Abstract
Introduction
Patients sometimes present for radiation therapy with high levels of anxiety. Communication skills training may assist radiation therapists to conduct more effective consultations with patients prior to treatment planning and treatment commencement. The overall aim of our research is to examine the effectiveness of a preparatory programme ‘RT Prepare’ delivered by radiation therapists to reduce patient psychological distress. The purpose of this manuscript was to describe the communication skills workshops developed for radiation therapists and evaluate participants’ feedback.
Methods
Radiation therapists were invited to participate in two communication skills workshops run on the same day: (1) Consultation skills in radiation therapy and (2) Eliciting and responding to patients’ emotional cues. Evaluation forms were completed. Radiation therapists’ consultations with patients were then audio‐recorded and evaluated prior to providing a follow‐up workshop with participants.
Results
Nine full day workshops were held. Sixty radiation therapists participated. Positive feedback was received for both workshops with 88% or more participants agreeing or strongly agreeing with all the statements about the different components of the two workshops. Radiation therapists highlighted participating in role play with an actor, discussing issues; receiving feedback; acquiring new skills and knowledge; watching others role play and practicing with checklist were their favourite aspects of the initial workshop. The follow‐up workshops provided radiation therapists with feedback on how they identified and addressed patients’ psychological concerns; time spent with patients during consultations and the importance of finding private space for consultations.
Conclusion
Communication skills training consisting of preparing patients for radiation therapy and eliciting and responding to emotional cues with follow‐up workshops has the potential to improve radiation therapists’ interactions with patients undergoing radiation therapy. Further research is warranted, similar to the RT Prepare study, to determine whether patient anxiety can be reduced as a result of improving communication and information provision.
Keywords: Communication skills training, evaluation, patient anxiety, patient preparation, radiation therapists, radiation therapy
Introduction
Approximately 30% of patients diagnosed with breast cancer present with fear and clinical levels of anxiety prior to radiation treatment planning.1 Evidence suggests that psychological morbidity is under‐recognised and managed throughout cancer care and patients often present with high information needs and unmet psychosocial needs.2, 3 Patients have been found to lack information about radiation therapy and its side effects prior to treatment.4, 5, 6, 7 Examples of information that patients require prior to commencing treatment include why radiation therapy has been recommended; what treatment involves, side effects, details of treatment planning, what happens during treatment and which staff will be involved in providing their treatment.8 Our previous research with patients diagnosed with breast cancer found that patients have high information needs prior to treatment planning and their anxiety levels do not drop significantly until after treatment commencement.1 Patients prefer information to be provided in a staggered way over time to enable them to process the information appropriately.9 A lack of information, usually arising from poor communication, psychosocial support not being provided or information being provided at the wrong time, results in increased patient anxiety, a loss of trust in health professionals, reduced sense of control and most seriously may lead patients to decline treatment.10 Hence, preparing patients for radiation therapy needs to be a high priority. In order to reduce patient anxiety prior to treatment commencement, health professionals have a responsibility to communicate with patients and provide appropriate information.11 Research needs to be conducted, using rigorous study designs, to provide substantial evidence about the best way to prepare patients who are commencing radiotherapy.12
Radiation therapists can play a key role in providing patients with information and support prior to their computed tomography (CT) planning appointment and commencing treatment.13, 14 However, information provision by radiation therapists is inconsistent and varies between departments.15 Furthermore, radiation therapists may not have time or the skills to determine and respond to patients’ emotional concerns while trying to complete the task of patient set up for planning or treatment.
Research on the need to prepare patients for threatening medical procedures has concluded that sensory and procedural information should be provided to allay patients’ fears and concerns relating to treatment and any psychological concerns patients have should be addressed.16 Sensory information involves informing patients about what they might feel, hear or smell during and after the procedure and procedural information describes the steps and processes involved. These principles have been successfully applied in providing chemotherapy education.17 Patient distress about radiation therapy may also be reduced if patients are provided with timely information prior to the procedure they are to undergo and if they are able to discuss their concerns. We have developed and piloted an intervention called ‘RT Prepare’ for patients undergoing radiation therapy for breast cancer based on the principles of preparing patients for threatening medical procedures.18, 19
RT prepare study
The overall aim of our larger research study was to examine the effectiveness of an innovative preparatory programme ‘RT Prepare’ delivered by radiation therapists to: reduce patient psychological distress; reduce specific concerns about radiation therapy; increase patient knowledge of radiation therapy; and increase patient preparedness for their treatment planning appointment and treatment.20 This study is being conducted with patients diagnosed with breast cancer. We are recruiting patients in three states: Western Australia, South Australia and Victoria.
The RT Prepare programme involves radiation therapists consulting with patients diagnosed with breast cancer prior to treatment planning and treatment and providing information and support. This intervention was informed by previous research conducted by the team which determined what information patients require at each stage of radiation therapy.1, 8 In order to deliver the intervention, we provided radiation therapists with communication skills training. Evaluation of this training was the focus of this manuscript.
Communication skills training for health professionals
Communication skills training has previously been trialled and evaluated with other oncology health professionals to show that the workshops are both useful and have positive impact on communication between health professionals and patients.21, 22, 23, 24, 25 Although health professionals may already have good general communication skills two recent systematic reviews have shown that training which focus specifically on responding to patients’ emotions and needs improve the quality of their communication and may improve patient outcomes.26, 27
Radiation therapists in Australia have had limited access to programmes that seek to further develop their communication skills so that they have the ability to respond to patients’ concerns and be prepared for more difficult conversations with their patients. Furthermore, any communication skills training that practicing radiation therapists have had the opportunity to participate in have been irregular sessions that to our knowledge have not been evaluated specifically for radiation therapists. Although radiation therapists might already be good communicators it is likely that they may benefit from training in providing more detailed sensory and procedural information related to radiation therapy.
Furthermore, radiation therapists skills may be improved if they are provided with training about determining and responding to patients’ emotional cues. Additional communication skills training is likely to advance best practice and enhance health professionals’ skills in identifying patients’ needs and addressing their emotions appropriately.28 As a result of this training patient anxiety levels prior to radiation therapy may be reduced. One study by Merckaert et al.29 reported they were successful in training radiation oncology professionals in communication skills in Belgium using a 38 h communication skills training programme. However, a programme such as this is not feasible for radiation therapists Australia‐wide due to the costs and time required to implement the training in every state and territory.
Previous literature indicates that communication skills training is most likely to be effective when it is delivered in small groups where participants are provided with the opportunity to practice and receive feedback.30 Hence, we planned to provide training to radiation therapists in small groups using two 3‐hour communication skills training sessions: one focusing on providing sensory and procedural information about radiation therapy and the second focusing on eliciting and responding to patients’ psychological concerns. These workshops were considered necessary because radiation therapists had previously had little training in eliciting and responding to patients’ emotional cues and needed to be informed about preparing patients appropriately for radiotherapy.
Evaluation of communication skills training for radiation therapists
The aim of this manuscript was to describe the communication skills workshops that were developed for radiation therapists and evaluate feedback received from radiation therapists who participated in the workshops.
Methods
In order to evaluate the workshops we collected participants’ demographics and then asked them to complete feedback surveys after workshops one and two. Ethics approval was gained from Curtin University and the participating sites for the RT Prepare study.
Participants
Radiation therapists were recruited at the three participating clinical sites through the chief radiation therapist at each site. Chief radiation therapists were informed about the larger study and asked to advertise the opportunity to participate in communication skills. In Victoria and Western Australia radiation therapists self‐nominated to participate. In South Australia, all staff members were encouraged to participate in the workshops; however, staff availability and interest impacted on their ability to participate.
Facilitators
Two facilitators (DY and SM) ran the workshops at all sites: one facilitator has a clinical psychology and communication skills background and the second has a radiation therapy background. Both facilitators had previously participated in communication skills workshops and received train‐the‐trainer training to facilitate the eliciting and responding to emotional cues workshops.
Actor/simulated patient
The same trained actor was employed to participate in the role plays for all workshops held for this study to ensure training consistency across all participants. For each workshop the actor was provided a detailed ‘backstory’ including information about her medical and social history, what radiation therapy involves and specific areas that she should cover for each workshop. The actress presented as a breast cancer patient attending for CT planning and treatment. For the first workshop the actor focused on gaining information about radiation therapy, for the second workshop she displayed four different emotions (distress, anger, anxiety, depression) that the radiation therapists needed to recognise and appropriately respond to.
Workshops
Two communication skills workshops were provided to radiation therapists: (1) Consultation skills in radiation therapy and (2) Eliciting and responding to emotional cues workshop. Each workshop was 3 h long and both were completed within the same day. The overall learning focus was on participants developing skills would be able to conduct a consultation with a patient to meet patients’ information needs and determine and respond to their emotional cues.
The objective of workshop 1 on consultation skills in radiation therapy was to provide radiation therapists with the skills and opportunity to practice having a consultation with a patient prior to CT planning and again prior to treatment commencement. Radiation therapists were provided with a background to the research study and detailed evidence on what radiation therapy specific sensory and procedural information patients require and when. After discussing the evidence about patients’ information needs radiation therapists were introduced to an adapted version of Pendleton's31 model of patient consultations to assist them in working through the required tasks they need to perform. This model consists of the following phases: (1) To define the reason for the patient's attendance; (2) To consider other problems; (3) To choose an appropriate action for each problem with the patient; (4) To achieve a shared understanding of the problems with the patient; (5) To involve the patient in the management and encourage him/her to accept appropriate responsibility; (6) To use time and resources appropriately and (7) To establish a relationship with the patient that helps to achieve the other tasks. Radiation therapists were also provided with a checklist to follow for CT planning and treatment commencement and given the opportunity to practice these tasks for both CT planning and treatment with a trained actor. This workshop and the checklist used have been described elsewhere.18, 19
The objective of workshop 2, ‘Eliciting and Responding to emotional cues’, was to ensure radiation therapists are resourced with appropriate communication skills and a framework in which to elicit and respond to emotional cues. This workshop was based on the ‘Eliciting and responding to emotional cues’ workshop21 currently offered to oncology professionals by Cancer Council Victoria and other groups. The materials for this workshop were provided by the Cancer Council Victoria. The content of this workshop was originally based on the National Breast and Ovarian Cancer Centre's guidelines for the psychosocial care of adults with cancer32 and subsequent guidelines on eliciting and responding to emotional cues.33
During these workshops radiation therapists were provided with detailed information about the different emotional cues that patients may present with and were provided with the opportunity to discuss appropriate ways of dealing with these emotional cues in the radiation therapy setting. Radiation therapists were also given ideas about when to refer patients for additional support and were given referral options. At the end of the workshops radiation therapists had the opportunity to practice communication skills with a trained actor and receive feedback about their communication skills from the facilitators, peers and the actor.
Follow‐up workshops
After the communication skills training was completed at each site, radiation therapists commenced conducting patient consultations prior to treatment planning and a second consultation prior to treatment commencement. At all sites, audio recording of consultations delivered to patients participating in the RT Prepare study were taken with their informed consent. Audio recordings of the consultations were taken for all patients receiving the RT Prepare Intervention in the study prior to CT planning and on day one of treatment. Radiation therapists were provided with day‐to‐day support from the RT Prepare study team to organise intervention delivery and to discuss any issues that they had with the trial.
After a period of at least 3 months, the facilitators who delivered the initial workshops visited each site to run a 2 h follow‐up workshop with radiation therapists involved in delivering the intervention.
Prior to each follow‐up workshop the two facilitators reviewed 5–10 tape recordings of the intervention delivery from each site to determine whether radiation therapists were providing adequate information and were eliciting and responding to patients’ emotional cues. Review of the tape recordings was based on a quality assurance protocol developed for the pilot study and included ensuring that radiation therapists described detailed information about radiation therapy and took time to determine and respond to patients’ emotions.18, 19 The quality assurance protocol considered how well the radiation therapist: set the scene; explained the procedure; determined patient understanding and their communication skills (including active listening techniques, responding empathetically to patient emotions and whether they used any blocking behaviours). The following patient emotions were considered within the QA analysis: patient anxiety; patient depression; patient distress and patient anger. Figure 1 provides a summary of the information assessed using the quality assurance protocol. Participants were also invited to email the facilitators to indicate (1) whether they were having any issues with delivering consultations and (2) what they wished to discuss in the follow‐up workshops.
Figure 1.
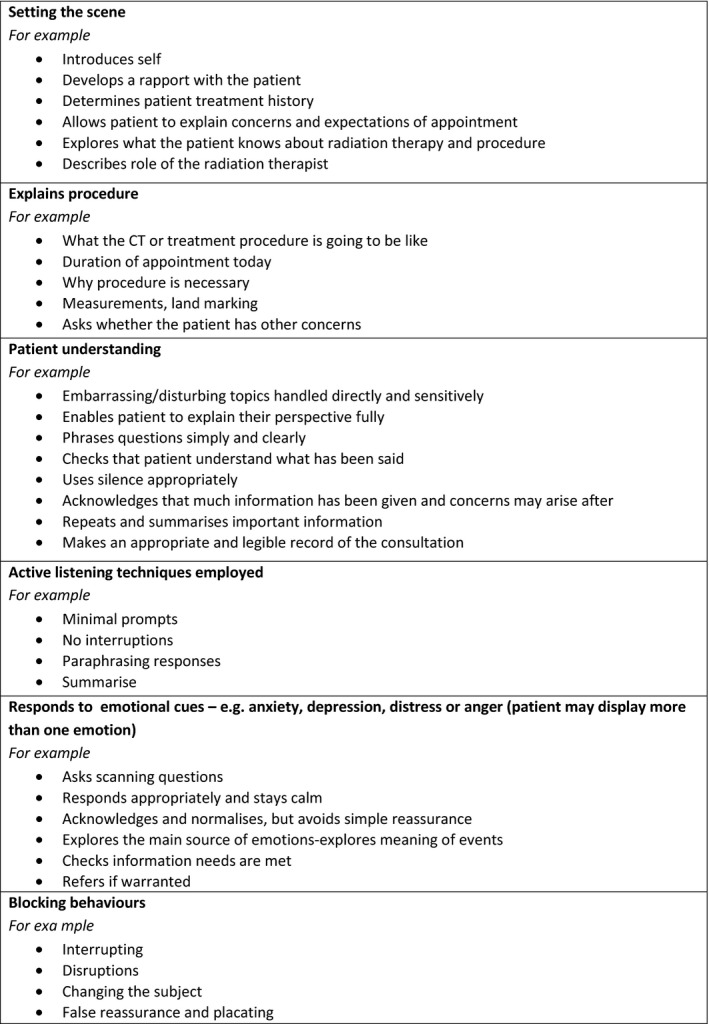
Summary of the QA analysis used for the radiation therapist consults with patients.
Measurement tools
Evaluation surveys were administered after the first two workshops. The workshops were evaluated by participants in terms of whether the information was practical and useful, whether they had the opportunity to discuss patient consultations, role play, timing, size of group, receiving feedback, style of workshop and content of the workshop. Questions focused on delivery of the workshops, content provided and length of the workshops as outlined in the tables below. These evaluation surveys were based on surveys previously used by Cancer Council Victoria for evaluating their communication training workshops.25 Participants also completed a brief demographics form prior to participating in workshops 1 and 2.
Analysis
Descriptive statistics were compiled for the quantitative survey responses. The qualitative data were analysed using content analysis. GH and MO analysed the content and then met regularly to discuss any differences and reach a consensus. The main responses for each question were compiled and then the number of responses alluding to each response was counted by the research assistant and checked by GH and MO.
Results
Nine full day workshops were held (each full day consisted of workshop 1 and 2). In total, 60 radiation therapists participated (15 from Victoria, 31 from South Australia and 14 from Western Australia). These workshops were held at different time points during 2013 and 2014 to coincide with the multiple baseline study format of the overall study. Table 1 provides the demographics of participants.
Table 1.
Demographics
| Perth | Melbourne | Adelaide | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | Frequency | % | |
| Gender | ||||||||
| Male | 4 | 29 | 1 | 7 | 6 | 19 | 11 | 18 |
| Female | 10 | 71 | 14 | 93 | 25 | 81 | 49 | 82 |
| Total | 14 | 100 | 15 | 100 | 31 | 100 | 60 | 100 |
| Employment | ||||||||
| Part time | 1 | 7 | 3 | 20 | 8 | 26 | 12 | 20 |
| Full time | 13 | 93 | 12 | 80 | 23 | 74 | 48 | 80 |
| Total | 14 | 100 | 15 | 100 | 31 | 100 | 60 | 100 |
| Education | ||||||||
| Certificate or diploma | 0 | 0 | 1 | 7 | 6 | 19 | 7 | 12 |
| Undergraduate degree | 11 | 79 | 12 | 86 | 25 | 81 | 48 | 81 |
| Master degree | 3 | 21 | 1 | 7 | 0 | 0 | 4 | 7 |
| Years practicing | ||||||||
| <5 | 10 | 71 | 5 | 33 | 7 | 23 | 22 | 37 |
| 5–9 | 2 | 14 | 5 | 33 | 10 | 32 | 17 | 28 |
| 10–14 | 1 | 7 | 1 | 6 | 6 | 19 | 8 | 13 |
| 15–19 | 1 | 7 | 2 | 13 | 4 | 13 | 7 | 12 |
| 20–24 | 0 | 0 | 0 | 1 | 3 | 1 | 2 | |
| 25< | 0 | 1 | 6 | 3 | 10 | 4 | 7 | |
| Missing | 0 | 0 | 1 | 6 | 0 | 0 | 1 | 2 |
| Total | 14 | 100 | 15 | 100 | 31 | 100 | 60 | 100 |
| Participated in any communication skills training during RT qualification | 9 | 64 | 5 | 36 | 12 | 39 | 26 | 44 |
| Participated in any communication skills training since qualifying | 5 | 36 | 6 | 43 | 5 | 16 | 16 | 27 |
Workshop one – consultation skills in radiation therapy
Table 2 summarises the overall quantitative results for all sites. There were no significant differences noted between sites for these evaluations.
Table 2.
Workshop 1: consultation skills in radiation therapy
| Workshop 1 | SA | A | N | D | SD | Percentage of A or SA |
|---|---|---|---|---|---|---|
| n | n | n | n | n | ||
| The workshops provided information which was practical and useful | 24 | 31 | 3 | 95 | ||
| I found it useful to have this opportunity to discuss patient consultations | 27 | 26 | 5 | 91 | ||
| The role play activities were useful in practicing consulting patients | 25 | 28 | 4 | 1 | 91 | |
| The size of the group was appropriate for this type of workshop | 42 | 13 | 3 | 95 | ||
| Participating in giving and receiving feedback was an effective learning experience for me | 24 | 29 | 5 | 91 | ||
| The style of the workshop was an effective way of introducing patient consultations | 29 | 26 | 3 | 95 | ||
| The content and amount of information provided was appropriate | 23 | 30 | 5 | 91 | ||
| The duration of the workshop was appropriate | 21 | 30 | 7 | 88 | ||
| I enjoyed participating in this workshop | 19 | 35 | 3 | 1 | 93 | |
| I would recommend the workshop to other staff in the department | 23 | 28 | 5 | 91 |
SA, strongly agree; A, agree; N, neither agree or disagree; D, disagree; SD, strongly disagree.
Participants were also asked to describe their favourite aspects of the workshops (multiple responses were allowed) and 47 responses were received. The most common aspects identified using content analysis included: participating in role play with actor (n = 23); discussions on issues identified (n = 10); feedback (n = 7); acquiring new skills and knowledge (n = 7); watching others in the role play (n = 5) and practice with checklist (n = 5).
Participants were also invited to provide suggestions for improvements to workshops. Content analysis identified the following responses: nothing, it was all good (n = 6); more feedback from role play/more time or opportunities for this (n = 5); information provided before the workshop (n = 3); group size smaller for role play (n = 2); change in structure of the workshop (e.g. shorter videos, separate workshops to two separate days (n = 2); more information about the future of the study (n = 1) and homework (n = 1).
Workshop 2 – eliciting and responding to patients’ emotional cues
After participating in the first workshop, participants were provided the opportunity to participate in the communication skills workshop on eliciting and responding to patients’ emotional cues. Results of the quantitative survey completed after Workshop 2 are provided in Table 3. There were no significant differences noted for differences between sites in terms of ratings.
Table 3.
Workshop 2: eliciting and responding to patients’ emotional cues
| Workshop 2 | SA | A | N | D | SD | Percentage of A or SA |
|---|---|---|---|---|---|---|
| n | n | n | n | n | ||
| The workshop: provided practical, relevant information | 40 | 19 | 100 | |||
| The workshop: increased confidence in my communication skills | 34 | 24 | 1 | 98 | ||
| The workshop: provided relevant case scenarios | 42 | 16 | 1 | 98 | ||
| The workshop: will be of benefit to my job | 46 | 12 | 1 | 98 | ||
| The workshop: increased my knowledge about communication with patients | 43 | 16 | 100 | |||
| The role plays: were believable | 45 | 14 | 100 | |||
| The role plays: the actors gave constructive feedback | 47 | 12 | 100 | |||
| The role plays: were safe and non‐threatening | 39 | 15 | 5 | 92 | ||
| The role plays: I had opportunities to practice new lines and phrases | 32 | 23 | 4 | 93 | ||
| The role plays: I developed skills during the role plays that I will be able to use in my work | 38 | 19 | 2 | 97 | ||
| The role plays: giving and receiving feedback was an effective learning experience for me | 42 | 17 | 100 |
SA, strongly agree; A, agree; N, neither agree or disagree; D, disagree; SD, strongly disagree.
Participants’ responses relating to the workshop characteristics including the booklet, time taken to deliver workshop, the DVD, the role play and the actor are provided in Table 4. Overall satisfaction was also rated with 44 participants indicating they were very satisfied and 11 stating that they were satisfied (5 responses were missing). Additional feedback about ‘the most useful part of workshop’ identified using content analysis included: role play (n = 38); practicing skills learned (n = 8); watching others (n = 7); feedback (n = 6) and learning new skills, techniques and phrases (n = 5).
Table 4.
Workshop 2 characteristics
| Workshop 2 | Effective | Good | Fair | Poor | Percentage of effective or good |
|---|---|---|---|---|---|
| n | n | n | n | ||
| Workshop booklet | 33 | 24 | 2 | 97 | |
| Allowed enough time to cover all material | 36 | 22 | 1 | 98 | |
| Comfort of the room/area used | 33 | 25 | 1 | 98 | |
| The facilitators | 47 | 8 | 100 | ||
| The DVD | 28 | 26 | 1 | 98 | |
| The role play | 46 | 9 | 100 | ||
| The actor | 53 | 1 | 100 |
Follow‐up workshops
When a sample (5 to 10 from each site) of tape recordings of the intervention delivery were reviewed using the quality assurance protocol three main findings emerged: It was found that: (1) although radiation therapists were thorough in providing information relating to radiation therapy, some struggled to identify and address patients’ emotional cues. (2) Some of the consultation times appeared to be brief (less than 10 min) and some radiation therapists did not listen and attend to all of the concerns that patients’ identified 3. Finding private space to conduct a consultation with patients proved difficult on some occasions.
As a result, the follow‐up workshops held with the radiation therapists included discussion about how the consultations were going, feedback about the audio recordings and the facilitators provided general tips/reminders about eliciting and responding to emotional cues (e.g. active listening, prompting, describing the emotion) and gave examples of how to respond to anxiety, depression, distress and anger. They also emphasised that although the radiation therapists were constrained by time limitations it is imperative to discuss patients’ concerns at these critical time points and the benefits of such discussions were reiterated.
Discussion
Previous studies have identified that health professionals’ communication skills are likely to improve if they participate in workshops.21, 23, 24, 26, 27 However, no published studies have focused specifically on providing education to radiation therapists that includes both what information to provide to patients about radiation therapy and how to respond to patients’ emotional cues. In this study, 60 radiation therapists participated in communication skills training in three states in Australia. Although the proportion of female participants in our sample was high, this was only slightly higher than the proportion reported in the 2011 national workforce survey (82% female vs. 73% females respectively) and is the proportion of part‐time participants comparable to reported (20% part‐time vs. 21.2% respectively).34 The results suggest that radiation therapists found both workshops useful in terms of the content provided and the opportunity to practice their skills with a trained actor.
For workshop 1, which focused on consultation skills in radiation therapy, we found that 88% or more participants strongly agreed or agreed with all of the statements about the content and running of this workshop. For workshop 2 which focused on eliciting and responding to patients’ emotional cues 92% or more participants agreed with all of the statements about this workshop. Although in a different setting, this finding is similar to results reported by Grainger et al.25 who used a similar evaluation survey and found that 89% or more participants agreed with comparable statements about the workshop they provided on transitioning to palliative care. Grainger et al. found that 11% of participants did not strongly agree or agree with the statement that their workshop allowed enough time cover all of the information. In our study, we found that the majority of participants provided extremely positive responses about both workshops, but content analysis identified that a small number of participants felt that more time, role play and opportunities to receive feedback might have improved the workshops. Despite this feedback, it is not feasible on a national level to consider running longer workshops, such as those run by Merckaert et al.29 However, it may be useful to provide radiation therapists with more opportunities to practice their skills and receive feedback after participation in these initial workshops. The follow‐up workshops we held provided an opportunity to receive feedback on consultations they had conducted.
Analysis of the audio‐recording of the consultations that radiation therapists had with patients enabled the researchers to ascertain whether the self‐identified usefulness of the workshops translated into practice and determine further training needs. An alternative way for improving communication skills following workshops with nurses described by Wilkinson et al.35 involved audio recording patient consultations and workshop participants reviewing their own patient consultations. In our study, the facilitators reviewed the recordings based on the QA protocol and provided a subsequent workshop with feedback; however, if these workshops are implemented into practice it may be useful to implement a similar process as that described by Wilkinson et al.35
The follow‐up workshop held in our study enabled the facilitators to touch base with participants and provide specific feedback based on their performance. Much of the feedback focused on eliciting and responding to emotional cues, making adequate time and finding appropriate space. Merchant et al.36 similarly reported the need for radiation therapy departments to provide spaces for confidential discussions with patients.
As mentioned previously, this communication skills training formed part of the preparation required for radiation therapists participating in the larger ‘RT Prepare’ study. This larger study is currently underway and will examine whether the addition of two consultations with radiation therapists, one prior to CT planning and one prior to treatment, are effective in reducing patient anxiety and improving patient knowledge prior to receiving radiation therapy for breast cancer. We propose that communication skills training, focusing on both preparing patients for radiation therapy and eliciting and responding to emotional cues, may be beneficial to all radiation therapists, reduce patient anxiety and potentially reduce costs to the health care system. We anticipate that the communication skills developed by radiation therapists can also be applied to all patients with cancer, not just those receiving radiotherapy for breast cancer. If this research demonstrates that the RT Prepare intervention is effective this type of education could be implemented successfully into clinical practice Australia wide for the benefit of patients, health professionals and the healthcare system.
Limitations
This manuscript reports on the feedback provided by radiation therapists about the workshops. One limitation of the study is that we present only the results of the radiation therapists’ self‐assessed evaluations of the workshops and a summary of the main findings following review of the tape recordings in this manuscript. We have not collected patient perspectives on the communication skills of radiation therapists after participating in the workshops.
It would be beneficial to evaluate whether radiation therapists’ skills are improved substantially and these improvements are sustained over time following participation in these workshops. Running additional workshops and evaluations will allow for further testing of a range of health professional and patient outcomes in the radiation therapy setting.
Conclusion
Communication skills training consisting of two workshops to help radiation therapists to: prepare patients for radiation therapy, and elicit and respond to emotional cues, has the potential to improve communication with patients undergoing radiation therapy. Both communication skills workshops were necessary because they focused on different aspects of the communication radiation therapists have with patients in order to prepare them for treatment. The use of tape recording and a follow‐up session proved useful in providing radiation therapists with feedback about their performance. Ways of incorporating this opportunity need to be considered for future workshops run with radiation therapists. Further research and analysis is warranted to determine whether patient anxiety can be reduced as a result of improving communication and information provision for patients.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
This project is funded by Cancer Australia and Beyond Blue through the Priority Driven Collaborative Cancer Research Scheme. We thank Laura Emery, Michelle Rogers, Robyn French, Lisa McGivern and the teams at each of the sites who assisted us with the organisation of the workshops and overall conduct of the project. We also thank Veronica, the actor, for her involvement in all of the workshops.
J Med Radiat Sci 63 (2016) 232–241
References
- 1. Halkett GK, Kristjanson LJ, Lobb E, et al. Information needs and preferences of women as they proceed through radiotherapy for breast cancer. Patient Educ Couns 2012; 86: 396–404. [DOI] [PubMed] [Google Scholar]
- 2. Sanson‐Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Cancer 2000; 88: 226–37. [DOI] [PubMed] [Google Scholar]
- 3. Newell SA, Sanson‐Fisher RW, Savolainen NJ. Systematic review of psychological therapies for cancer patients: Overview and recommendations for future research. J Natl Cancer Inst 2002; 94: 558–84. [DOI] [PubMed] [Google Scholar]
- 4. Gamble K. Communication and information: The experience of radiotherapy patients. Eur J Cancer Care 1998; 7: 153–61. [DOI] [PubMed] [Google Scholar]
- 5. Long L. Being informed: Undergoing radiation therapy. Cancer Nurs 2001; 24: 463–8. [DOI] [PubMed] [Google Scholar]
- 6. Johnson J. “Living with radiotherapy”: The experiences of women with breast cancer. J Radiother Pract 1999; 1: 17–25. [Google Scholar]
- 7. Halkett GK, Kristjanson LJ, Lobb EA. ‘If we get too close to your bones they'll go brittle’: Women's initial fears about radiotherapy for early breast cancer. Psychooncology 2008; 17: 877–84. [DOI] [PubMed] [Google Scholar]
- 8. Halkett GK, Kristjanson LJ, Lobb E, O'Driscoll C, Taylor M, Spry N. Meeting breast cancer patients’ information needs during radiotherapy: What can we do to improve the information and support that is currently provided? Eur J Cancer Care 2010; 19: 538–47. [DOI] [PubMed] [Google Scholar]
- 9. D'haese S, Vinh‐Hung V, Bijdekerke P, et al. The effect of timing of the provision of information on anxiety and satisfaction of cancer patients receiving radiotherapy. J Cancer Educ 2000;15:223–7. [DOI] [PubMed] [Google Scholar]
- 10. Jefford M, Tattersall MH. Informing and involving cancer patients in their own care. Lancet 2002; 3: 629–37. [DOI] [PubMed] [Google Scholar]
- 11. Schofield P, Butow P, Thompson J, Tattersall M, Beeney L, Dunn S. Psychological responses of patients receiving a diagnosis of cancer. Ann Oncol 2003; 14: 48–56. [DOI] [PubMed] [Google Scholar]
- 12. Waller A, Forshaw K, Bryant J, Mair S. Interventions for preparing patients for chemotherapy and radiotherapy: A systematic review. Support Care Cancer 2014; 22: 2297–308. [DOI] [PubMed] [Google Scholar]
- 13. Halkett G, O'Connor M. What is the best way to support patients undergoing radiation therapy? J Med Radiat Sci 2015; 62: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martin K‐L, Hodgson D. The role of counselling and communication skills: How can they enhance a patient's ‘first day’ experience? J Radiother Pract 2006; 5: 157–64. [Google Scholar]
- 15. Halkett GK, Short M, Kristjanson LJ. How do radiation oncology health professionals inform breast cancer patients about the medical and technical aspects of their treatment? Radiother Oncol 2009; 90: 153–9. [DOI] [PubMed] [Google Scholar]
- 16. Halkett G, Merchant S, Jiwa M, et al. Effective communication and information provision in radiotherapy ‐ the role of radiation therapists. J Radiother Pract 2009; 9: 3–16. [Google Scholar]
- 17. Aranda S, Jefford M, Yates P, et al. Impact of a novel nurse‐led prechemotherapy education intervention (ChemoEd) on patient distress, symptom burden, and treatment‐related information and support needs: Results from a randomised, controlled trial. Ann Oncol 2012; 23: 222–31. [DOI] [PubMed] [Google Scholar]
- 18. Halkett GK, Schofield P, O'Connor M, et al. Development and pilot testing of a radiation therapist‐led educational intervention for breast cancer patients prior to commencing radiotherapy. Asia Pac J Clin Oncol 2012; 8: e1–8. [DOI] [PubMed] [Google Scholar]
- 19. Halkett GK, O'Connor M, Aranda S, et al. Pilot randomised controlled trial of a radiation therapist‐led educational intervention for breast cancer patients prior to commencing radiotherapy. Support Care Cancer 2013; 21:1725–33. [DOI] [PubMed] [Google Scholar]
- 20. Halkett G, O'Connor M, Aranda S, et al. Protocol for the RT prepare trial: A multiple‐baseline study of radiation therapists delivering education and support to women with breast cancer who are referred for radiotherapy. BMJ Open 2014;4:e006116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Butow P, Cockburn J, Girgis A, et al. Increasing oncologists’ skills in eliciting and responding to emotional cues: Evaluation of a communication skills training program. Psychooncology 2008; 17: 209–18. [DOI] [PubMed] [Google Scholar]
- 22. National Breast Cancer Centre . Elciting and responding to emotional cues. Evidence from the literature and recommended steps. Camperdown, NSW: National Breast Cancer Centre, 2007. [Google Scholar]
- 23. Gysels M, Richardson A, Higginson I. Communication training for professionals who care for patients with cancer: A systematic review of effectiveness. Support Care Cancer 2004; 12: 692–700. [DOI] [PubMed] [Google Scholar]
- 24. Kissane DW, Bylund CL, Banerjee SC, et al. Communication skills training for oncology professionals. J Clin Oncol 2012; 30: 1242–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grainger MN, Hegarty S, Schofield P, White V, Jefford M. Discussing the transition to palliative care: Evaluation of a brief communication skills training program for oncology clinicians. Palliat Support Care 2010; 8: 441–7. [DOI] [PubMed] [Google Scholar]
- 26. De Vries AM, de Roten Y, Meystre C, Passchier J, Despland JN, Stiefel F. Clinician characteristics, communication, and patient outcome in oncology: A systematic review. Psychooncology 2014; 23: 375–81. [DOI] [PubMed] [Google Scholar]
- 27. Moore PM, Rivera Mercado S, Grez Artigues M, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3:CD003751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O'Connor M, Fisher C, French L, Halkett G, Jiwa M, Hughes J. Exploring the community pharmacist's role in palliative care: Focusing on the person not just the prescription. Patient Educ Couns 2011; 83: 458–64. [DOI] [PubMed] [Google Scholar]
- 29. Merckaert I, Delevallez F, Gibon AS, et al. Transfer of communication skills to the workplace: Impact of a 38‐hour communication skills training program designed for radiotherapy teams. J Clin Oncol 2015; 33: 901–9. [DOI] [PubMed] [Google Scholar]
- 30. Baile WF. Training oncology practitioners in communication skills. J Pediatr Hematol Oncol 2011; 33(Suppl. 2): S115–22. [DOI] [PubMed] [Google Scholar]
- 31. Pendleton D, Schofield T, Tate P, Havelock P. The Consultation: An Approach to Learning and Teaching. Oxford University Press, Oxford, 1982. [Google Scholar]
- 32. National Breast Cancer Centre, National Cancer Control Initiative . Clinical Practice Guidelines for the Psychosocial Care of Adults with Cancer. National Breast Cancer Centre, Camperdown, New South Wales, 2003. [Google Scholar]
- 33. National Breast Cancer Centre . Guidelines for Detecting and Addressing Emotional Cues. National Breast Cancer Centre, Camperdown, NSW, 2007. [Google Scholar]
- 34. Radiation Therapy Advisory Panel . 2011 Radiation Therapy Workforce Survey. Spectrum, Australian Institute of Radiography; 2012; Feburary: 20–2. [Google Scholar]
- 35. Wilkinson SM, Gambles M, Roberts A. The essence of cancer care: The impact of training on nurses’ ability to communicate effectively. J Adv Nurs 2002; 40: 731–8. [DOI] [PubMed] [Google Scholar]
- 36. Merchant S, O'Connor M, Halkett G. Time, space and technology in radiotherapy departments: How do these factors impact on patients’ experiences of radiotherapy? Eur J Cancer Care (Engl) 2015; doi: 10.1111/ecc.12354. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]


