Abstract
Objective:
The purpose of this study was to compare the dental and skeletal effects of canine retraction using conventional anchorage reinforcement systems and comparing them with the usage of TADs.
Materials and Methods:
The sample consisted of 50 patients having Class I malocclusions with bimaxillary protrusion indicated for first premolar extraction, and allocated into two groups. The first group consisted of 25 patients with a mean age of 18,7 years (min:14, max:22 years, 16 girls and 9 boys) that TADs were applied as an anchorage mechanic between attached gingiva of upper second premolar and first molar teeth. The second group consisted of 25 patients with a mean age of 19,4 years (min:15, max:23 years, 14 girls and 11 boys) that conventional molar anchorage with Transpalatal arch (TPA) was applied for the anchorage mechanics against canine retraction.
Results:
The results showed that mean mesial movement and the tipping of the first molars in TAD group between T0 - T1 were insignificant (P > 0,05), however in the TPA group were significant (P<0,01). Vertical movement of the molars were not significant when two groups were compared (P>0,05).
Conclusion:
Although TPA is a useful appliance, it doesn't provide an effective anchorage control on anteroposterior movement maxillary first molar teeth concerning first premolar extraction treatment. TADs are more convenient to provide absolute anchorage during maxillary canine retraction in contrast to transpalatal arch.
Keywords: Absolute anchorage, miniscrews, temporary anchorage devices, transpalatal arch
INTRODUCTION
The need of absolute anchorage with traditional approaches is a biomechanical challenge. The main orthodontic malocclusions that require maximum anchorage for premolar extraction are severe crowding and protrusion.[1,2,3,4] Extraction of permanent teeth to set the occlusion to Class I is a routine approach in orthodontic treatment.[5,6] Achieving maximum or absolute anchorage is the most important strategy among the systems minimizing the anchorage loss during space closure.[7,8] Anterior retraction is applied with specific mechanics and control mechanisms.[9] Recently, temporary anchorage devices (TADs) such as miniscrews, mini-implants, and miniplates have been introduced in orthodontic practice as absolute anchorage mechanics.[10,11,12]
Studies showed that bone anchorage treatments showed less anchorage loss than tooth anchorage mechanics.[1,13] Over the past 60 years, skeletal anchorage systems showed a variety of design, material, and placement locations.[14]
Miniscrews are applied for many treatment modalities such as the corrections in the anteroposterior dimension such as retraction, protraction, distalization,[15,16,17,18] and in the vertical dimension such as openbites, vertical control in high-angle patients, intrusion and extrusion of the teeth, deepbite, and canted occlusal planes.[19,20,21,22,23]
The purpose of the study is to determine the anchorage potential of TADs for canine retraction during space closure and compare and evaluate the amount of anchorage loss and the movement of molars during canine retraction in Class I dentoalveolar protrusion.[13,24,25]
MATERIALS AND METHODS
This retrospective study was designed to evaluate the effects of TADs as an absolute anchorage compared to conventional molar-anchored canine retraction. A total of fifty patients were selected having a Class I malocclusion with a treatment indication of bilateral maxillary first premolar extraction; and they were divided into two groups. The first group consisted of 25 patients with a mean age of 18.7 years (ranged 14–22 years; 16 girls and 9 boys) to whom TADs were applied as an anchorage mechanic between the attached gingiva of the upper second premolar and first molar teeth. The second group consisted of 25 patients with a mean age of 19.4 years (ranged 13–23 years; 14 girls and 11 boys), in whom conventional molar anchorage was reinforced with a transpalatal arch (TPA). The first molar bands were soldered to a transpalatal bar constructed on the plaster models, and the TPA is applied to the upper first molar teeth. All the patients were treated by the same orthodontist with 0.022” Roth-prescribed brackets.
Among the patients who have completed their fixed orthodontic treatment, the inclusion criteria were as follows: (1) Patients without any craniofacial deformity and systemic diseases, (2) having a malocclusion requiring first premolar extraction, (3) maximum anchorage need for space closure, (4) angle Class I malocclusion with anterior protrusion with an ANB angle of maximum 4° and minimum of 1°. The treatment schedules of all the selected patients were inspected, and the patients who received the standardized treatment protocol were chosen for this study. According to the treatment protocol, TADs had been placed between the upper second premolar and first molar teeth on the attached gingiva following leveling and aligning of the dental arch. Fifteen days after the implant placement, 9 mm closed Ni–Ti coil springs had been applied between the upper canine bracket and TAD on the 0.019 × 0.025” stainless steel arch to provide a continuous force of 150 g on a bracket slot of 0.022” with Roth's prescription. TPAs had been constructed on the plaster models and applied after the initial leveling and aligning of the upper arch.
Lateral cephalometric analysis
The landmarks and the cephalometric points, planes, and measurements are shown and described in Figure 1.
Figure 1.
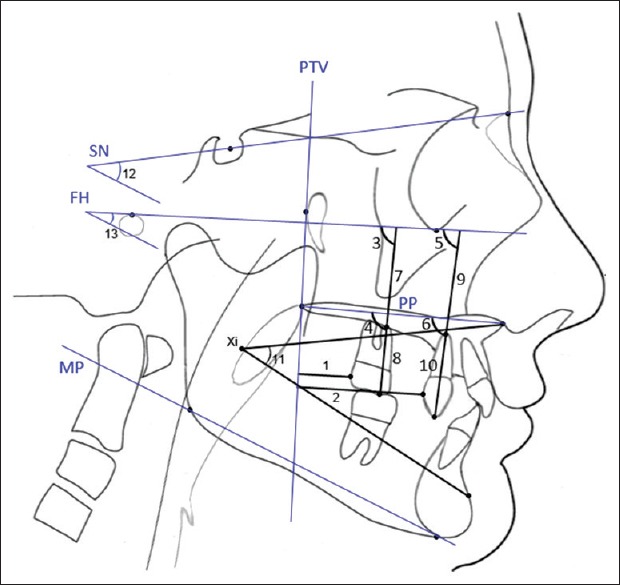
Lateral cephalometric analysis: (1) The distance between the upper molar and pterygoid vertical plane (U6 – pterygoid vertical plane distance); (2) the distance between the upper canine and pterygoid vertical plane (U3 – pterygoid vertical plane distance); (3) upper molar inclination (U6 - Frankfort horizontal angle); (4) upper molar inclination (U6 - PP angle); (5) upper canine inclination (U3 - Frankfort horizontal angle); (6) upper canine inclination (U3 - PP angle); (7) upper molar extrusion (U6 - Frankfort horizontal distance); (8) upper molar extrusion (U6 to PP distance); (9) upper canine extrusion (U3 - Frankfort horizontal distance); (10) upper canine extrusion (U3 - PP distance); (11) ANS-Xi-Pm; (12), Go-Gn-SN; (13) FMA
Statistical analysis
Pre- and post-treatment measurements were performed twice 2 weeks apart by the same examiner via the same digitizing software. Paired sample t-test was applied to measure the difference between the two measurements of the randomly selected twenty cephalograms, no significant difference was found (P > 0.05), and the values ranged between 0.86 and 0.94 in the accepted limits.
The normality of data was checked in two groups and the data were nonsignificant, thus a parametric statistical analysis was performed. The pre- and post-treatment comparisons within the same group were performed via paired sample t-test. The comparisons of TAD and TPA groups were analyzed via independent sample t-test via Statistical Package for Social Sciences (SPSS) Version 22.0 (IBM Corp, NY, USA).
RESULTS
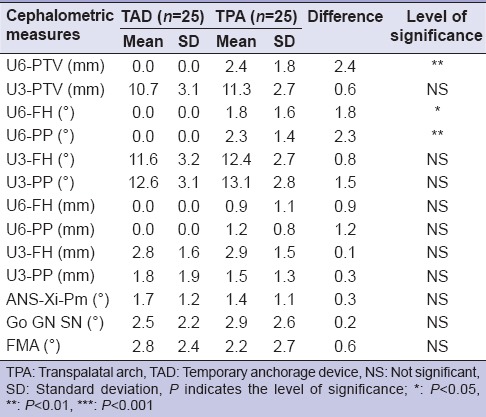
The pretreatment statistics of differences among the groups concerning the lateral cephalometric measurements is shown in Table 1. The differences achieved by canine retraction in both groups are shown in Table 2. After treatment, the difference between the values was 2.4 mm, indicating a significant difference (P < 0.01). Similarly, the upper molar angle relative to the Frankfort horizontal (FH) plane (P < 0.05) and palatal plane (P < 0.01) showed a significant difference after treatment when two groups were compared. The canine distalization showed a similar range of movement between the two groups concerning the inclination relative to FH and palatal plane that shows an insignificant difference (P > 0.05). The net difference for vertical movement of the maxillary first molar in relation to FH plane was 0.9 mm, and 1.2 mm relative to the palatal plane, however the differences were not significant (P > 0.05). The extrusion of the canine following distalization had similar values relative to FH and palatal plane when comparing the two groups, indicating an insignificant difference (P > 0.05). The vertical facial measurements (lower facial height, Go-GN-SN, and mandibular plane angle) showed no significant differences after treatment among the groups.
Table 1.
Comparison of temporary anchorage device and transpalatal arch groups at T0
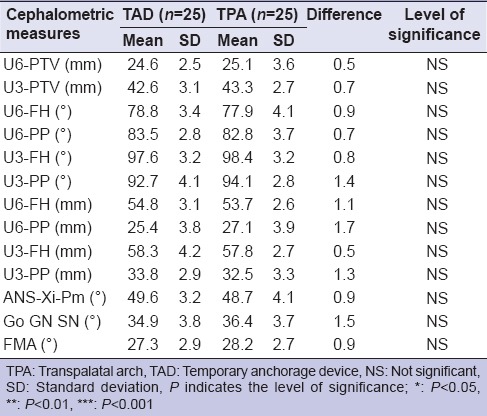
Table 2.
Comparison of treatment changes between T0 and T1
DISCUSSION
The main objective of this study was to evaluate the dental and skeletal effects and the efficiencies of TADs and TPAs for canine retraction movement.
The mean measurements at the beginning of the treatment for both groups are given in Table 1. The measurements of the two groups showed similar values indicating that the groups are harmonious. Both groups had mesofacial type. Analysis of the differences between the two groups showed the differences between absolute anchorage of TADs and reinforced anchorage mechanics (TPA). The results of this study agree with the results of the studies suggesting the placement of TADs for absolute anchorage.[26] Thiruvenkatachari et al.[27] and Herman et al.[17] compared the amount of anchorage loss observed in the first molars reinforced with and without TADs during canine retraction and stated that no anchorage was lost on the side where TAD was placed. Similarly, in our study, no anchorage loss was seen in the TAD group, but a mean 2.4 mm of mesial movement was observed in the TPA group. Garfinkle et al.[28] evaluated the effectiveness of TADs in a controlled clinical trial to provide anchorage for the closure of canine spaces in premolar extraction cases and reported that no anchorage was lost with the system; in addition, the stability of the miniscrews was constant up to 250 g force applied, showing a similarity with these results.
Several studies have investigated the relationship between optimum force magnitude and rate of canine retraction. Storey and Smith[29] have reported an optimum force of 150–200 g for retraction, Iwasaki et al.[30] suggested that an 18 g force could be an effective force for tooth movement; likewise, Ricketts[31] advocated a 75 g force and Lee[32] recommended a 150–200 g as the optimum force for canine retraction. Since in general, light forces are thought to be more biologic and less painful, in our study, 150 g force was applied to be effective for canine retraction.
Benson et al.[33] have compared two groups with midpalatal implants and reinforced anchorage with headgear, revealing that the skeletal and dental points moved mesially with an average of 0.5 mm in headgear group and no movement in midpalatal implant group. The findings of the anchorage loss in the study of Sharma et al.[34] showed an anchor loss of 4 mm in TPA anchorage systems. They have evaluated the maxillary molar distance as the indicator of anchorage loss, whereas in this study, the amount of molar mesialization, tipping, and extrusion was also inspected in the TPA group.
Storey and Smith[29] showed that with conventional orthodontic mechanics, 5–50% of the total extraction space can be taken up by an anchor unit made up of the first molar and second premolar for canine retraction, showing a similarity to our results. Whereas the mechanics combined with TPA may enhance the anchorage control of TPA.
TPA is not a convenient maximum anchorage device and does not provide a significant protection on the anteroposterior position, inclination, and extrusion of the maxillary first molars for canine retraction following extraction. These results showed that the mean anchorage loss was 2.4 mm; therefore, TPA did not adequately reinforce the posterior anchorage in maximum anchorage conditions.
It would be beneficial to evaluate the effectiveness of different approaches of achieving orthodontic space closure using TAD-supported anchorage.
CONCLUSION
Although the treatment duration cannot be reduced by TADs, the better posterior anchorage and greater retraction of the upper anterior teeth are achieved compared to the conventional anchorage systems. The conventional anchorage systems caused the molars to extrude, leading the vertical facial height to increase.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Park HS, Yoon DY, Park CS, Jeoung SH. Treatment effects and anchorage potential of sliding mechanics with titanium screws compared with the Tweed-Merrifield technique. Am J Orthod Dentofacial Orthop. 2008;133:593–600. doi: 10.1016/j.ajodo.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 2.Park HS, Bae SM, Kyung HM, Sung JH. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod. 2001;35:417–22. [PubMed] [Google Scholar]
- 3.Park YC, Chu JH, Choi YJ, Choi NC. Extraction space closure with vacuum-formed splints and miniscrew anchorage. J Clin Orthod. 2005;39:76–9. [PubMed] [Google Scholar]
- 4.Liu YH, Ding WH, Liu J, Li Q. Comparison of the differences in cephalometric parameters after active orthodontic treatment applying mini-screw implants or transpalatal arches in adult patients with bialveolar dental protrusion. J Oral Rehabil. 2009;36:687–95. doi: 10.1111/j.1365-2842.2009.01976.x. [DOI] [PubMed] [Google Scholar]
- 5.Burstone CJ. Rationale of the segmented arch. Am J Orthod. 1962;48:805–22. doi: 10.1016/0002-9416(62)90001-5. [DOI] [PubMed] [Google Scholar]
- 6.Burstone CJ. The segmented arch approach to space closure. Am J Orthod. 1982;82:361–78. doi: 10.1016/0002-9416(82)90185-3. [DOI] [PubMed] [Google Scholar]
- 7.Roberts WE, Helm FR, Marshall KJ, Gongloff RK. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 1989;59:247–56. doi: 10.1043/0003-3219(1989)059<0247:REIFOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Smith RJ, Burstone CJ. Mechanics of tooth movement. Am J Orthod. 1984;85:294–307. doi: 10.1016/0002-9416(84)90187-8. [DOI] [PubMed] [Google Scholar]
- 9.Ioi H, Nakata S, Nakasima A, Counts AL. Anteroposterior lip positions of the most-favored Japanese facial profiles. Am J Orthod Dentofacial Orthop. 2005;128:206–11. doi: 10.1016/j.ajodo.2004.04.030. [DOI] [PubMed] [Google Scholar]
- 10.Keim RG. Answering the questions about miniscrews. J Clin Orthod. 2005;39:7–8. [PubMed] [Google Scholar]
- 11.Park HS, Kwon OW, Sung JH. Microscrew implant anchorage sliding mechanics. World J Orthod. 2005;6:265–74. [PubMed] [Google Scholar]
- 12.Nanda R, Uribe FA. Temporary Anchorage Devices in Orthodontics. St. Louis, MO: Mosby Elsevier; 2009. [Google Scholar]
- 13.Upadhyay M, Yadav S, Patil S. Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: A clinical cephalometric study. Am J Orthod Dentofacial Orthop. 2008;134:803–10. doi: 10.1016/j.ajodo.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 14.Favero L, Brollo P, Bressan E. Orthodontic anchorage with specific fixtures: Related study analysis. Am J Orthod Dentofacial Orthop. 2002;122:84–94. doi: 10.1067/mod.2002.124870. [DOI] [PubMed] [Google Scholar]
- 15.Park HS, Kwon TG. Sliding mechanics with microscrew implant anchorage. Angle Orthod. 2004;74:703–10. doi: 10.1043/0003-3219(2004)074<0703:SMWMIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Gelgör IE, Büyükyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004;74:838–50. doi: 10.1043/0003-3219(2004)074<0838:ISUMD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Herman RJ, Currier GF, Miyake A. Mini-implant anchorage for maxillary canine retraction: A pilot study. Am J Orthod Dentofacial Orthop. 2006;130:228–35. doi: 10.1016/j.ajodo.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 18.Chung KR, Cho JH, Kim SH, Kook YA, Cozzani M. Unusual extraction treatment in Class II division 1 using C-orthodontic mini-implants. Angle Orthod. 2007;77:155–66. doi: 10.2319/020106-35R.1. [DOI] [PubMed] [Google Scholar]
- 19.Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983;17:266–9. [PubMed] [Google Scholar]
- 20.Kuroda S, Katayama A, Takano-Yamamoto T. Severe anterior open-bite case treated using titanium screw anchorage. Angle Orthod. 2004;74:558–67. doi: 10.1043/0003-3219(2004)074<0558:SAOCTU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: A cephalometric evaluation. Angle Orthod. 2004;74:381–90. doi: 10.1043/0003-3219(2004)074<0381:TUOSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Ohnishi H, Yagi T, Yasuda Y, Takada K. A mini-implant for orthodontic anchorage in a deep overbite case. Angle Orthod. 2005;75:444–52. doi: 10.1043/0003-3219(2005)75[444:AMFOAI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Jeon YJ, Kim YH, Son WS, Hans MG. Correction of a canted occlusal plane with miniscrews in a patient with facial asymmetry. Am J Orthod Dentofacial Orthop. 2006;130:244–52. doi: 10.1016/j.ajodo.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Yao CC, Lai EH, Chang JZ, Chen I, Chen YJ. Comparison of treatment outcomes between skeletal anchorage and extraoral anchorage in adults with maxillary dentoalveolar protrusion. Am J Orthod Dentofacial Orthop. 2008;134:615–24. doi: 10.1016/j.ajodo.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 25.Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: Comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008;134:636–45. doi: 10.1016/j.ajodo.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Janssen KI, Raghoebar GM, Vissink A, Sandham A. Skeletal anchorage in orthodontics – A review of various systems in animal and human studies. Int J Oral Maxillofac Implants. 2008;23:75–88. [PubMed] [Google Scholar]
- 27.Thiruvenkatachari B, Pavithranand A, Rajasigamani K, Kyung HM. Comparison and measurement of the amount of anchorage loss of the molars with and without the use of implant anchorage during canine retraction. Am J Orthod Dentofacial Orthop. 2006;129:551–4. doi: 10.1016/j.ajodo.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 28.Garfinkle JS, Cunningham LL, Jr, Beeman CS, Kluemper GT, Hicks EP, Kim MO. Evaluation of orthodontic mini-implant anchorage in premolar extraction therapy in adolescents. Am J Orthod Dentofacial Orthop. 2008;133:642–53. doi: 10.1016/j.ajodo.2006.04.053. [DOI] [PubMed] [Google Scholar]
- 29.Storey E, Smith R. Force in orthodontics and its relations to tooth movement. Aust J Dent. 1952;56:11–8. [Google Scholar]
- 30.Iwasaki LR, Haack JE, Nickel JC, Morton J. Human tooth movement in response to continuous stress of low magnitude. Am J Orthod Dentofacial Orthop. 2000;117:175–83. doi: 10.1016/s0889-5406(00)70229-0. [DOI] [PubMed] [Google Scholar]
- 31.Ricketts RM. Development of retraction sections. Found Orthod Res Newsletter. 1974;5:41–4. [Google Scholar]
- 32.Lee BW. Relationship between tooth-movement rate and estimated pressure applied. J Dent Res. 1965;44:1053. doi: 10.1177/00220345650440051001. [DOI] [PubMed] [Google Scholar]
- 33.Benson PE, Tinsley D, O'Dwyer JJ, Majumdar A, Doyle P, Sandler PJ. Midpalatal implants vs headgear for orthodontic anchorage – A randomized clinical trial: Cephalometric results. Am J Orthod Dentofacial Orthop. 2007;132:606–15. doi: 10.1016/j.ajodo.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 34.Sharma M, Sharma V, Khanna B. Mini-screw implant or transpalatal arch-mediated anchorage reinforcement during canine retraction: A randomized clinical trial. J Orthod. 2012;39:102–10. doi: 10.1179/14653121226878. [DOI] [PubMed] [Google Scholar]


