Abstract
Introduction
The relationship between low income and worse health outcomes is evident, yet its association with cognitive outcomes is less explored. Most studies have measured income at one time and none have examined how sustained exposure to low income influences cognition in a relatively young cohort. This study examined the effect of sustained poverty and perceived financial difficulty on cognitive function in midlife.
Methods
Income data were collected six times between 1985 and 2010 for 3,383 adults of the Coronary Artery Risk Development in Young Adults prospective cohort study. Sustained poverty was defined by the percentage of time participants’ household income was <200% of the federal poverty level—“never” in poverty, “0< to <1/3,” “≥1/3 to <100%” or “all-time.” In 2010, at a mean age of 50 years, participants underwent a cognitive battery. Data were analyzed in 2015.
Results
In demographic-adjusted linear regression models, individuals with all-time poverty performed significantly worse than individuals never in poverty: 0.92 points less on verbal memory (z-score, −0.28; 95% CI= −0.43, −0.13), 11.60 points less on processing speed (z-score, −0.72; 95% CI= −0.85, −0.58), and 3.50 more points on executive function (z-score, −0.32; 95% CI= −0.47, −0.17). Similar results were observed with perceived financial difficulty. Findings were robust when restricted to highly educated participants, suggesting little evidence for reverse causation.
Conclusions
Cumulative exposure to low income over 2 decades was strongly associated with worse cognitive function of a relatively young cohort. Poverty and perceived hardship may be important contributors to premature aging among disadvantaged populations.
Introduction
The recent increase in income inequality in the U.S. suggests that a large proportion of the population faces economic hardship.1 Individuals with low income may lack appropriate resources to follow healthy lifestyles and access care, resulting in disproportionate exposure to unfavorable health outcomes. Maintaining cognitive abilities is a key component of health and daily quality of life, and previous research has shown that exposure to poor socioeconomic conditions during childhood, adulthood, or cumulatively—mostly as a summary composite score of multiple socioeconomic factors, each measured one time—is associated with cognitive deficits.2–12 Yet, the majority of these studies involved older adults and thus it remains unknown whether economic adversity influences cognitive health much earlier in the life course. Furthermore, most previous studies relied on a single measure of socioeconomic adversity, which has rarely been income, or have measured income at only one point in time.
Income is dynamic and individuals are likely to experience income changes in response to economic trends or shocks.13–15 Studies suggest that most individuals experience some sort of income mobility between young adulthood and midlife.13,16 Therefore, monitoring changes in income and financial difficulty over an extended period of time and how these influence cognitive health will have important implications for public health policy. To the authors’ knowledge, most prior studies of income and health, especially cognitive health, have used one or two measurements of income,2,9–12 and thus fail to capture the effect of sustained exposure to low income on cognitive health.6
The study objective is to use repeated data of various economic parameters to examine the associations of sustained poverty and perceived financial difficulty on cognitive function in a cohort of young to middle-aged black and white adults of the Coronary Artery Risk Development in Young Adults (CARDIA) study.
Methods
Study Population
A total of 5,115 adults aged 18–30 years at baseline in 1985–1986 were recruited into the CARDIA study from four field centers: the University of Alabama at Birmingham, the University of Minnesota, Northwestern University, and Kaiser Permanente (Oakland, CA). Recruitment was balanced within center by sex, age, and education. Participants were examined at baseline and at follow-up examinations 2, 5, 7, 10, 15, 20, and 25 years after baseline. Standardized protocols were used to gather demographic, social, and clinical data. Details of the study have been described elsewhere.17 Cognitive function was assessed at Year 25. The study was approved by the appropriate IRBs, and informed consent was obtained from study participants. The present analysis was approved by the Publications and Presentations committee of the CARDIA study.
Measures
Sustained poverty was defined as the percentage of times between 1990 and 2010 that participants reported total household incomes that were <200% of the federal poverty level (FPL). The 200% cut point was used in accordance with the literature.6,18 Owing to the dose–response relationship between income and cognition, categories were defined as: “never” in poverty, “0< to <1/3 of the time,” “≥1/3 of the time to <100% of the time,” or “all-time.” Income data collected in 1990, 1992, 1995, 2000, 2005, and 2010 were used. More than 85% of the sample had at least five repeated income measurements. Pre-tax household income for the past 12 months from all sources was self-reported and recorded in income categories. The category midpoint was chosen as the participant’s income for that year (Appendix Table 1). Using income category midpoint and family size at each examination period, Census Bureau FPL thresholds19 were then used to identify households with incomes that were <200% of the FPL for that relevant year. The income cut offs for 200% of the FPL for a four-person household were $26,718 in 1990, $28,670 in 1992, $31,138 in 1995, $35,206 in 2000, $39,942 in 2005, and $44,630 in 2010.
Participants also repeatedly reported, at seven of the total eight study visits, their overall perceived difficulty in paying for basics such as food and heating. More than 70% of the sample had all seven repeated measurements of financial difficulty. Responses included: very hard, hard, somewhat hard, or not very hard. For each year, these groups were dichotomized into reporting “at least somewhat hard” versus “not very hard.”16 Sustained perceived financial difficulty was calculated as the percentage of times between 1985 and 2010 that participants reported difficulty with categories of: never, 0< to <1/3, ≥1/3 to <100%, or all-time.
At Year 25, all CARDIA participants were administered a cognitive battery that included three tests. The Rey Auditory–Verbal Learning Test (range, 0–15) measures verbal memory and assesses the ability to memorize and retrieve words, with higher score (in words) indicating better performance.20 The Digit Symbol Substitution Test (range, 0–133) is a subtest of the Wechsler Adult Intelligence Scale and measures performance on speed domains, with higher score (in symbols) indicating better performance.21 The interference score on the Stroop test (executive skills) measures the additional amount of processing needed to respond to one stimulus while suppressing another. The test was scored by seconds to spell out color words printed in a different color plus number of errors, thus higher score (seconds + errors) indicates worse performance.22 All three tests are widely used in the literature and are sensitive to detecting cognitive aging.
The CARDIA participants reported their sex, race, years of education, their parents’ years of education (highest of mother and father), and marital status. Lifetime cigarette pack years and daily alcohol use were calculated based on an interviewer-administered questionnaire. Participants reported the amount of time spent weekly in 13 categories of physical activity over the past year, and then the total amount in exercise units was calculated. BMI (kg/m2) was calculated using measured weight and height. Blood pressure was measured while seated using a standard automated blood pressure monitor. Type 2 diabetes was ascertained based on fasting glucose levels ≥126 mg/dL, self-reported medication use, a 2-hour postload glucose ≥200 mg/dL, or hemoglobin A1c ≥6.5%. Symptoms of depression were assessed using the 20-item Center for Epidemiologic Studies Depression Scale.23
For time-varying covariates, including mL of alcohol use, physical activity units, BMI, systolic and diastolic blood pressure, and depressive symptoms, previously published statistical techniques24 were followed to calculate cumulative exposure as a time-weighted average of each covariate over the study period.
Statistical Analysis
Participant characteristics were assessed across categories of sustained poverty and perceived financial difficulty. Differences in means and proportions between categories of sustained poverty and financial difficulty were tested using ANOVAs and chi-square tests, respectively. Using the Year 1990 dollar, average income was illustrated at each time point between 1990 and 2010 adjusted for inflation based on the Consumer Price Index.25
Multivariable linear regression models were used to examine the associations between each economic predictor and cognitive function. For ease of interpretation, the results were presented using standardized differences, with negative z-score indicative of worse cognitive performance. Covariates were included based on a priori literature and their associations with income and cognition. Potential confounders, including Year 25 age, sex, race, parental education, marital status, and study site, were first added. Next, education was added to the model. Then, potential explanatory factors, including diabetes status, history of coronary heart disease, lifetime cigarette pack years, and time-weighted averages of time-varying covariates, including physical activity, daily alcohol, BMI, systolic and diastolic blood pressure, and depressive symptoms were added in a separate final model. In model assessment, effect modification by race, sex, and education were each examined using interaction terms. Interactions were not significant (all p-values >0.05).
To address possible reverse causation, that is, that poor cognitive health caused poverty and economic hardship, two sensitivity analyses were conducted. Given the strong associations among cardiovascular and behavioral risk factors, education, and cognitive health,26,27 it was hypothesized that individuals who at baseline were healthy or had high education were less likely to have substantial cognitive deficits. As a first sensitivity analysis, the sample was restricted to participants without any known cardiovascular risk factors at baseline, including BMI <25 kg/m2, no high blood pressure, no diabetes, and no history of coronary heart disease (n=1,912). As a second sensitivity analysis, the sample was restricted to participants with more than high school education at baseline (n=2,218) as a proxy for high cognitive reserve.28 Finally, as income <200% of FPL may not fully account for conditions of economic deprivation,29 a sensitivity analysis was conducted in which perceived financial difficulty was additionally adjusted for in multivariable models of sustained poverty. All analyses were performed with Stata, version 14 _ and SAS, version 9.3. Significance testing was two-sided with a 5% significance level. Analyses were conducted in 2015.
Results
Of the 3,498 participants who participated at Year 25, the authors excluded 115 subjects who had missing cognitive battery, resulting in a final analytic sample of 3,383. There were no subjects missing data in the covariates of interest. Comparison of participants who were included in this analysis with those who were lost to follow-up revealed that the latter participants were more likely to be black and to have experienced all-time poverty (data not shown).
As shown in Table 1, 25.4% of the participants had all-time or ≥1/3 of the time income below 200% of the FPL between 1990 and 2010. Those with all-time or ≥1/3 of time in poverty were more likely to be women, black, have a high school education or less, have lower parental education, and more likely to have higher number of depressive symptoms, be less physically active, have higher BMI, and higher diastolic and systolic BP. Similar characteristic distribution was observed across categories of perceived financial difficulty. Participants with economic hardship performed significantly worse on each of the three cognitive tests—lower mean scores on the Rey Auditory–Verbal Learning Test and Digit Symbol Substitution Test, and higher mean scores on the Stroop test.
Table 1.
Characteristics of Study Participants According to Categories of Economic Hardship, CARDIA Study 1985 to 2010
| Characteristics | Sustained poverty: % of time income was <200% of FPL Mean (SD) or % |
% of time financial difficulty was reported Mean (SD) or % |
||||||
|---|---|---|---|---|---|---|---|---|
| Never 1771 (52.4) |
<1/3 754(22.3) |
≥1/3 574 (17.0) |
All-time 284(8.4) |
Never 1187(35.1) |
<1/3 1,167(24.5) |
≥1/3 952 (28.1) |
All-time 77 (2.3) |
|
| Age b,c | 50.7 (3.3) | 49.6 (3.8) | 49.4 (3.9) | 49.3 (3.9) | 50.5 (3.5) | 50.0 (3.6) | 50.0 (3.8) | 50.8 (3.2) |
| Women b,c | 53.9% | 55.8% | 60.3% | 65.5% | 52.2% | 55.7% | 61.0% | 72.7% |
| Black b,c | 31.3% | 46.8% | 72.0% | 87.3% | 33.0% | 48.5% | 59.1% | 61.0% |
| <HS education b,c | 11.3% | 19.8% | 39.0% | 64.8% | 11.5% | 20.5% | 36.7% | 41.6% |
| Average income, $ b,c | $52,120 | $35,894 | $21,810 | $9,446 | $50,393 | $40,420 | $27,365 | $19,905 |
| Parent’s education, yr b,c | 14.5 (3.1) | 14.1 (3.0) | 12.9 (3.0) | 11.9 (2.6) | 14.7 (3.0) | 14.0 (3.1) | 13.1 (3.0) | 12.1 (3.3) |
| Physical activity a,b,c | 475.0 (215.4) | 460.9 (223.4) | 416.2 (209.3) | 349.5 (196.6) | 480.4 (224.1) | 454.6 (215.7) | 416.1 (209.2) | 390.0 (184.9) |
| Alcohol use, ML a,b,c | 13.0 (12.8) | 12.9 (15.6) | 15.9 (21.3) | 17.9 (21.9) | 12.7 (12.8) | 13.9 (16.6) | 15.3 (18.2) | 15.1 (23.3) |
| Lifetime cigarette py b,c | 3.8 (8.4) | 4.7 (9.6) | 7.2 (11.0) | 8.6 (11.0) | 2.9 (7.0) | 4.9 (9.3) | 7.5 (11.2) | 9.1 (11.9) |
| BMI, kg/m2 a,b,c | 26.4 (5.0) | 27.2 (5.9) | 28.3 (6.2) | 29.1 (7.0) | 26.1 (5.4) | 27.3 (5.7) | 28.0 (6.0) | 28.7 (7.0) |
| Diastolic BP, mmHg a,b,c | 70.1 (6.4) | 70.6 (6.3) | 71.6 (6.7) | 72.4 (6.7) | 70.2 (6.4) | 70.8 (6.5) | 71.1 (6.5) | 70.8 (7.1) |
| Systolic BP, mmHg a,b,c | 111.6 (8.4) | 112.9 (8.7) | 113.6 (8.8) | 114.9 (9.6) | 111.7 (8.3) | 112.6 (8.9) | 113.2 (8.7) | 114.0 (10.9) |
| CES-D score a,b,c | 9.0 (5.3) | 10.5 (5.9) | 12.8 (7.2) | 16.4 (8.0) | 8.2 (5.0) | 10.1 (5.7) | 13.5 (7.2) | 16.9 (7.8) |
| Diabetes b,c | 16.4% | 18.6% | 20.7% | 28.9% | 15.1% | 18.4% | 21.7% | 40.3% |
| RAVLT score (0–15) b,c | 8.8 (3.2) | 8.5 (3.2) | 7.4 (3.3) | 6.4 (3.1) | 8.8 (3.2) | 8.3 (3.3) | 7.8 (3.3) | 7.6 (3.3) |
| DSST score (8–125) b,c | 74.1 (14.7) | 70.7 (15.1) | 63.7 (15.7) | 54.4 (15.7) | 74.5 (15.3) | 70.2 (15.4) | 64.7 (16.3) | 59.9 (15.6) |
| Stroop score (−46 to 127) b,c | 20.7 (8.9) | 22.2 (10.5) | 25.9 (13.0) | 30.8 (14.4) | 20.7 (9.6) | 22.5 (10.5) | 25.1 (12.1) | 28.5 (16.0) |
Indicates that the covariate was calculated as a time-weighted average (TWA) over the 25-year study period.
Indicates characteristic differs (p<0.05) across poverty groups based on ANOVA for continuous data and chi-square tests for categorical data.
Indicates characteristic differs (p<0.05) across financial difficulty groups based on ANOVA for continuous data and chi-square tests for categorical data.
BP, blood pressure; DSST, Digit Symbol Substitution Test; HS, high school; RAVLT, Rey Auditory Verbal Learning Test; CARDIA, Coronary Artery Risk Development in Young Adults Study; py, Pack Years; CES-D, Center for Epidemiologic Studies Depression Scale; ML, Milliliter
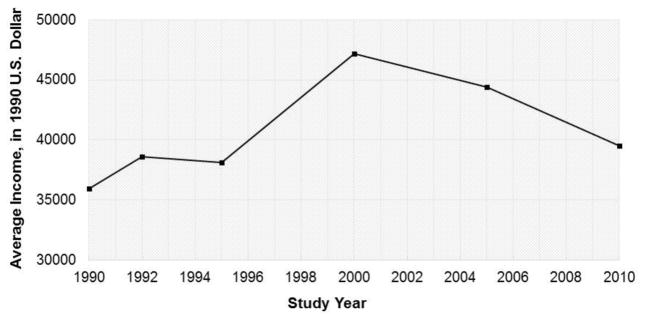
Figure 1 illustrates the trend in average household income between 1990 and 2010 using Year 1990 dollars. Average income was highest around 2000 and started decreasing since then.
Figure 1.
Average inflation-adjusted household income in the CARDIA Study between 1990 and 2010. Average income at each time point was adjusted for inflation based on the consumer price index. Income reported using the 1990 dollar.
There were significant and graded associations between sustained poverty and all three cognitive tests (Table 2). In a linear regression model adjusted for sociodemographic risk factors including education, compared with subjects who never experienced poverty between 1990 and 2010, those in poverty showed worse performance on all three cognitive tests (e.g., all-time poverty: verbal memory, −0.28, 95% CI= −0.43, −0.13; processing speed, −0.72, 95% CI= −0.85, −0.58; executive function, −0.32, 95% CI= −0.47, −0.17). In raw cognitive terms, compared with individuals who never experienced poverty, those with all-time poverty scored 0.92 points lower on the test of verbal memory, 11.60 points lower on the test of processing speed, and 3.50 points higher (i.e., worse) on the test of executive function. Additional adjustment for behavioral and cardiovascular disease risk factors slightly attenuated the associations but they remained significant.
Table 2.
Associations Between Markers of Sustained Economic Hardship and Cognitive Function
| Sustained poverty (i.e. % times income <200% of FPL) | Sustained perceived financial difficulty | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Demographic-adjusteda | + Education | + CVRFsb | Demographic-adjusteda | + Education | + CVRFsb | |
| Standardized difference (95% CI) | Standardized difference (95% CI) | |||||
| Verbal memory (N=3,363) | ||||||
| All-time | −0.42 (−0.57, −0.28) | −0.28 (−0.43, −0.13) | −0.26 (−0.41, −0.11) | −0.22 (−0.45, −0.003) | −0.13 (−0.35, 0.09) | −0.05 (−0.28, 0.17) |
| ≥1/3 | −0.17 (−0.27, −0.07) | −0.09 (−0.19, 0.01) | −0.08 (−0.18, 0.02) | −0.11 (−0.20, −0.03) | −0.04 (−0.13, 0.04) | −0.01 (−0.10, 0.08) |
| <1/3 | −0.01 (−0.09, 0.07) | 0.02 (−0.06, 0.10) | 0.03 (−0.05, 0.11) | −0.05 (−0.13, 0.03) | −0.02 (−0.10, 0.05) | −0.01 (−0.09, 0.07) |
| Never | Ref | Ref | Ref | Ref | Ref | Ref |
| Processing speed (N=3,368) | ||||||
| All-time | −0.91 (−1.04, −0.77) | −0.72 (−0.85, −0.58) | −0.61 (−0.75, −0.47) | −0.63 (−0.85, −0.42) | −0.51 (−0.71, −0.30) | −0.33 (−0.54, −0.12) |
| ≥1/3 | −0.42 (−0.52, −0.33) | −0.31 (−0.40, −0.22) | −0.25 (−0.34, −0.15) | −0.38 (−0.46, −0.30) | −0.29 (−0.37, −0.21) | −0.18 (−0.27, −0.10) |
| <1/3 | −0.16 (−0.24, −0.09) | −0.12 (−0.20, −0.05) | −0.10 (−0.17, −0.02) | −0.17 (−0.25, −0.10) | −0.14 (−0.21, −0.06) | −0.10 (−0.17, −0.03) |
| Never | Ref | Ref | Ref | Ref | Ref | Ref |
| Executive function (N=3,350) | ||||||
| All-time | −0.44 (−0.58, −0.29) | −0.32 (−0.47, −0.17) | −0.25 (−0.41, −0.10) | −0.44 (−0.66, −0.21) | −0.36 (−0.58, −0.13) | −0.26 (−0.49, −0.03) |
| ≥1/3 | −0.25 (−0.35, −0.14) | −0.18 (−0.28, −0.07) | −0.13 (−0.24, −0.03) | −0.16 (−0.24, −0.07) | −0.10 (−0.19, −0.02) | −0.03 (−0.12, 0.06) |
| <1/3 | −0.07 (−0.15, 0.01) | −0.04 (−0.12, 0.04) | −0.02 (−0.10, 0.07) | −0.05 (−0.13, 0.02) | −0.03 (−0.11, 0.04) | −0.01 (−0.08, 0.07) |
| Never | Ref | Ref | Ref | Ref | Ref | Ref |
Note: Boldface indicates statistical significance (p<0.05).
Demographics include: age, sex, race, marital status, parental education, and study site.
CVRFs include diabetes status, history of coronary heart disease, lifetime cigarette pack years, and time-weighted averages for ml of daily alcohol consumption, total physical activity units, BMI, SBP, DBP, and depressive symptoms.
CVRF, Cardiovascular Risk Factors; SBP, Systolic Blood Pressure; DBP, Diastolic Blood Pressure.
In sociodemographic-adjusted linear regression models (Table 2), compared with those who never reported perceived financial difficulty, those who reported difficulties performed worse on processing speed (e.g., all-time, −0.51, 95% CI= −0.71, −0.30) and executive function (e.g. all-time, −0.36, 95% CI= −0.58, −0.13), but not on verbal memory. In raw cognitive terms, in a fully adjusted model, compared with individuals who never reported financial difficulty, those who reported all-time difficulty scored 8.18 points lower on the test of processing speed and 3.94 points higher (i.e., worse) on the test of executive function. Additional adjustment for behavioral and cardiovascular disease risk factors slightly attenuated the associations but they remained significant.
Though there were no significant interactions by race or sex, stratification revealed stronger effect sizes in blacks and women. Results from the sensitivity analyses revealed comparable if not more pronounced results when restricted to healthy participants at baseline (Appendix Table 2) and slightly attenuated but still significant results when restricted to those with a high level of education at baseline (Table 3). Finally, with additional adjustment for perceived financial difficulty in models where sustained poverty was the main predictor, the effect sizes of sustained poverty were unchanged and thus independent of perceived financial difficulty.
Table 3.
Demographic-Adjusted Associationsa of Poverty and Perceived Financial Difficulty With Cognitive Performance Among High School Graduates (N=2,218)
| Standardized difference (95% CI) | ||
|---|---|---|
|
| ||
| % Time in poverty | % Time financial difficulty | |
| Verbal memory | ||
| All-time | −0.30 (−0.58, −0.02) | −0.33 (−0.64, −0.01) |
| ≥1/3 | −0.06 (−0.19, 0.08) | −0.05 (−0.15, 0.06) |
| <1/3 | 0.06 (−0.04, 0.15) | −0.02 (−0.11, 0.07) |
| Never | Ref | Ref |
| Processing speed | ||
| All-time | −0.59 (−0.85, −0.32) | −0.45 (−0.75, −0.15) |
| ≥1/3 | −0.17 (−0.30, −0.04) | −0.27 (−0.37, −0.17) |
| <1/3 | −0.10 (−0.19, −0.01) | −0.15 (−0.23, −0.06) |
| Never | Ref | Ref |
| Executive function | ||
| All-time | −0.30 (−0.56, −0.04) | −0.39 (−0.68, −0.09) |
| ≥1/3 | −0.09 (−0.22, 0.04) | −0.06 (−0.15, 0.04) |
| <1/3 | −0.02 (−0.10, 0.07) | −0.03 (−0.11, 0.04) |
| Never | Ref | Ref |
Note: Boldface indicates statistical significance (p<0.05).
Adjusted for age, sex, race, marital status, parental education, study site, and education.
Analysis restricted to CARDIA participants with more than high school education at baseline.
CARDIA, Coronary Artery Risk Development in Young Adults Study
Discussion
The findings support strong and graded associations of sustained exposure to poverty and perceived financial difficulty across 25 years with worse cognitive function in a relatively young cohort. The consistency of findings (in direction and statistical significance), especially in regard to processing speed outcome, across two related but separate economic parameters is quite important. The findings reveal a clear graded relationship such that cognitive performance, processing speed in particular, was worse with further cumulative exposure to economic adversity. The overall magnitude of the associations suggest that economic adversities experienced in young adulthood are important determinants of cognitive health in midlife. From a mechanistic perspective, economic hardship may be on the pathway and an important contributor to clinically significant cognitive deficit and premature aging among economically disadvantaged individuals. Furthermore, in analyses restricted to participants with a high level of education, significant associations were still observed, suggesting little evidence that reverse causation could explain these findings.
There are several pathways by which exposure to low income may affect health outcomes, including cognitive aging. First, exposure to low income and socioeconomic conditions has been associated with unhealthy behaviors30–32 such as alcohol use, smoking, and inadequate physical activity, which are in turn risk factors for small brain infarcts and poor cognition. Second, exposure to low income may influence educational attainment and ultimately shape many of the risk factors of cognition, including adult living environment (inadequate housing and sanitation), health behaviors, and access to resources. Furthermore, education may itself have a direct influence on cognitive function.27 In the current analyses, after adjusting for education and cumulative burden of time-varying behavioral risk factors over 25 years, the associations were only slightly attenuated. Third, the stress of exposure to low income has been shown to be associated with dysfunction of the hypothalamic–adrenocortical axis,33 which in turn is a pathway leading to worse risk factors of cognition.34 Fourth, income inequality may suggest a lack in public investment and health infrastructure, which then influence health through stress-induced mechanisms35,36 and decreased social and physical resources.37
The results from this study are consistent with prior findings primarily among older adults, showing associations between both childhood and adulthood socioeconomic conditions and late-life cognitive function. For example, Luo et al.5 showed that both childhood and adulthood SES was associated with cognition in those aged ≥50 years. In a cohort of older adults of Mexican descent, life course SES was associated with incidence of dementia and cognitive impairment11 and cumulative disadvantage was associated with greater cognitive deficits.2 Similarly, data from the Women’s Health Study showed that SES as measured through education and household income was inversely associated with cognitive impairment.12 Perhaps most striking about the current results are the strong graded associations between economic parameters and cognition seen in this relatively younger cohort (e.g., 10 points and 6 points less on processing speed test scores). These graded associations were more evident with processing speed than verbal memory or executive function. Furthermore, the strength of the associations, which persist beyond traditional risk factors and even education, a strong determinant of cognitive functioning,38 and parental education, a marker of childhood socioeconomic environment, is particularly notable considering mean age at cognitive assessment was around 50 years. If this level of cognitive deterioration is a pathway to further and greater cognitive impairment as one ages (with or without functional impairment), then these findings place economic hardship as being on the pathway to cognitive aging.
The current study built upon previous literature by utilizing recent income data and, more importantly, a younger cohort. The timeframe of the study encompassed both periods of economic acceleration and recession.39,40 With a clear decline in average income occurring post-2000, the income trajectory of the CARDIA study population, an ongoing prospective epidemiologic cohort in the U.S., reflects the current economic climate and provides a unique opportunity to reflect upon how such economic instability influences health.
Limitations
In this study, cognitive testing was not available at baseline. However, the authors still addressed reverse causation by first restricting the sample to participants with healthy cardiovascular risk profile at baseline, and second by restricting the sample to participants with high education at baseline. Although the findings suggested that the possibility of reverse causation is less likely, it important to note that reverse causation cannot be completely ruled out given the data in hand. The findings are likely a mix of the effects of economic hardship on cognition and that of reverse causation (i.e., cognition influencing trajectories of economic hardship). Furthermore, though most participants completed their education by the time income was first assessed in 1990 (mean age, 30.2 years), education and income are inter-related and thus it may not be possible to fully disentangle their effects on adult cognitive function. In addition, to be included in this analysis, participants had to survive and participate in the Year 25 examination during which the cognitive battery was administered. However, such attrition is likely to have biased the results toward the null. Finally, there may be residual confounding due to factors that are associated with both race and gender and that were not captured and adjusted for in this analysis.
Despite these limitations, this study’s strengths contribute to the existing literature in several ways. First, very few epidemiologic analyses examined the deleterious effects of low income on health and, more importantly, the present findings rely on repeated measurements of income going from young adulthood into midlife. Second, the consistency of findings across two related but separate measures of financial standing is very encouraging: Poverty defined by income (albeit reported) and the FPL thresholds is objective, whereas reported financial difficulty captures perception. Third, it is becoming increasingly clear that maintaining cognitive health is a lifelong process with a long preclinical period41,42; therefore, examining this association in a relatively young cohort will have important clinical implications. Finally, the strong and graded associations were independent of important risk factors of cognition, including education, parent’s education, and time-varying behavioral and cardiovascular risk factors, and these graded associations were robust to several sensitivity analyses.
Conclusions
In summary, findings from this study support strong and graded associations between sustained exposure to economic hardship and worse cognitive function in a relatively young cohort. These findings place economic hardship as being on the pathway to cognitive aging and as an important contributor to premature aging among economically disadvantaged individuals. It is important to monitor how trends in income and other social and economic parameters influence health outcomes.
Supplementary Material
Acknowledgments
The contents and views in this manuscript are those of the authors and should not be construed to represent the views of NIH or any of the sponsoring organizations and agencies of the U.S. government.
Dr. Zeki Al Hazzouri was supported by a grant from NIH, National Institute on Aging (NIA) (K01AG047273). Dr. Yaffe was supported by a grant from the NIH/NIA (k24AG031155). Tali Elfassy was supported by a T32 training grant from NIH, National Heart, Lung, and Blood Institute (NHLBI), “Behavioral Medicine Approaches to Cardiovascular Disease,” (HL 007426). Funding for this study was supported in part by the University of California at San Francisco Center for Aging in Diverse Communities (P30-AG15272) under the “Resource Centers for Minority Aging Research program of the National Institute on Aging.” The Coronary Artery Risk Development in Young Adults Study is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from NHLBI, the Intramural Research Program of NIA, and an intra-agency agreement between NIA and NHLBI (AG0005).
The sponsors had no role in the study design; collection, analysis, and interpretation of the data; writing the report; or the decision to submit the report for publication.
Dr. Zeki had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
No financial disclosures were reported by authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Watson T. Inequality and the measurement of residential segregation by income in American neighborhoods. Rev Income Wealth. 2009;55(3):820–844. http://dx.doi.org/10.1111/j.1475-4991.2009.00346.x. [Google Scholar]
- 2.Haan MN, Zeki Al-Hazzouri A, Aiello AE. Life-span socioeconomic trajectory, nativity, and cognitive aging in Mexican Americans: the Sacramento Area Latino Study on Aging. J Gerontol B Psychol Sci Soc Sci. 2011;66(Suppl 1):i102–10. doi: 10.1093/geronb/gbq071. http://dx.doi.org/10.1093/geronb/gbq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaplan GA, Turrell G, Lynch JW, Everson SA, Helkala EL, Salonen JT. Childhood socioeconomic position and cognitive function in adulthood. Int J Epidemiol. 2001;30(2):256–263. doi: 10.1093/ije/30.2.256. http://dx.doi.org/10.1093/ije/30.2.256. [DOI] [PubMed] [Google Scholar]
- 4.Karlamangla AS, Miller-Martinez D, Aneshensel CS, Seeman TE, Wight RG, Chodosh J. Trajectories of cognitive function in late life in the United States: demographic and socioeconomic predictors. Am J Epidemiol. 2009;170(3):331–342. doi: 10.1093/aje/kwp154. http://dx.doi.org/10.1093/aje/kwp154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):S93–S101. doi: 10.1093/geronb/60.2.s93. http://dx.doi.org/10.1093/geronb/60.2.S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med. 1997;337(26):1889–1895. doi: 10.1056/NEJM199712253372606. http://dx.doi.org/10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- 7.Moceri VM, Kukull WA, Emanual I, et al. Using census data and birth certificates to reconstruct the early-life socioeconomic environment and the relation to the development of Alzheimer’s disease. Epidemiology. 2001;12(4):383–389. doi: 10.1097/00001648-200107000-00007. http://dx.doi.org/10.1097/00001648-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Osler M, Avlund K, Mortensen EL. Socio-economic position early in life, cognitive development and cognitive change from young adulthood to middle age. Eur J Public Health. 2013;23(6):974–980. doi: 10.1093/eurpub/cks140. http://dx.doi.org/10.1093/eurpub/cks140. [DOI] [PubMed] [Google Scholar]
- 9.Schoon I, Jones E, Cheng H, Maughan B. Family hardship, family instability, and cognitive development. J Epidemiol Community Health. 2012;66(8):716–722. doi: 10.1136/jech.2010.121228. http://dx.doi.org/10.1136/jech.2010.121228. [DOI] [PubMed] [Google Scholar]
- 10.Turrell G, Lynch JW, Kaplan GA, et al. Socioeconomic position across the lifecourse and cognitive function in late middle age. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):S43–51. doi: 10.1093/geronb/57.1.s43. http://dx.doi.org/10.1093/geronb/57.1.S43. [DOI] [PubMed] [Google Scholar]
- 11.Zeki Al Hazzouri A, Haan MN, Kalbfleisch JD, Galea S, Lisabeth LD, Aiello AE. Life-course socioeconomic position and incidence of dementia and cognitive impairment without dementia in older Mexican Americans: results from the Sacramento area Latino study on aging. Am J Epidemiol. 2011;173(10):1148–1158. doi: 10.1093/aje/kwq483. http://dx.doi.org/10.1093/aje/kwq483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S, Buring JE, Cook NR, Grodstein F. The relation of education and income to cognitive function among professional women. Neuroepidemiology. 2006;26(2):93–101. doi: 10.1159/000090254. http://dx.doi.org/10.1159/000090254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duncan GJ. Income dynamics and health. Int J Health Serv. 1996;26(3):419–444. doi: 10.2190/1KU0-4Y3K-ACFL-BYU7. http://dx.doi.org/10.2190/1KU0-4Y3K-ACFL-BYU7. [DOI] [PubMed] [Google Scholar]
- 14.Dynana KEED, Sichel DE. Affairs DoRSaM, editor. The Evolution of Household Income Volatility. Washington, D.C: Federal Reserve Board; 2007. [Google Scholar]
- 15.Dynana KE, Sichel DE. The Evolution of Household Income Volatility. Federal Reserve Board; Washington, D.C: 2007. [Google Scholar]
- 16.Matthews KA, Kiefe CI, Lewis CE, et al. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension. 2002;39(3):772–776. doi: 10.1161/hy0302.105682. http://dx.doi.org/10.1161/hy0302.105682. [DOI] [PubMed] [Google Scholar]
- 17.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. http://dx.doi.org/10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 18.Kaiser Family Foundation. http://kff.org/other/state-indicator/population-up-to-200-fpl/
- 19.U.S. Census Bureau. Poverty thresholds. 2015 Jun 1; www.census.gov/hhes/www/poverty/data/threshld/
- 20.Rosenberg SJ, Ryan JJ, Prifitera A. Rey Auditory-Verbal Learning Test performance of patients with and without memory impairment. J Clin Psychol. 1984;40(3):785–787. doi: 10.1002/1097-4679(198405)40:3<785::aid-jclp2270400325>3.0.co;2-4. http://dx.doi.org/10.1002/1097-4679(198405)40:3<785::AID-JCLP2270400325>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 21.Wechsler D. Wechsler Adult Intelligence Scale-III (WAIS-III) San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- 22.MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull. 1991;109:163–203. doi: 10.1037/0033-2909.109.2.163. http://dx.doi.org/10.1037/0033-2909.109.2.163. [DOI] [PubMed] [Google Scholar]
- 23.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- 24.Yaffe K, Vittinghoff E, Pletcher MJ, et al. Early adult to midlife cardiovascular risk factors and cognitive function. Circulation. 2014;129(15):1560–1567. doi: 10.1161/CIRCULATIONAHA.113.004798. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CPI Inflation Calculator, Bureau of Labor Statistics. U.S. Department of Labor; Jun 1, 2015. www.bls.gov/data/inflation_calculator.htm. [Google Scholar]
- 26.Beeri MS, Ravona-Springer R, Silverman JM, Haroutunian V. The effects of cardiovascular risk factors on cognitive compromise. Dialogues Clin Neurosci. 2009;11(2):201–212. doi: 10.31887/DCNS.2009.11.2/msbeeri. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wight RG, Aneshensel CS, Seeman TE. Educational attainment, continued learning experience, and cognitive function among older men. J Aging Health. 2002;14(2):211–236. doi: 10.1177/089826430201400203. http://dx.doi.org/10.1177/089826430201400203. [DOI] [PubMed] [Google Scholar]
- 28.Rapp SR, Espeland MA, Manson JE, et al. Educational attainment, MRI changes, and cognitive function in older postmenopausal women from the Women’s Health Initiative Memory Study. Int J Psychiatry Med. 2013;46(2):121–143. doi: 10.2190/PM.46.2.a. http://dx.doi.org/10.2190/PM.46.2.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barrera M, Jr, Caples H, Tein JY. The psychological sense of economic hardship: measurement models, validity, and cross-ethnic equivalence for urban families. Am J Community Psychol. 2001;29(3):493–517. doi: 10.1023/a:1010328115110. http://dx.doi.org/10.1023/A:1010328115110. [DOI] [PubMed] [Google Scholar]
- 30.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44(6):809–819. doi: 10.1016/s0277-9536(96)00191-8. http://dx.doi.org/10.1016/S0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 31.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34(1):16–22. doi: 10.1016/j.amepre.2007.09.021. http://dx.doi.org/10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT, Kaplan GA. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. Am J Epidemiol. 2007;165(2):184–193. doi: 10.1093/aje/kwj357. http://dx.doi.org/10.1093/aje/kwj357. [DOI] [PubMed] [Google Scholar]
- 33.Brunner E. Stress and the biology of inequality. BMJ. 1997;314(7092):1472–1476. doi: 10.1136/bmj.314.7092.1472. http://dx.doi.org/10.1136/bmj.314.7092.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brindley DN. Neuroendocrine regulation and obesity. Int J Obes Relat Metab Disord. 1992;16(Suppl 3):S73–79. [PubMed] [Google Scholar]
- 35.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34(1 Pt 2):215–227. [PMC free article] [PubMed] [Google Scholar]
- 36.Lynch J, Smith GD, Harper S, et al. Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q. 2004;82(1):5–99. doi: 10.1111/j.0887-378X.2004.00302.x. http://dx.doi.org/10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychol. 2001;20(4):243–255. doi: 10.1037//0278-6133.20.4.243. http://dx.doi.org/10.1037/0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- 38.Lee S, Kawachi I, Berkman LF, Grodstein F. Education, other socioeconomic indicators, and cognitive function. Am J Epidemiol. 2003;157(8):712–720. doi: 10.1093/aje/kwg042. http://dx.doi.org/10.1093/aje/kwg042. [DOI] [PubMed] [Google Scholar]
- 39.Hamoudi A, Dowd JB. Housing wealth, psychological well-being, and cognitive functioning of older Americans. J Gerontol B Psychol Sci Soc Sci. 2014;69(2):253–262. doi: 10.1093/geronb/gbt114. http://dx.doi.org/10.1093/geronb/gbt114. [DOI] [PubMed] [Google Scholar]
- 40.Mehta K, Kramer H, Durazo-Arvizu R, Cao G, Tong L, Rao M. Depression in the U.S. population during the time periods surrounding the great recession. J Clin Psychiatry. 2015;76(4):e499–504. doi: 10.4088/JCP.14m09637. http://dx.doi.org/10.4088/JCP.14m09637. [DOI] [PubMed] [Google Scholar]
- 41.Launer LJ. The epidemiologic study of dementia: a life-long quest? Neurobiol Aging. 2005;26(3):335–340. doi: 10.1016/j.neurobiolaging.2004.03.016. http://dx.doi.org/10.1016/j.neurobiolaging.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 42.Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005;4(8):487–499. doi: 10.1016/S1474-4422(05)70141-1. http://dx.doi.org/10.1016/S1474-4422(05)70141-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.