Abstract
Introduction Fracture of the scaphoid bone is the most common fracture of the carpus. However, the fracture union occurs late or may not heal. Sometimes, fracture healing requires prolong immobilization. Because of potential for joint stiffness, muscle atrophy, or the inability to use the hand during and after prolonged immobilization, there is great incentive to develop therapies that will accelerate bone healing and allow a quick return to work. To date, the effect of platelet-rich plasma (PRP) on scaphoid fracture has not been studied. We aimed to assess the effect of intra-articular PRP injection on union: pain, range of motion, and function in patients with scaphoid fracture.
Hypothesis Union: pain reduction and functional improvement can be noticed after PRP use in scaphoid fracture.
Materials and Methods A randomized controlled trial was designed with 14 patients with scaphoid fractures (Herbert type B2). Casting was done for them. Seven patients received intra-articular autologous PRP. Patients were followed up 2 weeks after casting using radiography and then at 2 months using radiography and computed tomography (CT) scan to check bone healing. Then patients were followed up for 3 and 6 months and after evaluation of healing by CT scan, the patient-rated wrist evaluation questionnaire was completed and the range of motion of the wrist was measured.
Results Analysis revealed significant improvement in pain at rest, as well as during specific and usual activities following PRP injection in the case group. However, no statistically significant difference in wrist motion including radial and ulnar deviation, flexion, and extension was found in 6 months follow-up except some improvement in ulnar deviation after 3 months. However, this study showed that scaphoid union occurred earlier in the case group, but it was not statistically significant.
Conclusion PRP may have a significant effect on pain reduction at rest and amount of difficulty in functions including specific and usual activities in patients with scaphoid fractures.
Level of Evidence This is a level III, therapeutic trial.
Keywords: scaphoid fracture, PRP, union, pain, function, PRWE
Introduction
Union of the scaphoid fracture, which is the most common fracture of the carpus, occurs late or may not even heal. Nonunion or delayed union is the most common complications in this fracture which can lead to pain and disability.1 2 Also, fracture healing might require prolong immobilization. Prolonged immobilization can cause stiffness, muscle atrophy, or delay in returning to work.3 4 To reduce complications of fracture care and immobilization, special additional treatment may be considered to improve bone healing. Recently, attention is paid to the biologic agents to influence the body's natural process of bone healing to achieve better outcome. Platelet-rich plasma (PRP), which is a concentration of platelets in a small volume of plasma, has gained widespread use to improve fracture union and function in a variety of clinical applications.5 6 7 To date, the use of PRP has not been studied for its effects on scaphoid fracture.
We aimed to assess the effect of intra-articular PRP injection on union: pain, range of motion, and function in patients with scaphoid fracture.
Patients and Methods
We studied 14 randomly selected patients with scaphoid fractures treated at a referral university hospital from September 2013 to 2014. Our treatment protocols were approved by the local ethics committee and a written informed consent was signed or fingerprinted by each patient.
We included patients who had acute, unilateral nondisplaced middle-third scaphoid fractures type B2 according to Herbert classification.8 Patients who refused to participate in the study had displaced scaphoid fractures, proximal pole fractures, fracture dislocations of the corpus or comminuted fracture (Herbert types B4 and B5), presentation of > 7 days after injury, additional fracture of the wrist, previous wrist joint disease, and previous limited range of motion of the wrist joint were excluded.
We used Arthrex ACP (Autologous Conditioned Plasma) (Beasat Industrial Complex System, Tehran, Iran) double syringe system for PRP preparation. Several previous studies approved this system for PRP preparation and the product included concentrated growth factors.9 10 11 According to this protocol if PRP is going to be used within 30 minutes of blood withdrawal, the use of anticoagulant was not necessary. Approximately 20 mL of venous blood was slowly taken from the patients' hand at a rate of 1 mL every 2 seconds. The sample was centrifuged at 1,200 RPM for 5 minutes in the operation room under aseptic conditions. The supernatant of the first tube was transferred to the second tube and centrifuged at 2,600 RPM for 6 minutes. The final product was 1.5 mL of PRP.
The skin of the dorsum of the wrist joint was prepped and draped and 1.5 mL PRP was extracted and injected in radiocarpal joint from dorsal approach in a sterile condition using a 22-G needle. All injections in the radiocarpal joint were performed in less than 20 minutes after sampling.
The patients in the case and control groups received injections of PRP (1.5 mL) and normal saline (1.5 mL) in the wrist joint, respectively. Then, long scaphoid cast was applied. After 2 weeks, the first visit was done and radiography was taken to check any displacement or angulation. After 6 weeks, the second visit was done and long scaphoid cast was changed to short scaphoid cast. After 2 months, the fracture was checked using radiography and computed tomography (CT) scan (general electric/bright speed 8 slices). If the fracture was healed, the cast was removed and motion of the wrist was started under supervision of a physiotherapist. At 3 and 6 months after the operation, the patients were visited and fracture healing was checked using CT scan. Also, at each visit, the patient-rated wrist evaluation (PRWE) questionnaire was completed and range of motion of the wrist including flexion, extension, ulnar deviation, and radial deviation was measured and recorded. The PRWE, which evaluate pain and function, contains 15 items: a 5-item pain subscale (one question on frequency and four questions on pain intensity), a 6-item specific activities subscale, and a 4-item usual activities subscale. Special activities include pushups from a chair using affected hand, carrying a 10-lb object by the affected hand, using bathroom tissue by the affected hand, twisting door knobs using the affected hand, cutting meat using a knife by the affected hand, and closing buttons of a shirt. Usual activities that were evaluated include work (job or usual everyday work, recreational activities), personal care activities (dressing, washing), and household work (cleaning, maintenance). Patients rate their difficulty in all domains of function. Pain and function questions are answered from 0 (no pain) to 10 (the worst pain or greatest impairment). Individual subscales can be totaled. Previous publications support the PRWE's reliability, validity, responsiveness, and use for scaphoid fractures.12 13
Data were analyzed using SPSS software (SPSS Inc., Chicago, Illinois, United States). Variants were time of union: range of motion of the wrist (flexion, extension, ulnar deviation, and radial deviation), pain score, and functional evaluation (specific activities, usual activities). Descriptive data analysis of the items on the PRWE was done using SPSS software, version 18 (SPSS Inc.). Comparison of quantitative variables was conducted by Student t-test between the two groups. A p-value of less than 0.05 was considered statistically significant.
Results
The demographic and clinical features of the patients are presented in Table 1. No systemic or local complications were found at any time. We found a significant improvement in pain at rest, and total function (specific and usual activities) scores following PRP injection in the case group compared with the control group (Figs. 1 and 2). However, no statistically significant difference in wrist motions including radial deviation, ulnar deviation, flexion, and extension was found at 6 months follow-up, except for some improvement in ulnar deviation at 3 months follow-up. Also, this study shows that scaphoid union occurred earlier in the case group, but it was not statistically significant.
Table 1. The demographic and clinical features of the patient.
| Age (mean) | Fracture side (right/left) | Sex(male/female) | |
|---|---|---|---|
| Case (N = 7) | 31.71 | 5/2 | 7/0 |
| Control (N = 7) | 33.71 | 6/1 | 7/0 |
Fig. 1.
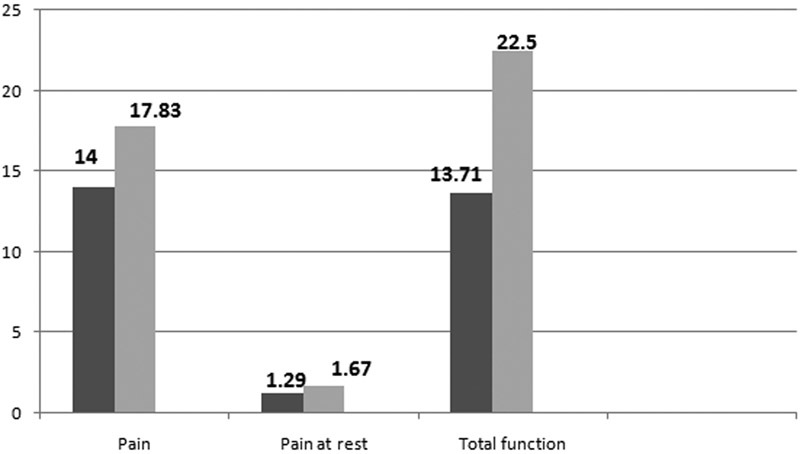
Scores of pain, pain at rest, and total function in 3 months follow-up in the two groups. Black, the case group; gray, the control group.
Fig. 2.
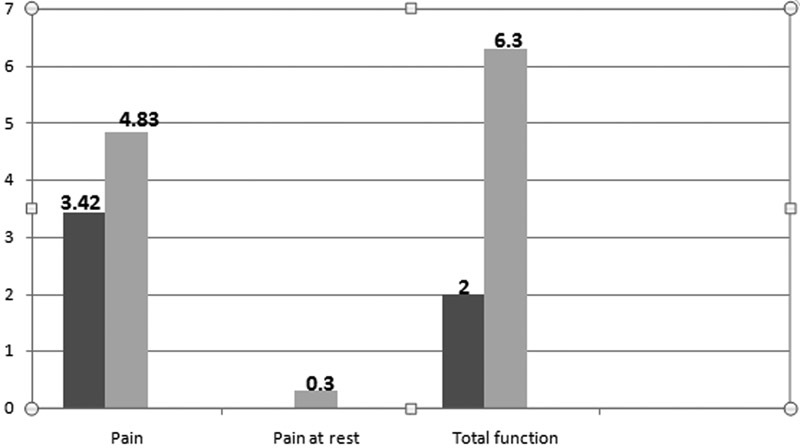
Scores of pain, pain at rest, and total function in 6 months follow-up in the two groups. Black, the case group; gray, the control group.
The comparison of the time to union: pain, usual and specific activities values, and wrist motions between the two groups are shown in Tables 2–4, respectively.
Table 2. Percentage of the healed fractures in 2nd, 3rd, and 6th months.
| Healed fracture (2nd mo) | Healed fracture (3rd mo) | Healed fracture (6th mo) | |
|---|---|---|---|
| Case (N = 7) | 5 (71.4%) | 7 (100%) | 7 (100%) |
| Control (N = 7) | 3 (42.8%) | 6 (85.7%) | 6 (85.7%) |
| p-Value | 0.59 | 0.99 | 0.99 |
Table 3. Scores of pain, pain at rest, and total function in 3 and 6 months follow-up in the two groups.
| Pain (3 mo) | Pain (6 mo) | Pain at rest (3 mo) | Pain at rest (6 mo) | Total function (3 mo) | Total function (6 mo) | ||
|---|---|---|---|---|---|---|---|
| Case (n = 7) | Mean | 14 | 3.42 | 1.29 | 0.00 | 13.71 | 2 |
| Max | 23 | 5 | 3 | 0.00 | 21 | 3 | |
| Min | 8 | 2 | 0 | 0.00 | 9 | 0.0 | |
| Control (n = 6) | Mean | 17.83 | 4.83 | 1.67 | 0.30 | 22.5 | 6.3 |
| Max | 26 | 8 | 4 | 1 | 26 | 9 | |
| Min | 14 | 3 | 0 | 0 | 20 | 4 | |
| p-Value | 0.22 | 0.23 | 0.22 | 0.03 | 0.014 | 0.002 | |
Table 4. Range of motion in 3 and 6 months follow-up in the two groups.
| Flexion (3 mo) | Flexion (6 mo) | Extension (3 mo) | Extension (6 mo) | Radial deviation (3 mo) | Radial deviation (6 mo) | Ulnar deviation (3 mo) | Ulnar deviation (6 mo) | ||
|---|---|---|---|---|---|---|---|---|---|
| Case (n = 7) | Mean | 55 | 73.29 | 54.71 | 64.14 | 10.43 | 19.71 | 22.14 | 30 |
| Max | 60 | 78 | 60 | 70 | 15 | 20 | 25 | 30 | |
| Min | 50 | 70 | 50 | 60 | 8 | 18 | 20 | 30 | |
| Control (n = 6) | Mean | 54.67 | 69.17 | 53.33 | 65 | 9.67 | 19.17 | 20.83 | 26 |
| Max | 60 | 75 | 60 | 70 | 12 | 20 | 28 | 30 | |
| Min | 50 | 65 | 50 | 60 | 8 | 17 | 18 | 25 | |
| p-Value | 0.82 | 0.067 | 0.49 | 0.24 | 0.64 | 0.38 | 0.20 | 0.004 | |
Discussion
The present study had three principal objectives: first, to investigate the effect of PRP on scaphoid fracture healing; second, to identify the potential increase of range of motion after PRP treatment; and third, to investigate if PRP intervention can reduce pain and improve function.
In our study, pain and function were assessed using the PRWE. MacDermid et al demonstrated that the PRWE provides a brief, reliable, and valid measure developed for assessing pain and function in individuals with scaphoid fracture.13
Our study was the first clinical trial assessing the effect of PRP on healing and functional results of scaphoid fractures. PRP, a platelet concentrate made of autologous blood, has been recently used for multiple clinical investigations. The advantage of using PRP is the ability to deliver an increased amount of growth factors in a small volume biological carrier. PRP is autologous and nontoxic, it is inherently safe, and any concerns of disease transmission or immunological reactions are eliminated.6 14 15 16 17
The increasing application of PRP in recent orthopedic surgeries presents significant opportunities as well as questions about the appropriate clinical use for this promising treatment. PRP has been used in a variety of orthopedic problems especially bone healing with variable degrees of successes and failures.
Despite its promising potential, it must be acknowledged that the use of PRP in bone healing is still weakly supported. However, the studies on the effect of PRP on bone healing were not all positive, mixed results were reported and therefore no definitive conclusion could be drawn. Aghaloo et al did not observe any positive additive effects of PRP and autologous bone grafting for bone healing in a prospective rabbit animal model.18 19
However, in this study, scaphoid union was formed earlier in the case group, but it was not statistically significant. The best possible explanation is that PRP is effective in promoting bone healing only if used with autologous bone graft. Kanthan et al demonstrated that use of PRP alone (without bone grafting) does not significantly increase the bone healing rate and provides limited advantage over placebo. Also, Say et al injected PRP in 20 patients with lower extremity fracture and stated that adequate healing was not determined in the treatment of nonunion with PRP injection. Similarly, Sarkar et al used an animal model to evaluate bone healing in the tibial diaphysis of 16 sheep injected either with autogenous PRP or placebo as control. Their study showed no significant difference between the PRP treated and placebo groups and no effect of PRP upon bone formation was observed. In conclusion, they also stated that bone healing might require more potent stimuli and autograft may be necessary.20 21 22
This study suggests that PRP may play a role in improving functional outcome in patients with scaphoid fracture. Total functional score including specific and usual activity significantly differed between the two groups. It means that patients who received PRP may have less difficulty in their functions. Also, PRP may have a significant effect in increasing ulnar deviation of the wrist.
Total pain score had no difference between both the groups, but in detail, pain at rest in the case group significantly differed from the control group.
The major limitation of this study was the small sample size. Another weak point of our study is that we did not perform CT scan earlier than 2 months. Therefore, we could not find any sign of healing in the case group before this time. On the contrary, the strength of this study was that no similar studies have been performed.
We found that intra-articular PRP injection was a valid additional treatment in scaphoid fracture. PRP may have significant effect on improving wrist function in these patients. However, further additional research with larger sample size is required.
It is believed that this study will provide a new insight into the effect of PRP on scaphoid fracture leading to provision of better treatment of these patients.
Acknowledgments
The present article was extracted from the thesis written by Kayedi Toomaj, MD, and was financially supported by Shiraz University of Medical Sciences. This work has been accomplished in collaboration with Bone and Joint Research Center.
Footnotes
Authors' Contribution Namazi Hamid drafted the article and assisted with data analysis; Kayedi Toomaj participated in study design and data collection. All authors read and approved the final article. Conflict of Interest None.
References
- 1.Hackney L A, Dodds S D. Assessment of scaphoid fracture healing. Curr Rev Musculoskelet Med. 2011;4(1):16–22. doi: 10.1007/s12178-011-9072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Jabri T, Mannan A, Giannoudis P. The use of the free vascularised bone graft for nonunion of the scaphoid: a systematic review. J Orthop Surg. 2014;9:21. doi: 10.1186/1749-799X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McQueen M M, Gelbke M K, Wakefield A, Will E M, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90(1):66–71. doi: 10.1302/0301-620X.90B1.19767. [DOI] [PubMed] [Google Scholar]
- 4.Bond C D, Shin A Y, McBride M T, Dao K D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83-A(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Gibbs N, Diamond R, Sekyere E O, Thomas W D. Management of knee osteoarthritis by combined stromal vascular fraction cell therapy, platelet-rich plasma, and musculoskeletal exercises: a case series. J Pain Res. 2015;8:799–806. doi: 10.2147/JPR.S92090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Namazi H, Mehbudi A. Investigating the effect of intra-articular PRP injection on pain and function improvement in patients with distal radius fracture. Orthop Traumatol Surg Res. 2016;102(1):47–52. doi: 10.1016/j.otsr.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Murray D J, Javed S, Jain N, Kemp S, Watts A C. Platelet-rich-plasma injections in treating lateral epicondylosis: a review of the recent evidence. J Hand Microsurg. 2015;7(2):320–325. doi: 10.1007/s12593-015-0193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herbert T J, Fisher W E. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66(1):114–123. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 9.Sundman E A, Cole B J, Fortier L A. Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011;39(10):2135–2140. doi: 10.1177/0363546511417792. [DOI] [PubMed] [Google Scholar]
- 10.Pifer M A, Maerz T, Baker K C, Anderson K. Matrix metalloproteinase content and activity in low-platelet, low-leukocyte and high-platelet, high-leukocyte platelet rich plasma (PRP) and the biologic response to PRP by human ligament fibroblasts. Am J Sports Med. 2014;42(5):1211–1218. doi: 10.1177/0363546514524710. [DOI] [PubMed] [Google Scholar]
- 11.Magalon J, Bausset O, Serratrice N. et al. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthroscopy. 2014;30(5):629–638. doi: 10.1016/j.arthro.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Smith M V, Calfee R P, Baumgarten K M, Brophy R H, Wright R W. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277–285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacDermid J C, Turgeon T, Richards R S, Beadle M, Roth J H. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Malhotra R, Kumar V, Garg B. et al. Role of autologous platelet-rich plasma in treatment of long-bone nonunions: a prospective study. Musculoskelet Surg. 2015;99(3):243–248. doi: 10.1007/s12306-015-0378-8. [DOI] [PubMed] [Google Scholar]
- 15.Bissell L, Tibrewal S, Sahni V, Khan W S. Growth factors and platelet rich plasma in anterior cruciate ligament reconstruction. Curr Stem Cell Res Ther. 2014;10(1):19–25. doi: 10.2174/1574888x09666140710102002. [DOI] [PubMed] [Google Scholar]
- 16.Willits K, Kaniki N, Bryant D. The use of platelet-rich plasma in orthopedic injuries. Sports Med Arthrosc Rev. 2013;21(4):225–230. doi: 10.1097/JSA.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 17.Browning S R, Weiser A M, Woolf N. et al. Platelet-rich plasma increases matrix metalloproteinases in cultures of human synovial fibroblasts. J Bone Joint Surg Am. 2012;94(23):e1721–e1727. doi: 10.2106/JBJS.K.01501. [DOI] [PubMed] [Google Scholar]
- 18.Zhang N, Wu Y P, Qian S J, Teng C, Chen S, Li H. Research progress in the mechanism of effect of PRP in bone deficiency healing. Sci World J. 2013;2013:134582. doi: 10.1155/2013/134582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aghaloo T L, Moy P K, Freymiller E G. Evaluation of platelet-rich plasma in combination with freeze-dried bone in the rabbit cranium. A pilot study. Clin Oral Implants Res. 2005;16(2):250–257. doi: 10.1111/j.1600-0501.2004.01075.x. [DOI] [PubMed] [Google Scholar]
- 20.Kanthan S R, Kavitha G, Addi S, Choon D S, Kamarul T. Platelet-rich plasma (PRP) enhances bone healing in non-united critical-sized defects: a preliminary study involving rabbit models. Injury. 2011;42(8):782–789. doi: 10.1016/j.injury.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Say F, Türkeli E, Bülbül M. Is platelet-rich plasma injection an effective choice in cases of non-union? Acta Chir Orthop Traumatol Cech. 2014;81(5):340–345. [PubMed] [Google Scholar]
- 22.Sarkar M R, Augat P, Shefelbine S J. et al. Bone formation in a long bone defect model using a platelet-rich plasma-loaded collagen scaffold. Biomaterials. 2006;27(9):1817–1823. doi: 10.1016/j.biomaterials.2005.10.039. [DOI] [PubMed] [Google Scholar]


