Abstract
Objective:
The objective of the study was to evaluate clinically and radiographically the efficacy of platelet-rich fibrin (PRF) versus β-tri-calcium phosphate (β-TCP) in the treatment of Grade II mandibular furcation defects.
Materials and Methods:
Forty-five Grade II furcation defect in mandibular molars which were assigned to open flap debridement (OFD) with PRF Group I (n = 15), to OFD with β-TCP Group II (n = 15), and to OFD alone Group III (n = 15) were analyzed for clinical parameters (probing pocket depth [PPD], vertical clinical attachment level [VCAL], horizontal clinical attachment level [HCAL], gingival recession, relative vertical height of furcation [r-VHF], and relative horizontal depth of furcation [r-HDF]) and radiographical parameters (horizontal depth of furcation [H-DOF], vertical height of furcation [V-HOF]) using cone-beam computed tomography (CBCT) at 6 months interval.
Results:
For clinical parameters, reduction in PPD and gain in VCAL and HCAL were higher in Group II as compared to Group I. Change in r-VHF and r-HDF was greater in Group II as compared to Group I. Mean percentage clinical vertical defect fill was higher in Group II as compared to Group I (58.52% ± 11.68% vs. 53.24% ± 13.22%, respectively). On CBCT, mean change at 6 months for all parameters showed nonsignificant difference between the two experimental groups. Mean change in V-HOF was higher in Group I as compared to Group II, but mean change in H-DOF and furcation width was more in Group II as compared to Group I.
Conclusion:
For both experimental and control groups, there was statistically significant improvement at 6 months follow-up from baseline values.
Keywords: Cone-beam computed tomography, Grade II furcation involvement, periodontal regeneration, platelet-rich fibrin, β-tri-calcium phosphate
INTRODUCTION
The destructive periodontal disease is defined as an inflammatory condition of the primary infectious cause, resulting in marginal alveolar bone resorption and attachment loss. As the destruction of the periodontium progresses apically, the furcation of multirooted teeth is exposed, leading to the irreversible bone loss in the interradicular area.[1] Molar teeth with furcation involvement are the most common teeth to be lost. Various regenerative procedures have been tried with the aim to obtain furcation closure.[2] Autogenous intraoral and extraoral bone, frozen bone allografts, freeze-dried bone allografts, calcium phosphate alloplastics, barrier techniques alone and in combination with bone replacement grafts have been used to regenerate lost periodontal structures in Grade II furcation.[3] Among bone grafts, alloplast hold a great promise as a bone graft material.[4] β-Tri-calcium phosphate (β-TCP) is a crystalline, biocompatible, and osteoconductive material.[5] The material is well tolerated, and until now, no adverse effects such as allergic reactions or rejection of the particles have been reported. The histologic analysis following filling of periodontal defects with β-TCP has provided evidence of bone formation around the particles, thus pointing to the good biocompatibility and osteoconductive properties of the material.[6]
Growth factors are naturally occurring polypeptides, functioning as potent biological mediators which stimulate various cellular activities during wound healing. The application of platelet-rich fibrin (PRF) that contains growth factors in furcation has been proposed to promote periodontal regeneration in humans.[7]
Walter et al.[8] reported that cone-beam computed tomography (CBCT) and intrasurgical assessments of furcation involvement were found to be in substantial agreement and that CBCT enabled the estimation and classification of furcation involvement as well as the visualization of the root morphologies with root proximities or root fusions. The efficacy of CBCT for measuring furcation defect has been validated by several researchers.[9,10,11]
Till now, limited publications have compared PRF and β-TCP for the treatment of Grade II furcation defect with CBCT. Jain et al.,[12] however, use the combination of β-TCP and PRF in a case report. The present study was designed to evaluate the regenerative potential of PRF and β-TCP in the treatment of mandibular Grade II furcation defects and to compare the efficacy of the two materials (β-TCP vs. PRF) clinically and radiographically.
MATERIALS AND METHODS
The present, randomized clinical study was conducted in the Department of Periodontology, Saraswati Dental College, Lucknow, between December 2013 and November 2015, after approval from the Institutional Research and Developmental Committee (IRDC) and Institutional Human Ethics Committee (IHEC) (Reference number SDC/IRDC/2013/MDS-P/27 and SDC/IHEC/2013/MDS-P/27, respectively). Nonsmoker (self-reported), nonalcoholic patients with noncontributory medical history were selected from the pool of Outpatient Department of Periodontology, Saraswati Dental College, Lucknow, India. All patients received complete verbal information regarding the study protocol, and written informed consent was obtained from each patient for participation in the study.
Inclusion criteria
Systemically, healthy patients within the age group 30–50 years suffering from moderate to severe generalized chronic periodontitis
Patient having, at least, one Glickman's buccal Grade II furcation defects in the mandibular first and second molars with ≥3 mm horizontal probing depth
The involved tooth must have gingival margin (GM) coronal to or at the level of the roof of furcation (fornix [Fx])
Patients who had not taken antibiotics or any other drug within 6 months that may modify the result of periodontal therapy
Nonmobile tooth
Adequate RCT must have been completed 3 months before the commencement of the study[13]
Compliant patient with full-mouth plaque score of 0.1–0.9 (good oral hygiene during Phase I therapy).
Study design
For the present clinical study, randomization was conducted with the help of the random selection of sealed envelope having the equal chance of selection. These identical sealed envelopes consisted of one of the three treatment modalities. Envelopes for each treatment modalities were equal in number to avoid heterogeneous sample size. The groups were as follows: Group I, open flap debridement (OFD) and PRF; Group II, OFD and β-TCP; and Group III, OFD alone [Figure 1].
Figure 1.

Flowchart showing study design
Sample size determination: For the present study, sample size (the number of sites treated in each group) was determined using pre hoc analysis with the following method:
n=2x(Zα/2+Zβ)2SD2/d2 (where n: Sample size per group; SD: Pooled standard deviation being 0.5 in this; d: Difference in the means [effect size]; Zα/2: Significance level, Zβ: power of the study).
Assuming 80% power, 5% significance level with 95% confidence interval, as well as assuming standard 0.50, the minimum required sample size per group was n = 11 sites. The minimal sample size of 13 sites in each group was advocated, assuming 20% loss during follow-up. For the present study, a total of fifty patients were initially enrolled in the study. After Phase I therapy, a total of 37 patients (10 female, 27 male) with 51 sites (17 each) were finally randomly assigned to receive either experimental or control treatment modalities.
Platelet-rich fibrin
Autologous PRF was obtained from patient's blood as suggested by Dohan et al.[14] using a table top centrifuge (REMI, Laboratories, India). PRF acquired in the middle clot was cautiously collected by removing RBC clot using sterilized scissor [Figure 2].[15] The centrifuge machine was kept closed to the operator, and all efforts were made to minimize the time between the preparation of PRF and its placement into the defect so as to retain maximum regenerative potential.[15]
Figure 2.

Platelet-rich fibrin procured
β-tri-calcium phosphate
Commercially available β-TCP is synthetic β-TCP granules (RTR Syringe, Septodont, and Quigley Boulevard – New Castle, USA). RTR syringe is a curved syringe containing 0.8 cm3 of β-TCP granules (particle size between 500 μm and 1 mm) in individual sterile packaging.[16]
Methodology
Initial therapy (nonsurgical therapy)
Patients meeting the selection criteria were selected and put on nonsurgical therapy of scaling and root planing including the oral hygiene instructions. After the completion of Phase I therapy, the motivated and compliant patients were scheduled for surgical phase. CBCT was taken as baseline radiographic assessment before surgery.
Stent preparation
On the follow-up visit, a diagnostic cast was prepared, and acrylic stent was made with pink and clear acrylic by the sprinkle-on method for both the test and control sites.[17] A hole in the horizontal direction approximately at the level of furcation entrance was made on the clear stent. The stent was used as the standardized, reproducible landmark to record the horizontal depth of furcation (H-DOF) at the follow-up interval [Figure 3]. In pink occlusal stent, a vertical groove was prepared at the middle of the tooth on stent to guide placement of the probe [Figure 4]. Stents were preserved with cast itself throughout the study. Disinfection of stent was done before every clinical measurement by immersion of stent in 0.525% sodium hypochlorite for 10 min.[18]
Figure 3.

Clear acrylic resin occlusal stent with hole in horizontal direction
Figure 4.
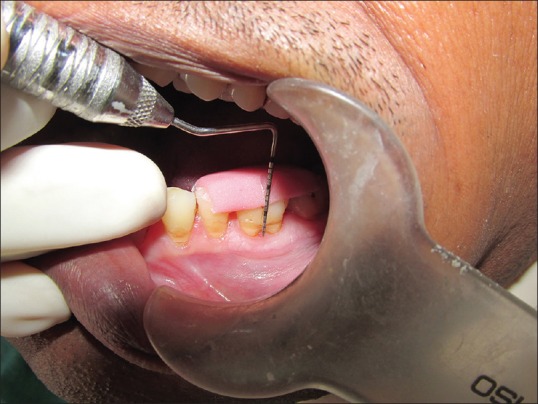
Pink occlusal acrylic stent with vertical groove
Surgical procedure
On the day of surgery, all baseline parameters were measured using prefabricated acrylic stent. A presurgical mouth rinse was performed using 10 ml of 0.2% chlorhexidine gluconate (hexidine 0.2% ICPA, India) solution. Swabbing of the extraoral face with 5% povidone-iodine solution (Betadine) was done. After administration of local anesthesia using xylocaine 2% with adrenaline 1:200,000, a sulcular incision (#15 blade) was made on the buccal and lingual aspect of one tooth distal and mesial to the involved tooth, and full thickness flap was raised by blunt dissection using periosteal elevator retaining sufficient tissue to attain primary closure. The furcation defects were thoroughly scaled and root planed with curettes (Quentin furcation curette) and ultrasonic scalers. Following the removal of granulation tissue and thorough debridement, enamel projections if noted were removed with rotary instruments. Following surgical debridement, the acrylic stent was placed, and clinical parameters were recorded. Prepared recipient site was randomly assigned to treatment modality as explained above.
For experimental Group I, procured PRF was inserted, squeezed, and adapted into the defect. The fluid obtained after squeezing was thus confined to the operated site [Figure 5].
Figure 5.

Group I; open flap debridement with platelet rich fibrin
For experimental Group II, the appropriate amount of graft material was taken in sterile-dappen dish. β-TCP was carried in a graft carrier and directly placed into the furcation defect and condensed in place to a level of the plane connecting the eminence of the root surface adjacent to the furcation defect. Small increments were added and condensed with an instrument until the defect was filled. Care was taken not to overfill the defect beyond the eminence plane [Figure 6].
Figure 6.

Group II; open flap debridement with β-tri-calcium phosphate
For control Group III, defects were thoroughly debrided and left as such for natural healing without adding any graft material [Figure 7].
Figure 7.

Group III; open flap debridement alone
The periodontal flap was repositioned back, and primary soft tissue closure was done with direct loop interrupted sutures using nonresorbable black silk suture (4-0). A periodontal dressing (Coe-Pak) was placed on the surgical area. After surgery, all the patients were prescribed systemic antibiotics amoxicillin 500 mg thrice daily and ibuprofen 400 mg 2 times a day for 5 days, and postoperative written instructions were given to all the patients. Patients were instructed to report to the department after 10 days. Coe-Pak and suture removal were done carefully without disturbing the healing soft tissue, and the surgical area was irrigated with normal saline. Supragingival scaling was done if required. During this period, plaque control was achieved with a 0.2% chlorhexidine solution rinse twice a day. Patients were recalled at monthly interval and oral hygiene instructions were reinforced. At 6 months postsurgery, clinical (soft tissue and hard tissue measurement) and radiographical measurements were taken.
Clinical parameters
Prameters recorded at baseline and 6 months were plaque index: Silness and Löe[19] and gingival index: Loe and Silness.[20]
Soft tissue measurements
Clinical measurements were recorded with the help of a University of North Carolina-15 (UNC-15) probe and Nabers probe for each surgical site at baseline before flap reflection and 6-month postsurgery. The apical end of the vertical groove of the stent was used as fixed reference point (FRP).
FRP to base of the pocket (BOP)
FRP to cementoenamel junction (CEJ).
FRP to gingival margin (GM).
The following clinical parameters were deducted from the clinical measurements recorded.
Probing pocket depth (PPD): PPD = (FRP to BOP) − (FRP to GM)
Vertical clinical attachment level (VCAL): VCAL = (FRP to BOP) − (FRP to CEJ)
Horizontal clinical attachment level (HCAL): It was calculated with the help of Nabers probe
Gingival recession (GR): GR = (FRP to GM) − (FRP to CEJ).
Clinical hard tissue parameters
Hard tissue measurements were taken at baseline during surgery (intrasurgical) and at 6 months postsurgery through bone sounding or transgingival probing method under local anesthetic infiltration.
Relative vertical height of furcation
To calculate relative vertical height of furcation (r-VHF), initially, the levels of fornix (Fx) and base of furcation defect (BOD) were recorded from FRP during surgery and deducted the distance between the FRP to base of furcation defect (BOD) and FRP to Fx of the furcation defect. Clinical vertical defect fill (c-VDF) was finally deducted from the difference between baseline and 6 months r-VHF. Percentage of mean change in r-VHF (percentage c-VDF [% c-VDF]) was calculated from the difference between baseline and 6 months value divided by baseline value.
Relative horizontal depth of furcation
It was recorded by horizontal probing with the UNC-15 probe and rubber stopper from a FRP on a clear acrylic stent at baseline after reflection. Six months postsurgery, transgingival probing was done with the UNC-15 probe under local anesthesia. By calculating the difference between baseline and 6-month measurements, clinical horizontal defect fill (c-HDF) was finally deducted. Percentage of mean change in relative horizontal depth of furcation (r-HDF) (percentage c-HDF [% c-HDF]) was calculated from the difference between baseline and 6 months value divided by baseline value.
Radiographic parameters
Cone-beam computed tomography
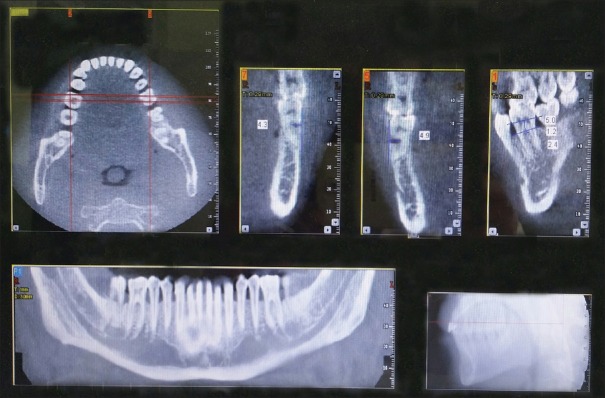
For the present study, high-resolution CBCT (Newtom 3G Cone Beam X-ray Technology QR DVT 9000 SRL, AFP Imaging Company, Verona, Italy) with large field of view (FORmax of 20 cm × 20 cm × 20 cm) equipped with three-dimensional image reconstruction software package (NNT Version 2.499, QR SRL, VERONA ITALY) was used for CT scanning and image reconstruction installed at the Department of Oral Medicine and Radiology, Faculty of Dental Sciences, King George Medical University, Lucknow. Data were captured in high resolution of 0.4 mm voxel size with the exposure time of 20 s scanning (110 kVp, 2.6 mAs) in the sagittal and coronal sections with the constant slice thickness of 1 mm [Figure 8]. The present study used 1.0 mm thick slices as this increment closely mimics the same error of measurement when using a manual periodontal probe and because smaller slices decreased the image resolution.[21]
Figure 8.
Cone-beam computed tomography data record
Standardization of radiographic technique
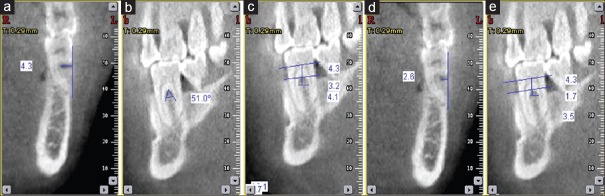
All the CBCT scans were taken by a single trained technician pre- and post-surgery. A calibration exercise was performed to obtain accruable intraexaminer consistency in CBCT measurements. The voltage, current, exposure time, and detection field were kept constant for each patient at both the time of exposure. The reference chosen to standardize the axial and sagittal planes was the bispinal line, coinciding with the vertical and horizontal planes, respectively.[21] The sagittal and coronal sections were reconstructed after 6 months at the same axial slicing to that of the baseline. The following calculations were made from the coronal and sagittal sections of CBCT at baseline and 6 months postsurgery [Figure 9].
Figure 9.
(a) Cone-beam computed tomography image showing coronal section at baseline measuring depth horizontal of furcation, (b) cone-beam computed tomography image showing sagittal section at baseline measuring furcation angle, (c) cone-beam computed tomography image showing coronal section at baseline measuring vertical depth of furcation, (d) cone-beam computed tomography image showing coronal section at 6 months measuring depth horizontal of furcation, (e) cone-beam computed tomography image showing coronal section at 6 months measuring vertical depth of furcation
Coronal section of cone-beam computed tomography
Horizontal depth of furcation
The perpendicular distance in the furcation area from the tangent connects the most prominent portion of tooth crown and the buccal cortical plate. By calculating the difference between baseline and 6-month measurements, HDF was finally deducted. Percentage of mean change in H-DOF (percentage HDF [% H-DF]) was calculated from the difference between baseline and 6 months value divided by baseline value.
Sagittal section of cone-beam computed tomography
Vertical height of furcation
It was the distance between the Fx to the crest of alveolar bone within the furcation. By calculating the difference between baseline and 6-month measurements, VDF was finally deducted. Percentage of mean change in vertical height of furcation (V-HOF) (% V-DF) was calculated from the difference between baseline and 6 months value divided by baseline value.
Furcation width (Fw)
It refered to width of the furcal orifice at its base, measured in a horizontal dimension at the level of the alveolar crest within the furcation.
Root trunk length (RTL)
It was the distance calculated from the CEJ line to the Fx.
Furcation angle (FA)
It was the angle formed at the Fx of the furcation describing root separation.
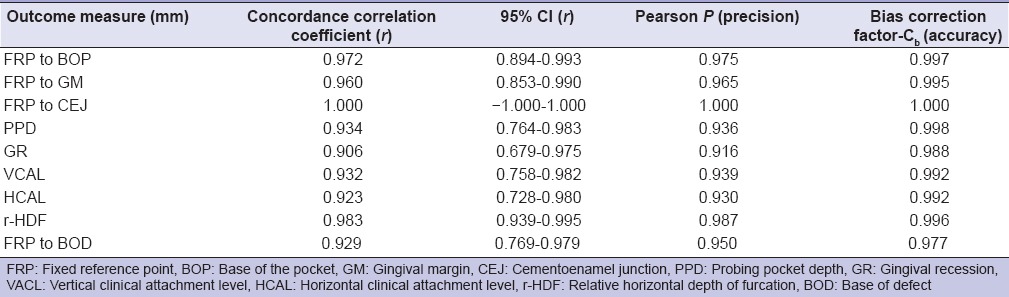
Intraobserver reliability
Before evaluating outcome measures, the reliability of outcome measures (FRP to BOP, FRP to GM, FRP to CEJ, PPD, GR, VCAL, HCAL, and r-HDF) was first checked. The measurement of each outcome was assessed twice, within 24 h, with at least 1 h between the examination,[22] and reliability of two measurements was compared by concordance correlation analysis. The concordance analysis showed high correlation (0.906–1.000) between the measurements in all outcome measures with high precision (92–100%) and accuracy (99–100%), indicating high intraobserver reliability [Table 1].
Table 1.
Intraobserver reliability of outcome measures using concordance correlation analysis (n=10)
Statistical analysis
Data were summarized as mean ± standard deviation. Groups were compared by one-way analysis of variance (ANOVA) and repeated measures two-way ANOVA, and the significance of mean difference within (intra) and between (inter) the groups was done by Tukey's post hoc test after ascertaining normality by Shapiro–Wilk's test and homogeneity of variance between groups by Levene's test. Categorical (discrete) groups were compared by Chi-square test. Pearson correlation analysis was done to assess the association between the variables. Concordance correlation analysis was done to assess intraobserver reliability. A two-tailed P < 0.05 was considered statistically significant. All analyses were performed on SPSS software (Statistics for Windows, Version 17.0. Chicago: SPSS Inc.). The relative association between two variables (X and Y) was calculated according to Karl Pearson correlation coefficient (r) method.
RESULTS
A total of 37 patients (10 females and 27 males) fulfilling the inclusion criteria were initially enrolled for the study. Among them, three male and three female patients were noncompliant and never reported after the surgical procedure. Consequently, a total of 24 male and 7 female patients completed the study, and 45 furcation sites were analyzed.
Demographic characteristics
The demographic characteristics, namely, age, gender, and tooth used for the treatment of three groups are summarized in Table 2. Comparing the gender proportions (M/F) of three groups, the Chi-square test showed similar frequency (%) of males and females among the two groups (χ2 = 0.00, P = 1.000), i.e. also not differed significantly.
Table 2.
Demographic characteristics of three groups

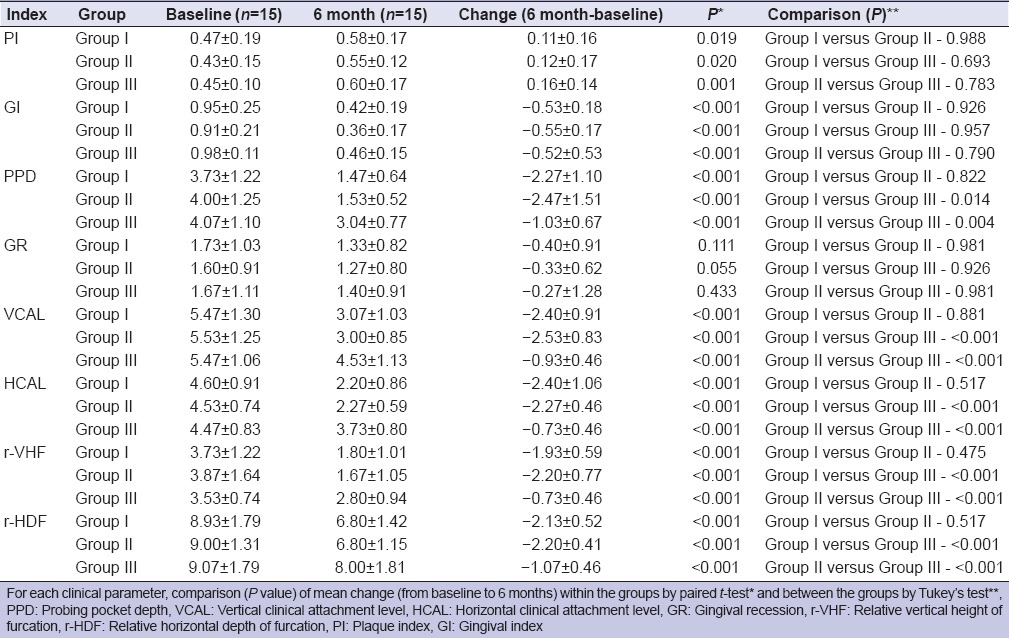
Clinical parameters
The baseline and 6-month follow-up periodontal health parameters score of three groups are summarized in Table 3. The % c-VDF was highest in Group II (58.52% ± 11.68%), followed by Group I (53.24% ± 13.22%) and Group III (21.89% ± 14.31%). The % c-HDF of Group I (51.78% ± 17.05%) was the highest, followed by Group II (50.44% ± 8.34%) and Group III (16.22% ± 10.55%).
Table 3.
Clinical values of three groups at baseline and 6 months
Radiographic parameters
Radiographic evaluation using CBCT is summarized in Table 4.
Table 4.
Radiographic values of three groups at baseline and 6 months

The mean root trunk length (RTL) of Group III was the highest, followed by Group II and Group I. The mean furcation angle (FA) of Group III was the highest, followed by Group I and Group II. Comparing the mean FA of three groups, Tukey's test showed similar (P > 0.05) FA among the groups, i.e. did not differ significantly. The mean baseline value of furcation width (Fw) in Group I was 3.97 ± 0.49 mm, Group II was 3.95 ± 0.52 mm, and Group III was 4.03 ± 0.67 mm, and the difference between the groups was statistically nonsignificant. The mean Fw in all group decreased significantly at 6-month follow-up. However, the decrease was highest in Group II (1.85 ± 0.46 mm), followed by Group I (1.73 ± 0.66 mm) and Group III (0.56 ± 0.33 mm).
Correlation of furcation angle with vertical height of furcation and furcation width
The correlation between FA at 6 months and change (6 months-baseline) in VHF and Fw of each group is summarized in Table 5. The Pearson correlation analysis showed negative (inverse) or positive (direct), but the insignificant correlation between change in Fw and V-HOF with FA in all groups, indicating the change in both V-HOF and Fw did not associate with FA.
Table 5.
Correlation of root trunk length with vertical height of furcation with furcation width and vertical height of furcation with furcation angle in three groups (n=15)
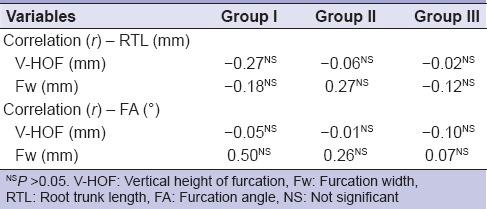
Correlation of root trunk length with vertical height of furcation and furcation width
The correlation of change (6 months-baseline) in V-HOF and Fw with RTL of each group is summarized in Table 5. The Pearson correlation analysis showed negative (inverse) or positive (direct), but the insignificant correlation between change in FA and V-HOF with RTL in all groups, indicating the change in both V-HOF and Fw did not associate with RTL.
DISCUSSION
The primary outcome of the study revealed defect fill in Class II/Grade II furcation defects in all the groups when evaluated clinically and radiographically. However, the test groups, i.e. Group I: OFD and PRF and Group II: OFD and β-TCP revealed significant changes as compared to control group (OFD alone).
Mean PPD, GR, and VCAL variability among three groups observed at baseline were nonsignificant. However, there was the significant decrease in PPD, GR, and gain in VCAL at 6 months in all three groups. Mean change in PPD and VCAL was highest in Group II, followed by Group I and Group III. The mean 6 months in GR was highest in Group I as compared to Group II and Group III at 6 months follow-up as compared to baseline values. Sharma and Pradeep[23] and Peres et al.[22] also observed significant PPD reduction as well as gain in CAL in Class II/Grade II furcation defects treated with OFD and PRF as compared to OFD alone.
Mean change in the value of the r-VHF, i.e. c-VDF was statistically significant between Group I versus Group III and between Group II versus Group III. However, the nonsignificant difference was found between Groups I and II. Mean % c-VDF was statistically significant between Group I versus Group III and between Group II versus Group III. However, the nonsignificant difference was found between Group I and Group II. Similar to the present study, Pepelassi et al.[24] advocated mean change in V-HOF of 2.31 ± 1.77 mm using doxycycline-tri-calcium phosphate composite graft at 6 months in the treatment of Class II/Grade II furcation defect. Peres et al.[22] measured mean change in relative vertical bone level (rVBL) of 1.47 ± 1.13 mm at 6 months follow-up, with HA/β-TCP in the treatment of proximal Class II/Grade II furcation defect. On comparing the r-HDF at baseline and 6 months, the significant decrease was found in all groups, and the decrease was highest in Group I, followed by Groups II and III.
The assessment of radiographic hard tissue parameters such as RTL, V-HOF (radiographic distance from Fx to alveolar crest), Fw (horizontal root separation at alveolar crest), H-DOF, and FA was done with CBCT. To evaluate and correlate the influence of RTL and FA on defect fill of furcation, the present study recorded RTL and FA at baseline. After 6-month follow-up, a significant decrease in V-HOF, i.e. VDF was observed in all groups, and the defect fill was highest in Group I, followed by Group II and Group III. Sharma and Pradeep[23] and Bajaj et al.[25] reported almost similar and significant mean bone defect depth fill and % VDF in PRF-treated group when observed radiographically (intraoral periapical radiograph) with computer-aided software in the treatment of mandibular degree II furcation defect. In contrast to above-mentioned studies, we utilized CBCT for measurement of vertical bone loss. Based on the view of Walter et al.,[8] results of the present study may demonstrate more accuracy in assessing the furcation defect analysis as compared to the previous study. At 6 months, a significant decrease in H-DOF, i.e. H-DF was seen in all groups and the defect fill was highest in Group II, followed by Group I and Group III.
To the best of our knowledge, no publication till now has reported HDF and association of FA with V-HOF and Fw in Class II/Grade II mandibular furcation defect using either PRF or β-TCP using CBCT. Asmita et al.[21] reported HDF in Class II mandibular furcation using two different forms of bioactive glass. The Pearson correlation analysis showed no association between RTL and FA on mean change in V-HOF and Fw when recorded on CBCT. Nonsignificant baseline mean value of RTL and FA, as well as low sample size, may attribute to this nonsignificant correlation. Horwitz et al.[26] in their study on Class II furcation defect stated that a long root trunk and a wide furcation entrance have negative influences on the success of therapy.
Unlike α-TCP, β-TCP is completely resorbed simultaneously with bone formation and is replaced by vital host bone without residue within 6–12 months. Further, local decrease in pH during the dissolution of material or direct chemical bonding of β-TCP with the bone through a reaction between calcium ions in the β-TCP particle, thus minimizes the use of barrier membrane.[27] For the present study, commercially available synthetic bone alloplastic resorbable tissue replacement was used that is extremely hydrophilic in nature. It can be drawn into the surgical site and could easily be contoured to fill any bony void, thus making it ideal for the treatment of furcation defects.
For the present study, no surgical reentry and histological examination were considered to confirm the quality of bone formation in experimental (PRF or β-TCP treated) and control sites. Radiographic interpretation using CBCT although is not a perfect method yet can be considered reliable mean for evaluation of furcation defects.[8,28] Even then, natural healing in the control group, accelerated bone healing in PRF-treated group, and scaffold-assisted bone healing in β-TCP treated group cannot be completely ascertained. Further, in β-TCP-treated sites, results (defect fill) may be influenced by radiopaque nature of graft material as well as the inconsistent rate of resorption of β-TCP granules (from 3 months up to 12 months) as high mechanical stability may prevent premature degradation of granules into microparticles and inhibit undesirable macrophage activity.
To the best of our knowledge, only Asmita et al.[21] had utilized CBCT for evaluating and recording above-mentioned parameters of the study. Most studies reported mean percentage defect fill on conventional and digital radiography using computer-aided program.[23,25] Till date, this study is the first prospective, randomized controlled clinical study that compared the regenerative potential of PRF and β-TCP in the management of Glickman's buccal Class II/Grade II mandibular furcation defects in terms of defect fill (horizontal depth, vertical height, and Fw) using CBCT. The present study demonstrated better result for both experimental groups (OFD with PRF and OFD with β-TCP) regarding probing depth reduction and clinical attachment level gain (VCAL and HCAL) as compared to OFD alone.
PRF-treated sites represented stabilized level of GM throughout the study. Statistically, significant improvement in V-HOF, H-DOF, and percentage defect fill was observed on CBCT analysis. Fibrin clot derived of PRF stimulates the high level of collagen type I synthesis and consists of the intimate assembly of cytokine, glycan chain, and structural glycoprotein enmeshed within a slowly polymerized explicit fibrin network. When placed in the periodontal defect, this meshwork acts as a bioscaffold with an integrated reservoir of growth factors which are released over prolonged periods, thus enhancing the regenerative potential of the surrounding tissues.[12]
The data from present study suggest that both experimental groups (OFD with PRF and OFD with β-TCP) result in significant improvement in hard tissue parameters, clinically and radiographically, compared with baselines values and as observed in control group (OFD alone). Hence, both experimental treatment modalities (OFD with PRF and OFD with β-TCP) might be an option for the treatment of mandibular Class II/Grade II furcation defects since both were capable of promising gain for all clinical and radiographical parameters evaluated although no predictable complete closure could be attributed to any therapy. Use of PRF in the periodontal regeneration procedure would be cost-effective and being autologous, more acceptable by the body, thus, would be better for both patient as well as clinicians.
Limitations
Small sample size in each group, lack of histomorphometric analysis of newly formed tissues, and short-term follow-up of 6 months were the drawbacks of the present study as 6 months is not enough time for β-TCP resorption. In addition, clinical hard tissue parameters were recorded as by different methods for two study periods. Further, results of the present study cannot be generalized for all furcation defects as we have discussed only mandibular tooth. Being single-centered study, morphological deviations in Fw, FA, and RTL due to geographic/genetic variations may influence the outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marcaccini AM, Pavanelo A, Nogueira AV, Souza JA, Porciúncula HF, Cirelli JA. Morphometric study of the root anatomy in furcation area of mandibular first molars. J Appl Oral Sci. 2012;20:76–81. doi: 10.1590/S1678-77572012000100014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jepsen S, Eberhard J, Herrera D, Needleman I. A systematic review of guided tissue regeneration for periodontal furcation defects. What is the effect of guided tissue regeneration compared with surgical debridement in the treatment of furcation defects? J Clin Periodontol. 2002;29(Suppl 3):103–16. doi: 10.1034/j.1600-051x.29.s3.6.x. [DOI] [PubMed] [Google Scholar]
- 3.Yukna RA. Clinical evaluation of HTR polymer bone replacement grafts in human mandibular Class II molar furcations. J Periodontol. 1994;65:342–9. doi: 10.1902/jop.1994.65.4.342. [DOI] [PubMed] [Google Scholar]
- 4.Saini N, Sikri P, Gupta H. Evaluation of the relative efficacy of autologous platelet rich plasma in combination with β-TCP alloplast versus an alloplast alone in the treatment of human periodontal intrabony defects. A clinical and radiological study. Indian J Dent Res. 2011;22:107–15. doi: 10.4103/0970-9290.80008. [DOI] [PubMed] [Google Scholar]
- 5.Döri F, Arweiler NB, Szántó E, Agics A, Gera I, Sculean A. Ten-year results following treatment of intrabony defects with an enamel matrix protein derivative combined with either a natural bone mineral or a ß-tricalcium phosphate. J Periodontol. 2013;84:749–57. doi: 10.1902/jop.2012.120238. [DOI] [PubMed] [Google Scholar]
- 6.Das S, Jhingran R, Bains VK, Madan R, Srivastava R, Rizvi I. preservation by beta-tri-calcium phosphate with collagen compared to platelet-rich fibrin: A clinico-radiographic study. Eur J Dent. 2016;10:264–76. doi: 10.4103/1305-7456.178298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park JB, Matsuura M, Han KY, Norderyd O, Lin WL, Genco RJ, et al. Periodontal regeneration in class III furcation defects of beagle dogs using guided tissue regenerative therapy with platelet-derived growth factor. J Periodontol. 1995;66:462–77. doi: 10.1902/jop.1995.66.6.462. [DOI] [PubMed] [Google Scholar]
- 8.Walter C, Weiger R, Zitzmann NU. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol. 2010;37:436–41. doi: 10.1111/j.1600-051X.2010.01556.x. [DOI] [PubMed] [Google Scholar]
- 9.Fuhrmann RA, Bücker A, Diedrich PR. Furcation involvement: Comparison of dental radiographs and HR-CT-slices in human specimens. J Periodontal Res. 1997;32:409–18. doi: 10.1111/j.1600-0765.1997.tb00553.x. [DOI] [PubMed] [Google Scholar]
- 10.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 11.Laky M, Majdalani S, Kapferer I, Frantal S, Gahleitner A, Moritz A, et al. Periodontal probing of dental furcations compared with diagnosis by low-dose computed tomography: A case series. J Periodontol. 2013;84:1740–6. doi: 10.1902/jop.2013.120698. [DOI] [PubMed] [Google Scholar]
- 12.Jain S, Mohan R, Karthik KM, Janardhana AB. Platelet rich fibrin and β-TCP for the treatment of grade II furcation defects. A case report. J Dent. 2014;1:20–3. [Google Scholar]
- 13.Parolia A, Gait TC, Porto IC, Mala K. Endo-perio lesion: A dilemma from 19th until 21st century. J Interdiscip Dent. 2013;3:2–11. [Google Scholar]
- 14.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal SK, Jhingran R, Bains VK, Srivastava R, Madan R, Rizvi I. Patient-centered evaluation of microsurgical management of gingival recession using coronally advanced flap with platelet-rich fibrin or amnion membrane: A comparative analysis. Eur J Dent. 2016;10:121–33. doi: 10.4103/1305-7456.175686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [Last accessed on 2016 Jul 28]. Available from: http://www.septodont.com.hr/pdf/rtr_apolonia.pdf .
- 17.Khanna D, Malhotra S, Naidu DV. Treatment of grade II furcation involvement using resorbable guided tissue regeneration membrane: A six-month study. J Indian Soc Periodontol. 2012;16:404–10. doi: 10.4103/0972-124X.100920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chau VB, Saunders TR, Pimsler M, Elfring DR. In-depth disinfection of acrylic resins. J Prosthet Dent. 1995;74:309–13. doi: 10.1016/s0022-3913(05)80140-4. [DOI] [PubMed] [Google Scholar]
- 19.Silness J, Löe H. Periodontal disease in pregnancy 3. Response to local treatment. Acta Odontol Scand. 1966;24:747–59. doi: 10.3109/00016356609028739. [DOI] [PubMed] [Google Scholar]
- 20.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 21.Asmita, Gupta V, Bains VK, Singh GP, Jhingran R. Clinical and cone beam computed tomography comparison of NovaBone Dental Putty and PerioGlas in the treatment of mandibular class II furcations. Indian J Dent Res. 2014;25:166–73. doi: 10.4103/0970-9290.135912. [DOI] [PubMed] [Google Scholar]
- 22.Peres MF, Ribeiro ED, Casarin RC, Ruiz KG, Junior FH, Sallum EA, et al. Hydroxyapatite/ß-tricalcium phosphate and enamel matrix derivative for treatment of proximal class II furcation defects: A randomized clinical trial. J Clin Periodontol. 2013;40:252–9. doi: 10.1111/jcpe.12054. [DOI] [PubMed] [Google Scholar]
- 23.Sharma A, Pradeep AR. Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: A randomized controlled clinical trial. J Periodontol. 2011;82:1705–12. doi: 10.1902/jop.2011.110075. [DOI] [PubMed] [Google Scholar]
- 24.Pepelassi EM, Bissada NF, Greenwell H, Fara CF. Doxycycline-tricalcium phosphate composite graft facilitates osseous healing in advance periodontal furcation defects. J Periodontol. 1991;62:106–15. doi: 10.1902/jop.1991.62.2.106. [DOI] [PubMed] [Google Scholar]
- 25.Bajaj P, Pradeep AR, Agarwal E, Rao NS, Naik SB, Priyanka N, et al. Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of mandibular degree II furcation defects: A randomized controlled clinical trial. J Periodontal Res. 2013;48:573–81. doi: 10.1111/jre.12040. [DOI] [PubMed] [Google Scholar]
- 26.Horwitz J, Machtei EE, Reitmeir P, Holle R, Kim TS, Eickholz P. Radiographic parameters as prognostic indicators for healing of class II furcation defects. J Clin Periodontol. 2004;31:105–11. doi: 10.1111/j.0303-6979.2004.00455.x. [DOI] [PubMed] [Google Scholar]
- 27.Brkovic BM, Prasad HS, Konandreas G, Milan R, Antunovic D, Sandor GK, et al. Simple preservation of maxillary extraction socket using β-TCP with type I collagen: Preliminary clinical ad histomorphometric observations. J Can Dent Assoc. 2008;74:513–8. [PubMed] [Google Scholar]
- 28.Ito K, Yoshinuma N, Goke E, Arai Y, Shinoda K. Clinical application of a new compact computed tomography system for evaluating the outcome of regenerative therapy: A case report. J Periodontol. 2001;72:696–702. doi: 10.1902/jop.2001.72.5.696. [DOI] [PubMed] [Google Scholar]