Abstract
Objective:
The aim of this study was to evaluate the oral health attitudes and behavior of students in the oral health curriculum in Australia and New Zealand.
Materials and Methods:
The Hiroshima University - Dental Behavioral Inventory was administered to students in the first (year 1) and final years (year 3) of the oral health curriculum at Charles Sturt University in Australia and the University of Otago in New Zealand. A total of fifty-two year 1 students and forty-five year 3 students completed English version of the questionnaire in 2013. The responses were statistically analyzed by Fisher's exact tests and exact logistic regression models.
Results:
The responses of students in years 1 and 3 differed significantly for “I worry about the color of my teeth” at Charles Sturt University and at the University Otago, for “I think my teeth are getting worse despite my daily brushing,” “I put off going to the dentist until I have a toothache,” and “I don't feel I've brushed well unless I brush with strong strokes.” The estimated odds ratios from the exact logistic regression models showed that year 1 students were more likely to agree with above-mentioned four questions.
Conclusions:
Oral Health students who had been educated in a 3-year oral health curriculum in Australia and New Zealand had more positive attitudes and behaviors related oral health than did students at the beginning of their curriculum.
Keywords: Curriculum, oral health attitude, oral health behaviors
INTRODUCTION
The role of mid-level dental care providers is increasing in importance due to the need for oral health promotion and disease prevention.[1] These workforce members can address the problem of access to care by means of complementary relationships with dentists, especially in underserved areas. One model of a mid-level provider, called the dental therapist, is a registered professional who can provide certain facets of dental treatment, including preventive and restorative procedures.[2,3] Nash et al. reported that 54 countries are currently utilizing dental therapists.[4] In some countries, the education of dental therapists and dental hygienists is combined in a 3-year undergraduate university curriculum leading to the Bachelor degree.[4] The dual-qualification curriculum is usually called the oral health curriculum.[2,5] In particular, in Australia, a dual-qualified dental therapists/hygienist is categorized as an oral health therapist under one registration.[6] Figure 1 summarizes the historical transition of the qualifications for dental therapists and dental hygienists in Australia and New Zealand.[2,6,7] These dual-qualified dental therapists/hygienists have accomplishments in a wide range of dental services involving diagnosing and recognizing oral conditions, planning and delivering preventive and restorative treatment, and collaborating with other dental and general health practitioners.[7]
Figure 1.
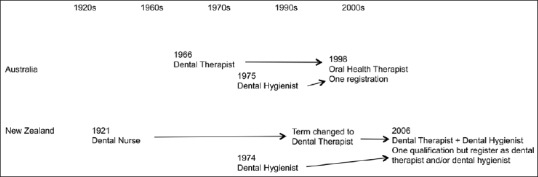
Historical transition of the qualification for dental therapists and dental hygienist in Australia and New Zealand
The Hiroshima University - Dental Behavioral Inventory (HU-DBI) is a questionnaire that consists of twenty items in a dichotomous format (agree/disagree) to observe oral health-related attitudes and behaviors regarding toothbrushing.[8] The HU-DBI has been previously used to examine the oral health attitudes and behaviors of dental students[9,10,11,12,13,14,15,16] and dental hygiene students.[17,18,19,20] Before this study, the HU-DBI had not previously been applied to oral health students.
While completing the undergraduate curriculum, oral health students should present themselves as good oral health models. The aim of this study was to determine the oral health attitudes and behaviors of 1st- and 3rd-year oral health students from Charles Sturt University, Australia and the University of Otago, New Zealand.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Charles Sturt University (Approval #414/2013/04) and by the University of Otago Human Ethics Committee.
Oral health students' oral health-related behaviors and attitudes were measured by means of the HU-DBI questionnaire in the 1st year of the curriculum (year 1) and the final year of the curriculum (year 3) at Charles Sturt University, in Australia and the University of Otago, in New Zealand. Year 1 and year 3 oral health students at the two universities were participated in this survey and responded to English version of the HU-DBI questionnaire. A total of 52 students in year 1 and 45 students in year 3 answered in 2013.
We analyzed the responses for each university by comparing the data from the year 1 students with the data from the year 3 students, using the Fisher's exact tests. We applied exact logistic regression models to each HU-DBI question separately to examine whether year 1 students have oral health behaviors similar to those of year 3 dental students while accounting for discrepancies between universities. These exact methods are statistically conservative to prevent erroneous conclusions and are appropriate for this study size. Statistical significance level was set at 0.05. The data were analyzed with SAS 9.3 (SAS Institute, Inc., Cary, NC, USA).
RESULTS
Table 1 shows the frequencies and percentages of students and their mean age in year 1 and year 3. At Charles Sturt University, the average ages (standard deviation [SD]) of year 1 and year 3 respondents were 24.2 (8.1) and 25.5 (6.9) years old, respectively. At the University of Otago, the average ages (SD) of year 1 and year 3 respondents were 24.9 (8.0) and 23.7 (4.2) years old, respectively.
Table 1.
Overview of the respondents' background characteristics
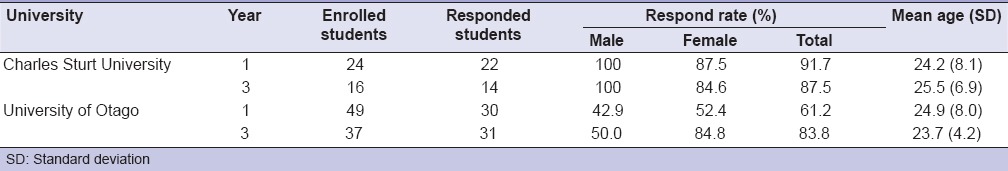
Table 2 shows the items on the HU-DBI questionnaire and the percentages of “agree” responses of the oral health students in year 1 and year 3 by university. The responses of the students in the two groups differed significantly only for question #3 at Charles Sturt University. The responses of the students in the two groups differed significantly to questions #8, #15, and #18 at the University of Otago.
Table 2.
Items on the Hiroshima University Dental Behavioral Inventory and percentages of “agree” responses of dental students in year 1 and year 3
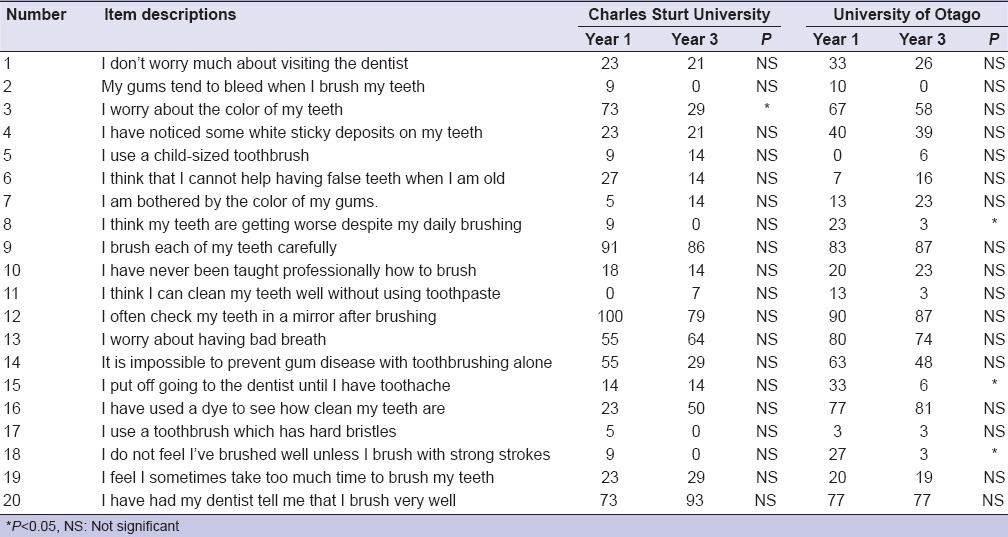
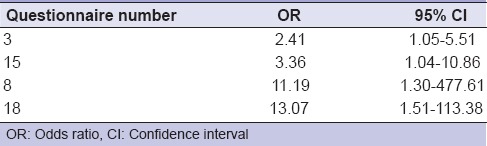
Table 3 shows that the estimated odds ratios and 95% confidence intervals from the exact logistic regression models were significant for only four questions. It was more likely that, after adjustment for university, year 1 students would agree on questions #3, #8, #15, and #18. For question #3, year 1 students had 2.4 times the odds of worrying about the color of their teeth than did those in year 3 (P = 0.03). For question #15, year 1 students had 3.4 times the odds of putting off going to the dentist until experiencing pain than did year 3 students (P = 0.03). For question #8, year 1 students had more than 11 times the odds of perceiving tooth decline despite brushing compared with year 3 students (P = 0.02). Year 1 students had more than 13 times the odds of feeling the need to brush with strong strokes than did year 3 students (P < 0.01).
Table 3.
Significant Hiroshima University-Dental Behavioral Inventory questions and odds ratios of agreement for year 1 versus year 3 students
DISCUSSION
The oral health curriculum in Australia and New Zealand consists of a 3-year curriculum that covers basic science, as well as education for dental therapy, dental hygiene, and oral health promotion. Year 1 students take mainly didactic courses. As they progress to year 3, students have opportunities to participate in clinical practice at university, community, and rural clinics under the supervision of registered clinicians. This curriculum promotes positive oral health-related attitudes and behaviors to students and enables oral health students to act as valuable role models for their patients and to promote oral health for individuals and the community.
The results of this study suggest that education for oral health students has a significant effect. Year 3 students were less likely to “agree” with responses to questions such as “I worry about the color of my teeth” (#3); “I think my teeth are getting worse despite my daily brushing” (#8); “I put off going to the dentist until I have toothache” (#15); and “I don't feel I've brushed well unless I brush with strong strokes” (#18). The exact logistic regression model revealed the biggest odds for question #18 where year 1 students had odds more than 13 times those of year 3 students. These results are consistent with studies focusing on dental students or oral hygiene students in other countries. The results for #8 are consistent with those in reports on dental students from Greece[11] and Peru.[15] The results for #18 are also consistent with those from a Colombian study.[16] Another report,[18] which compared dental hygiene and nursing students in Japan showed a significant decrease in “agree” responses to question #18 from dental hygiene students as their courses progressed, whereas there was no difference between first- and final-year nursing students.
Regarding the percentages of “agree” responses to #15, there was a notably low percentage except for the year 1 students at the University of Otago. Based on the responses, oral health students at the two universities studied seem to attend dental offices more frequently when compared with dental hygiene students in Japan,[18] Korea,[17] Jordan,[19] and Saudi Arabia.[20] The percentage of “agree” responses to #9 in all four responding groups was higher than 80%. This result is similar to that of a previous study of Australian dental students.[10] These attitudes may be attributed to cultural differences, socioeconomic backgrounds, personal experiences, and dental health knowledge.
The practical implication of this study is that it may serve as a reference for academic institutions considering the implementation of curricula to prepare mid-level providers into becoming a significant workforce. Although 54 countries, both developed and developing, have adopted this workforce in their societies,[4] controversy still exists over whether mid-level providers are adequately educated and competent to provide the appropriate level of care or not.[21,22] However, one review has clearly stated that mid-level providers have abilities to harmlessly and competently perform a limited set of irreversible dental procedures at least as well as dentists or dental students.[23] Moreover, results obtained in this study recognized that despite the limited 3-year curriculum, some aspects of modification of oral health attitudes and behaviors for oral health students are consistent with those for dental students in other countries.[9,10,11,12,13,14,15,16,19]
Dental disease is a silent epidemic among disadvantaged children, large portions of whom live in poverty or low-income households, as mentioned in the US Surgeon General's report, oral health in America.[24] That report also mentioned tooth decay as the most common chronic disease in these children. The prevalence of dental disease is due to a lack of access to dental services and an insufficient public health infrastructure. Hence, it will become increasing important to provide productive preventive treatment in collaboration with solving the access issue. Mid-level providers who are well-trained through an appropriate educational curriculum will have a significant potential to improve these issues by taking a significant role on the dental team.
CONCLUSIONS
Results from this study in Australia and New Zealand revealed that oral health students who had been educated with a 3-year curriculum had more positive oral health attitudes and behaviors than students who were at the beginning of their course. Well-educated mid-level providers on a dental team can play a key role in alleviating dental care access issues, thus benefiting both individuals and the community.
Financial support and sponsorship
NIH-U54GM104942.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.McGlashan G, Watson DJ, Shanks S. Professionals complementary to dentistry: The expanding role of PCDs. Dent Update. 2004;31:529–32. doi: 10.12968/denu.2004.31.9.529. [DOI] [PubMed] [Google Scholar]
- 2.Coates DE, Kardos TB, Moffat SM, Kardos RL. Dental therapists and dental hygienists educated for the New Zealand environment. J Dent Educ. 2009;73:1001–8. [PubMed] [Google Scholar]
- 3.Satur J. In: A new oral health professional – The oral health therapist. Oral Health Therapy Programs in Australia and New Zealand. Tsang A, editor. Queensland, Australia: Knowledge Books and Software; 2010. pp. 17–26. [Google Scholar]
- 4.Nash DA, Friedman JW, Mathu-Muju KR, Robinson PG, Satur J, Moffat S, et al. A review of the global literature on dental therapists. Community Dent Oral Epidemiol. 2014;42:1–10. doi: 10.1111/cdoe.12052. [DOI] [PubMed] [Google Scholar]
- 5.Tsang AK, Walsh LJ. Oral health students' perceptions of clinical reflective learning – relevance to their development as evolving professionals. Eur J Dent Educ. 2010;14:99–105. doi: 10.1111/j.1600-0579.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 6.Ford PJ, Farah CS. Oral health therapists: What is their role in Australian health care? Int J Dent Hyg. 2013;11:22–7. doi: 10.1111/j.1601-5037.2012.00564.x. [DOI] [PubMed] [Google Scholar]
- 7.Satur J, Moffat S. In: A history of oral health practice (Dental Therapy and Dental Hygiene) in Australia and New Zealand. Oral Health Therapy Programs in Australia and New Zealand. Tsang A, editor. Queensland, Australia: Knowledge Books and Software; 2010. pp. 1–16. [Google Scholar]
- 8.Kawamura M. Dental behavioral science. The relationship between perceptions of oral health and oral status in adults. Hiroshima Daigaku Shigaku Zasshi. 1988;20:273–86. [PubMed] [Google Scholar]
- 9.Komabayashi T, Kwan SY, Hu DY, Kajiwara K, Sasahara H, Kawamura M. A comparative study of oral health attitudes and behaviour using the Hiroshima University – Dental Behavioural Inventory (HU-DBI) between dental students in Britain and China. J Oral Sci. 2005;47:1–7. doi: 10.2334/josnusd.47.1. [DOI] [PubMed] [Google Scholar]
- 10.Kawamura M, Iwamoto Y, Wright FA. A comparison of self-reported dental health attitudes and behavior between selected Japanese and Australian students. J Dent Educ. 1997;61:354–60. [PubMed] [Google Scholar]
- 11.Polychronopoulou A, Kawamura M, Athanasouli T. Oral self-care behavior among dental school students in Greece. J Oral Sci. 2002;44:73–8. doi: 10.2334/josnusd.44.73. [DOI] [PubMed] [Google Scholar]
- 12.Peker I, Alkurt MT. Oral health attitudes and behavior among a group of Turkish dental students. Eur J Dent. 2009;3:24–31. [PMC free article] [PubMed] [Google Scholar]
- 13.Neeraja R, Kayalvizhi G, Sangeetha P. Oral health attitudes and behavior among a group of dental students in Bangalore, India. Eur J Dent. 2011;5:163–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Yildiz S, Dogan B. Self reported dental health attitudes and behaviour of dental students in Turkey. Eur J Dent. 2011;5:253–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Sato M, Camino J, Oyakawa HR, Rodriguez L, Tong L, Ahn C, et al. Effect of dental education on Peruvian dental students' oral health-related attitudes and behavior. J Dent Educ. 2013;77:1179–84. [PMC free article] [PubMed] [Google Scholar]
- 16.Jaramillo JA, Jaramillo F, Kador I, Masuoka D, Tong L, Ahn C, et al. A comparative study of oral health attitudes and behavior using the Hiroshima University-Dental Behavioral Inventory (HU-DBI) between dental and civil engineering students in Colombia. J Oral Sci. 2013;55:23–8. doi: 10.2334/josnusd.55.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawamura M, Spadafora A, Kim KJ, Komabayashi T. Comparison of United States and Korean dental hygiene students using the Hiroshima university-dental behavioural inventory (HU-DBI) Int Dent J. 2002;52:156–62. doi: 10.1111/j.1875-595x.2002.tb00621.x. [DOI] [PubMed] [Google Scholar]
- 18.Kawamura M, Ikeda-Nakaoka Y, Sasahara H. An assessment of oral self-care level among Japanese dental hygiene students and general nursing students using the Hiroshima University – Dental Behavioural Inventory (HU-DBI): Surveys in 1990/1999. Eur J Dent Educ. 2000;4:82–8. doi: 10.1034/j.1600-0579.2000.040206.x. [DOI] [PubMed] [Google Scholar]
- 19.Al-Wahadni AM, Al-Omiri MK, Kawamura M. Differences in self-reported oral health behavior between dental students and dental technology/dental hygiene students in Jordan. J Oral Sci. 2004;46:191–7. doi: 10.2334/josnusd.46.191. [DOI] [PubMed] [Google Scholar]
- 20.Baseer MA, Rahman G, Al Kawaey Z, Al Awamy B, Al Manmeen Z, Al Shalaty F. Evaluation of oral health behavior of female dental hygiene students and interns of Saudi Arabia by using Hiroshima University Dental Behavioural Inventory (HU-DBI) Oral Health Dent Manag. 2013;12:255–61. [PubMed] [Google Scholar]
- 21.Hinson P. Mid-level providers are not in the best interest of children. Pediatr Dent. 2009;31:375–6. [PubMed] [Google Scholar]
- 22.American academy of pediatric dentistry analysis and policy recommendations concerning mid-level dental providers. Pediatr Dent. 2010;32:21–6. [PubMed] [Google Scholar]
- 23.Phillips E, Shaefer HL. Dental therapists: Evidence of technical competence. J Dent Res. 2013;92(7 Suppl):11S–5S. doi: 10.1177/0022034513484333. [DOI] [PubMed] [Google Scholar]
- 24.U U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Reseach, National Institutes of Health. 2000 [Google Scholar]


