Abstract
A pathological fracture is one which occurs in diseased bone with trivial trauma or even without it. However, fracture occurring as a result of significant injury can masquerade underlying ominous bone pathology, which is highly likely to be missed in the garb of overwhelming traumatic aetiology.
Pathological fracture as the manifestation of tumour in children less than 10 years of age is rare.1, 2 Fracture following significant trauma masquerading as underlying malignancy is even rarer. We report a case of 7-year-old male child, he had history of significant trauma with fracture shaft of femur, pathology was “missed” initially in the outset of trauma and on subsequent follow up it was found to be osteosarcoma.
Keywords: Osteosarcoma, Femur, Pathological fracture, Child, Management
1. Case report
A 7-year-old male child presented in orthopaedic emergency department in January 2014 with alleged history of fall from around 10 ft height. On presentation primary and secondary survey of the patient was done and the child was resuscitated. Patient had significant swelling and deformity of the right thigh clinically suggestive of fracture shaft of femur. There was no prior history of previous injury at the same site or any other site of the body.
Careful review of digital plain radiographs revealed long spiral fracture of the femur along with buckling of cortex in the lateral metaphyseal area of distal femur (Fig. 1). Different management options (surgical versus nonoperative) for the child were offered, to which parents opted for non-operative treatment by skeletal traction. Informed consent was taken from parents and upper tibial skeletal traction was applied in the involved limb. Patient was kept on skeletal traction in ward with daily observations of the extremity traction assembly and after 3 weeks hip spica was applied after the removal of skeletal traction and he was discharged.
Fig. 1.

Plain radiograph at the time of presentation after fall from height shows spiral fracture of femur shaft with buckling at the lateral metaphyseal region.
Three months post-trauma patient presented in the outdoor department, with complaints of pain and significant swelling over the right distal thigh region. On clinical examination there was large circumferential swelling over right distal thigh region, with tense overlying skin and dilated veins (Fig. 2). The local temperature was raised, the mass was tender to touch and had variegated consistency. The patient was pale and there was no significant lymphadenopathy and no distal neurovascular deficit. Splintage of the involved limb was done, routine haematological investigations and X-ray of the right hip with whole thigh and right knee antero-posterior and lateral view was done. Digital plain radiographs showed united fracture shaft of femur with radiodense lesion over the metaphyseal region of the distal femur with zones of lucency extending to the diaphysis, along with loss of normal trabecular pattern of the bone and soft tissue swelling with loss of soft tissue plains (Fig. 2). Differential diagnosis of osteosarcoma or Ewing's sarcoma of femur was kept on the basis of plain radiograph. MRI of the involved limb showed hypointense T1 lesion and hyperintense T2 lesion in the lower metaphysis and involving the muscle plains. There was intramedullary extension of the lesion to whole diaphysis of femur. The physeal plate was not breached and knee joint was not involved (Fig. 3).
Fig. 2.
(a, b) Three months post-trauma, circumferential swelling of whole of thigh, shiny skin and dilated veins, (c) plain radiograph after three months shows united fracture shaft of femur with radiodense lesion at the metaphyseal region with zone of lucency, loss of soft tissue plain and normal trabecular pattern of bone.
Fig. 3.
T1 and T2 weighted images on MRI of whole lower limb shows lesion at the metaphyseal region which is involving the muscular plain and intramedullary extension involving whole of femur, there is sparing of physeal plate of distal femur.
On the basis of clinicoradiological investigations, differential diagnosis of osteosarcoma and Ewing's sarcoma was kept. Open biopsy of the involved lesion was performed, histological examination confirmed the lesion to be high grade osteosarcoma of osteoblastic type. CT scan of chest and abdomen was normal, with no signs suggestive of metastasis. As the lesion was aggressive and extracompartmental with whole of the femur involved, disarticulation of the hip was performed after taking informed consent from parents. Patient was started on chemotherapy postoperatively. He was started on cisplatin (60 mg/m2), doxorubicin (75 mg/m2) and high dose methotrexate (12 mg/m2). He has been given four cycles of chemotherapy post-surgery with each cycle of 21 days. After 9 months post-surgery, patient has no recurrence at the local site but PET scan shows metastasis to the opposite proximal femur, lumbar spine and lower lobe of lungs (Fig. 4).
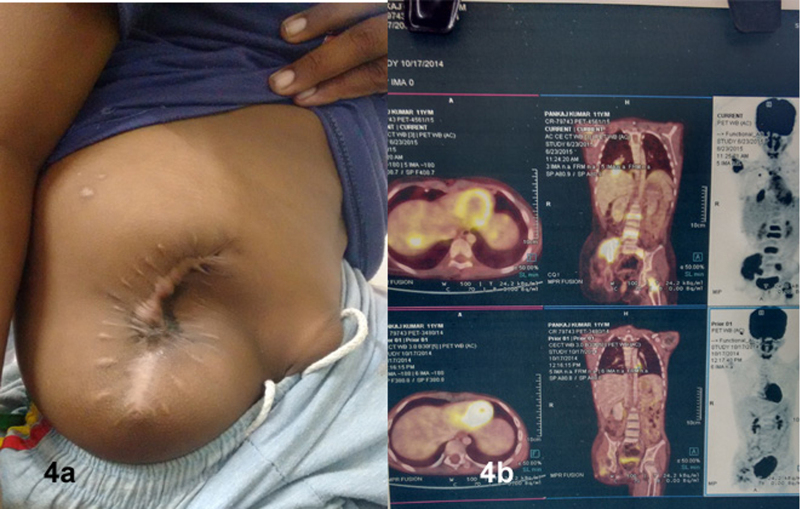
Fig. 4.
(a) Amputations stump 10 months following surgical dislocation of hip, the stump is healthy and no sign of recurrence or dehiscence at the local site. (b) PET CT shows metastasis to opposite proximal femur, lumbar spine and lower lobes of both lungs.
2. Discussion
In the reported case, 7-year-old child had history of significant trauma rather than trivial trauma. The overwhelming presentation of significant history of trauma with presence of a fracture at two sites in the femur i.e. a spiral fracture in the upper and middle third junction of the diaphysis and a distal metaphyseal buckling fracture (which rarely seen in a pathological long bone fracture), absence of any overt clinical signs of underlying metaphyseodiaphyseal malignancy at presentation, along with progression to early clinical union of the fracture masqueraded the presence of an underlying osteosarcoma which went unrecognized at the time of presentation and in the clinical setting of significant trauma despite careful review of good quality digital radiographs by team of senior orthopaedic surgeons. This led to an inadvertently missed initial diagnosis of probable bony malignancy in a femur fractured at two sites.
Further, clinically pathological long bone fractures are typically transverse and minimally displaced unlike in this case. There are several issues which remain difficult to explain in the current clinical scenario. The primary malignancy remained clinically non-apparent in the setting of displaced spiral femur fracture despite daily clinical observation and examination of the extremity. Hence significant trauma acted as a masquerade of underlying bony malignancy which probably was in “early” stage of pathogenesis and hence not clinically presentable. The uneventful timely fracture union at the time when suspicion of malignancy was first raised is also unusual, since pathological fracture rarely unite spontaneously.
Although an early diagnosis in this case would have been ideal but whether eventual outcome could be any different in case the bony malignancy was not missed initially is also open to debate. Early diagnosis probably would have resulted in early institution of chemotherapy and thus could have effect on prevention of metastasis. In the setting of fracture, limb salvage would have been contraindicated.
Limb salvage surgery is preferred treatment for malignant bone tumours in paediatric patients at most institutions; however, amputation still plays a role, especially when a satisfactory surgical margin cannot be obtained, or the residual limb will be non-functional. Several studies have demonstrated no adverse effect on local recurrence and overall survival in patients undergoing limb salvage surgery compared with those undergoing amputation.3, 4, 5, 6
In the current study the tumour had breached the compartmental barrier and there was intramedullary spread in the whole of femur; the hip and knee joint were spared as observed on MRI. The lesion was extensive and limb salvage could not be done and thus hip disarticulation was done.
The overwhelming presentation of significant trauma resulting in a long bone fracture at two or more sites in a child can masquerade an underlying bony malignancy by virtue of predominant signs and symptoms secondary to trauma. Extensive caution should be executed while radiographic review in this scenario since buckling metaphyseal fracture and radiodensities noted in such scenario should raise high index of suspicion of further detailed analysis to rule out any primary bony malignancy.
Conflicts of interest
The authors have none to declare.
Contributor Information
Amit Srivastava, Email: amitsrvstv00@gmail.com.
Aditya N. Aggarwal, Email: dranaggarwal@hotmail.com.
Puneet Mishra, Email: drpuneetmishra@gmail.com.
Dheeraj Bhateja, Email: drdheerajmamc@gmail.com.
References
- 1.Verheven E., De Boeck H., Opedecam P. Osteosarcoma appearing as a pathological fracture. Acta Orthop Belg. 1991;57(4):437–441. [PubMed] [Google Scholar]
- 2.Jackson W.F., Theologis T.N., Gibbons C.L., Mathews S., Kambouroglou G. Early management of pathological fracture in children. Injury. 2007;38:194–200. doi: 10.1016/j.injury.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 3.Abudu A., Sferopoulos N.K., Tillman R.M., Carter S.R., Grimer R.J. The surgical treatment and outcome of pathological fractures in localised osteosarcoma. J Bone Jt Surg Br. 1996;78B:694–698. [PubMed] [Google Scholar]
- 4.Natrajan M.V., Govardhan R.H., Williams S., Rajagopal T.S. Limb salvage surgery for pathological fractures in osteosarcoma. Int Orthop. 2000;24:170–172. doi: 10.1007/s002640000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Papagelopoulos P.J., Mavrogenis A.F., Savvidou O.D., Benetos I.S., Galanis E.S., Soucacos P.N. Pathological fractures in primary bone sarcomas. Injury. 2008;39(4):395–403. doi: 10.1016/j.injury.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Saraph V., Linhart W.E. Modern treatment of pathological fractures in children. Injury. 2005;36S:A64–A74. doi: 10.1016/j.injury.2004.12.015. [DOI] [PubMed] [Google Scholar]