Abstract
Objectives
To examine the circumstances, features and management of anaphylaxis in children and adults.
Design
Self-completed questionnaire.
Participants
The age of participants ranged from 0 to 72 years.
Setting
We analysed data from self-completed questionnaires collected over a 12-year period, i.e. 2001–2013, available to people by phone and, since 2012, for online completion through the Anaphylaxis Campaign.
Main outcome measure
We analysed data from self-completed questionnaires collected over a 12- year period, i.e. 2001-2013, available to people by phone and, since 2012, for online completion through the Anaphylaxis Campaign
Results
In total, 356 questionnaires were submitted, of which 54 did not meet the criteria for anaphylaxis. The remaining 302 anaphylactic reactions originated from 243 individuals; 193 (64%) of these reactions were in children. Approximately half of all reactions occurred at home (n = 148; 49%); 61% (n = 193) of reactions occurred in those reporting a history of asthma, and many (n = 76; 41%) of these individuals had asthma that they classified as being severe. In 57% (n = 173) cases, the respondent reacted to a known allergen. Self-injectable adrenaline (epinephrine) was available in 79% of the cases, and it was only used in 38% of episodes. The usage of self-injected adrenaline was lower in children (30%) than in adults (54%), even though 82% of children had adrenaline available at the time of the reaction compared to 74% of adults.
Conclusions
These data suggest that the majority of anaphylaxis reactions are triggered by exposure to known food allergens and that approximately half of these reactions occur at home. Access to self-injectable adrenaline was sub-optimal and when available it was only used in a minority of cases. Avoiding triggers, access to self-injectable adrenaline and its prompt use in the context of reactions need to be reinforced.
Keywords: anaphylaxis, allergy, asthma, adrenaline, food allergens, prevention, self-management
Introduction
There have been substantial increases in the numbers of hospital admissions from anaphylaxis noted in the UK over recent decades,1–3 thus reflecting a probable increase in lifetime risk.4 Similar increases have been noted in other parts of the world.5,6 Many of these reactions occur in those with known allergies and thus reflect failures in prevention and/or appropriate emergency when reactions occur.7 It is now recognised that these reactions commonly occur in community settings.8 In order to inform deliberations on how best to minimise the risk of anaphylaxis and optimise the self-management of reactions, it is therefore important to understand patient perspectives and experiences of such reactions.9 We sought to obtain such insights through analysis of a unique dataset compiled by the Anaphylaxis Campaign, a UK-wide patient charity that provides advice and support to patients/carers experiencing anaphylaxis and their healthcare professionals.
This work builds on a previous report by Uguz et al.,10 which reported an analysis of 109 individuals who reported on 126 reactions up until April 2001. The previous study concluded that the presence of asthma in children led to particularly severe reactions and that self-injectable adrenaline (epinephrine) was under-used, even when readily available. In the present study, we analysed data collected by the Anaphylaxis Campaign over the following 12-year period, i.e. 2001–2013.
Methods
Ethical considerations
The study was processed and approved by the University of Edinburgh’s ethical committee. The Medical Advisory Committee of the Anaphylaxis Campaign had previously approved the format of the final version of the questionnaire used in this study.
Recruitment and data collection
We used the same self-completed questionnaire that was used in the earlier survey.10 These self-completed questionnaires were collected over the period May 2001–September 2013.
Individuals calling the Anaphylaxis Campaign’s Helpline were made aware of the survey, and a copy was sent by post for carer/self-completion to those expressing an interest in participating. From 2012 onwards, it was also made available for online completion through the Anaphylaxis Campaign’s website (www.anaphylaxis.org.uk/)..
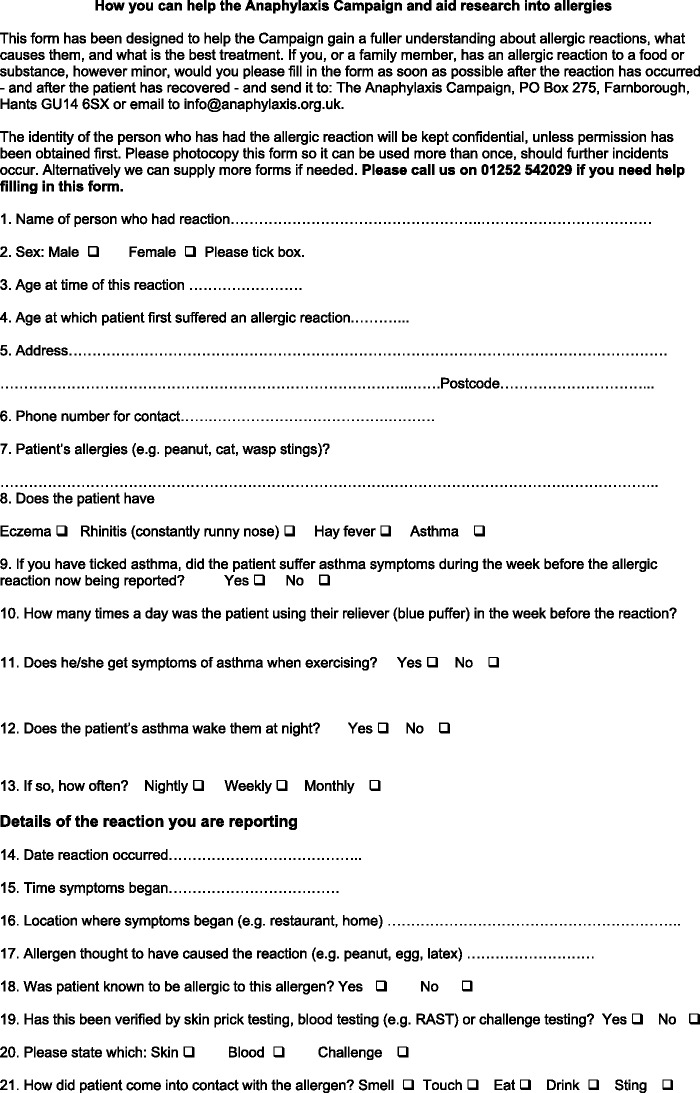
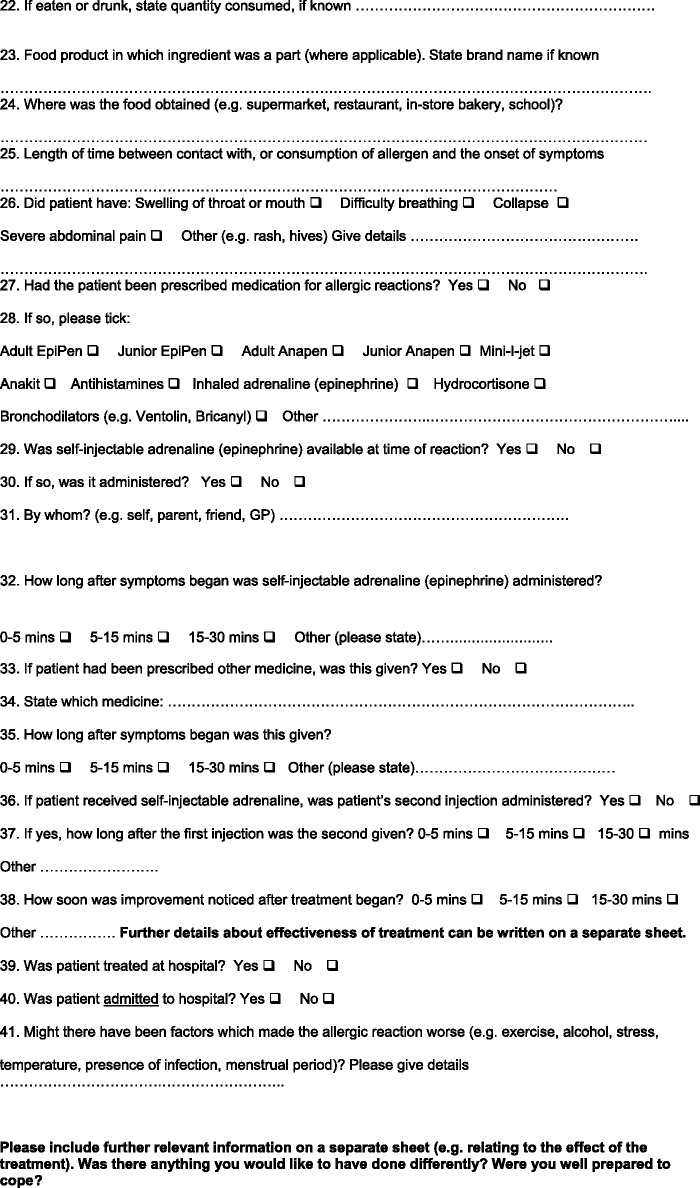
The questionnaire comprised 41 questions, of which approximately half were multiple choice in nature (see Appendix 1). These questions enquired about demographic information and relevant health and medical considerations such as the presence of known allergies. Participants were also asked to provide a description of the reaction that they were reporting; this description included details of the suspected allergen, the symptoms experienced, available treatments, treatments used and whether the reaction resulted in a hospital attendance.
Data processing and analysis
We first sought to determine if the reaction that was described was likely to have been anaphylaxis. This assessment was made by establishing whether there was evidence of a systemic allergic reaction in which respiratory and/or cardiovascular symptoms were also present.11 Those responses that were judged unlikely to represent anaphylaxis were not interrogated any further.
Data from probable reports of anaphylaxis were entered into and analysed using Microsoft Excel. For the purposes of this study, children were defined as those aged 0–16 years and adults were defined as those aged 17 years and over. Co-existent asthma was categorised as being severe if it was reported as causing waking at night; it was otherwise classified as mild-to-moderate.
Data were summarised using counts and percentages with accompanying 95% confidence intervals (CIs), where appropriate.
Results
In total, 356 questionnaires were submitted to the Anaphylaxis Campaign; 54 of these reports were excluded as they were judged unlikely to be reports of anaphylaxis. The following sections relate to the 302 reports that were judged to describe anaphylaxis. These 302 reports came from 243 unique individuals. Of these, 228 individuals provided a single report; the remaining 15 individuals provided a total of 74 reports with these individuals submitting between 2 and 25 incident reports.
Demographic characteristics of respondents
The age of those experiencing reactions ranged from 0 to 72 years with a mean age of 19.1 years (SD 16.6). Sixty-four percent (n = 193; 95% CI 0.58–0.69) of responses related to children; the remaining 36% of reports (n = 109; 95% CI 0.31–0.42) were in adults (i.e. aged 16–72 years).
Of the 243 unique respondents, 58% (n = 140) were female and of these 42% (n = 59) occurred in girls. Of the 103 (42%) unique male respondents, 80% (n = 82) of reactions occurred in boys.
In total, 53% (n = 160) of the reactions were reported by females; there were comparatively fewer reports of reactions in girls (n = 72; 37%) than boys (n = 121; 63%), but this pattern reversed in adults with women reporting a greater proportion of reactions (n = 88; 81%) than men (n = 21; 19%).
Presence of coexistent asthma
Sixty-one percent (n = 185; 95% CI 0.56–0.67) of all reports involved people with co-existent asthma; in 41% of these reports (n = 76; 95% CI 0.34–0.49), the asthma was categorised as being severe.
Setting of reaction and triggers
Forty-nine percent (n = 148) of reactions occurred whilst at home. Similar proportions of children and adults experienced reactions whilst at home (children: 53%, n = 103; 95% CI 0.46–0.61; adults: 41%, n = 45; 95% CI 0.32–0.51).
Of the 90 children’s reactions that occurred outside of the home environment, 26% (n = 23; 95% CI 0.17–0.36) occurred whilst at nursery or school. A further 18% of reactions (n = 16; 95% CI 0.11–0.27) occurred whilst eating out at a café or restaurant and four reactions (4%; 95% CI 0.01–0.11) occurred in hospital.
Sixty-four reactions in adults occurred outside of their homes; 31% (n = 20; 95% CI 0.20–0.44) occurred in a café or restaurant; 13% (n = 8; 95% CI 0.06–0.23) occurred whilst at work and 6% (n = 4; 95% CI 0.02–0.15) occurred whilst in hospital.
Fifty-seven percent (173; 95% CI 0.51–0.63) of reactions were triggered by exposure to a known allergen. The most common known allergen was tree nuts, which accounted for 39% (n = 67) of these reactions to known triggers. Peanuts accounted for 29% (n = 51) of these reactions, milk/dairy products for 11% (n = 19) and egg for 9% (n = 16). Non-food triggers described included inhalant allergens (grass, dust, cat, dog and horse), stinging insects (wasp and mosquito), drugs (antibiotics, aspirin, paracetamol and anaesthetics) and latex.
Self-management, hospital attendance/admission and outcomes
Although in the majority of cases (n = 240; 79%, 95% CI 0.74–0.84), self-injectable adrenaline (epinephrine) was available, it was only administered in 38% (n = 92; 95% CI 0.32–0.45) of cases.
Availability of self-injectable adrenaline was comparable in children (n = 159; 82%, 95% CI 0.76–0.87) and adults (n = 81; 74%, 95% CI 0.65–0.82). Children with available adrenaline were however less likely to receive/use it (n = 48; 30%; 95% CI 0.23–0.38) than adults 54% (n = 44; 95% CI 0.43–0.65).
Adults were more likely (n = 64; 59%, 95% CI 0.49–0.68) to be treated in hospital than children (n = 79; 41%, 95% CI 0.34–0.48). Twenty percent (n = 39; 95% CI 0.15–0.27) of children and 28% (n = 31; 95% CI 0.20–0.38) of adults were admitted to hospital.
There were no fatalities reported in this dataset.
Discussion
Statement of principal findings
This study has found that most cases of anaphylaxis being reported to the Anaphylaxis Campaign followed exposure to known food triggers at home or in other community settings. Reactions were more common in children, with important age-sex differences being found such that reactions were more common in male children and in adult females. Although there was access to self-injectable adrenaline in the majority of cases, it was only used in a minority of cases. Overall, under half of all reactions involved hospital attendance with fewer still resulting in admission. There were no fatalities reported.
Strengths and limitations
A key strength of this study is that it involved carers/individuals personally reporting details of their reactions onto a standard data collection form that had been previously scrutinised by a scientific committee and used in an earlier investigation.10
There are however a number of limitations that need to be considered when interpreting the findings from this research. Key amongst these was that the sample was self-selected raising concerns about the generalisability of the findings. Furthermore, it was not possible within the context of this study to validate the carer/self-reports of triggers, clinical features or self-management.
Interpretation of the findings in the light of previous research
This study echoes the findings from earlier research that the majority of reactions occur in community settings following exposure to known triggers.7,8,10 In keeping with previous research, reactions were common in males in childhood, with this pattern reversing in adults.12 It was of concern that approximately half of all reactions occurred in individuals with a history of asthma; this is because co-existent asthma is known to substantially increase the risk of poor outcomes from anaphylaxis.13,14 A relatively high proportion of individuals had access to adrenaline, this possibly reflecting the fact that this study was undertaken in those who were aware of/members of the Anaphylaxis Campaign – but this only translated into use of self-injectable adrenaline in a minority of cases.15 Further studies are needed to explore why patients do not readily use adrenaline and why they are reluctant to present at hospital. That all individuals survived, despite sub-optimal management in a number of cases, reflects the now known low case fatality ratio from anaphylaxis.16
Implications for policy, practice and future research
This work highlights the importance of providing patients with appropriate allergen advice and furthermore the need for support that will help them to implement this in the context of the complexities of everyday life. UK, European and international anaphylaxis guidelines all make clear the importance of having access to and prompt use of self-injectable adrenaline in the context of reactions, and there is therefore a need for health professionals to reinforce this message at regular intervals.17–21 This is important because the severity of reactions and fatalities can be difficult to predict, hence the need for prompt self-treatment.22,23 Guidelines also encourage a period of observation under medical care following a reaction and so individuals experiencing reactions should be advised to seek urgent medical attention whenever they experience anaphylaxis.17–21
Further research is needed to assess the generalisability of the findings from this work and this would ideally be done by prospectively following a cohort of individuals who record their reactions. This work also suggests that many episodes of anaphylaxis go unreported to medical attention. Such episodes need therefore to be taken into account in future studies into the epidemiology of anaphylaxis using routinely collected healthcare data. Finally, there is a need for further interventional studies which aim to improve the effectiveness of avoidance measures and self-care when avoidance measures fail.24
Conclusions
Many of the concerns highlighted by the previous survey persist, these including the failure of avoidance measures and inadequate carer/self-management in the context of experiencing anaphylaxis. There is a need for intervention studies designed to reduce the risk of recurrent reactions and to optimise self-management in the event of further reactions.
Appendix 1: Allergic reaction record
Declarations
Competing Interests
AaS and SD have a history of anaphylaxis. LR is Chief Executive of the Anaphylaxis Campaign. AzS has served as a consultant to ALK-Abello and Meda and is a member of the Anaphylaxis Campaign’s Clinical and Scientific Panel.
Funding
None declared
Ethical approval
The study was processed and approved by the University of Edinburgh’s ethical committee. The Medical Advisory Committee of the Anaphylaxis Campaign had previously approved the format of the final version of the questionnaire used in this study.
Guarantor
SD
Contributorship
The idea was conceived by the Anaphylaxis Campaign; LR and MA had the idea to analyse the questionnaires and commented on a draft of the paper. The manuscript was drafted by AaS and SD and revised in the light of critical comments from AzS.
Acknowledgements
We wish to express our gratitude to Anaphylaxis Campaign Helpline staff and to the individuals and carers who completed the questionnaire.
Provenance
Not commissioned; peer reviewed by Liz Angier
References
- 1.Sheikh A, Alves B. Hospital admissions for acute anaphylaxis: time trend study. BMJ 2000; 320: 1441–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson R. Upward trend in acute anaphylaxis continued in 1998–9. BMJ 2000; 321: 1021–1022. [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta R, Sheikh A, Strachan DP, Anderson HR. Time trends in allergic disorders in the UK. Thorax 2007; 62: 91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheikh A, Hippisley-Cox J, Newton J, Fenty J. Trends in national incidence, lifetime prevalence and adrenaline prescribing for anaphylaxis in England. J R Soc Med 2008; 101: 139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J Allergy Clin Immunol 2008; 122: 1161–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simons FE, Sampson HA. Anaphylaxis epidemic: fact or fiction? J Allergy Clin Immunol 2008; 122: 166–168. [DOI] [PubMed] [Google Scholar]
- 7.Meh A, Wahn U, Niggemann B. Anaphylactic reactions in children – a questionnaire-based survey in Germany. Allergy 2005; 60: 1440–1445. [DOI] [PubMed] [Google Scholar]
- 8.Beyer K, Eckermann O, Hompes S, Grabenhenrich L, Worm M. Anaphylaxis in an emergency setting – elicitors, therapy and incidence of severe allergic reactions. Allergy 2012; 67: 1451–1456. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher M, Worth A, Cunningham-Burley S, Sheikh A. Strategies for living with the risk of anaphylaxis in adolescence: qualitative study of young people and their parents. Prim Care Respir J 2012; 21: 392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uguz A, Lack G, Pumphrey R, Ewan P, Warner J, Dick J, et al. Allergic reactions in the community: a questionnaire survey of members of the anaphylaxis campaign. Clin Exp Allergy 2005; 35: 746–750. [DOI] [PubMed] [Google Scholar]
- 11.Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF, Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report. Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol 2006; 117: 391–397. [DOI] [PubMed] [Google Scholar]
- 12.Sheikh A, Alves B. Age, sex, geographical and socio-economic variations in admissions for anaphylaxis: analysis of four years of English hospital data. Clin Exp Allergy 2001; 31: 1571–1576. [DOI] [PubMed] [Google Scholar]
- 13.Calvani M, Cardinale F, Martelli A, Muraro A, Pucci N, Savino F, et al. Risk factors for severe pediatric food anaphylaxis in Italy. Pediatr Allergy Immunol 2011; 22: 813–819. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez-Perez A, Aponte Z, Vidaurre CF, Rodriguez LAG. Anaphylaxis epidemiology in patients with and patients without asthma: a United Kingdom database review. J Allergy Clin Immunol 2010; 125: 1098–1104. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher M, Worth A, Cunningham-Burley S, Sheikh A. Epinephrine auto-injector use in adolescents at risk of anaphylaxis: a qualitative study in Scotland, UK. Clin Exp Allergy 2011; 41: 869–877. [DOI] [PubMed] [Google Scholar]
- 16.Panesar SS, Javad S, de Silva D, Nwaru BI, Hickstein L, Muraro A, et al. The epidemiology of anaphylaxis in Europe: a systematic review. Allergy 2013; 68: 1353–1361. [DOI] [PubMed] [Google Scholar]
- 17.Alrasbi M, Sheikh A. Comparison of international guidelines for the emergency medical management of anaphylaxis. Allergy 2007; 62: 838–841. [DOI] [PubMed] [Google Scholar]
- 18.Soar J, Pumphrey R, Cant A, Clarke S, Corbett A, Dawson P, et al. Emergency treatment of anaphylactic reactions – guidelines for healthcare providers. Resuscitation 2008; 77: 157–169. [DOI] [PubMed] [Google Scholar]
- 19.Simons FE, Ardusso LR, Bilò MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy Organization anaphylaxis guidelines: summary. J Allergy Clin Immunol 2011; 127: 587–593.e1–22. [DOI] [PubMed] [Google Scholar]
- 20.Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Fernández Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy 2014; 69: 1026–1045. [DOI] [PubMed] [Google Scholar]
- 21.Simons FE, Ardusso LR, Bilò MB, Cardona V, Ebisawa M, El-Gamal YM, et al. International consensus on (ICON) anaphylaxis. World Allergy Organ J 2014; 7: 9–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000; 30: 1144–1150. [DOI] [PubMed] [Google Scholar]
- 23.Pumphrey R. Anaphylaxis: can we tell who is at risk of a fatal reaction? Curr Opin Allergy Clin Immunol 2004; 4: 285–290. [DOI] [PubMed] [Google Scholar]
- 24.Dhami S, Panesar SS, Roberts G, Muraro A, Worm M, Bilò MB, et al. Management of anaphylaxis: a systematic review. Allergy 2014; 69: 168–175. [DOI] [PubMed] [Google Scholar]