Abstract
Objective This study aims to evaluate the use of minilocked plates in the treatment of the metacarpal fractures.
Method A total of 30 patients of metacarpal fractures were treated by minilocked plates.
Results Union was achieved in all patients. There were 27 (90%) patients having satisfactory results (excellent and good results) and 3 patients (10%) had poor results.
Conclusion The use of minilocked plate is recommended for fixation of periarticular, comminuted, and osteoporotic metacarpal fractures that offer rigid fixation early mobilization, decreases the incidence of joints stiffness, and tendon adherence which maximized the hand function.
Keywords: metacarpal fracture, locked plates, miniplate
Introduction
Hand fractures represent 10% of all fractures and metacarpal fractures represent about one-third of hand fractures.1 Most metacarpal fractures occur in active working population; adolescents and young adults, they are documented to have a large economic impact in terms of the cost of treatment and disability.2 Metacarpal shaft fractures can be described as transverse, short oblique, spiral, and comminuted. The correction of shortening, dorsal angulation, and rotation are the main three objectives for treatment of displaced metacarpal shaft fractures.3 The most important objective is to correct rotation as rotational deformity is poorly tolerated.3 An average of 7 degrees of extensor lag at the metacarpophalangeal joint produced for every 2 mm of metacarpal shortening. The capacity of the metacarpophalangeal joint for active hyperextension may compensate for the extensor lag produced by metacarpal shortening in the clinical setting.4
At 2 mm of shortening, there is an approximately 8% loss of power generation, at 10 mm of metacarpal shortening the interosseous muscles are capable of only approximately 55% of its optimum power compared with the resting position.5 Union with rotational malalignment results in overlap or scissoring of the fingers during flexion. Rotational malalignment of less than 10 degrees is usually well-tolerated but deformity greater than this may impair hand function.4
The treatment is guided by the location of the fracture, the stability of the fracture, the resultant deformity, and number of metacarpal fractures.6 Operative treatment includes; closed reduction and percutaneous fixation with Kirschner (K)-wires, open reduction and fixation by intramedullary rods, open reduction and internal fixation using plate and screws, and fixation by using mini external fixator.6 7 8 9 Open reduction and internal fixation is indicated when the unstable fractures cannot be reduced by closed manipulation, multiple fractures, concomitant soft tissue injuries, and the subcapital spiral oblique fractures, which if allowed to heal in the shortened position may result in impingement at the metacarpophalangeal joint.10 A variety of techniques may be used: K-wire, intramedullary fixation, cerclage wiring, interosseous wiring, tension-band wiring, interfragmentary screw fixation, plate fixation, and locking compression plate.8 9 11 12 13 14 15 16
The aim of this study was to evaluate the results of locked palates in the treatment of metacarpal fractures.
Method
A total of 30 patients with closed unstable metacarpal fractures—thumb metacarpal was excluded—were treated by open reduction and internal fixation using minilocked plate 2.4 mm Synthese company (Salmiya, Hawalli Governorate, State of Kuwait), and screws in the period from July 2011 to March 2013. There were 28 males and 2 females; their ages ranged from 16 to 65 years with a mean of 37 years. Overall, 15 (50%) patients were manual workers, 6 patients (20%) did fine jobs, 2 (6.67%) were housewives, 5 (16.67%) were drivers, and 2 (6.67%) were students. The second metacarpal bone (MCB) was affected in 6 (20%) patients, the third MCB was injured in 5 (16.6%) patients, fourth MCB was fractured in 9 (30%) patients, and fifth MCB was fractured in 10 (33.3%) patients.
The period of follow-up ranged between 4 and 16 months (mean ∼13.4 months). All patients were operated within the first 3 weeks after trauma. In 17 cases (57%) surgery was performed under general anesthesia while the rest of cases (43%) were performed under regional anesthesia. A direct dorsal straight incision was done, then dissection of the subcutaneous tissue (transposition of the extensor tendons ulnarly or radially and occasionally sectioning the junction tendenium retraction of the interosseous muscles). The periosteal sleeve was also opened at the fracture site and the bone exposed subperiosteally to visualize the fracture. The fracture was then reduced by longitudinal traction on the digit, and the reduction was held in compression by a reduction clamp. The plates were placed and fixed by screws, and then the wound was sutured.
Postoperative Care and Assessment
Movements of the hand were started immediately. Stitches were removed by 2 weeks. Follow-up protocol included clinical and radiological evaluation including posteroanterior, lateral, and oblique views at first and second weeks, first, second, third, and fourth months. The clinical assessment of the results was based on the system adopted by Belsky et al.17 The results were considered excellent if there was no pain, full union, no angular or rotatory deformity, and total active movement (TAM) greater than 250 degrees (TAM refers to the additive sum of flexion at metacarpophalangeal, interphalangeal joints minus the extension deficit at the same joints). The normal range of TAM is 250 to 280 degrees.
The results were considered good if there was angular and rotatory deformity less than 10 and TAM greater than 180 degrees, and poor if the angular or rotatory deformity was more than 10 and TAM less than 180 degrees.17
Results
According to the system adopted by Belsky et al17, there were 22 (73.3%) patients having excellent results, 5 patients (16.67%) had good results, and 3 patients (10%) had poor results. Accordingly, satisfactory results (excellent and good) were found in 27 patients (90%) and unsatisfactory results (poor) were found in 3 patients (10%) (Table 1).
Table 1. Patients' information and results.
| Number | Age | Sex | Affected MCB | Mechanism of injury | Shape of fracture | Union (wk) | TAM (degree) | Belsky score | Dominant hand or nondominant |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | M | 4th | Twist | Spiral | 10 | 260 | Excellent | Dominant |
| 2 | 26 | M | 2nd | Direct | Transverse | 12 | 255 | Excellent | Dominant |
| 3 | 30 | M | 3rd | Direct | Oblique | 8 | 255 | Excellent | Nondominant |
| 4 | 63 | M | 2nd, 3rd | Direct | Comminuted | 16 | 170 | Poor | Nondominant |
| 5 | 65 | M | 5th | Direct | Transverse | 10 | 200 | Good | Nondominant |
| 6 | 32 | M | 2nd | Direct | Oblique | 8 | 255 | Excellent | Dominant |
| 7 | 22 | M | 3rd | Direct | Oblique | 12 | 255 | Excellent | Nondominant |
| 8 | 24 | M | 4th | Direct | Oblique | 16 | 200 | Good | Nondominant |
| 9 | 32 | M | 2nd | Direct | Transverse | 8 | 210 | Good | Nondominant |
| 10 | 34 | M | 5th | Direct | Comminuted | 8 | 170 | Poor | Nondominant |
| 11 | 38 | M | 4th | Direct | Oblique | 12 | 260 | Excellent | Nondominant |
| 12 | 44 | M | 5th | Direct | Oblique | 8 | 210 | Good | Dominant |
| 13 | 50 | M | 4th | Twist | Spiral | 10 | 260 | Excellent | Dominant |
| 14 | 33 | M | 4th | Direct | Oblique | 10 | 255 | Excellent | Dominant |
| 15 | 32 | M | 5th | Direct | Transverse | 10 | 260 | Excellent | Nondominant |
| 16 | 34 | M | 5th | Twist | Spiral | 8 | 250 | Excellent | Nondominant |
| 17 | 42 | M | 3rd | Direct | Transverse | 10 | 260 | Excellent | Dominant |
| 18 | 48 | M | 3rd | Twist | Oblique | 8 | 260 | Excellent | Nondominant |
| 19 | 44 | M | 5th | Direct | Transverse | 10 | 250 | Excellent | Dominant |
| 20 | 28 | M | 5th | Direct | Oblique | 8 | 175 | Excellent | Dominant |
| 21 | 54 | M | 4th | Direct | Transverse | 10 | 255 | Excellent | Dominant |
| 22 | 28 | M | 4th | Direct | Transverse | 12 | 260 | Excellent | Nondominant |
| 23 | 38 | M | 4th | Direct | Transverse | 12 | 255 | Excellent | Dominant |
| 24 | 50 | M | 2nd | Direct | Comminuted | 10 | 255 | Excellent | Nondominant |
| 25 | 52 | M | 3rd | Direct | Comminuted | 12 | 255 | Excellent | Dominant |
| 26 | 42 | M | 5th | Direct | Transverse | 10 | 200 | Good | Nondominant |
| 27 | 19 | M | 4th | Twist | Spiral | 10 | 270 | Excellent | Dominant |
| 28 | 18 | M | 2nd | Twist | Spiral | 10 | 270 | Excellent | Dominant |
| 29 | 28 | F | 5th | Twist | Spiral | 8 | 265 | Excellent | Nondominant |
| 30 | 45 | F | 5th | Twist | Spiral | 8 | 265 | Excellent | Dominant |
Abbreviations: F, female; M, male; MCB, metacarpal bone; TAM, total active movement.
Union was seen in all 30 patients, that is (100%). Two (6.67%) patients showed delayed union more than 16 weeks as they had comminuted fracture at the second and fifth MCB (Fig. 1).
Fig. 1.
(A) Fracture base of fifth metacarpal (B) postoperative X- ray (C and D) postoperative range of motion.
Two patients (6.67%) who had angular deformity, had poor results. The first had a 20 degrees dorsal angular deformity and the other one had 20 degrees radial angular deformity. The p value of < 0.001 was considered significant, which means that angular deformity significantly decreases the functional outcome .There was no case presented with rotational deformity (Fig. 2).
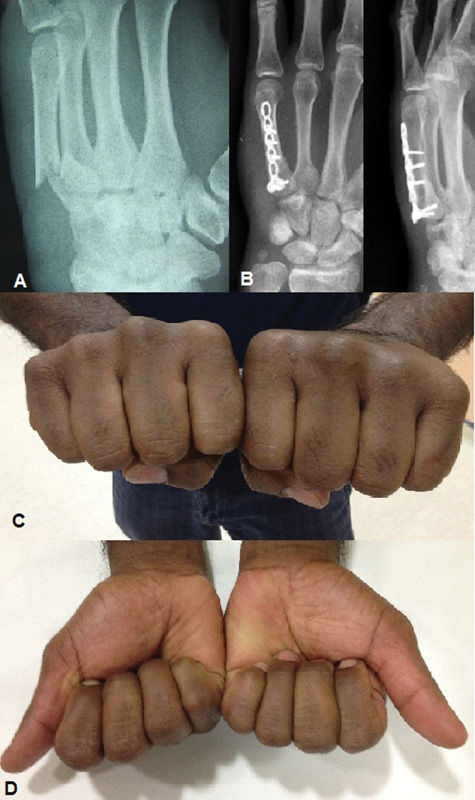
Fig. 2.

(A) Second and third metacarpals (B) postoperative X-ray (C and D) postoperative range of motion.
Two of three patients with unsatisfactory results were older than 60 years. Out of the 14 patients (46.67% of all patients) with dominant hand involvement, there were 10 patients (71.43%) with excellent results, 3 patients (21.4%) with good results, and 1 patient (7%) with poor results. The 16 patients with nondominant hands (53.33%) involvement, there were 12 patients (75%) with excellent results, 2 patients (12.5%) with good results, and 2 patients (12.5%) with poor results.
Two (13.3%) patients with unsatisfactory results were manual workers and the third one (20%) was a driver. The manual workers and drivers were associated with the worse results in our study. As regards the injured MCB, the second and the fifth metacarpals were associated with the worse results in the study and these finding was statistically significant p > 0.05. Two patients (33.3%) with unsatisfactory results had comminuted fracture, and one (12.5%) had an oblique fracture. The comminuted and oblique fractures were associated with the worse results in this study and these differences are statistically insignificant (p < 0.05).
In our study, there were two patients who had superficial wound infection that treated with dressing and antibiotics. Delayed union was reported in two patients and their results were unsatisfactory (TAM = 150 degrees). There were two patients with malunited fracture; one (50%) of them had unsatisfactory results (TAM = 150 degrees). Extensor tendon adherence occurred in two patients who resulted in extension lag which was treated by physiotherapy.
Discussion
The technology of minilocked plate and screws is a rigid method of open reduction and internal fixation for displaced, unstable metacarpal fractures. The locked plates are most appropriate and offer improved fixation stability in comminuted fractures, periarticular fractures, osteoporotic fractures, fractures with bone loss, and pathological fractures. Clinical experiences with locking plate technology in the hand trauma remain relatively limited compared with its application in the long bones.16
Since Burton and Eudell first used plate fixation in treating metacarpal fractures,18 the concept of stable methods of internal fixation that allows early motion has been increasingly stressed.15 18 Several biomechanical studies have assessed various methods of internal fixation of metacarpals, and these suggest that a plate placed along the dorsal midline, with at least two screws on either side of the fracture, afford the greatest strength. The average load to failure was significantly greater in the plate approximately 10 times more than crossed K-wire or intramedullary nails.19 20 This fixation technique has therefore become the most common method of open reduction internal fixation for displaced, unstable metacarpal fractures.19 The stable bony construct achievable by plates and screws fixation is the key to good functional results. Active mobilization can be started immediately after surgery; edema, fibrosis, and scar formation can be reduced; and tendon gliding can be preserved.16
Freeland and Orbay reported that the use of unicortical screw fixation of miniplates affords stability comparable to that of bicortical screw fixation in treating transverse extra-articular metacarpal fractures while unicortical screws create less bone damage.21 Using a porcine metacarpal model, Ochman et al compared the stiffness and load to failure of 2.3 mm straight titanium plates fixed with four nonlocking screws or four locking screws (two on either side of the fracture). Although the locking construct using unicortical screws was found to be stronger than the nonlocking construct using unicortical screws.22 The study of Barr et al reported biomechanical equivalence between simulated comminuted metacarpal fractures fixed using a dorsal plate with either three nonlocking screws (six cortices of fixation) or two locking screws (four cortices of fixation) on either side of the fracture so the advantage use of short plates was less soft tissue disruption—there is an opportunity for less soft tissue disruption.23
Locking plate technology offers improved fixation stability in osteoporotic bone and comminuted fractures. The additional stability per screw compared with that of nonlocked plate enhances its application, especially in osteopenic and comminuted fractures, particularly with the prevalence of fragility fractures in aging population and the increased high-energy fractures in young patients. The initial results in series that included a variety of fractures fixed by locking plates are encouraging.24
A comparison study assessed the results of usage of K-wires and miniplate in the management of metacarpal fractures. The results were good: no deformity, TAM > 210 degrees, strong grip in 50% of the K-wire fixation group and 79% in the miniplates and screws group. This difference may be due to solid stabilization and earlier mobilization in miniplates group.25
A total of 38 metacarpal fractures patients treated by intramedullary nails (IMN) fixation and 14 patients received plate–screws (PS) fixation. The mean follow-up time was 18 weeks in the IMN group and 19 weeks in the PS group. The mean and median total active motion was 237 and 250 degrees for the IMN group, 228 and 248 degrees for the PS group, with no statistically significant difference between the groups. The mean Disabilities of the Arm, Shoulder, and Hand score was 9.47 in the IMN group and 8.07 in the PS group. The association between hardware type and fracture location (middle or distal third of metacarpal) was not statistically significant. Also, the time to radiographic healing did not reach statistical significance between the groups. Operative time was significantly shorter with the use of the metacarpal nail. Five patients in the IMN group displayed loss of reduction; no failure was observed in the PS group.26
Puckett et al managed 50 metacarpal shaft fractures by open reduction and internal fixation using plate and screws, the mean TAM of the involved finger was regained to normal or near normal in all patients, only one patient developed nonunion possibly related to extensive periosteal stripping and five patients required late plate removal.27 Ford et al treated 26 fractured metacarpals by internal fixation using AO minifragment screws and plates. A total of 14 patients regained full movement. Four had TAM of 220 degrees or more in the involved ray and six patients had TAM between 180 and 220 degrees.28 The lower profile plates reduce the soft tissue irritation and complications, and smaller the plates less is the exposure and periosteal stripping.21 28
The good results which achieved in our study (90%) may be due to the stable bony construct and early active mobilization, which reduce the edema, fibrosis, and scar formation and can improve tendon gliding. Barton and Crawford reported satisfactory results in younger patients.29 30
Our results were poor in manual workers. The office workers seldom need to stay away from work at all and only patients with very heavy or rough jobs or with multiple hand fractures need to be off work longer than 3 to 4 weeks.29
As regard the mechanism of injury, the poor results occurred in direct impaction and these finding are similar to that reported by Barton who stated that comminuted fractures are commonly due to a crushing injury.29 Comminuted fractures had the worst results in our study while the spiral and oblique fractures had the best results. These results correlate with that of Barton who concluded that comminuted fractures gave a high proportion of poor results due to multiple fracture lines and crushing of the accompanying soft tissue.29
In the prospective study done by Stern et al complications were identified in 29% of acute metacarpal fractures. Stiffness and prominent hardware were the most common complication; early motion postoperatively can help prevent the former complication.31
Our results regarding hand dominance correlate with that of Absoud and Harrop who found the nondominant hands were injured slightly more frequently than the dominant one, whatever the circumstances of injury, dominant is a poor guide to the disability which may follow a given injury.32
Grundberg concluded that the treatment of unstable hand fractures is less satisfactory.33 Gonzalez et al reported that flexible intramedullary nails were contraindicated in comminuted metacarpal fractures.8 However Page and Stern found that fracture site comminution has no effect on neither the outcome nor the complication rate.34
We found that early fixation of metacarpal fractures had the best results and this correlated with Brown who stressed that time is an important factor in the result of treatment of hand fractures. The sooner the fixation is done after injury; the good result will be.35
The unsatisfactory results occurred in second and fifth metacarpal fractures. These results may be due to the fact that fifth carpometacarpal joint is more mobile than the other carpometacarpal joints, this creates a deforming force at the fracture site and this variation in carpometacarpal motion dictates the amount of angulation that can be accepted in the metacarpal fracture.8 Page and Stern reported no difference in the TAM in relation to the site of the metacarpal fracture.34
Our complications were delayed union (6.67%), malunion (6.67%). Around 50% of patients with delayed union developed in addition stiffness in the MCP joint and the end result was unsatisfactory (TAM = 150 degrees). Similar studies reported the relatively high incidence of delayed union and nonunion with miniplate fixation. While Page et al reported 4% incidence of delayed union and 2% nonunion rate while Pukett et al reported 4% incidence of delayed union and an 8% nonunion rate which may be due to extensive periosteal stripping.27 34
Angular malunion developed in two cases (6.7%) that occurred in second and fifth MCBs while Page et al reported a (4%) incidence of malunion with miniplates.34
Ruchelsman et al reported selected indications for the use of locked fixed plates in the hand fractures including periarticular metacarpal and phalangeal fractures, comminuted, multifragmentary diaphyseal fractures with bone loss—combined injuries of the hand—osteopenic, pathological fractures, nonunions, and corrective osteotomy fixation, and small joint arthrodesis.36
We recommend the use of minilocked plate for fixation of periarticular, comminuted, and osteoporotic metacarpal fractures. It offers stable rigid fixation of metacarpal fractures which allow early mobilization, decreases the incidence of joints stiffness and tendon adherence which maximized the hand function but a special attention should be considered for the specific locked plates that shared common features in their protocols for insertion, but unique differences in their design as individual locking mechanisms, uniaxial versus polyaxial locking capability, metallurgy, and plate profiles.36
Note
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.McNemar T B, Howell J W, Chang E. Management of metacarpal fractures. J Hand Ther. 2003;16(2):143–151. doi: 10.1016/s0894-1130(03)80009-1. [DOI] [PubMed] [Google Scholar]
- 2.de Jonge J J, Kingma J, van der Lei B, Klasen H J. Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury. 1994;25(6):365–369. doi: 10.1016/0020-1383(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 3.Day C S, Stern P J. Philadelphia, PA: Elsevier Churchill Living stone; 2010. Fractures of metacarpals and phalanges; pp. 239–290. [Google Scholar]
- 4.Strauch R J, Rosenwasser M P, Lunt J G. Metacarpal shaft fractures: the effect of shortening on the extensor tendon mechanism. J Hand Surg Am. 1998;23(3):519–523. doi: 10.1016/S0363-5023(05)80471-X. [DOI] [PubMed] [Google Scholar]
- 5.Meunier M J, Hentzen E, Ryan M, Shin A Y, Lieber R L. Predicted effects of metacarpal shortening on interosseous muscle function. J Hand Surg Am. 2004;29(4):689–693. doi: 10.1016/j.jhsa.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Kozin S H, Thoder J J, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000;8(2):111–121. doi: 10.5435/00124635-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Jabaley M E, Freeland A E. Rigid internal fixation in the hand: 104 cases. Plast Reconstr Surg. 1986;77(2):288–298. doi: 10.1097/00006534-198602000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez M H, Igram C M, Hall R F Jr. Flexible intramedullary nailing for metacarpal fractures. J Hand Surg Am. 1995;20(3):382–387. doi: 10.1016/S0363-5023(05)80091-7. [DOI] [PubMed] [Google Scholar]
- 9.Lister G. Intraosseous wiring of the digital skeleton. J Hand Surg Am. 1978;3(5):427–435. doi: 10.1016/s0363-5023(78)80135-x. [DOI] [PubMed] [Google Scholar]
- 10.Salom M, Aroca J E, Chover V, Alonso R, Vilar R. Distraction-lengthening of digital rays using a small external fixator. J Hand Surg [Br] 1998;23(6):781–784. doi: 10.1016/s0266-7681(98)80096-x. [DOI] [PubMed] [Google Scholar]
- 11.Jupiter J B, Koniuch M P, Smith R J. The management of delayed union and nonunion of the metacarpals and phalanges. J Hand Surg Am. 1985;10(4):457–466. doi: 10.1016/s0363-5023(85)80066-6. [DOI] [PubMed] [Google Scholar]
- 12.Weiss A P, Hastings H II. Distal unicondylar fractures of the proximal phalanx. J Hand Surg Am. 1993;18(4):594–599. doi: 10.1016/0363-5023(93)90297-G. [DOI] [PubMed] [Google Scholar]
- 13.Hall R F Jr. Treatment of metacarpal and phalangeal fractures in noncompliant patients. Clin Orthop Relat Res. 1987;(214):31–36. [PubMed] [Google Scholar]
- 14.Freeland A E, Geissler W B, Weiss A P. Operative treatment of common displaced and unstable fractures of the hand. J Bone Joint Surg Am. 2001;83:928–945. [Google Scholar]
- 15.Dabezies E J, Schutte J P. Fixation of metacarpal and phalangeal fractures with miniature plates and screws. J Hand Surg Am. 1986;11(2):283–288. doi: 10.1016/s0363-5023(86)80072-7. [DOI] [PubMed] [Google Scholar]
- 16.Haidukewych G J. Innovations in locking plate technology. J Am Acad Orthop Surg. 2004;12(4):205–212. doi: 10.5435/00124635-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Belsky M R, Eaton R G, Lane L B. Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am. 1984;9(5):725–729. doi: 10.1016/s0363-5023(84)80023-4. [DOI] [PubMed] [Google Scholar]
- 18.Kilbourne B C, Paul E G. The use of small bone screws in the treatment of metacarpal, metatarsal, and phalangeal fractures. J Bone Joint Surg Am. 1958;40-A(2):375–383. [PubMed] [Google Scholar]
- 19.Prevel C D, Eppley B L, Jackson J R. et al. Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical study. J Hand Surg Am. 1995;20(1):44–49. doi: 10.1016/s0363-5023(05)80057-7. [DOI] [PubMed] [Google Scholar]
- 20.Curtis B D, Fajolu O, Ruff M E, Litsky A S. Fixation of metacarpal shaft Fractures: Biomechanical comparison of intramedullary nail, crossed K-wires and plate-screw constructs. Orthop Surg. 2015;7(3):256–260. doi: 10.1111/os.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freeland A E, Orbay J L. Extraarticular hand fractures in adults: a review of new developments. Clin Orthop Relat Res. 2006;(445):133–145. doi: 10.1097/01.blo.0000205888.04200.c5. [DOI] [PubMed] [Google Scholar]
- 22.Ochman S, Doht S, Paletta J, Langer M, Raschke M J, Meffert R H. Comparison between locking and non-locking plates for fixation of metacarpal fractures in an animal model. J Hand Surg Am. 2010;35(4):597–603. doi: 10.1016/j.jhsa.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 23.Barr C, Behn A W, Yao J. Plating of metacarpal fractures with locked or nonlocked screws, a biomechanical study: how many cortices are really necessary? Hand (NY) 2013;8(4):454–459. doi: 10.1007/s11552-013-9544-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith W R, Ziran B H, Anglen J O, Stahel P F. Locking plates: tips and tricks. J Bone Joint Surg Am. 2007;89(10):2298–2307. doi: 10.2106/00004623-200710000-00028. [DOI] [PubMed] [Google Scholar]
- 25.Diwaker H N, Stothard J. The role of internal fixation in closed fractures of the proximal phalanges and metacarpals in adults. J Hand Surg [Br] 1986;11(1):103–108. doi: 10.1016/0266-7681(86)90027-6. [DOI] [PubMed] [Google Scholar]
- 26.Ozer K, Gillani S, Williams A, Peterson S L, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724–1731. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Puckett C L Welsh C F Croll G H Concannon M J Application of maxillofacial miniplating and microplating systems to the hand Plast Reconstr Surg 1993924699–707., discussion 708–709 [PubMed] [Google Scholar]
- 28.Ford D J, el-Hadidi S, Lunn P G, Burke F D. Fractures of the metacarpals: treatment by A. O. screw and plate fixation. J Hand Surg [Br] 1987;12(1):34–37. doi: 10.1016/0266-7681_87_90050-7. [DOI] [PubMed] [Google Scholar]
- 29.Barton N J. Fractures of the shafts of the phalanges of the hand. Hand. 1979;11(2):119–133. doi: 10.1016/s0072-968x(79)80024-8. [DOI] [PubMed] [Google Scholar]
- 30.Crawford G P. Screw fixation for certain fractures of the phalanges and metacarpals. J Bone Joint Surg Am. 1976;58(4):487–492. [PubMed] [Google Scholar]
- 31.Stern P J, Wieser M J, Reilly D G. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res. 1987;(214):59–65. [PubMed] [Google Scholar]
- 32.Absoud E M, Harrop S N. Hand injuries at work. J Hand Surg [Br] 1984;9(2):211–215. [PubMed] [Google Scholar]
- 33.Grundberg A B. Intramedullary fixation for fractures of the hand. J Hand Surg Am. 1981;6(6):568–573. doi: 10.1016/s0363-5023(81)80134-7. [DOI] [PubMed] [Google Scholar]
- 34.Page S M, Stern P J. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827–832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 35.Brown P W. The management of phalangeal and metacarpal fractures. Surg Clin North Am. 1973;53(6):1393–1437. doi: 10.1016/s0039-6109(16)40185-4. [DOI] [PubMed] [Google Scholar]
- 36.Ruchelsman D E, Mudgal C S, Jupiter J B. The role of locking technology in the hand. Hand Clin. 2010;26(3):307–319, v. doi: 10.1016/j.hcl.2010.04.001. [DOI] [PubMed] [Google Scholar]


