Abstract
Aims
Recent guidelines for management of cardiac arrest recommend chest compression rates of 100-120 compressions/min. However, animal studies have found cardiac output to increase with rates up to 150 compressions/min. The objective of this study was to test the association between chest compression rates during cardiopulmonary resuscitation for in-hospital cardiac arrest (IHCA) and outcome.
Methods
We conducted a prospective observational study at a single academic medical center. Inclusion criteria: age ≥18, IHCA, cardiopulmonary resuscitation performed. We analyzed chest compression rates measured by defibrillation electrodes, which recorded changes in thoracic impedance. The primary outcome was return of spontaneous circulation (ROSC). We used multivariable logistic regression to determine odds ratios for ROSC by chest compression rate categories (100-120, 121-140, >140 compressions/min), adjusted for chest compression fraction (proportion of time chest compressions provided) and other known predictors of outcome. We set 100-120 compressions/min as the reference category for the multivariable model.
Results
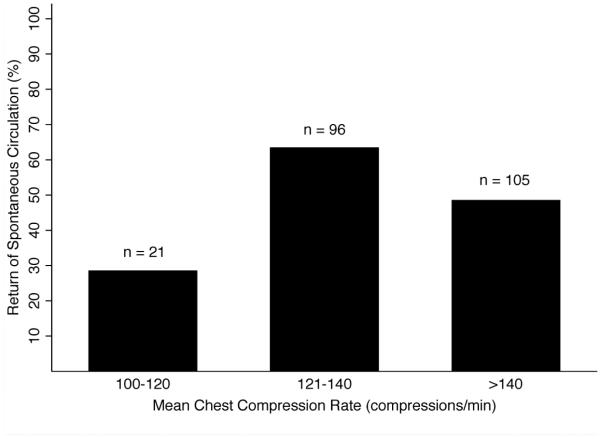
We enrolled 222 consecutive patients and found a mean chest compression rate of 139±15. Overall 53% achieved ROSC; among 100-120, 121-140, and >140 compressions/min, ROSC was 29%, 64%, and 49% respectively. A chest compression rate of 121-140 compressions/min had the greatest likelihood of ROSC, odds ratio 4.48 (95% CI 1.42-14.14).
Conclusions
In this sample of adult IHCA patients, a chest compression rate of 121-140 compressions/min had the highest odds ratio of ROSC. Rates above the currently recommended 100-120 compressions/min may improve the chances of ROSC among IHCA patients.
Keywords: cardiopulmonary resuscitation, cardiac arrest, heart arrest, resuscitation
Introduction
Cardiac arrest is a leading cause of death worldwide, with an estimated survival to hospital discharge rate less than 10% for out-of-hospital cardiac arrest (OHCA)1 and 20% for in-hospital cardiac arrest.2 Since its inception in 1960, improving outcomes with cardiopulmonary resuscitation (CPR) has been the focus of intense investigation, and guidelines continue to evolve. It has previously been demonstrated that high quality chest compressions are essential for successful return of spontaneous circulation (ROSC).3 Components of high quality chest compressions include rate, depth, and chest compression fraction (CCF). In the original article published by Kouwenhoven et al,4 a chest compression rate of 60 compressions/min was recommended. In 2010, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care recommended a chest compression rate of at least 100 compressions/min (no upper limit),5 while the European Resuscitation Council Guidelines recommended a rate of at least 100 compressions/min, but not to exceed 120 compressions/min.6 Most recently the 2015 AHA guidelines and the 2015 International Liaison Committee on Resuscitation (ILCOR) consensus statement recommended a rate of 100-120 compressions/min.3,7
These latest guidelines recommending an upper limit of 120 compressions/min were based on two recent observational studies, one which found ROSC rates peaked at a chest compression rate of 125 compressions/min8 and the second which found an association between an average chest compression rate of 100-120 compressions/min and survival to hospital discharge compared to higher and lower rates.9 Both of these studies examined chest compression rates provided by emergency medical services (EMS) during out-of-hospital cardiac arrest. Compared to in-hospital CPR, it is possible overall quality of CPR may be lower out-of-hospital, due to the need to rapidly transfer the patient10 and the limited number of providers to alternate performing compressions resulting in rescuer fatigue. Currently there is a paucity of data on the association between chest compression rates and clinical outcomes among patients with in-hospital cardiac arrest.
The objectives of this prospective cohort study were to test the associations between chest compression rate and (1) successful ROSC and (2) good neurological outcome at hospital discharge, among patients with in-hospital cardiac arrest.
Methods
Setting
This was a prospective observational study conducted at a single urban academic medical center, Cooper University Hospital in Camden, New Jersey. Cooper University Hospital is the regional Cardiac Resuscitation Center for southern New Jersey, and has in place the infrastructure and clinical capabilities considered by the AHA to be essential elements of a “Level 1” center for cardiac arrest and post-cardiac arrest care.11 Subjects were enrolled in the emergency department (ED), non-trauma intensive care units (ICU), and hospital wards from 2013 to 2015. In order to prospectively identify consecutive cardiac arrest patients, we utilized a 24-hour per day, 7-day per week notification system. The notification system was activated in one of two ways: a) a hospital wide “code blue” activation anytime a cardiac arrest occurred in the hospital; and b) an automated email alert anytime our standardized code documentation narrator was opened in a patient’s electronic medical record. Our institution utilizes an electronic standardized code documentation narrator for real time documentation during resuscitation. In each case, an on-call investigator received the notification and responded to the cardiac arrest event to download data. The Institutional Review Board approved this study with a waiver of written informed consent.
Participants
We included adult in-hospital cardiac arrest patients from August 2013 to March 2015. The inclusion criteria were: 1) age ≥ 18 years, 2) cardiac arrest, defined as a documented absence of pulse and CPR initiated, and 3) cardiac arrest witnessed in-hospital. We excluded patients with cardiac arrest related to trauma.
Data collection
Defibrillator monitors were utilized to measure chest compression rate during CPR. Our institution uniformly uses the Physio-Control LIFEPAK® 20 (Redmond, WA, USA) during patient resuscitation. The presence and rate of chest compressions were measured by changes in thoracic impedance recorded from the defibrillation electrodes.12 Electronic recordings were reviewed for accuracy by trained personnel, and then analyzed with specialized software [Physio-Control CodeStat® (Redmond, WA, USA)] that automatically calculated mean chest compression rate for the full duration of CPR (i.e. until successful ROSC or termination of resuscitation). Chest compression rate was defined as the rate during which chest compressions were actually performed (i.e. independent of chest compression interruptions) during one-minute intervals.3 Interruptions in chest compressions (i.e. time without chest compressions) were defined as a pause greater than or equal to three seconds. Therefore, the rate was the same regardless if chest compressions were given during the entire one-minute interval or only part of the one-minute interval.8,9 The software also calculated the CCF, defined as the proportion of each one-minute interval during which chest compressions were provided.
We collect data pertaining to the index cardiac arrest event, and outcomes consistent with the Utstein style for reporting cardiac arrest research.13,14 We recorded subject demographics, comorbidities, if ROSC was successfully achieved, and neurological status at hospital discharge [defined by the Cerebral Performance Category (CPC)]. We entered all data into Research Electronic Data Capture (REDCap), a secure, web-based application designed to support data capture for research studies15 and exported into Stata/SE 14.1 for Mac, StataCorp LP (College Station, TX, USA).
Outcomes
The primary outcome was successful ROSC for at least 20 minutes. Our secondary outcomes were (1) good neurological function at hospital discharge, defined as a Cerebral Performance Category (CPC) < 3 and (2) preservation of neurological status, defined as no increase in CPC at hospital discharge compared to the CPC at the time of cardiac arrest. The CPC is a validated five-point scale of neurological disability and historically the most commonly used outcome measure in post-cardiac arrest research (1: good cerebral performance, 2: moderate cerebral disability, 3: severe cerebral disability, 4: coma/vegetative state, 5: death).13,16 The CPC at the time of cardiac arrest was obtained through review of the electronic medical record and the CPC at hospital discharge was prospectively determined for each patient at the time of hospital discharge. Patients with a CPC of 1 or 2 had sufficient cerebral function at discharge to live independently. The investigator who determined the pre-arrest CPC and assessed subjects to determine the CPC at hospital discharge was blinded to the chest compression rate.
Data Analysis
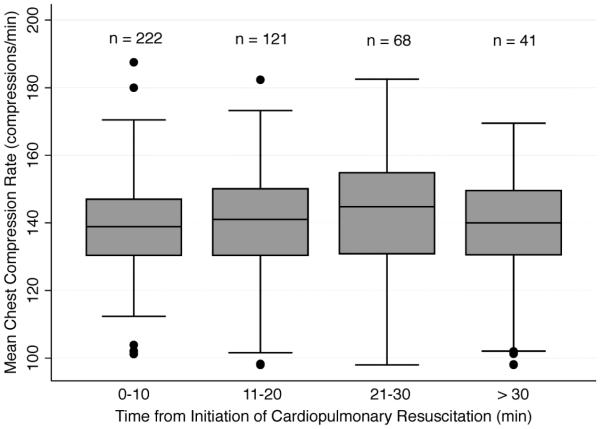
We began the analysis with descriptive statistics. We displayed categorical data as counts and proportions, and continuous data as mean values and standard deviation (SD) or median values and interquartile range (IQR), based on distribution of data. In order to assess if mean chest compression rates changed over the duration of CPR, we used boxplots to graph the distribution of the mean chest compression rates over the following time intervals: 0-10, 11-20, 21-30, and > 30 minutes. We used repeated-measures ANOVA to test for differences in mean chest compression rates at 0-10, 11-20, 21-30, and > 30 minutes. We a priori categorized subjects based on mean chest compression rate over the duration of CPR: 100-120, 121-140, and greater than 140 compressions/min. These categories were based on previous literature, which identified greatest likelihood of ROSC to occur in the 100-120 compressions/min range, among OHCA patients.8,9 We graphed the proportion of successful ROSC for each mean chest compression range.
We calculated odds ratios using multivariable logistic regression analyses to test the association between mean chest compression rate, and successful ROSC and good neurological outcome at hospital discharge. We designated 100-120 compressions/min as the reference range. We a priori selected the following candidate variables for the regression model that were previously demonstrated to be associated with outcome in cardiac arrest patients: age (decile), initial cardiac rhythm [asystole or pulseless electrical activity (PEA) versus ventricular fibrillation/ventricular tachycardia (VF/VT)], and pre-arrest co-morbidities (i.e. Charlson comorbidities index).17-22 We also adjusted for the CCF. For purposes of analysis we categorized CCF into five ranges: 0–20%, 21– 40%, 41–60%, 61–80%, and 81-100%.8 Finally we inserted subject location at the time of cardiac arrest (monitored vs. non-monitored bed) into the model.
We performed several post hoc sensitivity analyses with successful ROSC as the dependent variable. First, we analyzed subject compression rate over time and identified subjects with exposure to a chest compression rate less than 100 compressions/min for at least one minute and further adjusted our original model for exposure to chest compression rate < 100 compressions/min (yes/no). Second, to further test if a chest compression rate of 121-140 compressions/min was independently associated with successful ROSC we performed a separate secondary analysis adjusting for mechanical ventilation prior to cardiac arrest (yes/no), as well as performed a subgroup analysis testing the association between chest compression rate and successful ROSC among only those subjects who were mechanically ventilated prior to cardiac arrest. Finally, among subjects for whom the etiology of cardiac arrest was clear we adjusted our model for etiology of cardiac arrest [i.e. cardiac vs. respiratory vs. other (etiology of cardiac arrest determined not to be cardiac or respiratory)].
In order to further evaluate the association between chest compression rate, and successful ROSC and good neurological outcome at hospital discharge we performed a sensitivity analysis testing narrower ranges for chest compression rates (i.e. 121-130, 131-140, 141-150, > 150 compressions/min) compared to the current recommended rate of 100-120 compressions/min. Multivariable models were adjusted for the same variables in the original model described above.
Sample size calculation
To ensure adequate power to test eight covariates (including the three chest compression categories described above) in a multivariable model, we estimated the necessary sample size, based on the following assumptions: a) a predicted successful ROSC rate of 40% based on previous literature (published rates of ROSC for in-hospital cardiac arrest range from 55-67%,2 we conservatively estimated 40% to ensure we accrued adequate subjects with successful ROSC), and b) an estimated event (successful ROSC) per covariate ratio of 10:1 necessary for multivariable modeling.23,24 To accrue the necessary 80 subjects with successful ROSC we estimated that a minimum of 200 total cases would be necessary.
Results
Four hundred and eighty-three consecutive cardiac arrest subjects from the ED, ICU, and hospital wards were screened for potential enrollment and 222 subjects who met all inclusion and no exclusion criteria had thoracic impedance recorded. Of these 21 (10%) had a mean compression rate 100-120 compressions/min, 96 (43%) had a mean compression rate 121-140 compressions/min, and 105 (47%) had a mean compression rate greater than 140 compressions/min. The overall mean chest compression rate for the entire cohort was 139±15 and the median was 140 (IQR 132 – 149). The mean CCF was 90±7% and the median was 91% (IQR 87% – 94%). There was little correlation between CCF and mean chest compression rate (correlation coefficient = −0.08, p = 0.23).
Table 1 displays baseline data for all subjects in the cohort, as well as patients in each mean chest compression rate category. The median time from collapse to initiation of CPR was less than one minute for subjects in each of the three chest compression categories. This is likely due to the fact that the majority of the subjects had a witnessed cardiac arrest (91%) Figure 1 displays the distribution of the mean chest compression rates over increasing time intervals. We did not find a statistically significant difference in mean chest compression rates between 0-10, 11-20, 21-30, and > 30 minutes (p = 0.25 using repeated-measures ANOVA). We identified only 18 subjects with exposure to a chest compression rate < 100 compressions/min. Fifty-three percent of all subjects were found to have the primary outcome of successful ROSC. The mean (SD) time to ROSC among those who achieved successful ROSC was 15(18), 16(13), 14(19), 15(17) minutes for the entire cohort, and chest compression rates 100-120, 121-140, and > 140 respectively. Figure 2 displays the proportion of subjects with successful ROSC in relation to mean chest compression rate category. Among the subjects who achieved successful ROSC, 41%, 67%, 38%, and 41% had CPR performed again after maintaining ROSC for at least 20 minutes in the entire cohort, and chest compression rates 100-120, 121-140, and > 140 respectively. Ten percent of all patients were found to have the secondary outcome of good neurological function at hospital discharge [CPC 1, 21/222 (9%); CPC 2, 2/222 (1%); CPC 3, 8/222 (4%); CPC 4, 2/222 (1%); CPC 5, 189/222 (85%)]. We found 5%, 11%, and 10% of subjects with a chest compression rate of 100-120, 121-140, and > 140 compressions/min had good neurological function at hospital discharge, respectively. We also found 6%, 14%, and 12% of subjects with a chest compression rate of 100-120, 121-140, and > 140 compressions/min had preservation of neurological status respectively.
Table 1.
Characteristics for all subjects at the time of cardiac arrest.
| Chest Compression Rate Categories |
||||
|---|---|---|---|---|
| All Subjects n = 222 |
100-120 n = 21 |
121-140 n = 96 |
>140 n = 105 |
|
| Age [years (SD)] | 66 (14) | 63 (18) | 64 (15) | 68 (13) |
| Female gender [n (%)] | 86 (39) | 6 (29) | 37 (39) | 43 (41) |
| Pre-existing comorbidities [n (%)] | ||||
| Diabetes | 85 (38) | 5 (24) | 33 (34) | 47 (45) |
| Known coronary artery disease | 82 (37) | 4 (19) | 35 (36) | 43 (41) |
| Hypertension | 140 (63) | 10 (48) | 58 (60) | 72 (69) |
| Malignancy | 58 (26) | 5 (24) | 24 (25) | 29 (28) |
| Renal insufficiency | 60 (27) | 3 (14) | 23 (24) | 34 (32) |
| Pulmonary disease | 48 (22) | 4 (19) | 21 (22) | 23 (22) |
| Cerebral vascular disease | 26 (12) | 2 (10) | 11 (11) | 13 (12) |
| Congestive heart failure | 48 (22) | 4 (19) | 19 (20) | 25 (24) |
| Charlson comorbidity score19
[median (IQR)] |
2 (1 - 4) | 1 (0 - 4) | 2 (1 - 4) | 3 (1 - 4) |
| Pre-arrest Cerebral Performance Category [median (IQR)] |
1 (1 – 3) | 1 (1 – 3) | 1 (1 – 3) | 2 (1 – 3) |
| Initial arrest rhythm [n (%)] | ||||
| PEA/asystole | 165 (74) | 15 (72) | 76 (79) | 74 (70) |
| VF/VT | 46 (21) | 3 (14) | 15 (16) | 28 (27) |
| Unknown | 11 (5) | 3 (14) | 5 (5) | 3 (3) |
| Etiology of cardiac arrest [n(%)] | ||||
| Cardiac | 29 (13) | 4 (19) | 12 (13) | 13 (12) |
| Respiratory | 68 (30) | 6 (28) | 27 (28) | 35 (33) |
| Other* | 37 (17) | 1 (5) | 22 (23) | 14 (13) |
| Unknown | 88 (40) | 10 (48) | 35 (36) | 43 (41) |
| Witnessed cardiac arrest | 202 (91%) | 18 (86) | 86 (90) | 98 (93) |
| Arrest Location [n (%)] | ||||
| Monitored bed | 154 (69) | 19 (90) | 70 (73) | 65 (62) |
| Endotracheal intubation [n (%)] | ||||
| Pre-cardiac arrest | 100 (45) | 8 (38) | 44 (46) | 48 (46) |
| Intra-cardiac arrest | 95 (43) | 9 (43) | 40 (42) | 46 (44) |
| Chest compression fraction [median (IQR)] |
91 (87 - 94) | 91 (87 - 95) | 92 (88 - 94) | 90 (87 - 93) |
Etiology of cardiac arrest determined not to be cardiac or respiratory; IQR, interquartile range; PEA, pulseless electrical activity; SD, standard deviation; VF, ventricular fibrillation; VT, ventricular tachycardia
Figure 1.
Distribution of mean chest compression rates over time.
Figure 2.
Proportion of patients with successful return of spontaneous circulation in relation to mean chest compression rate during the duration of cardiopulmonary resuscitation.
Table 2 displays the results of the multivariable logistic regression model with successful ROSC, good neurological outcome at hospital discharge, and preservation of neurological status as the dependent variables. Compared to the mean chest compression rate reference range (100-120 compressions/min), 121-140 compressions/min had the highest odds ratio of successful ROSC after adjusting for age, initial cardiac rhythm, pre-arrest co-morbidities, bed location, and CCF, odds ratio 4.48 (95% CI 1.42-14.14). After adding exposure to chest compression rate < 100 compressions/min into the model, 121-140 compressions/min remained statistically significant, odds ratio 3.88 (95% CI 1.02 – 14.72). The results of our additional sensitivity analyses are displayed in Table 3. Although we found the highest proportion of patients with good neurological outcome at hospital discharge among the 121-140 compressions/min group, this was not found to be statistically significant, adjusted odds ratio 2.67 (95% CI 0.30 – 24.21). Of note, the majority of our subjects [203/222 (91%)] had a CCF 81-100%. Nineteen (9%) had a CCF 61-80% and 0 subjects had a CCF less than 61%.
Table 2.
Multivariable logistic regression models: (a) successful return of spontaneous circulation as the dependent variable, (b) good neurological outcome [defined as Cerebral Performance Category (CPC) < 3 at hospital discharge] as the dependent variable, (c) preservation of neurological status, defined as no increase in CPC at hospital discharge compared to the CPC at the time of cardiac arrest as the dependent variable.
| a) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| Chest compression rate* | |||||
| 100 – 120 | Reference | ||||
| 121 – 140 | 4.48 | 1.42 | 14.14 | 2.63 | 0.010 |
| > 140 | 1.93 | 0.61 | 6.07 | 1.13 | 0.262 |
| Age (decile) | 1.09 | 0.89 | 1.34 | 0.11 | 0.402 |
| VT/VF initial rhythm | 1.86 | 0.91 | 3.79 | 0.68 | 0.089 |
| Charlson comorbidity score | 1.16 | 0.87 | 1.56 | 0.17 | 0.308 |
| Chest compression fraction | 2.45 | 0.83 | 7.17 | 1.34 | 0.103 |
| Monitored bed | 0.74 | 0.39 | 1.41 | 0.24 | 0.363 |
| b) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| Chest Compression rate* | |||||
| 100 – 120* | Reference | ||||
| 121 – 140* | 2.67 | 0.30 | 24.21 | 3.01 | 0.382 |
| > 140* | 1.32 | 0.14 | 12.36 | 1.51 | 0.808 |
| Age (decile) | 0.99 | 0.70 | 1.39 | 0.17 | 0.935 |
| VT/VF initial rhythm | 7.55 | 2.68 | 21.28 | 3.99 | 0.000 |
| Charlson comorbidity score | 0.63 | 0.39 | 1.04 | 0.16 | 0.070 |
| Chest compression fraction | 0.61 | 0.14 | 2.63 | 0.45 | 0.505 |
| Monitored bed | 0.84 | 0.26 | 2.71 | 0.50 | 0.772 |
| (c) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| Chest Compression rate* | |||||
| 100 – 120* | Reference | ||||
| 121 – 140* | 1.86 | 0.20 | 17.39 | 2.12 | 0.588 |
| > 140* | 0.92 | 0.09 | 8.97 | 1.07 | 0.943 |
| Age (decile) | 1.03 | 0.74 | 1.44 | 0.18 | 0.863 |
| VT/VF initial rhythm | 6.14 | 2.30 | 16.37 | 3.07 | 0.000 |
| Charlson comorbidity score | 0.75 | 0.47 | 1.20 | 0.18 | 0.231 |
| Chest compression fraction | 0.55 | 0.13 | 2.34 | 0.41 | 0.419 |
| Monitored bed | 0.90 | 0.30 | 2.66 | 0.50 | 0.842 |
Mean chest compression rate for duration of cardiopulmonary resuscitation (compressions/minute); LCI, lower confidence interval; UCI, upper confidence interval; VF, ventricular fibrillation; VT, ventricular tachycardia.
Table 3.
Sensitivity analyses testing the association between chest compression rate of 121-140 compressions/min (independent variable) and successful return of spontaneous circulation (dependent variable): (a) entire cohort, (b) subjects receiving mechanical ventilation prior to cardiac arrest (n = 100), (c) subjects with a clear etiology of cardiac arrest (n = 134).
| (a) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| 121 – 140* | 2.54 | 1.41 | 4.56 | 0.76 | 0.002 |
| Age (decile) | 1.11 | 0.90 | 1.35 | 0.11 | 0.326 |
| VT/VF initial rhythm | 1.85 | 0.91 | 3.74 | 0.66 | 0.087 |
| Charlson comorbidity score | 1.18 | 0.88 | 1.58 | 0.18 | 0.281 |
| Chest compression fraction | 2.46 | 0.83 | 7.24 | 1.35 | 0.103 |
| Pre-arrest mechanical ventilation | 0.79 | 0.44 | 1.41 | 0.23 | 0.423 |
| (b) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| 121 – 140* | 2.42 | 1.04 | 5.64 | 1.04 | 0.040 |
| Age (decile) | 1.06 | 0.79 | 1.41 | 0.16 | 0.709 |
| VT/VF initial rhythm | 1.40 | 0.52 | 3.77 | 0.71 | 0.509 |
| Charlson comorbidity score | 1.29 | 0.82 | 2.03 | 0.30 | 0.263 |
| Chest compression fraction | 1.99 | 0.41 | 9.56 | 1.59 | 0.391 |
| (c) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| 121 – 140* | 2.41 | 1.11 | 5.27 | 0.96 | 0.027 |
| Age (decile) | 1.10 | 0.85 | 1.43 | 0.15 | 0.475 |
| VT/VF initial rhythm | 0.73 | 0.29 | 1.81 | 0.34 | 0.497 |
| Chest compression fraction | 1.25 | 0.24 | 6.42 | 1.04 | 0.790 |
| Cardiac etiology of arrest | 3.03 | 0.96 | 9.56 | 1.78 | 0.058 |
| Respiratory etiology of arrest | 1.99 | 0.83 | 4.75 | 0.88 | 0.122 |
Mean chest compression rate for duration of cardiopulmonary resuscitation (compressions/minute); LCI, lower confidence interval; UCI, upper confidence interval; VF, ventricular fibrillation; VT, ventricular tachycardia.
Table 4 displays the adjusted logistic regression models testing narrower ranges for mean chest compression rates (i.e. 121-130, 131-140, 141-150, > 150 compressions/min) compared to the current recommended rate of 100-120 compressions/min. We found a mean chest compression rate of 121-130 compressions/min to have the highest odds ratio for successful ROSC, 5.17 (95% CI 1.38 – 19.45). A mean chest compression rate of 131-140 compressions/min was also found to have a higher odds ratio compared to the reference range, 4.21 (95% 1.28 – 13.84). We found a mean chest compression rate of 121-130 to have the highest odds ratio for good neurological outcome at hospital discharge; however, this was not found to be statistically significant, adjusted odds ratio 3.92 (95% CI 0.38 – 43.04)
Table 4.
Sensitivity analyses testing sequential intervals of ten compressions/min compared to the reference range of 100-120 compressions/min: multivariable logistic regression models testing (a) successful return of spontaneous circulation as the dependent variable, and (b) good neurological outcome [defined as Cerebral Performance Category (CPC) < 3 at hospital discharge] as the dependent variable.
| a) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| Chest compression rate* | |||||
| 100 – 120 | Reference | ||||
| 121 – 130 | 5.17 | 1.38 | 19.45 | 3.50 | 0.015 |
| 131 – 140 | 4.21 | 1.28 | 13.84 | 2.56 | 0.018 |
| 141 – 150 | 2.03 | 0.61 | 6.78 | 1.25 | 0.247 |
| > 150 | 1.78 | 0.52 | 6.15 | 1.13 | 0.360 |
| Age (decile) | 1.09 | 0.89 | 1.34 | 0.11 | 0.393 |
| VT/VF initial rhythm | 1.90 | 0.92 | 3.90 | 0.70 | 0.082 |
| Charlson comorbidity score | 1.15 | 0.86 | 1.54 | 0.17 | 0.357 |
| Chest compression fraction | 2.49 | 0.85 | 7.33 | 1.37 | 0.097 |
| Monitored bed | 0.73 | 0.38 | 1.41 | 0.25 | 0.349 |
| b) | |||||
|---|---|---|---|---|---|
| Variables | Odds Ratio | 95% LCI | 95% UCI | Standard Error | p-value |
| Chest compression rate* | |||||
| 100 – 120 | Reference | ||||
| 121 – 130 | 3.92 | 0.36 | 43.04 | 4.79 | 0.264 |
| 131 – 140 | 2.19 | 0.23 | 21.21 | 2.54 | 0.498 |
| 141 – 150 | 1.10 | 0.10 | 11.91 | 1.33 | 0.940 |
| > 150 | 1.51 | 0.15 | 15.65 | 1.80 | 0.729 |
| Age (decile) | 0.98 | 0.70 | 1.37 | 0.17 | 0.893 |
| VT/VF initial rhythm | 7.86 | 2.72 | 22.71 | 4.26 | 0.000 |
| Charlson comorbidity score | 0.61 | 0.37 | 1.02 | 0.16 | 0.057 |
| Chest compression fraction | 0.59 | 0.14 | 2.51 | 0.43 | 0.470 |
| Monitored bed | 0.72 | 0.21 | 2.48 | 0.46 | 0.609 |
Mean chest compression rate for duration of cardiopulmonary resuscitation (compressions/minute); LCI, lower confidence interval; UCI, upper confidence interval; VF, ventricular fibrillation; VT, ventricular tachycardia.
Discussion
In this study, we prospectively identified consecutive adult in-hospital cardiac arrest patients who had chest compressions performed by trained hospital personnel in a regional Cardiac Resuscitation Center, and determined the mean chest compression rate during the duration of CPR. Our objective was to test if chest compression rates during in-hospital CPR were associated with ROSC and neurological outcome. Using multivariable logistic regression, we found a mean chest compression rate of 121-140 compressions/min to have a highest odds ratio of successful ROSC. These findings suggest a higher chest compression rate than the current AHA recommendations of 100-120 compressions/min may improve the chances of successful ROSC among in-hospital cardiac arrest patients.
Our sensitivity analyses found a mean chest compression rate of 121-130 compression/min to have the strongest association with successful ROSC. This finding is in line with a previous observational study of OHCA patients, which found ROSC rates peaked at a chest compression rate of 125 compressions/min.8 However, a second observational study of OHCA patients from the same group, found an association between an average chest compression rate of 100-120 compressions/min and survival to hospital discharge compared to higher and lower rates.9 There are several important differences between our patient population and the patient populations in these previous studies. First, our subjects all received in-hospital CPR from Cardiac Resuscitation Center trained hospital personnel with the patient in a stationary location, and thus overall likely to have better CPR quality compared to EMS who are burdened with the additional task of transporting the patient;10,25 this is supported by our noticeably higher CCF (91% vs. 70%).9 Our high CCF is likely secondary to the fact that the majority of our subjects were intubated prior to (45%), or rapidly during (43%), cardiac arrest. Once a definitive airway was established our clinicians followed the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, which recommends ten breaths per minute while performing continuous chest compressions.26 Thus our high proportion of intubated subjects removed the need to pause chest compressions to administer ventilation breaths. Second, our overall mean chest compression rate was higher than the aforementioned studies (139 vs. 111 and 112 compressions/min).8,9 None of the subjects in our cohort had an initial mean chest compression rate less than 100 compressions/min compared to 27%,9 with chest compression rates as low as 45 compressions/min,8 in the previous studies. In addition, in our cohort the majority (90%) had a mean chest compression rate greater than 120 compressions/min compared to 25% in a previous study.9 Our data was prospectively collected during the era of the 2010 AHA guidelines (i.e. recommended chest compression goals were a rate of at least 100 compressions/min). CPR training at our institution did not endorse a specific chest compression rate other than to reinforce maintaining rates above 100 compressions/min. Real time feedback devices were not used to monitor CPR quality during in-hospital cardiac arrest. None of the chest compression providers were aware of this study; however, providers were aware CPR quality measures were being recorded and reviewed by our Hospital Code Committee for quality improvement. This knowledge of being monitored and our CPR training reinforcing prevention of chest compression rates below 100 compression/min could potentially explain our high chest compression rates. Our training in frequent and rapid compressor exchanges likely prevents fatigue and ensures continued high quality chest compressions, which can be difficult to maintain at these higher rates.9,25,27 At least three individuals are available to perform compressions during a cardiac arrest at our institution and chest compression providers are educated to rotate compressors every two minutes, or earlier if the active chest compression provider feels fatigued or is identified by another team member to have a decline in chest compression quality. Finally, compared to the previously mentioned studies, we determined the mean chest compression rate over the full duration of CPR as opposed to the initial five minutes of CPR.8,9
Support for chest compression rates as high as 120 is drawn from animal models, which demonstrated increase in blood flow and survival with chest compression rates of 120 compressions/min compared to 60 compressions/min.28,29 Additional studies in humans found improved end-tidal carbon dioxide (EtCO2), a surrogate marker of blood flow, with rates of 120 compressions/min compared to lower rates.30 These initial animal and human studies did not investigate chest compression rates above 120 compressions/min.
One concern of higher chest compression rates is a decreased time in diastole and thus a decreased time to perfuse the coronary arteries. One animal model found increasing rates to 150 compressions/min increased cardiac output (CO) and diastolic pressure, which increased peak diastolic coronary blood flow velocity and systolic coronary blood flow. However, given the decrease time in diastole they concluded coronary perfusion to be optimized at a rate of 120 compressions/min.31 A second animal study found increasing rates to 150 compressions/min increased mean arterial pressure (MAP) and CO while maintaining coronary blood flow.32 These findings support the idea that higher chest compression rates could potentially attenuate the ischemic neurological injury caused by cardiac arrest by increasing cerebral perfusion through increased blood pressure and CO, while maintaining coronary blood flow to allow for successful ROSC. Our results demonstrating increased odds of successful ROSC among subjects who received chest compression rates higher than the current AHA recommendations of 100-120 compressions/min suggest adequate coronary blood flow is maintained at these higher rates.
We acknowledge that this study has important limitations to consider. First, we found a mean chest compression rate of 121-140 compressions/min to have a large odds ratio for successful ROSC compared to previous studies. Although we hypothesize this increase in ROSC is secondary to improved cardiac output and coronary blood flow at these higher rates, we did not measure coronary or cerebral blood flow, or end-tidal carbon dioxide in our subjects, and therefore were unable to determine the direct effects of chest compression rates on hemodynamics during CPR. Second, although we used multivariable logistic regression analyses to adjust for CCF and other cardiac arrest characteristics known to predict outcome, there still exists the potential of unmeasured confounders, which could have influenced our results. For example we did not account for cause of death in those subjects who did not survive to hospital discharge. Cause of death is often determined subjectively or is unknown all together; therefore, we were unable to use the cause of death in our analyses. Similarly we were unable to determine the etiology of cardiac arrest for a large proportion of subjects (40%). We therefore were limited in adjusting our sensitivity analysis for etiology of cardiac arrest. Third, we did not measure depth of compressions during CPR. Inadequate chest compression depth has been associated with poor clinical outcomes and chest compression depth plays an important role in CPR quality.33,34 However, measurement of chest compression depth can be difficult to obtain in clinical practice and is often inaccurate as it is known to be affected by the compliant and variable surfaces on which cardiac arrest patients are positioned during CPR in the hospital setting, regardless of whether or not CPR backboards are used.35,36 In regards to compression depth, it has previously been demonstrated that higher chest compression rates are associated with a decrease in chest compression depth.9,25 However, the same group found including depth in their multivariable model did not change the estimated relationship between chest compression rate and ROSC or between chest compression rate and survival among OHCA patients.8 In our sample, if this inverse relationship held true, and did influenced the relationship between chest compression rate and ROSC, we would expect the 120-140 compressions/min group to have a greater proportion of subjects with inadequate chest compression depth compared to the 100-120 compressions/min group, and thus we would expect adjusting for compression depth would potentially increase, not decrease, the odds ratio of ROSC in the 121-140 compressions/min group compared to the 100-120 compressions/min group. However, chest compression depth is still a potential important confounder of our results. Fourth, we utilized software to measure both the chest compression rate and CCF. The accuracy of such software is a potential limitation; however, the use of this software has been previously tested and is in line with previous studies.8,9 Fifth, previous literature has demonstrated an association between CCF and ROSC.3 We did not find a statistically significant association at the α = 0.05 level in this study (p = 0.10 in the multivariable model). This is likely explained by the fact that we had minimal variability in CCF; all of our subjects received a chest compression rate greater than 60% and the majority (91%) received a CCF greater than 81%. Sixth, we found a higher proportion of patients with good neurological outcome at hospital discharge among the 121-140 compressions/min group compared to the 100-120 compressions/min group, 11% vs. 5% respectively. However, this finding was not statistically significant in our cohort; possibly secondary to the high proportion of patients with a CPC of 5 (death), resulting in not enough power to find a statistically significant difference in neurological outcome. Although our overall survival and survival with good neurological outcome at hospital discharge were low (15% and 10% respectively), given the majority of our subjects had PEA/asystole as the initial cardiac rhythm our findings are in line with other recently published studies.37-39 A larger study in this patient population is warranted to further examine the relationship between chest compression rates and cognitive and functional outcomes among survivors.40 Seventh, this study was limited to a single center. Lastly, this was an observational study and thus we can only report association rather than infer causation. We were unable to report on who initiated CPR (i.e. unit nurse or response team). It is possible providers compress faster for subjects they believe have a higher chance of good outcome.
Conclusion
In this sample of adult in-hospital cardiac arrest patients, we found a chest compression rate of 121-140 compressions/min to have the highest odds ratio of successful ROSC. These data suggest that chest compression rates above the AHA and ILCOR recommended 100-120 compressions/min may improve the chances of successful ROSC among in-hospital cardiac arrest patients. Further research is required to test the association between higher chest compression rates and neurological outcome.
Acknowledgements
Dr. Trzeciak’s effort to this project was supported by a grant from the National Institutes of Health/National Heart, Lung, and Blood Institute (R01HL112185). Dr. Roberts’ effort to this project was supported by a grant from the National Institutes of Health/National Heart, Lung, and Blood Institute (K23HL126979).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest statement
None of the authors have potential financial conflicts of interest to disclose. Physiocontrol/Medtronic provided the Code Stat software free of charge to Cooper University Health Care for the purpose of conducting CPR quality assurance and research. There was no other financial arrangement or payments other than the provision of the Code Stat software.
References
- 1.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S414–435. doi: 10.1161/CIR.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 4.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. Jama. 1960;173:1064–1067. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 5.Berg RA, Hemphill R, Abella BS, et al. Part 5: adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S685–705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 6.Koster RW, Baubin MA, Bossaert LL, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Asourceult basic life support and use of automated external defibrillators. Resuscitation. 2010;81(10):1277–1292. doi: 10.1016/j.resuscitation.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perkins GD, Travers AH, Berg RA, et al. Part 3: Adult basic life support and automated external defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95:e43–69. doi: 10.1016/j.resuscitation.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 8.Idris AH, Guffey D, Aufderheide TP, et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125(24):3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Idris AH, Guffey D, Pepe PE, et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015;43(4):840–848. doi: 10.1097/CCM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 10.Krarup NH, Terkelsen CJ, Johnsen SP, et al. Quality of cardiopulmonary resuscitation in out-of-hospital cardiac arrest is hampered by interruptions in chest compressions--a nationwide prospective feasibility study. Resuscitation. 2011;82(3):263–269. doi: 10.1016/j.resuscitation.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Roberts BW, Kilgannon JH, Mitchell JA, et al. Emergency department inter-hospital transfer for post-cardiac arrest care: initial experience with implementation of a regional cardiac resuscitation center in the United States. Resuscitation. 2013;84(5):596–601. doi: 10.1016/j.resuscitation.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Stecher FS, Olsen JA, Stickney RE, Wik L. Transthoracic impedance used to evaluate performance of cardiopulmonary resuscitation during out of hospital cardiac arrest. Resuscitation. 2008;79(3):432–437. doi: 10.1016/j.resuscitation.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110(21):3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 14.Langhelle A, Nolan J, Herlitz J, et al. Recommended guidelines for reviewing, reporting, and conducting research on post-resuscitation care: the Utstein style. Resuscitation. 2005;66(3):271–283. doi: 10.1016/j.resuscitation.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trzeciak S, Jones AE, Kilgannon JH, et al. Outcome measures utilized in clinical trials of interventions for post-cardiac arrest syndrome: a systematic review. Resuscitation. 2009;80(6):617–623. doi: 10.1016/j.resuscitation.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaul GB, Gruska M, Titscher G, et al. Prediction of survival after out-of-hospital cardiac arrest: results of a community-based study in Vienna. Resuscitation. 1996;32(3):169–176. doi: 10.1016/0300-9572(96)00956-2. [DOI] [PubMed] [Google Scholar]
- 18.Hajbaghery MA, Mousavi G, Akbari H. Factors influencing survival after in-hospital cardiopulmonary resuscitation. Resuscitation. 2005;66(3):317–321. doi: 10.1016/j.resuscitation.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Langhelle A, Tyvold SS, Lexow K, Hapnes SA, Sunde K, Steen PA. In-hospital factors associated with improved outcome after out-of-hospital cardiac arrest. Asource between four regions in Norway. Resuscitation. 2003;56(3):247–263. doi: 10.1016/s0300-9572(02)00409-4. [DOI] [PubMed] [Google Scholar]
- 20.Murray SB, Bates DW, Ngo L, Ufberg JW, Shapiro NI. Charlson Index is associated with one-year mortality in emergency department patients with suspected infection. Acad Emerg Med. 2006;13(5):530–536. doi: 10.1197/j.aem.2005.11.084. [DOI] [PubMed] [Google Scholar]
- 21.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. Jama. 2006;295(1):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 22.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 23.Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. Isource. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48(12):1503–1510. doi: 10.1016/0895-4356(95)00048-8. [DOI] [PubMed] [Google Scholar]
- 24.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 25.Monsieurs KG, De Regge M, Vansteelandt K, et al. Excessive chest compression rate is associated with insufficient compression depth in prehospital cardiac arrest. Resuscitation. 2012;83(11):1319–1323. doi: 10.1016/j.resuscitation.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S444–464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 27.McDonald CH, Heggie J, Jones CM, Thorne CJ, Hulme J. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Emerg Med J. 2013;30(8):623–627. doi: 10.1136/emermed-2012-201610. [DOI] [PubMed] [Google Scholar]
- 28.Feneley MP, Maier GW, Kern KB, et al. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988;77(1):240–250. doi: 10.1161/01.cir.77.1.240. [DOI] [PubMed] [Google Scholar]
- 29.Harris LC, Kirimli B, Safar P. Ventilation-cardiac compression rates and ratios in cardiopulmonary resuscitation. Anesthesiology. 1967;28(5):806–813. doi: 10.1097/00000542-196709000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Kern KB, Sanders AB, Raife J, Milander MM, Otto CW, Ewy GA. A study of chest compression rates during cardiopulmonary resuscitation in humans. Tsource importance of rate-directed chest compressions. Archives of internal medicine. 1992;152(1):145–149. [PubMed] [Google Scholar]
- 31.Wolfe JA, Maier GW, Newton JR, Jr., et al. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988;95(3):523–532. [PubMed] [Google Scholar]
- 32.Maier GW, Tyson GS, Jr., Olsen CO, et al. The physiology of external cardiac massage: high-impulse cardiopulmonary resuscitation. Circulation. 1984;70(1):86–101. doi: 10.1161/01.cir.70.1.86. [DOI] [PubMed] [Google Scholar]
- 33.Enohumah KO, Moerer O, Kirmse C, Bahr J, Neumann P, Quintel M. Outcome of cardiopulmonary resuscitation in intensive care units in a university hospital. Resuscitation. 2006;71(2):161–170. doi: 10.1016/j.resuscitation.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 34.Vadeboncoeur T, Stolz U, Panchal A, et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014;85(2):182–188. doi: 10.1016/j.resuscitation.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Perkins GD, Kocierz L, Smith SC, McCulloch RA, Davies RP. Compression feedback devices over estimate chest compression depth when performed on a bed. Resuscitation. 2009;80(1):79–82. doi: 10.1016/j.resuscitation.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 36.Noordergraaf GJ, Paulussen IW, Venema A, et al. The impact of compliant surfaces on in-hospital chest compressions: effects of common mattresses and a backboard. Resuscitation. 2009;80(5):546–552. doi: 10.1016/j.resuscitation.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 37.Donnino MW, Salciccioli JD, Howell MD, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. Bmj. 2014;348:g3028. doi: 10.1136/bmj.g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. Jama. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 39.McHugh MD, Rochman MF, Sloane DM, et al. Better Nurse Staffing and Nurse Work Environments Associated With Increased Survival of In-Hospital Cardiac Arrest Patients. Medical care. 2016;54(1):74–80. doi: 10.1097/MLR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Becker LB, Aufderheide TP, Geocadin RG, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation. 2011;124(19):2158–2177. doi: 10.1161/CIR.0b013e3182340239. [DOI] [PMC free article] [PubMed] [Google Scholar]