Abstract
Objective To test the effectiveness of an evidence based model for management of depression in primary care with support from quality improvement resources.
Design Cluster randomised controlled trial.
Setting Five healthcare organisations in the United States and 60 affiliated practices.
Patients 405 patients, aged ≥ 18 years, starting or changing treatment for depression.
Intervention Care provided by clinicians, with staff providing telephone support under supervision from a psychiatrist.
Main outcome measures Severity of depression at three and six months (Hopkins symptom checklist-20): response to treatment (≥ 50% decrease in scores) and remission (score of < 0.5).
Results At six months, 60% (106 of 177) of patients in intervention practices had responded to treatment compared with 47% (68 of 146) of patients in usual care practices (P = 0.02). At six months, 37% of intervention patients showed remission compared with 27% for usual care patients (P = 0.014). 90% of intervention patients rated their depression care as good or excellent at six months compared with 75% of usual care patients (P = 0.0003).
Conclusion Resources such as quality improvement programmes can be used effectively in primary care to implement evidence based management of depression and improve outcomes for patients with depression.
Introduction
Depression is frequently treated in primary care,1 yet there are barriers to its effective management.2,3 Recent randomised controlled trials in primary care showed benefits for patients with depression from increased telephone support, better cooperation between primary care and mental health professionals, and more systematic follow up.4-6 Some of these changes are costly, however, and their implementation has required intensive support from research teams. Changes have also proved difficult to sustain outside externally funded research.7
To disseminate these models widely, strategies are needed to support their implementation and maintenance in community settings. To be practical, these strategies should be based on available resources. Our project, the re-engineering systems for primary care treatment of depression, relied on established quality improvement programmes. In the United States these programmes are typically part of the infrastructure of large medical groups. Their charge includes the collection of data on performance quality, the provision of these data to clinicians and administrators, and assistance for clinicians and practices to meet targets through educational support, additional resources, and changes in practice organisation. Similar resources could be developed through national health programmes and professional organisations.8,9
We developed and tested a model of evidence based management of depression that could be widely disseminated. We hypothesised that implementation would improve targeted processes for management of depression and improve outcomes at six months.
Methods
We recruited five healthcare organisations (three medical groups and two health plans) across the United States. To be eligible, each needed to be affiliated with at least 10 primary care practices, have an established quality improvement programme, and be willing to sustain and disseminate our model if it added value at reasonable cost. Methods are described in detail elsewhere.10
Leaders of the five organisations invited the affiliated practices to participate. Sixty practices were identified. An evaluation centre randomised these practices after stratification by healthcare organisation. The practices were paired on the basis of clinicians' specialty (internal medicine or family practice), number of clinicians, onsite mental health care (yes or no), and distance from the organisation's central office. Within pairs, practices were randomly assigned to intervention or usual care by flip of a coin.
Participant flow and follow up
Between February 2002 and February 2003 the clinicians identified patients aged 18 years or older who were starting or changing treatment for depression. Participants had to have a telephone, speak English, and meet the criteria of the Diagnostic and Statistical Manual of Mental Disorders fourth edition for major depressive disorder and dysthymia. The evaluation centre determined diagnoses using a structured interview.11 The severity of depression was assessed with the Hopkins symptom checklist-20, with a score of 0.5 or more required for enrolment.12
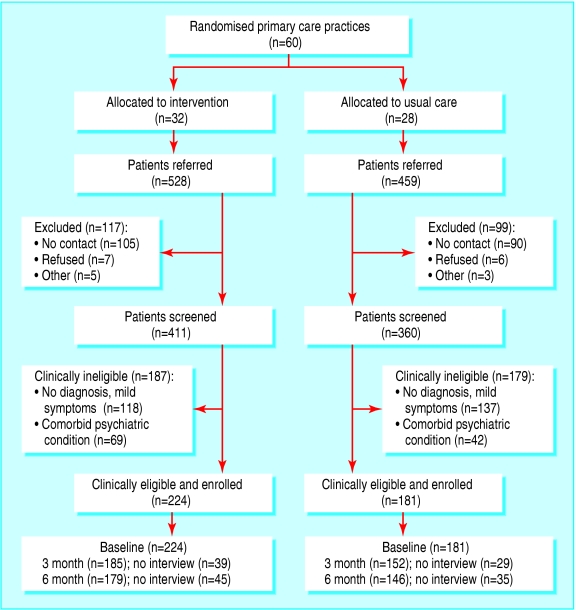
Patients were excluded if they were unobtainable for an evaluation interview within 14 days of their index primary care visit, were pregnant, or had suicidal thoughts, schizophrenia, bipolar disorder, post-traumatic stress disorder, or a substance misuse disorder. Figure 1 shows the flow of patients through the trial.
Figure 1.
Flow of patients through trial
Intervention
The intervention concerned a systematic approach to the assessment and management of depression by the clinician, with a centrally based care manager providing telephone support for patients.13 Most of the care managers had backgrounds in primary care or mental health nursing. The patient health questionnaire-9 was used to aid in diagnosis, to monitor treatment response, and to guide changes in treatment.11,14,15
Patients received a follow up telephone call from the care manager one week after their initial visit. Thereafter they were telephoned monthly and as needed until remission. The care managers assisted patients in overcoming barriers to adherence to the protocol. They supported self management practices such as exercise or engaging in social activities. At the monthly calls the questionnaire was re-administered. The clinician was provided with the reports, including the score from the questionnaire.
Psychiatrists employed by the organisations supervised the care managers through weekly telephone contact. During these contacts, the care managers presented new patients and follow up contacts. Based on the participants' responses to the questionnaire, the psychiatrist could suggest changes either through the care manager or by direct contact with the clinician. Clinicians were also able to contact the psychiatrists for informal telephone advice.
Depending on experience, the care managers received training for 4-8 hours. The psychiatrists received one hour's training. Intervention clinicians took part in a one to two hour educational programme that addressed the diagnosis of depression, assessment of suicidal thoughts, response to management on the basis of responses to the questionnaire, and modification of management to achieve remission. Staff in the intervention practices received a 45 minute course on the intervention, and both they and the clinicians were instructed on procedures for enrolling patients.
Clinicians in the practices allocated to usual care took part in a 45-60 minute programme on diagnosis of depression and assessment of suicidal thoughts. Both they and their staff were instructed on procedures for enrolling patients.
With financial support from our project, the five organisations developed the autonomy to implement the model and to maintain it through follow up with the practices. The organisations identified care managers and psychiatrists, who were trained by employees of the organisations. These employees gradually assumed responsibility for training.
Blinding and data collection
The evaluation centre assessed the clinical course of the patients through interviews by telephone at baseline and at three and six months. Interviewers were blind to study group assignment, followed computer aided scripts, and had no knowledge of the purpose of the study or of the intervention. The Hopkins symptom check list-20 was used to assess the severity of depression. The interviewers also asked about current drugs, recent care, and satisfaction with care. Interviews lasted about 30 minutes.
Statistical analysis
We use means (standard deviations) for continuous variables and percentages for categorical variables. Our primary outcomes included depressive symptoms (scores on the Hopkins symptom check list-20), response to treatment (50% or more reduction in depression score from baseline), and remission (< 0.5 depression score). The process of treatment was analysed for the number of patient visits to primary care for depression, the number of follow up telephone contacts, continued use of antidepressants, and use of psychological counselling during the past three months.
We used linear mixed effects regression models, including both fixed and random effects, to analyse the effect of the intervention on continuous outcomes. We analysed the effect of the intervention on binary outcomes with generalised linear mixed effect models with a logit link. The random effects portion of these models provides the structure needed to account for clustering or potential lack of independence that may exist between observations for the same practice.16 We fitted the mixed effects using SAS Proc mixed and Proc nlmixed. Both progams use all data to yield unbiased estimates of variables for mixed effect models when outcomes are missing at random.17
We fit a random intercept model that included the fixed effects of depression severity at baseline, intervention, and time. We also fit models of a two way interaction (intervention by time) for both the continuous and binary outcomes. Further, we tested a three way interaction among intervention, time, and baseline depression scores by testing intervention by time interaction effect within each stratum defined by baseline scores of more than two.
Our sample size calculation is based on a baseline depression score of 1.5, a two tailed t test, and a between group clinically meaningful difference of 0.15 (SD 0.50) in depression scores at follow up. Adjusting for potential design effects, we determined that we needed to recruit 60 practices (30 in each group).18 We analysed our data on an intention to treat basis. Using methodology to adjust for patient clustering within practice and a range of practice intraclass correlation coefficients based on prior results, we found that for a β of 0.2, an α of 0.05, and allowing for 15% dropouts, we required 400 patients.19,20
Results
The characteristics of the practices and patients were well balanced (tables 1 and 2). The mean depression score on the Hopkins symptom checklist-20 for the total sample was 2.01, which is consistent with moderate to severe symptoms. According to the mental disorders patient health questionnaire,21 47% of usual care patients and 51% of intervention patients (P = 0.42) had generalised anxiety, panic disorder, or both.
Table 1.
Characteristics of practices randomised to manage patients with depression using evidence based model or usual care. Values are numbers (percentages) unless stated otherwise
| Characteristic | Intervention practices (n=32) | Usual care practices (n=28) |
|---|---|---|
| Mean (SD) No of clinicians | 3.8 (3.4) | 3.7 (2.7) |
| Mean (SD) No of km from organisation central office | 33.5 (31.7) | 33.9 (29.1) |
| On-site mental health care | 7 (22) | 8 (29) |
| Specialty: | ||
| Family practice | 21 (66) | 19 (68) |
| Internal medicine | 11 (34) | 9 (32) |
| Location: | ||
| Suburban or rural | 26 (81) | 23 (82) |
| Urban | 7 (22) | 5 (18) |
| Ownership: | ||
| Healthcare organisation | 17 (53) | 20 (71) |
| Affiliated to, but not owned by, organisation | 15 (47) | 8 (29) |
Table 2.
Baseline characteristics of patients being managed for depression with evidence based model or usual care. Values are numbers (percentages) unless stated otherwise
| Characteristic | Intervention group (n=224) | Usual care group (n=181) |
|---|---|---|
| Women | 83.5 | 76.2 |
| Mean (SD) age (years) | 41.8 (14.1) | 42.2 (15.3) |
| Mean (SD) education | 13.3 (2.4) | 13.2 (2.2) |
| Ethnic minority | 36 (16) | 32 (18) |
| Married | 127 (57) | 97 (54) |
| Lives with others | 193 (86) | 162 (90) |
| Income above poverty level | 172 (77) | 41 (74) |
| Paid employment | 135 (60) | 114 (63) |
| Mean (SD) severity of depression* | 2.03 (0.65) | 1.98 (0.65) |
| Major depression | 176 (79) | 142 (79) |
| Major depression and dysthymia | 44 (20) | 34 (19) |
| Dysthymia | 4 (2) | 5 (3) |
| Generalised anxiety disorder | 93 (42) | 72 (40) |
| Panic disorder | 51 (23) | 32 (18) |
20 items (Hopkins symptom checklist-20) from Hopkins symptom checklist-90.
Table 3 describes the process of care. Compared with the usual care clinicians the intervention clinicians more often asked patients about suicidal thoughts, offered educational materials, and assisted in setting self management goals. Intervention patients also received more follow up contact by visits or telephone and were significantly more likely at both three and six months to report receiving good or excellent care. We found no differences between the groups for frequency with which clinicians presented patients with treatment options or elicited their preferences. The patterns of management (drugs alone, counselling alone, or both) did not differ significantly. No adverse events were reported.
Table 3.
Process of care for patients being managed for depression with evidence based model or usual care. Values are percentages (numbers/total numbers)
| Variable | Intervention group | Usual care group | P value |
|---|---|---|---|
| Actions at index visit: | |||
| Asked about suicidal thoughts | 88 (190/217) | 69 (120/174) | <.0001 |
| Presented treatment options | 69 (153/223) | 68 (121/179) | 0.83 |
| Asked about treatment preference | 55 (120/220) | 54 (94/175) | 0.87 |
| Offered educational materials | 71 (156/221) | 40 (70/176) | <.0001 |
| Assisted in setting self management goals | 31 (68/220) | 19 (34/179) | 0.007 |
| Taking antidepressants: | |||
| Baseline | 92 (204/223) | 88 (159/181) | 0.23 |
| 3 months | 88 (161/183) | 85 (128/150) | 0.48 |
| 6 months | 79 (140/177) | 81 (116/144) | 0.74 |
| Receiving counselling (past three months): | |||
| Baseline | 16 (35/223) | 15 (26/179) | 0.75 |
| 0-3 months | 26 (47/182) | 23 (34/149) | 0.53 |
| 4-6 months | 26 (46/177) | 24 (35/146) | 0.68 |
| ≥ follow up visits for depression: | |||
| 0-3 months | 85 (156/183) | 71 (107/150) | 0.002 |
| 4-6 months | 65 (114/175) | 51 (74/145) | 0.01 |
| ≥ follow up telephone calls for depression | |||
| 0-3 months | 64 (116/181) | 8 (12/148) | <0.0001 |
| 4-6 months | 59 (104/177) | 3 (5/146) | <0.0001 |
| Patient rating of care as good to excellent: | |||
| 3 months | 91 (163/179) | 81 (119/147) | 0.008 |
| 6 months | 90 (160/177) | 75 (110/146) | 0.0003 |
Denominators vary owing to missing data.
Table 4 presents depression scores, response, and remission based on intention to treat. Intervention patients had better outcomes on all measures at both follow up intervals. Although mean depression scores declined among patients in both groups, the decline was significantly greater in intervention patients: the intervention effect size on the Hopkins symptom checklist-20 was 0.23 at three months and 0.29 at six months.
Table 4.
Clinical outcomes for patients being managed for depression with evidence based model or usual care. Values are percentages (number of patients/total number) unless stated otherwise
| Outcomes | Intervention patients | Usual care patients | Between group difference or odds ratio (95% CI)* | P value |
|---|---|---|---|---|
| Mean (SD) severity of depression†: | ||||
| Baseline | 2.04 (0.66) | 1.98 (0.65) | 0.15 (−0.03 to 0.33) | 0.105 |
| 3 months | 1.16 (0.80) | 1.29 (0.76) | −0.16 (−0.32 to −0.002) | 0.048 |
| 6 months | 0.97 (0.80) | 1.09 (0.74) | −0.20 (−0.39 to −0.014) | 0.036 |
| Response‡: | ||||
| 3 months | 53.0 (97/183) | 34.2 (52/152) | 2.2 (1.4 to 3.4) | 0.001 |
| 6 months | 59.9 (106/177) | 46.6 (68/146) | 1.7 (1.1 to 2.7) | 0.021 |
| Remission§: | ||||
| 3 months | 26.2 (48/183) | 16.5 (25/152) | 2.1 (1.2 to 3.7) | 0.018 |
| 6 months | 37.3 (66/177) | 26.7 (39/146) | 1.9 (1.2 to 3.3) | 0.014 |
Adjusted for variability in practices. All patients have at least 0.5 score on Hopkins symptom checklist-20 at baseline.
Scores on Hopkins symptom checklist-20.
At least 50% decrease in depression score from baseline.
Score of <0.5 on Hopkins symptom checklist-20.
Log books completed by the care managers indicated that a mean of 20 minutes was expended for each telephone call, including record keeping. The psychiatrists had infrequent contact with the clinicians (< 5% of patients). The clinicians reported negligible time demands from the model aside from administrative duties such as obtaining consent.
Now that our trial is complete, the leaders of the organisations have sustained the model and disseminated it further with local resources. As of March 31, 2004 an additional 139 practices have been supported to implement the model.
Discussion
Enhanced management of depression can improve outcomes for patients when implemented through quality improvement resources increasingly available to community practices. Depressed patients in our intervention practices reported significantly milder symptoms of depression and had higher response and remission rates at follow up than patients in the usual care practices. The effect sizes are comparable to those of other trials on depression in primary care.22
We identified elements that possibly influence clinical outcomes. The intervention patients had more telephone contacts and more visits. Intervention patients reported that the clinicians were more likely to assess suicide risk, offer educational materials, and assist with self management goals. Counselling and adherence to antidepressants were similar between the groups, suggesting that specific but modest support for patients result in better outcomes for depression and higher patient ratings for quality of care.
Although clinical outcomes were enhanced, these effects were modest. At least four features of our study may help to explain this. Firstly, rather than identifying potentially ambivalent patients through screening, all patients were identified during routine care by the clinicians, had accepted the diagnosis of depression, and had agreed to be managed with drugs or by counselling. Secondly, the usual care clinicians performed well on process and outcome measures compared with those in other trials,22,23 creating a high standard of comparison. Thirdly, there was potential for attenuation of the intervention tasks compared with their direct implementation by researchers using a strict protocol.24 Finally, our intervention was modest compared with other recent large trials. Unlike our trial, IMPACT (improving mood-promoting access to collaborative treatment), PIC (partners in care), and PROSPECT (prevention of suicide in primary care elderly: collaborative trial) offered increased access to mental health services at no or reduced cost.20,23,25
Given these design features and dependence of the intervention on training manuals and existing quality improvement resources rather than research protocols and transient resources, the superior outcomes compared with usual care are noteworthy. We acknowledge that remission rates at six months indicate that most patients had at least partial symptoms. These patients continued to receive support and may have improved further, as found in longer term studies.20,23,26 Evaluation interviews in our study were completed by six months after patient enrolment in keeping with the commitment to provide the model to usual care practices in that time.
We suggest that by recruiting 60 practices in diverse locations, our trial extends the generalisability of earlier findings on efficacy of telephone support and primary care specialty cooperation beyond special settings. Many of these earlier studies took place in health maintenance organisations, academic sites, or veterans administration practices.27-31 Our trial adds to this knowledge by showing that modest resources delivered through established programmes can approach outcomes achieved by more research intense, resource rich interventions. These findings take on added importance in light of the negative result from the Hampshire depression project in which the intervention was based on clinician education but did not include telephone support or psychiatry for patients.32 In addition, some US government bodies have called for more intensive monitoring of patients prescribed antidepressants.33 Our model provides this, including assessment of suicidal thoughts.
The generalisability of our findings to primary care are constrained because the practices had access to established quality improvement programmes and care management staff, resources which are becoming more widely, but not yet universally, available. Attention to quality improvement is growing.8,9,34 Primary care trusts in the United Kingdom may be able to assume this function, and in some countries professional societies and regional health authorities could play a part.
Our study shows the feasibility of doing rigorous research in community practice settings relying on established resources to deliver the intervention rather than on transient research teams. Using this approach would enable future research in primary care to explore sustainability and dissemination of interventions. In addition, materials created to support these interventions could be more readily modified for application outside the research setting.
What is already known on this topic
Trials have shown improved outcomes for depression in primary care patients using models for the management of chronic illness
These models involve more systematic follow up and monitoring, patient telephone support, and cooperation between primary care and psychiatry
Implementation of these models has usually depended on research teams and has not been sustainable when research support ends
What this study adds
Evidence based models of depression management can be implemented in primary care with support from existing quality improvement resources
These models can improve outcomes for depression
Our model for depression produced significantly better outcomes and more favourable patient responses on quality of care than usual care. The model requires only modest changes from practices and creates a framework to study long term sustainability and dissemination of evidence based care.
We thank James E Barrett, Leon Eisenberg (initiative steering committee), Laurie Garduque, Robert Rose (John D and Catherine T MacArthur Foundation) for their contributions to this work. For their leadership: Wayne Cannon, Brenda Reiss-Brennan, and Debby Giordano (Intermountain Health Care); Neil Korsen, Lisa M Letourneau, and Robert McArtor, (MaineHealth); James Cox-Chapman, Jonathan Rosen, and Steven Cole MD of ProHealth; Marshall Thomas MD and Jeannette Waxmonsky PhD of Colorado (Access); and Alan Axelson, Carol Chase, and Scott Leatherbery (Highmark, an independent licensee of the Blue Cross Blue Shield Association). Training manuals and other resources are available at www.depression-primarycare.org/clinicians/re_engineering/
Contributors: AJD, TEO, JWWJr, HCS, KR, PAN, MG, and KK initiated and designed the study. AJD, TEO, JWWJr, HCS, MLB, PWL, PJR, and JJL acquired, analysed, and interpreted the data. AJD, TEO, HCS, MLB, and JJL drafted the paper. AJD, TEO, JWWJr, HCS, MLB, PWL, PJR, SB, MH, KR, PAN, MG, and KK revised the paper. AJD, TEO and JWWJr obtained funding. PWL and PJR provided administrative support. SB acquired an interpreted the data and carried out fieldwork. JJL, MH, and KR provided statistical expertise. MH analysed and interpreted the data. AD is guarantor for the paper.
Funding: John D and Catherine T MacArthur Foundation through its initiative on depression and primary care. The staff participated in discussions about the conceptualisation of the study, but were not otherwise involved. The views expressed in this article are those of the authors and do not necessarily represent the views of the foundation or of the US Department of Veterans Affairs.
Competing interests: AJD has received honorariums from Forest Laboratories and Pfizer and has consulted for Wyeth Pharmaceuticals. TEO has received honorariums from Pfizer for presenting at two conferences on primary care education. JWWJr has received honorariums from GlaxoSmithKline, Pfizer, and Wyeth-Ayerst and has received funding from Eli Lilly and Pfizer. MLB has received an unrestricted education grant from Janssen Pharmaceuticals. KR has been reimbursed by Forest Pharmaceuticals for attending a symposium. KK has received research support and honorariums from Eli Lilly and Wyeth and honorariums from Pfizer. PAN has been funded by Eli Lilly to study patient perceptions of the options for hormone replacement therapy as presented by primary care clinicians.
Ethical approval: Our study was approved by the committees for the protection of human participants at Dartmouth Medical School, Weill Medical College of Cornell University, and participating organisations.
References
- 1.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry 1993;50: 85-94. [DOI] [PubMed] [Google Scholar]
- 2.Ford DE. Managing patients with depression: is primary care up to the challenge? J Gen Intern Med 2000;15: 344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nutting PA, Rost K, Dickinson M, Werner JJ, Dickinson P, Smith JL, et al. Barriers to initiating depression treatment in primary care practice. J Gen Intern Med 2002;17: 103-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Von Korff M, Goldberg D. Improving outcomes in depression. BMJ 2001;323: 948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rost K, Smith J. Retooling multiple levels to improve primary care depression treatment. J Gen Intern Med 2001;16: 644-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA 2003;289: 3145-51. [DOI] [PubMed] [Google Scholar]
- 7.Lin EH, Simon GE, Katon WJ, Russo JE, Von Korff M, Bush TM, et al. Can enhanced acute-phase treatment of depression improve long-term outcomes? A report of randomized trials in primary care. Am J Psychiatry 1999;156: 643-5. [DOI] [PubMed] [Google Scholar]
- 8.Leatherman S, Sutherland K. Quality of care in the NHS of England. BMJ 2004;328: 288-90. [DOI] [PubMed] [Google Scholar]
- 9.Lewis R, Dixon J. Rethinking management of chronic diseases. BMJ 2004;328: 220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dietrich AJ, Oxman TE, Williams JW, Kroenke K, Schulberg HC, Bruce M, et al. Going to scale: re-engineering systems for primary care treatment of depression. Annals Fam Med 2004;2: 301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders patient health questionnaire. JAMA 1999;282: 1737-44. [DOI] [PubMed] [Google Scholar]
- 12.Lipman RS, Covi L, Shapiro AK. The Hopkins symptom checklist (HSCL)—factors derived from the HSCL-90. J Affect Disord 1979;1: 9-24. [DOI] [PubMed] [Google Scholar]
- 13.Oxman TE, Dietrich AJ, Williams JW Jr, Kroenke K. A three-component model for reengineering systems for the treatment of depression in primary care. Psychosomatics 2002;43: 441-50. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16: 606-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Annals 2002;32: 509-21. [Google Scholar]
- 16.Raudenbush S, Bryk A. Hierarchical linear models. 2nd ed. New York: Sage, 2002.
- 17.Verbeke G, Molenberghs G. Linear mixed models in practice: a SAS-oriented approach. New York: Springer, 1997: 222-33.
- 18.Diggle P, Liang K, Zeger S. Analysis of longitudinal data. New York: Oxford University Press, 1994.
- 19.Hsieh FY. Sample size formulae for intervention studies with the cluster as unit of randomization. Stat Med 1988;7: 1195-201. [DOI] [PubMed] [Google Scholar]
- 20.Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000;283: 212-20. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994;272: 1749-56. [PubMed] [Google Scholar]
- 22.Badamgarav E, Weingarten S, Henning J, Knight K, Hasselblad V, Gano A, et al. Effectiveness of disease management programs in depression: a systematic review. Am J Psychiatry 2003;160: 2080-90. [DOI] [PubMed] [Google Scholar]
- 23.Unutzer J, Katon W, Callahan CM, Williams JW Jr., Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288: 2836-45. [DOI] [PubMed] [Google Scholar]
- 24.Eisenberg JM, Power EJ. Transforming insurance coverage into quality health care: voltage drops from potential to delivered quality. JAMA 2000;284: 2100-7. [DOI] [PubMed] [Google Scholar]
- 25.Bruce ML, Ten Have TR, Reynolds CF 3rd, Katz I, Schulberg HC, Mulsant BH, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA 2004;291: 1081-91. [DOI] [PubMed] [Google Scholar]
- 26.Rost K, Nutting P, Smith JL, Elliott CE, Dickinson M. Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ 2002;325: 934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA 1995;273: 1026-31. [PubMed] [Google Scholar]
- 28.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry 1999;56: 1109-15. [DOI] [PubMed] [Google Scholar]
- 29.Simon GE, Von Korff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ 2000;320: 550-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hunkeler E, Meresman J, Hargreaves W, Fireman B, Berman W, Kirsch A, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med 2000;9: 700-8. [DOI] [PubMed] [Google Scholar]
- 31.Hedrick SC, Chaney EF, Felker B, Liu CF, Hasenberg N, Heagerty P, et al. Effectiveness of collaborative care depression treatment in veterans' affairs primary care. J Gen Intern Med 2003;18: 9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thompson C, Kinmonth AL, Stevens L, Peveler RC, Stevens A, Ostler KJ, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire depression project randomised controlled trial. Lancet 2000;355: 185-91. [DOI] [PubMed] [Google Scholar]
- 33.Moynihan R. FDA advisory panel calls for suicide warnings over new antidepressants. BMJ 2004;328: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith R. Quality improvement reports: a new kind of article [editorial]. BMJ 2000;321: 1428. [DOI] [PMC free article] [PubMed] [Google Scholar]