatic heart disease
Patients with cyanotic congenital heart disease
Patients with a cyanotic congenital heart disease
Any patient with history of cardiac disease
Patients with previous history of infective endocarditis
Cardiac bypass
Patients with pacemaker
Mitral valve prolapsed or regurgitation
Physiologic murmur
Cardiac transplantation
Do not know.
Which of the following procedures would require the administration of prophylactic antibiotics to prevent infective endocarditis?
Surgical tooth extraction
Periodontal surgery
Implants
Biopsy
Apicoectomy
Reimplantation of avulsed tooth
Scaling and polishing
Simple tooth extraction
Endodontic treatment
Abscess drainage
Dentoalveolar trauma
Placement of fixed orthodontic band
Simple and complex restorations
Tooth preparation and impression taking
Placement of rubber dam
Placement of matrix band and wedges
Intraligamentary anesthesia
Inferior dental nerve block
Do not know.
Which antibiotics do you prescribe for prevention of infective endocarditis before dental procedures?
Type
Dose
Duration.
REFERENCES
- 1.Jain P, Stevenson T, Sheppard A, Rankin K, Compton SM, Preshing W, et al. Antibiotic prophylaxis for infective endocarditis: Knowledge and implementation of American Heart Association Guidelines among dentists and dental hygienists in Alberta, Canada. J Am Dent Assoc. 2015;146:743–50. doi: 10.1016/j.adaj.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Germano F, Bramanti E, Arcuri C, Cecchetti F, Cicciù M. Atomic force microscopy of bacteria from periodontal subgingival biofilm: Preliminary study results. Eur J Dent. 2013;7:152–8. doi: 10.4103/1305-7456.110155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahammam MA, Abdelaziz NM. Awareness of antimicrobial prophylaxis for infective endocarditis among dental students and interns at a teaching hospital in Jeddah, Saudi Arabia. Open Dent J. 2015;9:176–80. doi: 10.2174/1874210601509010176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thornhill MH, Lockhart PB, Prendergast B, Chambers JB, Shanson D. NICE and antibiotic prophylaxis to prevent endocarditis. Br Dent J. 2015;218:619–21. doi: 10.1038/sj.bdj.2015.496. [DOI] [PubMed] [Google Scholar]
- 5.Kazi DS, Bolger AF. Infective endocarditis and antibiotic prophylaxis. Lancet. 2015;386:530. doi: 10.1016/S0140-6736(15)61469-6. [DOI] [PubMed] [Google Scholar]
- 6.Di Filippo S. Prophylaxis of infective endocarditis in patients with congenital heart disease in the context of recent modified guidelines. Arch Cardiovasc Dis. 2012;105:454–60. doi: 10.1016/j.acvd.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Diz Dios P. Infective endocarditis prophylaxis. Oral Dis. 2014;20:325–8. doi: 10.1111/odi.12221. [DOI] [PubMed] [Google Scholar]
- 8.Al-Fouzan AF, Al-Shinaiber RM, Al-Baijan RS, Al-Balawi MM. Antibiotic prophylaxis against infective endocarditis in adult and child patients. Knowledge among dentists in Saudi Arabia. Saudi Med J. 2015;36:554–61. doi: 10.15537/smj.2015.5.10738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghaderi F, Oshagh M, Dehghani R, Hasanshahi R. Awareness of Iranian's general dentists regarding the latest prophylaxis guideline for prevention of infective endocarditis. J Dent (Shiraz) 2013;14:6–12. [PMC free article] [PubMed] [Google Scholar]
- 10.Lockhart PB, Hanson NB, Ristic H, Menezes AR, Baddour L. Acceptance among and impact on dental practitioners and patients of American Heart Association recommendations for antibiotic prophylaxis. J Am Dent Assoc. 2013;144:1030–5. doi: 10.14219/jada.archive.2013.0230. [DOI] [PubMed] [Google Scholar]
- 11.Farook SA, Davis AK, Khawaja N, Sheikh AM. NICE guideline and current practice of antibiotic prophylaxis for high risk cardiac patients (HRCP) among dental trainers and trainees in the United Kingdom (UK) Br Dent J. 2012;213:E6. doi: 10.1038/sj.bdj.2012.723. [DOI] [PubMed] [Google Scholar]
- 12.Thornhill MH. Infective endocarditis: The impact of the NICE guidelines for antibiotic prophylaxis. Dent Update. 2012;39:6–10, 12. doi: 10.12968/denu.2012.39.1.6. [DOI] [PubMed] [Google Scholar]
- 13.Dayer MJ, Chambers JB, Prendergast B, Sandoe JA, Thornhill MH. NICE guidance on antibiotic prophylaxis to prevent infective endocarditis: A survey of clinicians' attitudes. QJM. 2013;106:237–43. doi: 10.1093/qjmed/hcs235. [DOI] [PubMed] [Google Scholar]
- 14.Ahmadi-Motamayel F, Vaziri S, Roshanaei G. Knowledge of general dentists and senior dental students in Iran about prevention of infective endocarditis. Chonnam Med J. 2012;48:15–20. doi: 10.4068/cmj.2012.48.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hashemipour M, Korki M. Antibiotic prophylaxis for bacterial endocarditis: A study of knowledge of guidelines among dentists participated in the 47th international congress of dentistry. Dent J Tehran Univ Med Sci. 2008;21:210–8. [Google Scholar]
- 16.Adeyemo WL, Oderinu OH, Olojede AC, Ayodele AO, Fashina AA. Nigerian dentists' knowledge of the current guidelines for preventing infective endocarditis. Community Dent Health. 2011;28:178–81. [PubMed] [Google Scholar]
- 17.Nakano K, Ooshima T. Common knowledge regarding prevention of infective endocarditis among general dentists in Japan. J Cardiol. 2011;57:123–30. doi: 10.1016/j.jjcc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Pallasch T. Antibiotic prophylaxis. Endodontic Topics. 2003;4:46–59. [Google Scholar]
- 19.Al-Shamiri HM, Alaizari NA, Al-Maweri SA, Tarakji B. Knowledge and attitude of dental trauma among dental students in Saudi Arabia. Eur J Dent. 2015;9:518–22. doi: 10.4103/1305-7456.172636. [DOI] [PMC free article] [PubMed] [Google Scholar]


