Abstract
Fat embolism syndrome presented with the classical triad of respiratory manifestations (95%), cerebral effects (60%) and Petechial rash (33%). Focal neurological symptoms in the form of combined bilateral cortical blindness and motor aphasia even prior to respiratory symptoms have been never reported in previous literature. We describe a case of these rare focal neurological symptoms secondary to the fat embolism syndrome in a young adult male following closed femur fracture.
Keywords: Femur fracture, Fat embolism syndrome, Cortical blindness, Motor aphasia, Gurd's criteria
1. Introduction
Fat embolism is a condition of presence of fat globules in circulation generally after fracture of long bones, pelvis or other major trauma.1, 2, 3 This condition is quite common after major orthopedic trauma and is largely subclinical but the fat embolism syndrome is an uncommon serious condition characterized by a clinical triad of dyspnea, petechiae and clinical confusion.2 Its incidence varies from 1 to 33%, depending upon the number and fractured bone.3
Neurological features resulting from cerebral embolism frequently present in the early stages and often occur after the development of respiratory distress. The changes range across a wide spectrum from mild confusion and drowsiness through to severe seizures. The most common presentation is with an acute confusional state, but focal neurological signs, including hemiplegia, aphasia, apraxia, visual field disturbances and anisocoria are not so common.1 There is only a few case reports in English literature presented with either bilateral cortical blindness or motor aphasia.6, 7, 8, 9 Fortunately, almost all neurological deficits are transient and fully reversible.6, 7, 8, 9 We report a case unusual presentation of fat embolism syndrome (FES) in form of transient post-traumatic cortical blindness and motor aphasia after unilateral femur fracture in young adult male which was managed successfully with complete functional recovery, emphasizing on high degree of suspicion and prompt management.
2. Case report
A 20-year-old male reported to our trauma center emergency with a closed fracture of the left femoral shaft within 6 h of injury. Patient was conscious, well oriented to time, place and person and hemodynamically stable at the admission. The patient had no history any loss of consciousness, vomiting, ENT bleed or seizure till the time of admission. Thoracic, abdominal and pelvic injuries were ruled out with thorough clinical and radiological examination. His vitals were stable, except slight tachycardia (heart rate 112 min–1), borderline tachypnea (respiratory rate 24 min–1), blood pressure 100/70 mm Hg, and oxygen saturation was 98% on room air at the time of admission. Patient's limb was immobilized with Thomas splint with fixed traction and resuscitated adequately. A radiograph of femur showed type 32A2 fracture (Fig. 1.1). Chest radiograph was clear (Fig. 1.2). Routine pre-operative blood investigations at that time of admission including complete hemogram, renal function tests, liver function tests, serum electrolytes and random blood sugar were within normal limits.
Fig. 1.1.
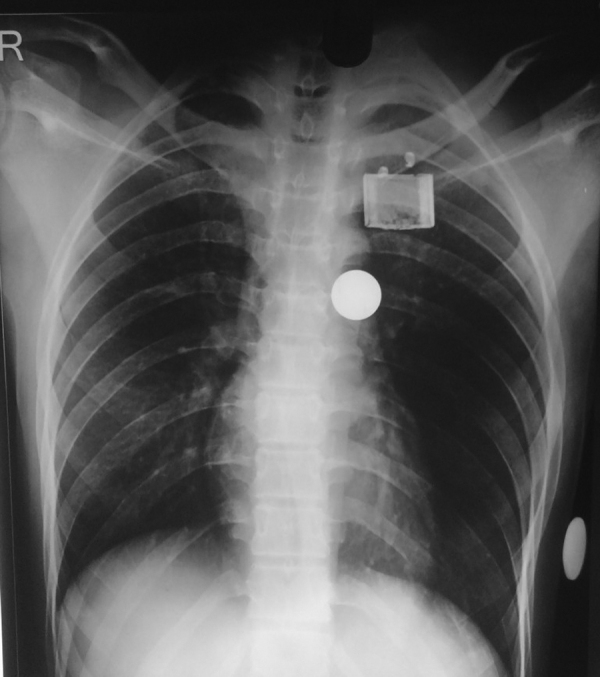
Chest radiograph at the time of admission without any infiltrate.
Fig. 1.2.

X-ray of right femur fracture.
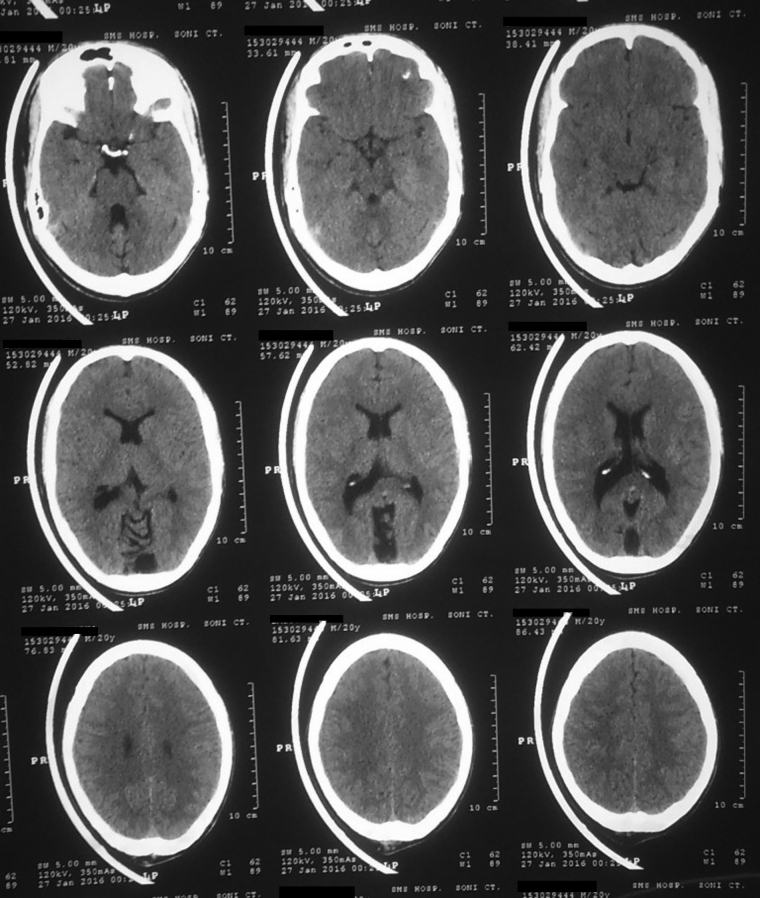
After 8 h of admission, patient started complaining of blurring of vision. He also developed sudden loss of vision and slurring of speech along with agitation an hour later. Also there was fall in saturation as SPO2 was 88%. He soon developed breathlessness and complete aphasia within 2 h and SPO2 was declining in spite of nasal oxygen. The pulse rate was 130 min–1, blood pressure 108/70 mm Hg, respiratory rate 30 min–1. The patient was intubated and put on mechanical ventilation with CPAP mode. ECG was unremarkable showing sinus tachycardia only. An arterial blood gas analysis showed PAO2 of 86% on FIO2 and had put normal electrolytes. An urgent CT scan of brain was done which was normal (Fig. 1.3).
Fig. 1.3.
Normal NCCT Brain of patient.
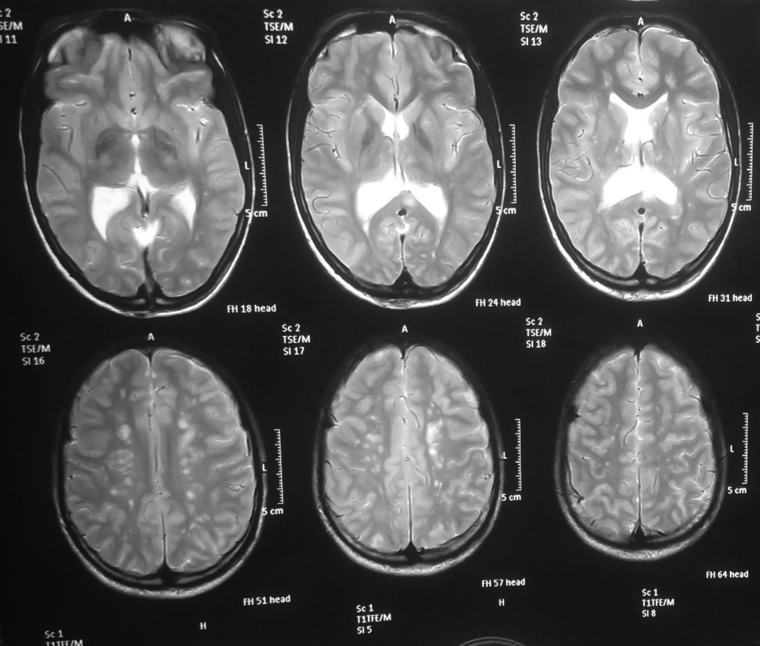
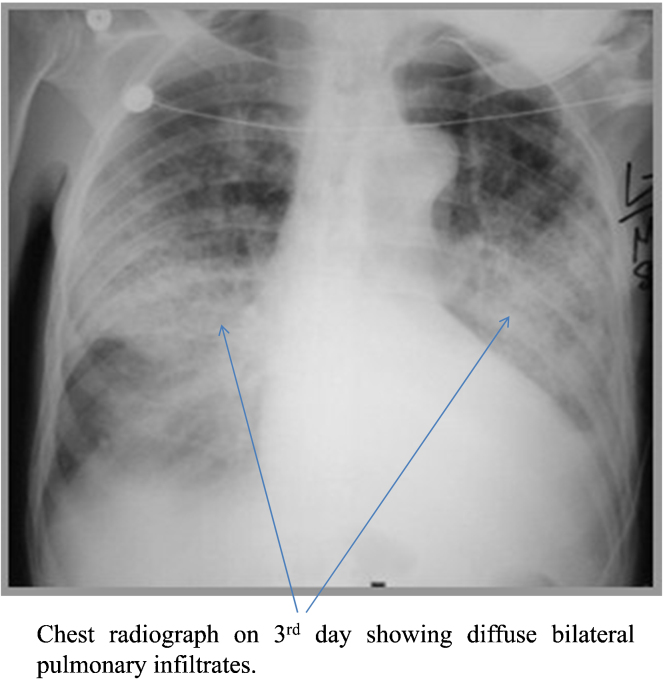
Blood work on the next day showed hemoglobin of 8.6 g/dl, platelet count of 1.4 lakhs/mm3, normal TLC, DLC, electrolytes, renal function and liver function tests. Urine for fat globules was negative. Ophthalmologist report concluded as cortical blindness because of normal fundoscopy and papillary reaction. MRI brain was performed and high resolution T1, T2, FLAIR images obtained in sagittal and axial planes in a 3.0 T scanner. MRI showed relative hypointense areas on T1-weighted images and T2-weighted images showed multiple nonconfluent areas of high signal intensity in the corpus callosum, periventricular and deep white matter, basal ganglia, thalami and cerebellar hemispheres likely due to a shower of micro emboli which causes breakdown of the blood–brain barrier with vasogenic edema or cytotoxic edema or both (Fig. 1.4). Lesions were characteristically located along the boundary zones of the major vascular territories. CT pulmonary angiography was done which showed the presence of irregularity in second and third order branch of descending branch of left pulmonary artery due to hypodense lesion in lumen probably thromboembolic in nature (Fig. 1.5). Chest radiograph which was clear initially showed diffuse bilateral pulmonary infiltrates on day 3 (Fig. 1.6). So the patient was diagnosed with fat embolism syndrome according to Gurd's criteria.4
Fig. 1.4.
MRI with multiple small infarcts in corpus callosum, periventricular and deep white matter, basal ganglia, thalami and cerebellar hemispheres.
Fig. 1.5.
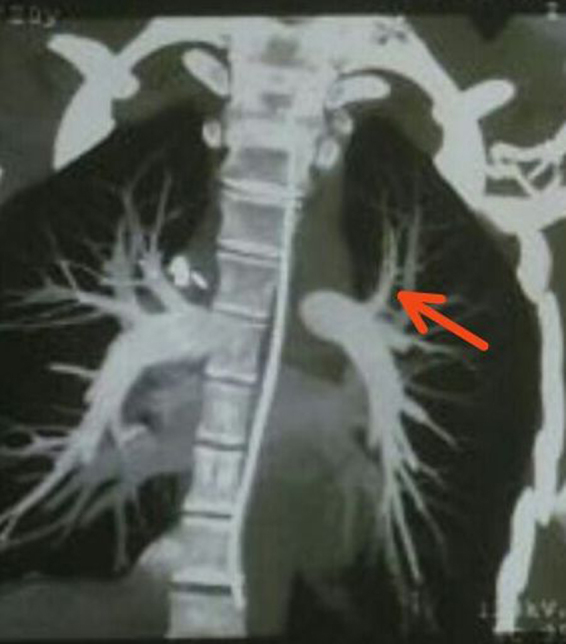
CT pulmonary angiography showing the presence of irregularity in second and third order branch of descending branch of left pulmonary artery.
Fig. 1.6.
Chest radiograph on 3rd day showing diffuse bilateral pulmonary infiltrates.
The patient was managed symptomatically and remained hemodynamically stable throughout his hospital stay. He was extubated 5 days later, and he recovered from his blindness and speech loss completely by the 7th day. The patient was finally operated on the 11th day with an interlocking femur nail without reaming. The postoperative recovery was uneventful and the patient was discharged on his 14th day of admission.
3. Discussion
This case report was an atypical presentation of fat embolism syndrome because of early focal neurological symptoms in the form of sudden onset cortical blindness along with motor aphasia, even prior to respiratory symptoms. The diagnosis of fat embolism was made on this patient on the basis of Gurd and Wilson criteria,4 with 2 major criteria (central nervous system involvement disproportionate to hypoxemia and respiratory insufficiency) and 2 minor criteria (tachycardia and pyrexia) and 2 laboratory findings (fall in hemoglobin from 12.2 to 8.6 g/dl and sudden thrombocytopenia from 3.27 to 1.4 lakhs/mm3). Later on the chest radiograph and MRI brain further confirmed our diagnosis. CT angiogram showing partial vessel block which is unusual and against the more common changes i.e. bilateral ground-glass opacities and thickening of the interlobular septa.11
The differential diagnoses of our case were head injury, pulmonary embolism and cerebrovascular accident, but head injury was ruled out by detailed history and radiological investigations, pulmonary embolism was also ruled out on the basis of lack of pre-disposing factors, clinical history, ECG and d-dimer assay and cerebrovascular accident was ruled out because of age of patient, the absence of previous history of hypertension and on the basis of MRI findings. The rapidity of onset of symptoms was noteworthy in our case, with complaint of deteriorating vision along with aphasia as the first symptom and complete recovery of both later on. Classically, the symptoms of fat embolism syndrome appear in 24–72 h with a clinical triad of lung, brain and skin involvement, but in our case onset of symptoms were early and atypical. The respiratory symptom is present in 95% of the cases and is usually the earliest symptom to appear. Dyspnea, tachypnea and hypoxemia are most frequently seen as early findings.1, 2, 3
Nervous system involvement is present in 60–86% of cases; often occur after the development of respiratory distress. The changes range across a wide spectrum from mild confusion and drowsiness through to severe seizures. The more common presentation is an acute confusional state, but focal neurological signs, including hemiplegia, aphasia, apraxia, visual field disturbances and anisocoria have been described but uncommon.1, 10 The presence of both cortical blindness and motor aphasia has been never described in previous English literature.
Magnetic resonance imaging (MRI) with diffusion-weighted sequences is the most sensitive technique for the detection of fat embolism syndrome (FES). It shows the multiple high intensity and non confluent injuries in the white and gray matter.10 MRI of our case was showing multiple small infarcts in the corpus callosum, periventricular and deep white matter, basal ganglia, thalami and cerebellar hemispheres likely due to a shower of micro emboli of fat globules.
A petechial rash is the last component to develop and is present in up to 60% of cases in the conjunctiva, oral mucous membrane and skin folds of the upper body, especially the neck and axilla,1, 2, 3 these were seen our case also (Fig. 1.7). Ocular manifestation of fat embolism syndrome is rare and mostly because of ‘Purtscher's retinopathy’, seen as cotton wool exudates, macular edema and macular hemorrhage,5 but it was excluded in our case from normal fundoscopic examination and a diagnosis of cortical blindness due to fat embolism was made.
Fig. 1.7.

Clinical photograph showing axillary petechiae.
In conclusion, fat embolism syndrome may present with early focal neurological symptoms in the form of acute bilateral blindness along with motor aphasia even before to respiratory manifestations so possibility of FES should be kept in mind while dealing with these kind of patients.
Author's contribution
RKL – conceived the idea and co-wrote the paper. UKM – analyzed the notes, acquisition, and contributed to the discussion. RKM – Analyze the notes and contributed to the discussion. PA and MS – co-wrote the paper and revised it critically before submission.
Source of support/funding
None declared.
Conflicts of interest
The authors have none to declare.
Contributor Information
Umesh Kumar Meena, Email: drumesh_meena@yahoo.co.in.
Ravinder Kumar Lamoria, Email: drravisms@yahoo.com.
Ravi Kant Millan, Email: orthodoc.ravi009@gmail.com.
Piyush Agarwal, Email: piyushagarwal87@gmail.com.
Mahendra Singh, Email: drmstak1988@yahoo.com.
Mahesh Chand Bansal, Email: dr.maheshbansal@gmail.com.
References
- 1.Jain S., Mittal M., Kansal A., Singh Y., Kolar P.R., Saigal R. Fat embolism syndrome. JAPI. 2008;56(April):245–249. [PubMed] [Google Scholar]
- 2.Ten Duis H.J. The fat embolism syndrome. Injury. 1997;28:77–85. doi: 10.1016/s0020-1383(96)00085-x. [DOI] [PubMed] [Google Scholar]
- 3.Levy D. The fat embolism syndrome. A review. Clin Ortop. 1990;261:281–286. [PubMed] [Google Scholar]
- 4.Gurd A.R. Fat embolism: an aid to diagnosis. J Bone Joint Surg Br. 1970;52(4):732–737. [PubMed] [Google Scholar]
- 5.Suresh S.S., Philips G.M., Balachandra C. Sudden loss of vision following bilateral closed femoral nailing: a case of Purtscher's retinopathy. Acta Orthop Traumatol Turc. 2013;47(4):295–298. doi: 10.3944/aott.2013.2954. [DOI] [PubMed] [Google Scholar]
- 6.Saeed-Banadaky S.H., Valizadeh S., Ghilian M. Motor aphasia as a rare presentation of fat embolism syndrome; a case report. Arch Bone Joint Surg. 2015;3(1):64. [PMC free article] [PubMed] [Google Scholar]
- 7.Nandi R., Krishna H.M., Shetty N. Fat embolism syndrome presenting as sudden loss of consciousness. J Anaesthesiol Clin Pharmacol. 2010;26(4):549. [PMC free article] [PubMed] [Google Scholar]
- 8.Lim S.F., Chong C.K., Ng P., Koh S. Transient post-traumatic cortical blindness due to bilateral occipital lobe infarcts in a multiply-injured patient: a case report. Inj Extra. 2013;44(6):54–57. [Google Scholar]
- 9.Shahrulazua A., Ariff M.S., Aziz M.A. Cortical blindness in fat embolism syndrome following fracture manipulative procedure. Malays Ophthalmol J. 2010;4:35–38. [Google Scholar]
- 10.Salazar J.A., Romero F., Padilla F., Arboleda J.A., Fernandez O. Neurological manifestations of fat embolism syndrome. Neurologia (Barcelona, Spain) 1995;10(2):65–69. [PubMed] [Google Scholar]
- 11.Malagari K., Economopoulos N., Stoupis C. High-resolution CT findings in mild pulmonary fat embolism. CHEST J. 2003;123(April (4)):1196–1201. doi: 10.1378/chest.123.4.1196. [DOI] [PubMed] [Google Scholar]