Abstract
Background: Psychiatric distress (depression and anxiety), sexual dysfunction, sleep disturbances, and pain are frequent comorbidities in multiple sclerosis (MS) that have the potential to interfere with functioning and quality of life. Often, patients benefit from a combination of medical and psychotherapeutic interventions. However, the literature suggests that many of these issues have been underdiagnosed or undertreated. To better understand current practices, this study aimed to gain a multidisciplinary perspective on how MS providers assess and treat these five problems.
Methods: An online questionnaire was completed by 42 members of the Consortium of Multiple Sclerosis Centers on their assessment procedures, treatment recommendations, and prevalence rates of these issues in their practices.
Results: More than 80% of participants reported routinely assessing for depression, anxiety, sleep, and pain, but only slightly more than half ask about sexual dysfunction. Most of these health-care providers endorsed using a general question in their assessments and recommending a pharmaceutical intervention.
Conclusions: Health-care providers are aware of the prevalence of these issues in their patients with MS. Promoting the use of validated screening measures and increased research on psychotherapeutic interventions for sleep and pain are two potential avenues for improving patient care.
Multiple sclerosis (MS) is a chronic autoimmune disorder of the central nervous system that can affect multiple areas of functioning. Psychiatric distress is common in MS—23.7% for depression and 21.9% for anxiety—and can negatively influence quality of life.1,2 However, historically it has often been underdiagnosed, with estimated prevalence as high as 30% for depression and 34% for anxiety.3,4 Although there are few treatment studies, there is evidence that a combination of pharmacologic and psychological interventions, such as cognitive-behavioral therapy (CBT), can reduce depression symptoms in MS.5 Unfortunately, inadequate treatment, such as a subthreshold antidepressant drug dosage, is common.3,6
Besides primary depression and anxiety, individuals with MS can also experience psychiatric distress in response to their physical symptoms, which, in turn, can worsen those symptoms. In those cases, psychotherapeutic interventions can often be beneficial in conjunction with medical treatments. One such example is sexual dysfunction. Although it is a common problem in MS, occurring in 40% to 80% of patients, sexual dysfunction has a high risk of undertreatment because providers frequently do not initiate the conversation with the patient.7,8 Untreated sexual dysfunction not only tends to worsen over time in the number and severity of symptoms but also can be detrimental to the mental health aspect of patients' health-related quality of life.9–11 Treatment-wise, the current literature is sparse. That said, commonly used pharmaceutical treatments, such as phosphodiesterase type 5 (PDE5) inhibitors (eg, sildenafil citrate), have been noted to have limited efficacy in the MS population.12,13 Instead, cognitive-behavioral treatments (eg, self-help educational materials, telephone interventions, and in-person interventions) have been posed as possible beneficial alternatives, with several studies demonstrating the potential for improvement of sexual dysfunction from these interventions.14–16
Sleep disturbances are another comorbidity that can negatively affect quality of life, with women with MS tending to endorse greater sleep problems compared with other chronically ill individuals or the overall general population.17 More than 50% of individuals with MS report sleep disorders, such as restless leg syndrome, insomnia, and obstructive sleep apnea, which can contribute to fatigue.18 Certain treatments for sleep disturbances, such as zolpidem and melatonin for insomnia, carry certain risks. For example, zolpidem has adverse effects that include rebound insomnia and complex sleep-related behaviors, and melatonin provides only short-term benefits (ie, approximately 2–4 weeks).19,20 Alternatives include nonpharmacologic options, such as CBT for insomnia (CBT-I), which targets the issues underlying sleep problems by having patients learn and practice techniques such as good sleep hygiene, relaxation training, and stimulus control. For individuals with insomnia and comorbid medical or psychiatric conditions, CBT-I has been found to be an effective intervention.21 Although the research is limited, there is emerging evidence on the efficacy of CBT-I in individuals with MS.22
Similar to sleep disturbances, pain affects more than half of individuals with MS and has been associated with decreased quality of life, in addition to psychosocial and functional difficulties.23,24 Furthermore, individuals with higher pain severity are more likely to have elevated depression and anxiety symptoms.25 Besides managing pain with medications (eg, antidepressants, antiepileptics, and analgesics), individuals with MS may benefit from nonpharmacologic treatments, such as psychosocial and psychotherapeutic interventions, exercise and physical adjustment (eg, changing position, massage), and rest.26 For example, individuals who participated in an interdisciplinary outpatient rehabilitation program, which included psychotherapy and relaxation training, had substantial decreases in their level of pain.27
As such, these mental and behavioral health issues not only are prevalent in the MS population but also can have a significant influence on individuals' quality of life. Given that all five of these issues can be treated pharmacologically and psychologically, this study aimed to gain an understanding of MS providers' current practices. In addition to examining their treatment recommendations, their assessments for each problem were also of interest. These areas are particularly important to reexamine because the literature on potential underdiagnosis and treatment for psychiatric distress and sexual dysfunction is older.3,4,6,8 Furthermore, exploring how psychiatric, sexual, sleep, and pain concerns are being assessed and treated in MS may result in identifying potential strategies for improving patient care.
Methods
Participants
Participants were recruited through the Consortium of Multiple Sclerosis Centers (CMSC), a multidisciplinary organization of health-care professionals in the United States and Canada, which includes physicians, mental health clinicians, nurses, and rehabilitation therapists (eg, physical therapists and occupational therapists). All participants were members of the CMSC who previously consented to be contacted for MS-related research studies. The CMSC administrative staff sent an e-mail invitation to 1623 members in October 2015 with a link to the Google Forms survey, which included an online research consent form approved by the institutional review board of Albert Einstein College of Medicine (Bronx, NY). Responses were collected through December 2015. Because overlapping surveys were being conducted during this time frame, a second request for participation could not be sent.
Measures
The questionnaire used was based on a similar study28 that surveyed CMSC members' screening and assessment methods for cognitive dysfunction. All the responses were anonymous, and no patient-protected information was collected. Participants were asked demographic questions regarding their clinical practices and access to mental health professionals.
For each of the five mental and behavioral health issues, participants were asked whether they routinely assess for it and whether they use a general question or a series of specific questions (eg, a structured interview, a validated measure, or a measure created specifically for their practice). A free-text option was available to write in specific published measures being used. Based on previous research on MS providers' assessment of sexual dysfunction, participants who endorsed not routinely inquiring about it were asked to indicate why from a list of potential barriers.8 Participants were then asked to indicate which treatment recommendation(s) they make for each health issue, selecting as many as applicable from a list of preset choices (ie, prescribe a medication, refer to another provider or specialist for medication management, and refer to a mental health provider for psychotherapy), with a free-text option to write in others. Finally, participants were asked whether they could provide an armchair estimate of the prevalence of each issue in their practice, which they selected from preset percentage ranges (ie, 1%–10%, 11%–20%, 21%–40%, 41%–60%, 61%–80%, 81%–90%, and 91%–100%).
Statistical Analyses
Data from Google Forms were exported to an Excel spreadsheet (Microsoft Corp, Redmond, WA) to code free-text responses numerically into groups for analyses. These responses were first examined to see whether they fit into the same category as one of the preset options. The remaining responses were then grouped together based on their content, such as the same measure (for assessment), technique/intervention, or referral to a specific profession (eg, brief counseling, psychoeducation, referral to physical therapy). If a response did not share similar characteristics with other answers, it was kept separate and given its own numerical code. The data were then exported to a statistical software program (IBM SPSS Statistics version 21 for Windows; IBM Corp, Armonk, NY), where frequency analyses were run for assessment, treatment, and armchair estimate responses for each of the five health issues. Because neurologists were the most represented profession in this sample, t tests were run to determine whether there were differences in assessment trends based on their access to mental health providers.
Results
Demographics of Health-Care Providers
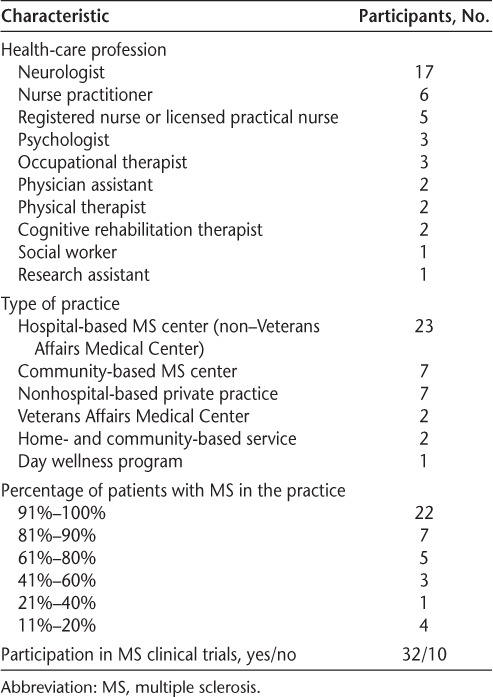
Two hundred twenty-six of the 1291 CMSC members who were contacted and whose e-mails did not bounce back (17.5%) were recorded as opening the e-mail invitation for this study, with 42 of them completing the survey. Most respondents were neurologists (n = 17) and nurses (n = 11) (Table 1). More than half of their practices (n = 22) consisted of 91% to 100% of patients with MS, and more than three-quarters (n = 32) participated in MS clinical trials. Although the age groups of their patient populations were not assessed, there was at least one provider working with children, as indicated by his or her use of pediatric measures.
Table 1.
Profession and practice information for the 42 study participants
All but one participant had access to a mental health provider. Most participants had a provider in either their practice (n = 18) or the same medical center (n = 9). Almost all the participants with a mental health provider in the same practice worked in a non–Veterans Affairs hospital (n = 15). Other participants referred their patients to providers in the community as needed (n = 14). Most participants had access to a social worker (n = 17), psychiatrist (n = 16), or psychologist (n = 14) in their practice or medical center, with a small number having a psychiatric nurse practitioner (n = 2), licensed mental health counselor (n = 2), or marriage and family therapist (n = 1). Nearly half of the neurologists in the sample (n = 8) have a mental health provider in the same practice, most frequently a psychologist (n = 6), psychiatrist (n = 6), or social worker (n = 5).
Assessment and Treatment of Depression
Almost 93% of participants (n = 39) routinely assess patients' mood, primarily using a general question (n = 23). Sixteen providers endorsed using specific questions, which included validated measures such as the Beck Depression Inventory (n = 6), Patient Health Questionnaire (n = 5), Hospital Anxiety and Depression Scale (n = 1), Behavior Assessment System for Children (n = 1), Center for Epidemiologic Studies Depression Scale (n = 1), and Children's Depression Inventory (n = 1). In addition, one participant endorsed using a measure specifically created for his or her practice. Neurologists who had a mental health provider in their same practice were more likely to use a list of specific questions when assessing for depression compared with neurologists who did not (t14 = 2.160, P = .049).
Of the 36 participants who provided an armchair estimate, most (n = 19) reported that 41% to 60% of their patients present with depression (Figure 1).
Figure 1.
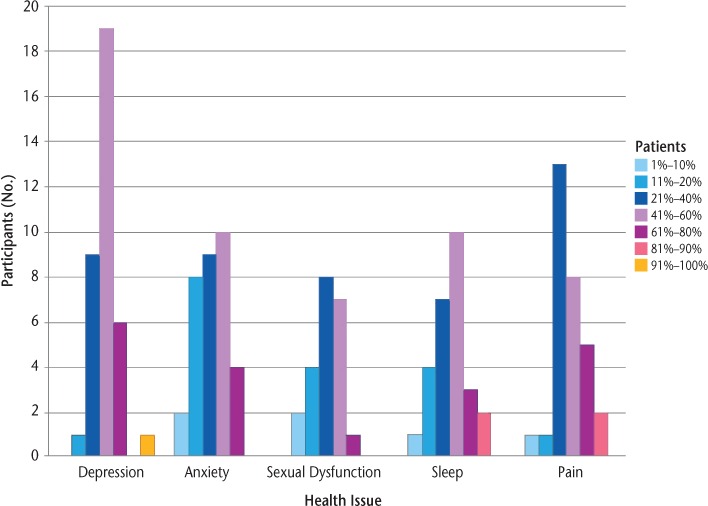
Armchair estimates of the percentage of patients with depression, anxiety, sexual dysfunction, sleep problems, and pain
Medication was the most common treatment recommendation for depression, either prescribed by the participant (n = 28) or through a referral to another provider for medication management (n = 14). More than half of the participants (n = 28) reported referring their patients for psychotherapy. Other referrals and recommended treatments included psychoeducation (n = 1), cognitive remediation therapy (n = 1), physical therapy (n = 1), neuropsychological testing (n = 1), and neurology (n = 1).
Assessment and Treatment of Anxiety
Of the 81% of participants (n = 34) who routinely ask about anxiety, most (n = 28) use a general question in their assessment. The remaining six providers use specific questions, which included validated measures such as the Beck Anxiety Inventory (n = 2), Generalized Anxiety Disorder-7 (n = 1), Behavior Assessment System for Children (n = 1), and Multidimensional Anxiety Scale for Children (n = 1), as well as a measure created specifically for their practice (n = 1). There were no differences in the assessment of anxiety between neurologists with and without a mental health provider in the same practice (P > .05).
Of the 33 participants who provided an estimate, the largest number (n = 10) reported that 41% to 60% of their patients have anxiety (Figure 1).
Treatment recommendations for anxiety were similar to those for depression, with medication being the most common, either prescribed by the participant (n = 25) or through a referral to another provider for medication management (n = 15), followed by psychotherapy (n = 26). In addition to psychoeducation (n = 1), cognitive remediation therapy (n = 1), and referrals to physical therapy (n = 1) and neurology (n = 1), participants endorsed providing brief counseling or instruction on relaxation techniques (n = 3).
Assessment and Treatment of Sexual Dysfunction
Unlike psychiatric distress, sexual dysfunction was assessed by only slightly more than half of the participants (n = 24) as part of their routine examination. Using a general question was the most common assessment method, with only four providers using specific questions, which included the MS Intimacy and Sexuality Questionnaire (n = 1) and a measure specifically created for his or her practice (n = 1). Neurologists with and without a mental health provider in the same practice did not differ in their assessments of sexual dysfunction (P > .05).
Of the 21 participants who provided an armchair estimate, the largest number (n = 8) noted that 21% to 40% of their patients have sexual dysfunction (Figure 1).
In terms of why participants do not routinely ask about sexual dysfunction, the most common reason was that they wait until their patients bring up having a problem (n = 11). Only one provider reported discomfort regarding the topic. Other barriers endorsed were not enough time with the patient (n = 3) and not feeling confident enough in his or her knowledge of the treatment options (n = 1).
More than half of the participants (n = 24) refer their patients to a urologist (or an obstetrician-gynecologist for a female patient). Prescribing a medication was also a common treatment, such as a PDE5 inhibitor (n = 21) or a medication to control other symptoms that may be affecting patients' sexuality (eg, bladder or bowel dysfunction) (n = 22). Several providers endorsed using psychotherapeutic and educational interventions, such as giving patients educational materials (n = 21), referring them to a psychologist (n = 16) or a sex therapist (n = 6), problem-solving sexual problem areas with the patient (n = 16), and directing them to MS organizations (n = 1). Other reported referrals were for nursing (n = 6), physical therapy (n = 5), and neurology (n = 2).
Assessment and Treatment of Sleep Issues
Sleep was routinely assessed by more than 88% of participants (n = 37), with most using a general question (n = 27). Among those who reported using specific questions, several providers listed measures that assess fatigue or quality of life, such as the Fatigue Severity Scale (n = 1), Modified Fatigue Impact Scale (n = 1), Pediatric Quality of Life Inventory Multidimensional Fatigue Scale (n = 1), and Quality of Life in Neurological Disorders (n = 1). One participant endorsed using the Sleep Hygiene Questionnaire, and two others have a measure created specifically for their practices. There were no differences in the assessments used for sleep between neurologists with and without a mental health provider in the same practice (P > .05).
Of the 26 participants who provided an armchair estimate, the largest number (n = 10) reported that 41% to 60% of their patients have sleep problems (Figure 1).
The most common treatment recommendation was referring to another provider specializing in sleep medicine, such as a physician or nurse practitioner (n = 31). Approximately half of the participants (n = 22) reported prescribing a medication, with approximately a quarter (n = 11) referring their patients to a health psychologist.
Assessment and Treatment of Pain
Nearly 93% of participants (n = 39) routinely ask about pain, primarily using a general question (n = 29). Nine providers endorsed using specific questions in their assessments, which included the visual analogue scale of pain (n = 1), Pain Disability Index (n = 1), and a measure created specifically for their practice (n = 2). Neurologists with and without a mental health provider in the same practice did not differ in their assessment of pain (P > .05).
Nearly 74% of participants (n = 31) provided an armchair estimate, with the largest number (n = 13) noting that 21% to 40% of their patients have pain, followed by 41% to 60% (n = 8) (Figure 1).
As with sleep, the most frequently endorsed treatment recommendation was referring to another provider who specializes in pain management, such as a physician or nurse practitioner (n = 32), followed by prescribing a medication (n = 25). Approximately 26% of participants (n = 11) reported referring patients to a health psychologist. Other interventions included referring the patient to physical therapy (n = 3) and providing psychoeducation (n = 3).
Discussion
Considering the prevalence and functional impact of psychiatric distress, sexual dysfunction, poor sleep, and pain in the MS population, it is imperative that patients are properly assessed and receive appropriate symptomatic treatment. The purpose of this study was to gain a multidisciplinary perspective on how these issues are screened and managed by clinicians working with patients with MS. By identifying the common practices, recommendations can potentially be made to inform and improve patient care.
In this sample, most respondents estimated that 41% to 60% of their patients have depression or anxiety. Although this number is higher than recently noted prevalence figures,1 the present study did not ask participants to specify whether their patients met the clinical criteria for a diagnosis. Sexual dysfunction estimates, however, were lower than expected.23 One potential explanation is that only slightly more than half of the participants reported that they routinely ask their patients, which may result in an underestimation. Consistent with previous findings, providers tend to wait for their patients to initiate the conversation,8 and as such they may not be aware that there is a problem unless the patient brings it up. That said, a reassuring finding was that only a minority of participants endorsed discomfort about discussing sexual dysfunction. Because untreated sexual dysfunction is related to decreased quality of life and worsening symptoms,9–11 continued work is needed to help providers increase their level of conversation surrounding the topic. Previous suggestions have included more training about sexual dysfunction in MS, which has been associated with increasing clinicians' initiation with patients.8
Although previous research indicated that psychiatric distress has been underdiagnosed in MS,3,4 these findings show that most providers are asking their patients about their mood and anxiety, as well as their sleep and pain levels. That said, many endorsed using a general question to assess. Although this method allows for a potential problem to be screened quickly, which can be helpful when a provider has limited time with a patient, important diagnostic information might be overlooked. For example, if a patient denies having a depressed mood but instead has anhedonia (ie, decreased interest in activities), using only a general question about mood may result in a missed opportunity for a more in-depth evaluation. A validated screening measure, on the other hand, includes more specific questions and may aid in improved diagnostic accuracy. Nevertheless, although a more comprehensive questionnaire, such as the Beck Depression Inventory, may elicit valuable information, it may not be compatible with a clinician's practice or time constraints. In those situations, the two-question version of the Patient Health Questionnaire may be an option. Regardless of the measure selected, providers need to use their clinical judgment in their interpretations because there may be overlap between depression and MS-related symptoms (ie, fatigue). Furthermore, there will be limitations on the information collected based on the measure used. For example, although the Modified Fatigue Impact Scale assesses how fatigue affects a patient's functioning, it does not include questions on sleep duration or initiation, which are important factors to consider when assessing for dysfunctional sleep.
Having a mental health provider in the same practice may influence other clinicians' assessments, at least with mood. Although it can be hypothesized that clinicians working with a mental health provider may defer to their colleague for a more in-depth evaluation, it emerged rather that neurologists working in these types of practices were more likely to use specific questions when asking about depression. One possible reason may be that neurologists who work closely with mental health providers are more attuned to the different symptoms of depression and, thus, use additional questions in their routine examinations. Further investigation into this practice model, and the setup of these clinics beyond access to mental health providers, is warranted.
Although prescribing a medication or referring to another provider for medication management were the most commonly reported interventions, many participants endorsed referring their patients for psychotherapy, particularly for depression (66.7%) and anxiety (61.9%). Although only a third of participants referred patients with sexual dysfunction for psychotherapy, and, as a whole, were more likely (50%) to prescribe a PDE5 inhibitor despite its limited efficacy in this population,12,13 50% of participants stated that they provide patients with educational materials, an intervention that has been associated with potential improvement in sexual dysfunction.14 Unfortunately, only slightly more than a quarter of providers reported referring patients with pain or sleep issues to a health psychologist. One possible reason for these low referral rates may relate to the availability of these treatments. Although all but one participant in the present study endorsed having a mental health provider in the same practice, medical center, or community, providers may not have access to a professional trained in delivering these specific health psychology services. A second consideration may be the paucity of peer-reviewed, evidence-based interventions for some of these common symptoms, which would typically guide a practitioner's recommendations. For example, although CBT has been demonstrated to be an effective treatment for chronic pain,29 there is limited research on its efficacy in MS. That said, psychosocial factors, such as coping style, may perpetuate an individual's pain experience, contributing to chronic pain.30 As such, additional research is needed in evaluating nonpharmacologic treatments for these issues in MS.
There are several limitations to this study. The first is the low number of participants who completed the survey (<3% of the entire CMSC membership), with these findings representing a restricted view of current practices. A greater response rate may be garnered in the future by surveying providers during an MS conference, such as the CMSC Annual Meeting, which would also allow for additional discussion on these topics that could not be captured in this study's current format (eg, follow-up questioning on how their practices are set up and whether providers in the same practice are expected to assess different problems). In addition, there may be a selection bias because providers who responded may be more likely to assess for these issues. Although more than 80% of participants indicated that they routinely assess for psychiatric distress, pain, and sleep, this study did not ask those who do not as to their reasons, which was done for sexual dysfunction. This may have provided additional information about how assessment of these issues in MS can be improved. In addition, all participants were members of the CMSC who work primarily with patients with MS in the United States and Canada. As such, these results may not represent how depression, anxiety, sexual dysfunction, sleep problems, and pain in MS are assessed or treated in general practices or in other countries. Owing to limitations of the survey, data such as the type of psychotherapy that patients were referred to and the percentage of patients who followed up on referrals to other providers were not collected but are potential areas for additional exploration.
These results provide valuable insight into how MS providers assess and treat psychiatric distress, sexual dysfunction, sleep disturbances, and pain. In particular, although more providers use a general question, which can limit their assessment, neurologists who work in the same practice as mental health providers are more likely to use a list of specific questions when assessing mood. This suggests that collaboration with mental health providers may help other clinicians' assessment of psychiatric distress in MS. Promoting the use of validated screening measures and increased research on psychotherapeutic interventions for sleep and pain are two potential avenues for improving patient care.
PracticePoints
Most MS providers routinely assess for depression, anxiety, dysfunctional sleep, and pain, and they frequently do so using a general question instead of a specific question list. Neurologists who have a mental health provider in the same practice were more likely to use specific questions when assessing for depression.
Many MS providers report not routinely assessing for sexual dysfunction, primarily waiting for their patients to initiate the conversation instead.
Medication is the most commonly recommended treatment for these mental and physical health comorbidities. Patients are referred more often for psychotherapy when they present with depression and anxiety, with low rates for pain and sleep issues.
Acknowledgments
We thank June Halper for her assistance in distributing the survey to CMSC members and Jessica Sloan and Jeffrey Portnoy for their help in the literature search.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1. Marrie RA, Reingold S, Cohen J, . et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler J. 2015; 21: 305– 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fruehwald S, Loeffler-Stastka H, Eher R, Saletu B, Baumhackl U.. Depression and quality of life in multiple sclerosis. Acta Neurol Scand. 2001; 104: 257– 261. [DOI] [PubMed] [Google Scholar]
- 3. Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T.. The burden of mental comorbidity in multiple sclerosis: frequent, underdiagnosed, and undertreated. Mult Scler. 2009; 15: 385– 392. [DOI] [PubMed] [Google Scholar]
- 4. Korostil M, Feinstein A.. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007; 13: 67– 72. [DOI] [PubMed] [Google Scholar]
- 5. Fiest KM, Walker JR, Bernstein CN, . et al. Systematic review and meta-analysis of interventions for depression and anxiety in persons with multiple sclerosis. Mult Scler Relat Disord. 2016; 5: 12– 26. [DOI] [PubMed] [Google Scholar]
- 6. Mohr D, Hart S, Fonareva I, Tasch E.. Treatment of depression for patients with multiple sclerosis in neurology clinics. Mult Scler. 2006; 12: 204– 208. [DOI] [PubMed] [Google Scholar]
- 7. Foley FW. . Assessment and treatment of sexual dysfunction in multiple sclerosis. : Giesser B, Primer on Multiple Sclerosis. New York, NY: Oxford University Press; 2011: 211– 220. [Google Scholar]
- 8. Griswold G, Foley F, Halper J, LaRocca N, Zemon V.. Multiple sclerosis and sexuality: a survey of MS health professionals' comfort, training, and inquiry about sexual dysfunction. Int J MS Care. 2003; 5: 37– 51. [Google Scholar]
- 9. Stenager E, Stenager EN, Jensen K.. Sexual aspects of multiple sclerosis. Semin Neurol. 1992; 12: 120– 124. [DOI] [PubMed] [Google Scholar]
- 10. Zorzon M, Zivadinov R, Monti Bragadin L, . et al. Sexual dysfunction in multiple sclerosis: a 2-year follow-up study. J Neurol Sci. 2001; 187: 1– 5. [DOI] [PubMed] [Google Scholar]
- 11. Schairer L, Foley F, Zemon V, . et al. The impact of sexual dysfunction on health-related quality of life in people with multiple sclerosis. Mult Scler J. 2013; 20: 610– 616. [DOI] [PubMed] [Google Scholar]
- 12. Safarinejad M. Evaluation of the safety and efficacy of sildenafil citrate for erectile dysfunction in men with multiple sclerosis: a double-blind, placebo controlled, randomized study. J Urol. 2009; 181: 252– 258. [DOI] [PubMed] [Google Scholar]
- 13. DasGupta R, Wiseman O, Kanabar G, Fowler C.. Efficacy of sildenafil in the treatment of female sexual dysfunction due to multiple sclerosis. J Urol. 2004; 171: 1189– 1193. [DOI] [PubMed] [Google Scholar]
- 14. Christopherson J, Moore K, Foley F, Warren K.. A comparison of written materials vs. materials and counselling for women with sexual dysfunction and multiple sclerosis. J Clin Nurs. 2006; 15: 742– 750. [DOI] [PubMed] [Google Scholar]
- 15. Foley F, LaRocca N, Sanders A, Zemon V.. Rehabilitation of intimacy and sexual dysfunction in couples with multiple sclerosis. Mult Scler. 2001; 7: 417– 421. [DOI] [PubMed] [Google Scholar]
- 16. Schairer LC, Quinn H, Flood S, . et al. Pilot randomized control trial of a brief multidisciplinary consultation intervention for treating sexual dysfunction in multiple sclerosis. Poster presented at: Joint Meeting of Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) and European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS); September 2014; Boston, MA. [Google Scholar]
- 17. Bamer AM, Johnson KL, Amtmann D, Kraft GH.. Prevalence of sleep problems in individuals with multiple sclerosis. Mult Scler J. 2008; 14: 1127– 1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bamer AM, Marrie RA, Reider N, . et al. A systematic review of the incidence and prevalence of sleep disorders and seizure disorders in multiple sclerosis. Mult Scler J. 2015; 21: 342– 349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. MacFarlane J, Morin C, Montplaisir J.. Hypnotics in insomnia: the experience of zolpidem. Clin Ther. 2014; 36: 1676– 1701. [DOI] [PubMed] [Google Scholar]
- 20. Smith M, Perlis M, Park A, . et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002; 159: 5– 11. [DOI] [PubMed] [Google Scholar]
- 21. Geiger-Brown JM, Rogers VE, Liu E, Ludeman EM, Downton KD, Diaz-Abad M.. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. 2015; 23: 54– 67. [DOI] [PubMed] [Google Scholar]
- 22. Clancy M, Drerup M, Sullivan AB.. Outcomes of cognitive-behavioral treatment for insomnia, depression, and fatigue for individuals with multiple sclerosis: a case series. Int J MS Care. 2015; 17: 261– 267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Foley P, Vesterinen H, Laird B, . et al. Prevalence and natural history of pain in adults with multiple sclerosis: systematic review and meta-analysis. Pain. 2013; 154: 632– 642. [DOI] [PubMed] [Google Scholar]
- 24. Hadjimichael O, Kerns R, Rizzo M, Cutter G, Vollmer T.. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007; 127: 35– 41. [DOI] [PubMed] [Google Scholar]
- 25. Kalia L, O'Connor P.. Severity of chronic pain and its relationship to quality of life in multiple sclerosis. Mult Scler. 2005; 11: 322– 327. [DOI] [PubMed] [Google Scholar]
- 26. Heckman-Stone C, Stone C.. Pain management techniques used by patients with multiple sclerosis. J Pain. 2001; 2: 205– 208. [DOI] [PubMed] [Google Scholar]
- 27. Sullivan A, Scheman J, LoPresti A, Prayor-Patterson H.. Interdisciplinary treatment of patients with multiple sclerosis and chronic pain. Int J MS Care. 2012; 14: 216– 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Foley F, Benedict R, Gromisch E, DeLuca J.. The need for screening, assessment, and treatment for cognitive dysfunction in multiple sclerosis. Int J MS Care. 2012; 14: 58– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morley S, Eccleston C, Williams A.. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999; 80: 1– 13. [DOI] [PubMed] [Google Scholar]
- 30. Kerns RD. Psychosocial aspects of pain. Int J MS Care. 2000; 2: 35– 38. [Google Scholar]


