Abstract
Background
There were a limited number of studies about β-cell function after insulin initiation in patients exposed to long durations of sulfonylurea treatment. In this study, we aimed to evaluate the recovery of β-cell function and the efficacy of concurrent sulfonylurea use after the start of long-acting insulin.
Methods
In this randomized controlled study, patients with type 2 diabetes mellitus (T2DM), receiving sulfonylurea for at least 2 years with glycosylated hemoglobin (HbA1c) >7%, were randomly assigned to two groups: sulfonylurea maintenance (SM) and sulfonylurea reduction (SR). Following a 75-g oral glucose tolerance test (OGTT), we administered long-acting basal insulin to the two groups. After a 6-month follow-up, we repeated the OGTT.
Results
Among 69 enrolled patients, 57 completed the study and were analyzed: 31 in the SM and 26 in the SR group. At baseline, there was no significant difference except for the longer duration of diabetes and lower triglycerides in the SR group. After 6 months, the HbA1c was similarly reduced in both groups, but there was little difference in the insulin dose. In addition, insulin secretion during OGTT was significantly increased by 20% to 30% in both groups. A significant weight gain was observed in the SM group only. The insulinogenic index was more significantly improved in the SR group.
Conclusion
Long-acting basal insulin replacement could improve the glycemic status and restore β-cell function in the T2DM patients undergoing sulfonylurea-based treatment, irrespective of the sulfonylurea dose reduction. The dose reduction of the concurrent sulfonylurea might be beneficial with regard to weight grain.
Keywords: Basal insulin; Beta-cell; Diabetes mellitus, type 2; Recovery; Sulfonylurea
INTRODUCTION
Insulin resistance and defective β-cell function are well-known pathophysiological mechanisms for the development of type 2 diabetes mellitus (T2DM) [1]. β-Cell dysfunction comprises both secretory dysfunction and decreased mass. Studies have reported that, rather than insulin resistance, defective β-cell function is an important factor in Asian people, including Koreans [2,3,4].
As one of the oldest hypoglycemic agents, sulfonylurea stimulates pancreatic β-cells to release insulin in a rather glucose-independent manner. With the introduction of new oral hypoglycemic agents, the use of sulfonylurea has rapidly declined. Nevertheless, this drug remains one of the most commonly prescribed second-line oral agents in combination with metformin [5], and an option when the combination of basal insulin and oral hypoglycemia agent is considered [6,7,8].
Although the efficacy of sulfonylurea is strong, Kahn et al. [9] showed that the glycemic durability of sulfonylureas was not persistent for long periods. In addition, sulfonylurea showed a higher secondary therapeutic failure rate and more rapid loss of β-cell function compared with metformin and rosiglitazone. There are several hypotheses concerning the mechanisms of sulfonylurea-induced β-cell dysfunction. For example, accelerated β-cell apoptosis resulting from endoplasmic reticulum stress, decreased functional expression of adenosine triphosphate sensitive K+ channels, and reduced insulin content could induce secondary β-cell failure [10,11,12]. Therefore, the long-term use of sulfonylurea in Korean people with T2DM could induce early β-cell failure and further aggravate diabetes.
The protection of β-cell function through appropriate insulin replacement is a generally accepted treatment guideline in patients with T2DM [13,14,15,16,17,18]. Evidence is well-established of the beneficial effect of insulin on β-cell function and glycemic control compared with the sulfonylurea in patients recently diagnosed with T2DM [16,17,19]. However, there is a limited number of studies about β-cell recovery after insulin therapy in patients already exposed to long durations of sulfonylurea treatment or who showed a secondary failure of sulfonylurea [20,21,22]. Karam et al. [23] reported unresponsiveness of β-cells to acute sulfonylurea stimulation during long sulfonylurea treatment in diabetic patients. Once sustained therapy with sulfonylurea was discontinued, β-cell response to acute sulfonylurea stimulation was restored. Based on such a background, we hypothesized that basal insulin replacement relieves loading on β-cells for insulin secretion and reduces β-cell stress in subjects with T2DM based on previous long-term sulfonylurea treatment, and this relief could improve β-cell function. Moreover, additional effects could occur with sulfonylurea dose reduction.
The aim of the present study was to research the recovery of β-cell function through long-acting basal insulin replacement in patients with inadequately controlled T2DM, receiving long-term sulfonylurea-based treatment. In addition, we evaluated the efficacy of concurrent sulfonylurea with the start of basal insulin by comparing the sulfonylurea maintenance (SM) and sulfonylurea reduction (SR) groups.
METHODS
Subjects
In the present study, we enrolled subjects who visited the diabetes center of St. Vincent's Hospital. Eligible patients had T2DM with inadequate glycemic control (glycosylated hemoglobin [HbA1c] >7%). The patients were over 35 years old and had been treated with a stable dose of sulfonylurea for at least 2 years, with or without metformin. Patients taking α-glucosidase inhibitors, thiazolidinediones, and other oral hypoglycemic agents rather than sulfonylurea and metformin were excluded. Other exclusion criteria consisted of renal impairment (serum creatinine >133 µmol/L), hepatic dysfunction (aspartate aminotransaminase [AST] and alanine aminotransaminase [ALT] >3 times the upper normal level), major severe diabetic complications, severe medical illnesses, and previous insulin treatment. Informed consent was obtained from all participants, and this study was approved through the International Review Board of St. Vincent's Hospital (VIRB-00034-002).
Study design
At enrollment, we performed basic anthropometric measurements and baseline laboratory tests, including HbA1c, lipid profiles (total cholesterol, triglyceride, high density lipoprotein and low density lipoprotein cholesterol), blood urea nitrogen, creatinine, AST, and ALT. To examine β-cell function, we performed a 75-g oral glucose tolerance test (OGTT) and measured plasma glucose and insulin at 0, 30, 60, 90, and 120 minutes after glucose loading. The HbA1c was measured using high-performance liquid chromatography instruments (BIO-RAD Variant II; Bio-Rad, Hercules, CA, USA). Plasma glucose levels were assayed using the glucose oxidase method. Plasma insulin values were tested using a chemiluminescent immunoassay (IMMULITE; Siemens, Berlin and Munich, Germany).
After the baseline study, the patients were randomly assigned in a 1:1 ratio to two groups: SM and SR groups. While maintaining antidiabetic medications, all participants in both groups were treated with long-acting insulin (insulin glargine) immediately after randomization. The initial doses were 0.1 to 0.2 unit/kg/day, and the patients self-adjusted the insulin dose according to self-monitoring blood glucose (SMBG) levels until fasting blood glucose levels were less than 6.7 mmol/L (120 mg/dL). When hypoglycemia was experienced, the insulin doses were reduced two units. The subjects visited the diabetes center at 1, 3, and 6 months after insulin administration was initiated, and we appropriately modified the insulin doses. At every visit, the body weight was assessed. For the SR group, we reduced the amounts of sulfonylurea more than 50% when the fasting SMBG level was less than 6.7 mmol/L at the 1- or 3-month visit. We did not change the metformin dose during the study period. At the 3-month visit, we followed up the HbA1c level. At the 6-month visit, we repeated the baseline laboratory studies, including the 75-g OGTT. Insulin treatment was discontinued for 48 hours prior to the OGTT at the 6-month visit.
We calculated several indices to evaluate insulin secretion and resistance. The insulinogenic index was defined as the ratio of the 30-minute increment in insulin concentration (pmol/L) to the 30-minute increment in glucose concentration (mmol/L) following oral glucose loading [24]. The homeostatic model assessment of insulin resistance (HOMA-IR) was calculated based on the index from the product of the fasting plasma insulin (µU/mL) and plasma glucose (mmol/L) divided by 22.5 [25]. In accordance with Matsuda and DeFronzo [26], the insulin sensitivity index (ISI) was calculated using the following equation: ISI composite=10,000/square root of [(mean plasma insulin [µU/mL]×mean plasma glucose [mg/dL] during OGTT)×(fasting plasma glucose×fasting plasma insulin)]. The area under the curve (AUC) was calculated using trapezoidal integration.
Sample size
We expected more increments of insulin secretion after glucose loading in the SR group (25%) compared with the SM group (5%) [21]. Therefore, the calculation of the sample size was based on an expected difference of 20% in the increment of insulin secretion after glucose loading with α of 0.05 and β of 0.20. By multiplication of the assumed withdrawal rate of 10%, a sample size of 55 in each group was obtained.
Statistical analysis
The baseline characteristics of the subjects enrolled in the present study are expressed as the mean±standard deviation or number (%). The data for the results are expressed as the mean±standard error. A chi-square analysis was used for discontinuous variables. The distinction between the two study groups was analyzed using an independent t-test. In the same group, differences between pretreatment and posttreatment of basal insulin were examined using a paired t-test. Repeated measurements of analysis of variance were used to compare the change of the β-cell function between the two groups. All data were analyzed using PASW statistics version 18.0 (SPSS Inc., Chicago, IL, USA). Statistically significant differences were considered at a P<0.05.
RESULTS
Characteristics of the subjects
A total of 69 patients underwent randomization. Among these patients, 35 subjects were assigned to the SM group, and 34 subjects were assigned to the SR group. After 6 months, four patients from the SM group and eight patients from the SR group were excluded due to the refusal of OGTT or the follow-up loss. Thus, a total of 31 patients in the SM group and 26 patients in the SR group were analyzed in the present study.
The clinical characteristics and biochemical parameters of the patients in both groups are shown in Table 1. The mean age was 54.6±11.1 years, and the mean duration of diabetes was 9.3±5.7 years. There was no significant difference in age, sex, body mass index, and blood pressure between the two groups. However, the mean duration of diabetes in the SR group was significantly higher than that in the SM group. The baseline laboratory evaluations showed no statistical differences between the two groups, except the triglyceride level.
Table 1. Baseline characteristics of the subjects.
| Characteristic | Total (n=57) | Sulfonylurea-maintenance (n=31) | Sulfonylurea-reduction (n=26) | P value |
|---|---|---|---|---|
| Age, yr | 54.6±11.1 | 52.9±11.5 | 54.5±10.8 | 0.577 |
| Male sex | 33 (57.9) | 18 (58.1) | 15 (57.7) | 0.977 |
| Weight, kg | 66.7±11.3 | 68.1±11.2 | 65.0±11.5 | 0.313 |
| BMI, kg/m2a | 24.9±3.4 | 25.5±3.6 | 24.3±3.0 | 0.187 |
| Duration of diabetes, yr | 9.3±5.7 | 7.2±4.7 | 11.9±5.8 | 0.002 |
| SBP, mm Hg | 131.9±14.8 | 133.7±13.2 | 129.9±16.5 | 0.338 |
| DBP, mm Hg | 74.7±9.7 | 76.7±9.2 | 72.2±9.8 | 0.082 |
| HbA1c, % | 9.2±1.2 | 9.3±1.2 | 9.0±1.2 | 0.361 |
| Total cholesterol, mmol/L | 4.7±0.9 | 4.9±0.9 | 4.5±0.9 | 0.114 |
| Triglyceride, mmol/L | 1.8±1.2 | 2.2±1.4 | 1.4±0.7 | 0.007 |
| HDL-C, mmol/L | 1.1±0.2 | 1.1±0.2 | 1.1±0.2 | 0.227 |
| LDL-C, mmol/L | 2.9±0.8 | 2.9±0.9 | 2.8±0.7 | 0.538 |
| Insulin at 0 min, pmol/Lb | 45.9±29.8 | 51.2±31.9 | 39.6±26.4 | 0.149 |
| Insulin at 120 min, pmol/Lb | 132.5±83.3 | 131.2±92.4 | 134.1±72.7 | 0.898 |
| Insulinogenic index | 5.0±5.0 | 4.5±4.2 | 5.5±6.0 | 0.461 |
| HOMA-IR | 3.0±2.2 | 3.4±2.1 | 2.5±2.3 | 0.128 |
| ISI composite (Matsuda index) | 7.5±7.1 | 7.2±7.7 | 7.8±6.5 | 0.754 |
| Metformin dose, mg | 1,021.7±632.7 | 854.8±580.1 | 1,115.4±652.8 | 0.116 |
| Types of sulfonylurea | 0.536 | |||
| Glimepiride | 39 (70.2) | 23 (74.2) | 17 (65.4) | |
| Dose, mg | 3.7±1.4 | 3.5±1.3 | 4.1±1.3 | |
| Gliclazide | 4 (7.0) | 1 (3.2) | 3 (11.5) | |
| Dose, mg | 140±40.0 | 0080 | 160±0.0 | |
| Gliclazide MR | 5 (8.8) | 2 (6.5) | 3 (11.5) | |
| Dose, mg | 60.0±21.2 | 45±21.2 | 70±17.3 | |
| Glibenclamide | 8 (14.0) | 5 (16.1) | 3 (11.5) | |
| Dose, mg | 9.8±4.2 | 9.8±3.9 | 9.7±5.5 |
Values are presented as mean±standard deviation or number (%).
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HbA1c, glycosylated hemoglobin; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; HOMA-IR, homeostatic model assessment of insulin resistance; ISI, insulin sensitivity index; OHA, oral hypoglycemic agents; MR, modified release.
aThe BMI was calculated as the weight in kilograms divided by the square of the height in meters, bInsulin level during the 75-g oral glucose tolerance test.
The most commonly used sulfonylurea in all participants was glimepiride. The average dose of glimepiride was 3.5±1.3 mg in the SM group and 4.1±1.3 mg in the SR group. Other sulfonylureas used were gliclazide, gliclazide MR, and glibenclamide.
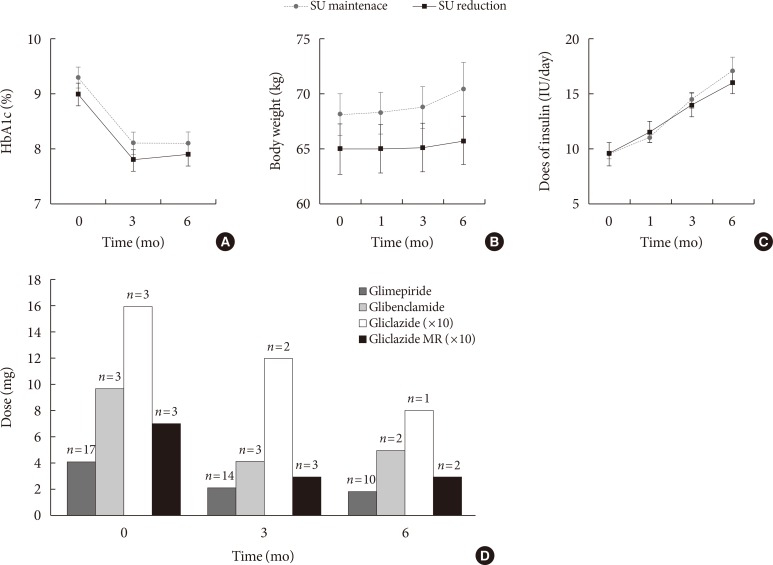
Changes in the glucose level and body weight
In both study groups, the HbA1c level was significantly decreased at the first follow-up at 3 months after initiating long-acting insulin treatment. However, the HbA1c values were only slightly changed during the last 3 months of the study period (Fig. 1A). The initial HbA1c values of 9.3%±0.2% in the SM group and 9.0%±0.2% in the SR group decreased to 8.1%±0.2% (P<0.001) and 7.9%±0.2% (P=0.003) at the 6-month follow-up, respectively. Fig. 1B shows the changes in body weight during the follow-up period. At the 6-month follow-up, the average body weight significantly increased from 68.1±1.9 to 70.4±2.5 kg in the SM group (P=0.003) but showed no difference from 65.0±2.3 to 65.7±2.2 kg in the SR group (P=0.074). The average weight gain in the SM group was significantly higher than that in the SR group. Fig. 1C shows the daily dosage of insulin administered to the subjects. During the study period, the insulin dose was increased from 9.4±0.3 to 17.1±1.2 IU/day in the SM group and from 9.5±0.5 to 16.0±1.3 IU/day in the SR group, and there was no significant difference in the insulin dose between the two groups (P=0.550). At the end of the investigation, 11 patients (42.3%) discontinued sulfonylurea treatment in the SR group, and the drug dosage was reduced more than 50% in the remaining 15 patients (57.7%) (Fig. 1D).
Fig. 1. Changes in the glucose levels, body weight, and insulin and sulfonylurea (SU) doses over 6 months. Changes in the (A) glycosylated hemoglobin (HbA1c) levels, (B) body weight, and (C) injected insulin dose in the SU maintenance and SU reduction groups during the study period. (D) Dose reduction of SU in the SU reduction group. The data are presented as the mean±standard error.
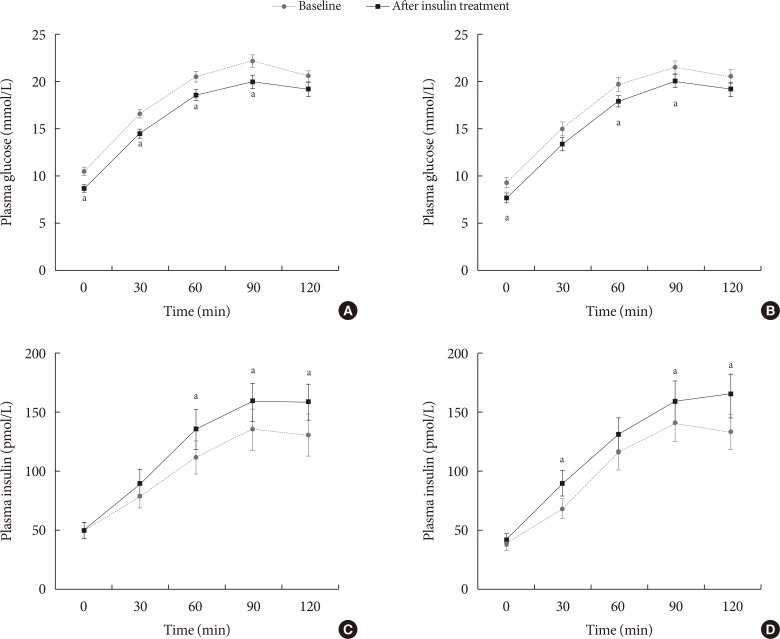
Change in β-cell function and insulin resistance
The levels of glucose and insulin after 75-g glucose loading at baseline and the 6-month follow-up are illustrated in Fig. 2. Compared with the levels prior to insulin treatment, plasma glucose at OGTT was significantly decreased, and plasma insulin was significantly increased 20% to 30% after the administration of insulin in both groups.
Fig. 2. Changes in β-cell function and insulin resistance. Results of the 75-g oral glucose tolerance test. (A) The plasma glucose levels in the sulfonylurea (SU) maintenance and (B) SU reduction groups. (C) The plasma insulin levels in the SU maintenance and (D) SU reduction groups. The data are presented as the mean±standard error. aP<0.05 before and after insulin treatment.
Table 2 reveals the changes in the biochemical measures of the study groups. Almost all parameters representing β-cell function in the OGTT were improved after 6 months of insulin therapy in both groups. The AUC insulin/glucose ratio was significantly increased in both groups, and the insulinogenic index, reflecting first-phase insulin secretion, also markedly increased in both groups. Although the sulfonylurea dose was reduced in the SR group, the insulinogenic index was more significantly improved in the SR group. The HOMA-IR and ISI, representing insulin resistance, showed no significant changes from baseline to the end of the follow-up period in the two study groups.
Table 2. Changes in β-cell function and insulin resistance.
| Parameter | Sulfonylurea-maintenance (n=31) | Sulfonylurea-reduction (n=26) | Between-group P value | ||||
|---|---|---|---|---|---|---|---|
| Baseline | 6 Months | P value | Baseline | 6 Months | P value | ||
| AUCg, mmol/L·hr | 37.0±0.8 | 32.4±1.5 | 0.002 | 35.6±1.2 | 32.5±1.0 | 0.069 | 0.143 |
| AUCi, pmol/L·hr | 209.0±25.1 | 245.2±23.9 | 0.022 | 177.8±22.2 | 241.7±25.1 | 0.016 | 0.178 |
| AUCi/AUCg | 5.6±0.7 | 7.4±0.8 | 0.003 | 5.9±0.6 | 7.5±0.8 | 0.009 | 0.404 |
| HOMA-IR | 3.4±0.4 | 2.9±0.4 | 0.068 | 2.3±0.4 | 2.1±0.4 | 0.428 | 0.275 |
| Insulinogenic index | 4.6±0.8 | 6.9±1.2 | 0.031 | 5.7±1.2 | 16.3±6.4 | 0.045 | <0.001 |
| ISI composite (Matsuda index) | 7.4±1.5 | 7.7±1.5 | 0.714 | 8.0±1.3 | 8.3±1.3 | 0.812 | 0.696 |
Values are presented as mean±standard error.
AUCg, area under the response curve of glucose; AUCi, area under the response curve of insulin; HOMA-IR, homeostatic model assessment of insulin resistance; ISI, insulin sensitivity index.
Hypoglycemia
The number of symptomatic hypoglycemia events during the treatment was similar between the two groups (SM group, 9.7%; SR group, 11.5%); no event of severe hypoglycemia occurred.
DISCUSSION
In the present study, we demonstrated that basal insulin replacement in patients undergoing long-term sulfonylurea-based treatment improved not only glycemic control status but also β-cell function, irrespective of the sulfonylurea dose reduction.
Although the use of sulfonylureas has rapidly decreased, this drug remains the preferred oral agent when patients show relatively high glucose levels or refuse insulin therapy. These agents will likely initially improve the hyperglycemic state. However, hyperglycemia could paradoxically worsen with time because these drugs could induce the exhaustion of pancreatic β-cells, particularly in subjects with predominant β-cell dysfunction [9].
Thus, we evaluated the recovery of insulin secretory function particularly in patients receiving long durations of sulfonylurea-based treatments. We thought that a reduction of the sulfonylurea dose would increase the insulin requirement compared with SM. Interestingly, the decrement in HbA1c was similar between these two conditions, and there was no difference in insulin requirement, despite a reduction in the sulfonylurea dose or even the termination of sulfonylurea treatment.
Prior studies have reported beneficial effects of basal insulin on insulin secretion by glucagon stimulation, compared with the sulfonylurea in patients with recently diagnosed T2DM [16,17,19]. In our study, there was little difference in the insulin secretion after glucose loading in both groups, irrespective of the sulfonylurea dose reduction. These findings indirectly suggested that there might be relatively similar self-reliant insulin secretion between SM and SR. Patients presenting with significant hyperglycemia could benefit from the initiation of insulin treatment, which restores the deleterious effects of excessive glucose (glucotoxicity) and lipid (lipotoxicity) exposure on β-cell function and insulin action [27,28,29]. In the present study, we considered an added effect of improved glucose toxicity, resulting in more improvements in insulin secretion after glucose loading. However, the insulinogenic index, a marker for β-cell function, was more significantly improved in SR group. This result has a thread of connection with results in Karam's study [23]. As mentioned in introduction, Karam et al. [23] reported recovery of β-cell response to acute sulfonylurea stimulation when sustained therapy with sulfonylurea was discontinued.
In addition, patients' body weight significantly increased in the SM group at 6 months after basal insulin replacement, whereas there was no change in body weight in the SR group. Thus, we concluded that when basal insulin was replaced, an additional effect of sulfonylurea was not observed; therefore, sulfonylurea could be reduced or discontinued without an increase in the basal insulin dose.
Previous studies have revealed that early insulinization could more effectively achieve adequate glycemic target levels and improve β-cell function compared with the use of oral hypoglycemic agents in newly diagnosed patients or subjects with short disease durations [14,16,17]. In the present study, the patients had relatively longer average diabetes durations, and the glucose control status was poorer than in previously reported studies. Although the HbA1c levels were decreased and the insulin secretory function was slightly recovered in the present study, we expect that if the diabetes duration had been shorter, the results would have been better.
We did not observe any improvements in HbA1c after the 3- and 6-month follow-ups, likely reflecting the fact that the glucose increment levels after OGTT did not sufficiently decrease to target levels, despite adequate control of fasting blood glucose levels. This finding suggests that another approach, such as glucagon-like peptide-1 agonists or rapid-acting insulin, is needed for postprandial glucose control in combination with basal insulin replacement, although basal insulin replacement could normalize fasting blood glucose levels and slightly restore postprandial insulin secretion in patients undergoing sulfonylurea-based treatment.
There are several limitations in the present study. First, the sample size was small. We were unable to fulfill the planned 110 patients, making this study an underpowered analysis. In additionally, the follow-up duration was short. To evaluate sulfonylurea durability and the long-term effect of β-cell dysfunction recovery, longer studies are needed. Moreover, diet and exercise were not monitored during the 6-month treatment period. However, the present study was a prospective, randomized, controlled study that evaluated the efficacy of SR with basal insulin replacement in patients receiving sulfonylurea-based treatment over 2 years.
In conclusion, basal insulin replacement in Korean patients with T2DM receiving long durations of sulfonylurea-based treatment is beneficial to restore β-cell function. Indeed, when basal insulin is replaced, sulfonylurea-based treatment can be reduced or even discontinued without affecting glycemic control status and insulin requirements. Moreover, the dose reduction of the concurrent sulfonylurea might be beneficial with regard to weight gain. Further studies are needed to target a large number of subjects over a longer period.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.DeFronzo RA. Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver. A collusion responsible for NIDDM. Diabetes. 1988;37:667–687. doi: 10.2337/diab.37.6.667. [DOI] [PubMed] [Google Scholar]
- 2.Kim DJ, Lee MS, Kim KW, Lee MK. Insulin secretory dysfunction and insulin resistance in the pathogenesis of Korean type 2 diabetes mellitus. Metabolism. 2001;50:590–593. doi: 10.1053/meta.2001.22558. [DOI] [PubMed] [Google Scholar]
- 3.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 4.Yoon KH, Ko SH, Cho JH, Lee JM, Ahn YB, Song KH, Yoo SJ, Kang MI, Cha BY, Lee KW, Son HY, Kang SK, Kim HS, Lee IK, Bonner-Weir S. Selective beta-cell loss and alpha-cell expansion in patients with type 2 diabetes mellitus in Korea. J Clin Endocrinol Metab. 2003;88:2300–2308. doi: 10.1210/jc.2002-020735. [DOI] [PubMed] [Google Scholar]
- 5.Turner LW, Nartey D, Stafford RS, Singh S, Alexander GC. Ambulatory treatment of type 2 diabetes in the U.S., 1997-2012. Diabetes Care. 2014;37:985–992. doi: 10.2337/dc13-2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeon JY, Kim DJ, Ko SH, Kwon HS, Lim S, Choi SH, Kim CS, An JH, Kim NH, Won JC, Kim JH, Cha BY, Song KH Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Current status of glycemic control of patients with diabetes in Korea: the fifth Korea National Health and Nutrition Examination Survey. Diabetes Metab J. 2014;38:197–203. doi: 10.4093/dmj.2014.38.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suk JH, Lee CW, Son SP, Kim MC, Ahn JH, Lee KJ, Park JY, Shin SH, Kwon MJ, Kim SS, Kim BH, Lee SH, Park JH, Kim IJ Relationship between Cardiovascular Disease and Brachial-Ankle Pulse Wave Velocity (baPWV) in Patients with Type 2 Diabetes (REBOUND) Study Group. Current status of prescription in type 2 diabetic patients from general hospitals in Busan. Diabetes Metab J. 2014;38:230–239. doi: 10.4093/dmj.2014.38.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–149. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 9.Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, Kravitz BG, Lachin JM, O'Neill MC, Zinman B, Viberti G ADOPT Study Group. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355:2427–2443. doi: 10.1056/NEJMoa066224. [DOI] [PubMed] [Google Scholar]
- 10.Qian L, Zhang S, Xu L, Peng Y. Endoplasmic reticulum stress in beta cells: latent mechanism of secondary sulfonylurea failure in type 2 diabetes? Med Hypotheses. 2008;71:889–891. doi: 10.1016/j.mehy.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 11.Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab. 2005;90:501–506. doi: 10.1210/jc.2004-0699. [DOI] [PubMed] [Google Scholar]
- 12.Takahashi A, Nagashima K, Hamasaki A, Kuwamura N, Kawasaki Y, Ikeda H, Yamada Y, Inagaki N, Seino Y. Sulfonylurea and glinide reduce insulin content, functional expression of K(ATP) channels, and accelerate apoptotic beta-cell death in the chronic phase. Diabetes Res Clin Pract. 2007;77:343–350. doi: 10.1016/j.diabres.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Bolli GB, Lucidi P, Porcellati F, Fanelli CG. Pivotal role of timely basal insulin replacement after metformin failure in sustaining long-term blood glucose control at a target in type 2 diabetes. Diabetes Care. 2011;34(Suppl 2):S220–S224. doi: 10.2337/dc11-s224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvarsson M, Berntorp K, Fernqvist-Forbes E, Lager I, Steen L, Orn T, Grill V. Effects of insulin versus sulphonylurea on beta-cell secretion in recently diagnosed type 2 diabetes patients: a 6-year follow-up study. Rev Diabet Stud. 2010;7:225–232. doi: 10.1900/RDS.2010.7.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meneghini LF. Early insulin treatment in type 2 diabetes: what are the pros? Diabetes Care. 2009;32(Suppl 2):S266–S269. doi: 10.2337/dc09-S320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D, Hu Y, Zhou Z, Yan X, Tian H, Ran X, Luo Z, Xian J, Yan L, Li F, Zeng L, Chen Y, Yang L, Yan S, Liu J, Li M, Fu Z, Cheng H. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet. 2008;371:1753–1760. doi: 10.1016/S0140-6736(08)60762-X. [DOI] [PubMed] [Google Scholar]
- 17.Chen HS, Wu TE, Jap TS, Hsiao LC, Lee SH, Lin HD. Beneficial effects of insulin on glycemic control and beta-cell function in newly diagnosed type 2 diabetes with severe hyperglycemia after short-term intensive insulin therapy. Diabetes Care. 2008;31:1927–1932. doi: 10.2337/dc08-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pfutzner A, Lorra B, Abdollahnia MR, Kann PH, Mathieu D, Pehnert C, Oligschleger C, Kaiser M, Forst T. The switch from sulfonylurea to preprandial short-acting insulin analog substitution has an immediate and comprehensive beta-cell protective effect in patients with type 2 diabetes mellitus. Diabetes Technol Ther. 2006;8:375–384. doi: 10.1089/dia.2006.8.375. [DOI] [PubMed] [Google Scholar]
- 19.Alvarsson M, Sundkvist G, Lager I, Henricsson M, Berntorp K, Fernqvist-Forbes E, Steen L, Westermark G, Westermark P, Orn T, Grill V. Beneficial effects of insulin versus sulphonylurea on insulin secretion and metabolic control in recently diagnosed type 2 diabetic patients. Diabetes Care. 2003;26:2231–2237. doi: 10.2337/diacare.26.8.2231. [DOI] [PubMed] [Google Scholar]
- 20.Castillo M, Scheen AJ, Paolisso G, Lefebvre PJ. The addition of glipizide to insulin therapy in type-II diabetic patients with secondary failure to sulfonylureas is useful only in the presence of a significant residual insulin secretion. Acta Endocrinol (Copenh) 1987;116:364–372. doi: 10.1530/acta.0.1160364. [DOI] [PubMed] [Google Scholar]
- 21.Del Prato S, Vigili de Kreutzenberg S, Riccio A, Maifreni L, Duner E, Lisato G, Iavicoli M, Tiengo A. Partial recovery of insulin secretion and action after combined insulin-sulfonylurea treatment in type 2 (non-insulin-dependent) diabetic patients with secondary failure to oral agents. Diabetologia. 1990;33:688–695. doi: 10.1007/BF00400571. [DOI] [PubMed] [Google Scholar]
- 22.Wolffenbuttel BH, Weber RF, Weeks L, van Koetsveld PM, Verschoor L. Twice daily insulin therapy in patients with type 2 diabetes and secondary failure to sulphonylureas. Diabetes Res. 1990;13:79–84. [PubMed] [Google Scholar]
- 23.Karam JH, Sanz N, Salamon E, Nolte MS. Selective unresponsiveness of pancreatic beta-cells to acute sulfonylurea stimulation during sulfonylurea therapy in NIDDM. Diabetes. 1986;35:1314–1320. doi: 10.2337/diab.35.12.1314. [DOI] [PubMed] [Google Scholar]
- 24.Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med. 1994;11:286–292. doi: 10.1111/j.1464-5491.1994.tb00273.x. [DOI] [PubMed] [Google Scholar]
- 25.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 26.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–1470. doi: 10.2337/diacare.22.9.1462. [DOI] [PubMed] [Google Scholar]
- 27.Unger RH, Grundy S. Hyperglycaemia as an inducer as well as a consequence of impaired islet cell function and insulin resistance: implications for the management of diabetes. Diabetologia. 1985;28:119–121. doi: 10.1007/BF00273856. [DOI] [PubMed] [Google Scholar]
- 28.Rossetti L, Giaccari A, DeFronzo RA. Glucose toxicity. Diabetes Care. 1990;13:610–630. doi: 10.2337/diacare.13.6.610. [DOI] [PubMed] [Google Scholar]
- 29.Garvey WT, Olefsky JM, Griffin J, Hamman RF, Kolterman OG. The effect of insulin treatment on insulin secretion and insulin action in type II diabetes mellitus. Diabetes. 1985;34:222–234. doi: 10.2337/diab.34.3.222. [DOI] [PubMed] [Google Scholar]