Abstract
Background
Some patients with type 2 diabetes mellitus (T2DM) do not develop diabetic kidney disease (DKD) despite the presence of advanced diabetic retinopathy (DR). We aimed to investigate the presence of DKD and its risk factors in patients with T2DM and advanced DR.
Methods
We conducted a cross-sectional study in 317 patients with T2DM and advanced DR. The phenotypes of DKD were divided into three groups according to the urine albumin/creatinine ratio (uACR, mg/g) and estimated glomerular filtration rate (eGFR, mL/min/1.73 m2): no DKD (uACR <30 and eGFR ≥60), non-severe DKD (uACR ≥30 or eGFR <60), and severe DKD (uACR ≥30 and eGFR <60). Mean systolic and diastolic blood pressure, mean glycosylated hemoglobin (HbA1c) level, and HbA1c variability (standard deviation [SD] of serial HbA1c values or HbA1c-SD) were calculated for the preceding 2 years.
Results
The prevalence of no DKD, non-severe DKD, and severe DKD was 37.2% (n=118), 37.0% (n=117), and 25.8% (n=82), respectively. HbA1c-SD and the triglyceride/high density lipoprotein cholesterol (TG/HDL-C) ratio correlated positively with uACR and negatively with eGFR. Multiple linear regression analyses showed that the HbA1c-SD and TG/HDL-C ratio were significantly related with eGFR. Multiple logistic regression analyses after adjusting for several risk factors showed that HbA1c-SD and the TG/HDL-C ratio were significant risk factors for severe DKD.
Conclusion
The prevalence of DKD was about 60% in patients with T2DM and advanced DR. HbA1c variability and TG/HDL-C ratio may affect the development and progression of DKD in these patients.
Keywords: Cholesterol, HDL; Diabetes mellitus, type 2; Diabetic nephropathies; Diabetic retinopathy; Hemoglobin A1c protein, human; Triglycerides
INTRODUCTION
The major complications of diabetes mellitus are diabetic retinopathy (DR) and diabetic nephropathy/diabetic kidney disease (DKD), which can ultimately lead to blindness and end-stage renal disease, respectively. Both are closely associated with morbidity and mortality in patients with diabetes. Long-term exposure to high glucose levels and high blood pressure (BP) are risk factors for both DR and DKD [1,2], and DKD is often accompanied by DR.
Recently, some studies have reported the discordance between DR and DKD in patients with diabetes. In type 1 diabetes mellitus (T1DM), about one-quarter of participants (23.6%) had discordant progression of DR and DKD during the Diabetes Control and Complications Trial [3]. In the Italian multicenter Renal Insufficiency and Cardiovascular Events (RIACE) study, 637 of 1,540 patients (41.4%) with type 2 diabetes mellitus (T2DM) and advanced DR—including severe non-proliferative DR (non-PDR), pre-PDR, maculopathy, or blindness—showed no evidence of DKD, which is characterized by normoalbuminuria and normal estimated glomerular filtration rate (eGFR) [4]. Interestingly, this study reported that age, male sex, duration of diabetes, glycosylated hemoglobin (HbA1c) level, hypertension, high triglyceride (TG) level, and low high density lipoprotein cholesterol (HDL-C) level were associated with the presence of DKD in patients with advanced DR. By contrast, diabetes treatment, albuminuria, age, age at diabetes diagnosis, and smoking were associated with the presence of advanced DR in patients with DKD. Another study [5] showed that 85 of 196 patients (43.4%) with PDR had normoalbuminuria. Nighttime diastolic BP and a relative increase in platelet count were associated with albuminuria in patients with PDR.
The variability of glycemic control comprises both "glucose variability" and "HbA1c variability" [6]. Glucose variability is the daily fluctuations in the blood glucose level and represents a short-term change, whereas HbA1c variability reflects longer-term fluctuations in the blood glucose. Recent studies suggest that HbA1c variability is an independent risk factor for microvascular and macrovascular complications in patients with T1DM [7,8]. In patients with T2DM, HbA1c variability is associated with microalbuminuria [9,10]. Interestingly, in the Italian multicenter RIACE study, HbA1c variability was an independent predictor of DKD, but not of DR [6].
All of these studies suggest that some patients do not develop any signs of DKD despite the presence of advanced DR and that different factors may play roles in the pathogenesis of DR and DKD. However, the risk factors for the development and progression of DKD have not been clarified fully in patients with T2DM and advanced DR. Therefore, the first aim of this study was to investigate the prevalence of DKD in these patients. The second aim was to identify which risk factors including HbA1c variability were valuable to predict the progression of DKD in patients with advanced DR.
METHODS
Subjects
The inclusion criteria for the study subjects were as follows: (1) diagnosed with T2DM; (2) visited both the Eye Clinic and Diabetes Clinic at Yeouido St. Mary's Hospital, Seoul, Korea, from January 2013 to December 2013; and (3) had HbA1c measurements at least four times during the preceding 2 years so that the mean HbA1c levels and HbA1c variability could be calculated. The exclusion criteria were as follows: (1) diagnosed with T1DM (fasting C-peptide <0.6 ng/mL or positive result of islet cell antibody [ICA] or glutamic acid decarboxylase antibody) or secondary diabetes (history of chronic pancreatitis or pancreatectomy); (2) had primary renal disease or received a nephrectomy or renal transplantation; (3) had severe systemic disease (liver cirrhosis, active malignancy, or immune disorders); (4) pregnant women; and (5) had history of hyperglycemia caused by medications such as steroid or immunosuppressant. Thirty-five patients were excluded, and 984 patients were included in this study. This study was approved by the Institutional Review Board of Yeouido St. Mary's Hospital.
Measurements
The following information about the study subjects was collected from their medical records: age, sex, body weight, BP, duration of diabetes, insulin use, smoking status, history of hypertension and cardiovascular disease (CVD), use of an angiotensin-converting-enzyme inhibitor (ACEi) or angiotensin receptor blocker (ARB), and laboratory data. Hypertension was defined as a systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg or any use of antihypertensive medications. CVD was defined as a history of coronary artery disease or cerebrovascular disease. Body mass index (BMI) was calculated using the following formula: BMI=weight (kg)/height (m2).
The presence of DR was assessed by two expert ophthalmologists using a digital fundus camera (TRC-NW6S; Topcon, Tokyo, Japan). The type of DR was classified as reported by the Global Diabetic Retinopathy Project Group [11]. Patients were classified into the following categories: absent DR; mild, moderate, or severe non-PDR; and PDR. Using the classification of the worse eye, patients with absent DR or mild non-PDR were classified as having non-advanced DR, and those with moderate or severe non-PDR or PDR were classified as having advanced DR [12]. A total of 317 patients (32.2%) were classified as having advanced DR.
The presence of DKD was identified by assessing albuminuria and the eGFR. Albuminuria was identified by calculating the urine albumin/creatinine ratio (uACR, mg/g) in first-voided spot urine samples, and eGFR (mL/min/1.73 m2) was calculated using the Modification of Diet in Renal Disease study equation [13]. Phenotypes of DKD were classified according to the following categories: no DKD (uACR <30 and eGFR ≥60), non-severe DKD (uACR ≥30 or eGFR <60), and severe DKD (uACR ≥30 and eGFR <60).
Mean systolic and diastolic BP, and mean HbA1c level were calculated during the preceding 2 years. HbA1c variability was calculated for each patient as the intraindividual standard deviation (SD) of serial HbA1c values (HbA1c-SD) during the preceding 2 years. To correct for the interindividual differences in the number of HbA1c assessments, an adjusted value (adj-HbA1c-SD) was also calculated according to the following formula: adj-HbA1c-SD=SD/square root of [n/(n−1)], where n was the number of HbA1c measurements [7]. The coefficient of variation of HbA1c (HbA1c-CV) was calculated as the ratio of HbA1c-SD to mean HbA1c to adjust for larger SDs because of higher absolute values of mean HbA1c [8].
Statistical analysis
All statistical analyses were performed using SAS software version 9.3 (SAS Institute, Cary, NC, USA). Data are presented as mean±SD for continuous variables except for TG concentration, ACR, and the TG/HDL-C ratio, which are presented as geometric mean (95% confidence interval [CI]), and as proportions for categorical variables. The t-test or chi-square test was performed to identify differences in baseline clinical characteristics between the non-advanced DR and advanced DR groups. Analysis of variance or the chi-square test were used to compare the clinical characteristics between the no DKD, non-severe DKD, and severe DKD groups of patients with T2DM and advanced DR. Post hoc analysis was used to compare between no DKD and severe DKD groups. Spearman correlation analysis was used to confirm the associations between HbA1c variability and uACR or eGFR, and between the TG/HDL-C ratio and uACR or eGFR.
Multiple linear regression analysis was used to identify associations between uACR or eGFR and HbA1c variability or the TG/HDL-C ratio. The results are reported for both before and after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin, mean HbA1c levels, and the TG/HDL-C ratio or HbA1c-SD. Finally, multivariate logistic regression analysis was performed to confirm HbA1c variability or TG/HDL-C ratio as risk factors for severe DKD. The results are shown both before and after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin and mean HbA1c levels, and the TG/HDL-C ratio or HbA1c-SD. A P<0.05 was considered significant.
RESULTS
The baseline clinical characteristics of all the study subjects are shown in Table 1. Compared with patients with non-advanced DR, those with advanced DR were older; predominantly male; had a higher systolic BP; longer duration of diabetes; more frequent use of insulin, ACEi, or ARB; and more frequent history of hypertension and CVD. The prevalence of DKD (non-severe+severe DKD) was higher in patients with advanced DR than in those with non-advanced DR (62.8% vs. 28.6%, P<0.01).
Table 1. Baseline clinical characteristics of all the study subjects.
| Characteristic | Non-advanced DR | Advanced DR | P value |
|---|---|---|---|
| Number | 667 (67.8) | 317 (32.7) | - |
| Age, yr | 59.58±11.04 | 63.20±10.74 | <0.01 |
| Female sex | 379 (56.82) | 155 (48.90) | 0.02 |
| BMI, kg/m2 | 25.24±3.49 | 25.01±3.40 | 0.33 |
| SBP, mm Hg | 126.54±14.61 | 132.06±17.12 | <0.01 |
| DBP, mm Hg | 76.51±10.61 | 75.27±11.41 | 0.09 |
| Diabetes duration, yr | 11.33±7.17 | 19.84±8.15 | <0.01 |
| Insulin user | 66 (9.90) | 155 (48.90) | <0.01 |
| Current smoker | 124 (18.59) | 47 (14.83) | <0.01 |
| Hypertension history | 388 (58.17) | 238 (75.08) | <0.01 |
| ACEi or ARBs user | 349 (52.32) | 213 (67.19) | <0.01 |
| Statin user | 496 (74.4) | 224 (70.7) | 0.22 |
| Fenofibrate user | 67 (10.0) | 18 (5.7) | 0.02 |
| CVD history | 175 (26.24) | 123 (38.8) | <0.01 |
| Mean HbA1c | 7.06±0.85 | 7.76±1.05 | <0.01 |
| DKD | <0.01 | ||
| No DKD | 476 (71.36) | 118 (37.22) | |
| Non-severe DKD | 154 (23.09) | 117 (36.91) | |
| Severe DKD | 37 (5.55) | 82 (25.87) | |
| DR | <0.01 | ||
| Absent DR | 494 (74.1) | - | |
| Mild non-PDR | 173 (25.9) | - | |
| Moderate non-PDR | - | 80 (25.2) | |
| Severe non-PDR | - | 130 (41.0) | |
| PDR | - | 107 (33.8) |
Values are presented as number (%) or mean±standard deviation.
DR, diabetic retinopathy; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; ACEi, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker; CVD, cardiovascular disease; HbA1c, glycosylated hemoglobin; DKD, diabetic kidney disease; PDR, proliferative diabetic retinopathy.
In study subjects with advanced DR, the prevalence of no DKD, non-severe DKD, and severe DKD was 37.2% (n=118), 37.0% (n=117), and 25.8% (n=82), respectively (Table 2). Compared with the no DKD group, the severe DKD group had higher systolic BP (127.99±10.88 mm Hg vs. 132.65±10.65 mm Hg, P=0.01); lower HDL-C (1.21±0.30 mmol/L vs. 1.03±0.29 mmol/L, P<0.01); higher TG (1.18 [1.09 to 1.29] mmol/L vs. 1.64 [1.47 to 1.83] mmol/L, P<0.01); and higher TG/HDL-C ratio (2.3 [2.1 to 2.6] vs. 3.8 [3.3 to 4.3], P<0.01) by post hoc analysis. Compared with the no DKD group, the severe DKD group had higher values for all three indices of HbA1c variability: HbA1c-SD, 0.58±0.39 vs. 0.74±0.43 (P=0.03); adj-HbA1c-SD, 0.53±0.35 vs. 0.68±0.39 (P=0.02); and HbA1c-CV 0.07±0.04 vs. 0.09±0.05 (P=0.01). However, BMI, duration of diabetes, and mean HbA1c and LDL-C levels did not differ significantly between the no DKD and severe DKD groups.
Table 2. Clinical characteristics of the patients with type 2 diabetes mellitus and advanced diabetic retinopathy according to DKD.
| Characteristic | No DKD | Non-severe DKD | Severe DKD | P value |
|---|---|---|---|---|
| Number | 118 (37.2) | 117 (37.0) | 82 (25.8) | - |
| Age, yr | 62.73±8.92 | 63.18±11.26 | 63.90±12.38 | 0.75 |
| Female sex | 62 (52.54) | 50 (42.74) | 50 (60.98) | 0.04 |
| BMI, kg/m2 | 24.94±3.58 | 24.66±2.95 | 25.61±3.69 | 0.16 |
| Mean SBP, mm Hg | 127.99±10.88 | 129.29±11.68 | 132.65±10.65 | 0.01 |
| Mean DBP, mm Hg | 72.86±7.08 | 73.35±7.99 | 74.70±16.99 | 0.49 |
| Diabetes duration, yr | 19.79±8.21 | 19.38±8.17 | 20.55±8.09 | 0.61 |
| Insulin user | 51 (43.22) | 51 (43.59) | 53 (64.63) | <0.01 |
| Current smoker | 16 (14.41) | 22 (19.47) | 9 (11.39) | 0.29 |
| Hypertension history | 76 (64.41) | 89 (76.07) | 73 (90.12) | <0.01 |
| ACEi or ARB user | 70 (59.32) | 84 (72.41) | 59 (71.95) | 0.06 |
| Statin user | 80 (67.8) | 81 (69.2) | 63 (76.8) | 0.35 |
| Fenofibrate user | 9 (7.6) | 7 (6.0) | 2 (2.4) | 0.29 |
| CVD history | 49 (41.53) | 37 (31.62) | 37 (45.12) | 0.12 |
| C-peptide, nmol/L | 0.92±0.72 | 1.01±0.69 | 1.41±1.14 | <0.01 |
| Hemoglobin, g/L | 135.2±13.6 | 129.8±16.0 | 115.4±15.0 | <0.01 |
| Mean HbA1c, % | 7.70±1.03 | 7.82±1.08 | 7.74±1.04 | 0.68 |
| Mean HbA1c, mmol/mol | 61±12 | 62±12 | 61±12 | 0.68 |
| HbA1c-SD, % | 0.58±0.39 | 0.61±0.39 | 0.74±0.43 | 0.02 |
| Adj-HbA1c-SD, % | 0.53±0.35 | 0.56±0.36 | 0.68±0.39 | 0.02 |
| HbA1c-CV, % | 0.07±0.04 | 0.08±0.04 | 0.09±0.05 | <0.01 |
| HDL-C, mmol/L | 1.21±0.30 | 1.17±0.35 | 1.03±0.29 | <0.01 |
| LDL-C, mmol/L | 2.13±0.66 | 2.08±0.70 | 2.09±0.70 | 0.84 |
| TG, mmol/L | 1.18 (1.09–1.29) | 1.47 (1.34–1.62) | 1.64 (1.47–1.83) | <0.01 |
| TG/HDL-C ratio | 2.3 (2.1–2.6) | 3 (2.7–3.4) | 3.8 (3.3–4.3) | <0.01 |
| Creatinine, µmol/L | 78.68±12.38 | 94.59±35.36 | 194.5±161.8 | <0.01 |
| eGFR, mL/min/1.73 m2 | 80.88±13.32 | 71.62±17.84 | 38.20±15.32 | <0.01 |
| uACR, µg/mg | 11.51 (10.46–12.67) | 81.87 (62.36–107.49) | 494.57 (334.1–732.1) | <0.01 |
Values are presented as number (%), mean±standard deviation, or geometric mean (95% confidence interval).
DKD, diabetic kidney disease; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; ACEi, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker; CVD, cardiovascular disease; HbA1c, glycosylated hemoglobin; SD, standard deviation; Adj, adjusted; CV, coefficient of variation; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; TG, triglyceride; eGFR, estimated glomerular filtration rate; uACR, urine albumin/creatinine ratio.
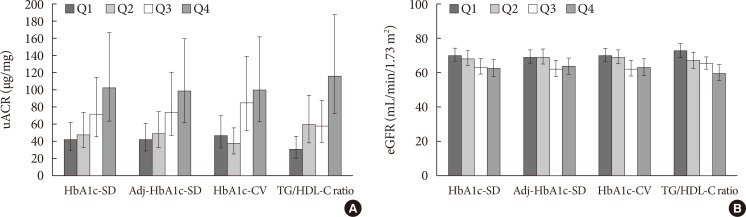
In study subjects with advanced DR, the indices of HbA1c variability correlated positively with uACR (HbA1c-SD, r=0.17, P<0.01; adj-HbA1c-SD, r=0.17, P<0.01; HbA1c-CV, r=0.18, P<0.01). These indices correlated negatively with eGFR (HbA1c-SD, r=–0.11, P=0.049; adj-HbA1c-SD, r=–0.11, P=0.048; HbA1c-CV, r=–0.14, P=0.01). The TG/HDL-C ratio correlated significantly with uACR (r=0.27, P<0.01) and eGFR (r=–0.21, P<0.01). The mean uACR and eGFR and 95% CI according to four quartiles (Q1, Q2, Q3, and Q4) of indices of HbA1c variability and the TG/HDL-C ratio in patients with T2DM and advanced DR are presented in Fig. 1. uACR increased significantly as HbA1c variability and the TG/HDL-C ratio increased (Fig. 1A, all P for trend <0.01). By contrast, eGFR decreased significantly as HbA1c variability and the TG/HDL-C ratio increased (Fig. 1B) (HbA1c-SD, P for trend=0.01; adj-HbA1c-SD, P for trend=0.04; HbA1c-CV, P for trend=0.01; TG/HDL-C ratio, P for trend <0.01).
Fig. 1. The mean (A) urine albumin/creatinine ratio (uACR; µg/mg) or (B) estimated glomerular filtration rate (eGFR; mL/min/1.73 m2) and 95% confidence interval according to four quartiles (Q1, Q2, Q3, and Q4) of indices of glycosylated hemoglobin (HbA1c) variability and the triglyceride (TG)/high density lipoprotein cholesterol (HDL-C) ratio in patients with type 2 diabetes mellitus and advanced diabetic retinopathy were presented in the figure. Median and interquartile ranges of indices of HbA1c variability were 0.56 (0.35 to 0.78) for HbA1c-standard deviation (SD), 0.51 (0.32 to 0.72) for adjusted (Adj)-HbA1c-SD and 0.07 (0.05 to 0.10) for HbA1c-coefficient of variation (CV), respectively. Median and interquartile ranges of indices of the TG/HDL-C ratio were 2.9 (1.8 to 4.5). All P for trend <0.05 by analysis of variance.
We have conducted additional analyses to confirm whether HbA1c variability and TG/HDL ratio are risk factors of DKD progression in patients with advanced DR. Multiple linear regression analysis (Table 3) showed that indices of HbA1c variability were negatively related to eGFR both before and after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin, mean HbA1c levels, and the TG/HDL-C ratio in the study subjects with advanced DR. Indices of HbA1c variability were positively related to uACR before and after adjusting for age and sex. Similarly, the TG/HDL-C ratio was significantly related to uACR and eGFR both before and after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin, mean HbA1c levels, and HbA1c-SD. Therefore, HbA1c variability and the TG/HDL-C ratio were independent risk factors of eGFR aggravation in these patients.
Table 3. Multiple linear regression analyses in patients with type 2 diabetes mellitus and advanced diabetic retinopathy.
| Variable | uACR | eGFR | ||
|---|---|---|---|---|
| β | P value | β | P value | |
| HbA1c-SD | ||||
| Model 1 | 0.56 | <0.01 | −4.24 | 0.05 |
| Model 2 | 0.50 | <0.01 | −4.99 | 0.02 |
| Model 3 | 0.22 | 0.26 | −5.04 | 0.02 |
| Adj-HbA1c-SD | ||||
| Model 1 | 0.56 | <0.01 | −4.23 | 0.05 |
| Model 2 | 0.50 | <0.01 | −4.97 | 0.02 |
| Model 3 | 0.23 | 0.24 | −5.06 | 0.02 |
| HbA1c-CV | ||||
| Model 1 | 0.64 | <0.01 | −5.87 | 0.01 |
| Model 2 | 0.57 | <0.01 | −7.01 | <0.01 |
| Model 3 | 0.23 | 0.25 | −5.14 | 0.02 |
| TG/HDL-C ratio | ||||
| Model 1 | 0.80 | <0.01 | −7.26 | <0.01 |
| Model 2 | 0.77 | <0.01 | −8.28 | <0.01 |
| Model 3 | 0.58 | <0.01 | −6.66 | <0.01 |
Model 1: non-adjusted; model 2: adjustments for age and sex; model 3: model 2 plus adjustments for mean systolic blood pressure (SBP), diabetes duration, hemoglobin, mean HbA1c, TG/HDL-C ratio; model 3a: model 2 plus adjustments for mean SBP, diabetes duration, hemoglobin, mean HbA1c, HbA1c-SD.
uACR, urine albumin/creatinine ratio; eGFR, estimated glomerular filtration rate; HbA1c, glycosylated hemoglobin; SD, standard deviation; Adj, adjusted; CV, coefficient of variation; TG, triglyceride; HDL-C, high density lipoprotein cholesterol.
Finally, after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin, and mean HbA1c levels, the multivariate logistic regression analysis showed that HbA1c variability and the TG/HDL-C ratio were significant and independent risk factors for severe DKD in study subjects with advanced DR (Table 4).
Table 4. Multivariate logistic regression analyses of HbA1c variability or TG/HDL-C ratio as predictors of the severe diabetic kidney disease in patients with type 2 diabetes mellitus and advanced diabetic retinopathy.
| Variable | OR (95% CI)a | |||
|---|---|---|---|---|
| HbA1c-SD | Adj-HbA1c-SD | HbA1c-CV | TG/HDL-C ratio | |
| Model 1 | 1.92 (1.24–2.97) | 1.91 (1.24–2.97) | 2.26 (1.38–3.69) | 2.43 (1.58–3.74) |
| Model 2 | 2.03 (1.29–3.18) | 2.02 (1.29–3.17) | 2.47 (1.49–4.11) | 2.65 (1.69–4.14) |
| Model 3 | 2.22 (1.17–4.22) | 2.22 (1.17–4.21) | 2.24 (1.18–4.25) | - |
| Model 3a | - | - | - | 2.51 (1.46–4.30) |
Model 1: non-adjusted; model 2: adjustments for age and sex; model 3: model 2 plus adjustments for mean systolic blood pressure (SBP), diabetes duration, hemoglobin, mean HbA1c, TG/HDL-C ratio; model 3a: model 2 plus adjustments for mean SBP, diabetes duration, hemoglobin, mean HbA1c, HbA1c-SD.
HbA1c, glycosylated hemoglobin; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; OR, odds ratio; CI, confidence interval; SD, standard deviation; Adj, adjusted; CV, coefficient of variation.
aAll P<0.05.
DISCUSSION
In this cross-sectional study, we found that the prevalence of DKD (non-severe+severe DKD) was 62.8% in patients with advanced DR. Indices of HbA1c variability and the TG/HDL-C ratio were significantly associated with uACR and eGFR, and were significant risk factors for the presence of severe DKD. These associations were independent of age, sex, mean systolic BP, duration of diabetes, hemoglobin, and mean HbA1c levels.
DKD, which is defined as kidney disease attributable to diabetes, remains one of the most frequent complications of T2DM and the leading cause of end-stage renal disease. DKD is closely associated with DR, possibly because both share long-term exposure to high glucose. However, some patients do not develop any sign of DKD despite the presence of advanced DR. Thus, it is crucial to identify the risk factors for the development and progression of DKD in patients with DR. Identifying and monitoring DKD requires assessment of both kidney function, usually an eGFR <60 mL/min/1.73 m2, and albuminuria, usually an uACR >30 mg/g creatinine [14]. Because both eGFR and albuminuria have limitations in the evaluation of DKD, we attempted to divide the phenotypes of DKD into no DKD (no reduced eGFR and no albuminuria), non-severe DKD (reduced eGFR or albuminuria), and severe DKD (reduced eGFR and albuminuria) on the basis of the eGFR and uACR values. In the present study, the prevalence of DKD (non-severe DKD, 37.0%; severe DKD, 25.8%) in patients with advanced DR was 62.8%. This finding is consistent with the results of the RIACE study, which found that 58.6% of 1,540 patients with advanced DR had DKD (non-severe DKD, 39.9%; severe DKD, 18.7%), although the definition of advanced DR was a little different [4].
Evidence suggests that short- or long-term glycemic variability (i.e., glucose or HbA1c variability) is independently associated with microvascular complications in patients with diabetes [6,15]. This reflects that glycemic instability, and not just hyperglycemia, contributes to the development of diabetic complications. Several prospective studies have demonstrated that HbA1c variability influences the development of microalbuminuria and reduced eGFR [9,10,16]. Although the mechanisms underlying the deleterious effects of HbA1c variability in the kidney are not clear, one possible mechanism involves "metabolic memory" from repeated exposure to glycemic instability [17], which causes increased oxidative stress [18,19]. In the present study, HbA1c variability was significantly associated with uACR and eGFR, and was a significant risk factor of the presence of severe DKD after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin and mean HbA1c levels, and the TG/HDL-C ratio in patients with advanced DR. This finding is consistent with those of other studies [6,9,10,16]. Interestingly, the RIACE study demonstrated that HbA1c variability affected the DKD phenotype with both albuminuria and reduced eGFR (severe DKD in the present study) more than average HbA1c [6].
Dyslipidemia occurs frequently in patients with T2DM and plays a central role in the development of atherosclerosis. High TG and low HDL-C concentrations are the main features of dyslipidemia in patients with diabetes [20]. Several studies have reported that a higher HDL-C level is protective against the progression of DKD in patients with T2DM [21,22]. In particular, the Action in Diabetes and Vascular Disease: preterAx and diamicroN-MR Controlled Evaluation (ADVANCE) study, which was the largest prospective analysis that specifically addressed HDL-C level and risk of microvascular disease in patients with T2DM [23], showed that a lower baseline HDL-C level is a significant and independent predictor of the development and progression of DKD. By contrast, there was no association between baseline HDL-C level and the risk of DR. The association between HDL-C level and the progression of DKD has been attributed to several possible pathological mechanisms. The HDL involves reverse cholesterol transport pathway and plays an important role in glomerulosclerosis and tubulointerstitial damage. HDL also has antioxidant and anti-inflammatory properties [24,25].
In addition, hypertriglyceridemia can aggregate fat infiltration and deposition within renal tubules, which results in progressive tubulointerstitial damage [26,27]. The Fenofibrate Intervention and Event Lowering in Diabetes Study and the Diabetes Atherosclerosis Intervention Study showed that improvement of hypertriglyceridemia by fenofibrate reduced albuminuria and slowed the reduction of eGFR [28,29]. Another study in Korean patients with T2DM also showed that hypertriglyceridemia significantly affected the progression of DKD [30]. Therefore, it is not surprising that a high TG/HDL-C ratio is an independent risk factor for the development of reduced eGFR in patient with T2DM [21]. Consistent with the aforementioned studies, in our patients with advanced DR, the TG/HDL-C ratio was significantly associated with uACR and eGFR, and was a significant risk factor of the presence of the severe DKD after adjusting for age, sex, mean systolic BP, duration of diabetes, hemoglobin, and mean HbA1c levels.
There are some limitations in the present study. First, database in the present study is based on cross-sectional data, except HbA1c and BP. Therefore, it is difficult to prove that HbA1c variability and TG/HDL-C ratio are predictors of DKD progression in patients with T2DM and advanced DR. However, according to various analyses in this study, HbA1c variability and TG/HDL-C ratio were significantly related with eGFR, uACR, and severe DKD. Then, large scale, prospective studies were needed to confirm the causal relationship of HbA1c variability or TG/HDL-C ratio and severe DKD in patients with advanced DR. Second, this study was performed by data collection from a single center, and with a relatively small number of patients. Third, the study subjects might have had other etiologies for chronic kidney disease in addition to diabetes mellitus. Patients diagnosed with primary renal disease and/or history of nephrectomy or renal transplantation according to chart review were excluded. However, a limitation of the study includes the fact that not all of the patients underwent renal biopsy. Fourth, the HbA1c variability could be affected by glycemic status and other comorbidities of patients during previous 2 years. Thus, certain medications and other interventions had confounding results. However, we excluded the subjects who had severe systemic disease such as liver cirrhosis, active malignancy, or immune disorders.
In conclusion, the prevalence of DKD was about 60% in patients with T2DM and advanced DR. HbA1c variability and TG/HDL-C ratio may affect the development and progression of DKD in these patients. In other words, patients with no evidence of DKD despite the presence of advanced DR showed relatively good glucose variability, lower TG, and higher HDL-C. Thus, control of glucose variability, TG, and HDL-C can be thought to be important in order to prevent the progression of DKD in patients with advanced DR. However, the present study is cross-sectional design, so it is difficult to investigate the causal relationship. The large scale, well-designed prospective studies about DKD progression according to glucose variability and lipid profile in patients with T2DM and advanced DR are needed to confirm the associations observed here.
ACKNOWLEDGMENTS
The authors thank Kyungdo Han in Department of Medical Statistics, College of Medicine, The Catholic University of Korea, for his statistical analysis.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Molitch ME, DeFronzo RA, Franz MJ, Keane WF, Mogensen CE, Parving HH American Diabetes Association. Diabetic nephropathy. Diabetes Care. 2003;26(Suppl 1):S94–S98. doi: 10.2337/diacare.26.2007.s94. [DOI] [PubMed] [Google Scholar]
- 2.Fong DS, Aiello L, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL, 3rd, Klein R American Diabetes Association. Retinopathy in diabetes. Diabetes Care. 2004;27(Suppl 1):S84–S87. doi: 10.2337/diacare.27.2007.s84. [DOI] [PubMed] [Google Scholar]
- 3.Kramer CK, Retnakaran R. Concordance of retinopathy and nephropathy over time in type 1 diabetes: an analysis of data from the Diabetes Control and Complications Trial. Diabet Med. 2013;30:1333–1341. doi: 10.1111/dme.12296. [DOI] [PubMed] [Google Scholar]
- 4.Penno G, Solini A, Zoppini G, Orsi E, Zerbini G, Trevisan R, Gruden G, Cavalot F, Laviola L, Morano S, Nicolucci A, Pugliese G Renal Insufficiency And Cardiovascular Events (RIACE) Study Group. Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2012;35:2317–2323. doi: 10.2337/dc12-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magri CJ, Calleja N, Buhagiar G, Fava S, Vassallo J. Factors associated with diabetic nephropathy in subjects with proliferative retinopathy. Int Urol Nephrol. 2012;44:197–206. doi: 10.1007/s11255-011-9958-1. [DOI] [PubMed] [Google Scholar]
- 6.Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, Morano S, Cavalot F, Lamacchia O, Laviola L, Nicolucci A, Pugliese G Renal Insufficiency And Cardiovascular Events Study Group. HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2013;36:2301–2310. doi: 10.2337/dc12-2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kilpatrick ES, Rigby AS, Atkin SL. A1C variability and the risk of microvascular complications in type 1 diabetes: data from the Diabetes Control and Complications Trial. Diabetes Care. 2008;31:2198–2202. doi: 10.2337/dc08-0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waden J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop PH Finnish Diabetic Nephropathy Study Group. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes. 2009;58:2649–2655. doi: 10.2337/db09-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu CC, Chang HY, Huang MC, Hwang SJ, Yang YC, Lee YS, Shin SJ, Tai TY. HbA1c variability is associated with microalbuminuria development in type 2 diabetes: a 7-year prospective cohort study. Diabetologia. 2012;55:3163–3172. doi: 10.1007/s00125-012-2700-4. [DOI] [PubMed] [Google Scholar]
- 10.Sugawara A, Kawai K, Motohashi S, Saito K, Kodama S, Yachi Y, Hirasawa R, Shimano H, Yamazaki K, Sone H. HbA(1c) variability and the development of microalbuminuria in type 2 diabetes: Tsukuba Kawai Diabetes Registry 2. Diabetologia. 2012;55:2128–2131. doi: 10.1007/s00125-012-2572-7. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson CP, Ferris FL, 3rd, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT Global Diabetic Retinopathy Project Group. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–1682. doi: 10.1016/S0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 12.Matsumoto A, Iwashima Y, Abiko A, Morikawa A, Sekiguchi M, Eto M, Makino I. Detection of the association between a deletion polymorphism in the gene encoding angiotensin I-converting enzyme and advanced diabetic retinopathy. Diabetes Res Clin Pract. 2000;50:195–202. doi: 10.1016/s0168-8227(00)00194-7. [DOI] [PubMed] [Google Scholar]
- 13.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F Chronic Kidney Disease Epidemiology Collaboration. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 14.Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, Hirsch IB, Kalantar-Zadeh K, Narva AS, Navaneethan SD, Neumiller JJ, Patel UD, Ratner RE, Whaley-Connell AT, Molitch ME. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37:2864–2883. doi: 10.2337/dc14-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nalysnyk L, Hernandez-Medina M, Krishnarajah G. Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab. 2010;12:288–298. doi: 10.1111/j.1463-1326.2009.01160.x. [DOI] [PubMed] [Google Scholar]
- 16.Luk AO, Ma RC, Lau ES, Yang X, Lau WW, Yu LW, Chow FC, Chan JC, So WY. Risk association of HbA1c variability with chronic kidney disease and cardiovascular disease in type 2 diabetes: prospective analysis of the Hong Kong Diabetes Registry. Diabetes Metab Res Rev. 2013;29:384–390. doi: 10.1002/dmrr.2404. [DOI] [PubMed] [Google Scholar]
- 17.Ihnat MA, Thorpe JE, Ceriello A. Hypothesis: the 'metabolic memory', the new challenge of diabetes. Diabet Med. 2007;24:582–586. doi: 10.1111/j.1464-5491.2007.02138.x. [DOI] [PubMed] [Google Scholar]
- 18.Rizzo MR, Barbieri M, Marfella R, Paolisso G. Reduction of oxidative stress and inflammation by blunting daily acute glucose fluctuations in patients with type 2 diabetes: role of dipeptidyl peptidase-IV inhibition. Diabetes Care. 2012;35:2076–2082. doi: 10.2337/dc12-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–1687. doi: 10.1001/jama.295.14.1681. [DOI] [PubMed] [Google Scholar]
- 20.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–2581. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- 21.Lee IT, Wang CY, Huang CN, Fu CC, Sheu WH. High triglyceride-to-HDL cholesterol ratio associated with albuminuria in type 2 diabetic subjects. J Diabetes Complications. 2013;27:243–247. doi: 10.1016/j.jdiacomp.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Chang YH, Chang DM, Lin KC, Hsieh CH, Lee YJ. High-density lipoprotein cholesterol and the risk of nephropathy in type 2 diabetic patients. Nutr Metab Cardiovasc Dis. 2013;23:751–757. doi: 10.1016/j.numecd.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 23.Morton J, Zoungas S, Li Q, Patel AA, Chalmers J, Woodward M, Celermajer DS, Beulens JW, Stolk RP, Glasziou P, Ng MK ADVANCE Collaborative Group. Low HDL cholesterol and the risk of diabetic nephropathy and retinopathy: results of the ADVANCE study. Diabetes Care. 2012;35:2201–2206. doi: 10.2337/dc12-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabet F, Rye KA. High-density lipoproteins, inflammation and oxidative stress. Clin Sci (Lond) 2009;116:87–98. doi: 10.1042/CS20080106. [DOI] [PubMed] [Google Scholar]
- 25.Vaziri ND. Lipotoxicity and impaired high density lipoprotein-mediated reverse cholesterol transport in chronic kidney disease. J Ren Nutr. 2010;20(5 Suppl):S35–S43. doi: 10.1053/j.jrn.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Attman PO. Progression of renal failure and lipids: is there evidence for a link in humans? Nephrol Dial Transplant. 1998;13:545–547. doi: 10.1093/ndt/13.3.545. [DOI] [PubMed] [Google Scholar]
- 27.Weinberg JM. Lipotoxicity. Kidney Int. 2006;70:1560–1566. doi: 10.1038/sj.ki.5001834. [DOI] [PubMed] [Google Scholar]
- 28.Davis TM, Ting R, Best JD, Donoghoe MW, Drury PL, Sullivan DR, Jenkins AJ, O'Connell RL, Whiting MJ, Glasziou PP, Simes RJ, Kesäniemi YA, Gebski VJ, Scott RS, Keech AC Fenofibrate Intervention and Event Lowering in Diabetes Study investigators. Effects of fenofibrate on renal function in patients with type 2 diabetes mellitus: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) Study. Diabetologia. 2011;54:280–290. doi: 10.1007/s00125-010-1951-1. [DOI] [PubMed] [Google Scholar]
- 29.Ansquer JC, Foucher C, Rattier S, Taskinen MR, Steiner G DAIS Investigators. Fenofibrate reduces progression to microalbuminuria over 3 years in a placebo-controlled study in type 2 diabetes: results from the Diabetes Atherosclerosis Intervention Study (DAIS) Am J Kidney Dis. 2005;45:485–493. doi: 10.1053/j.ajkd.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Kim DM, Ahn CW, Park JS, Cha BS, Lim SK, Kim KR, Lee HC, Huh KB. An implication of hypertriglyceridemia in the progression of diabetic nephropathy in metabolically obese, normal weight patients with type 2 diabetes mellitus in Korea. Diabetes Res Clin Pract. 2004;66(Suppl 1):S169–S172. doi: 10.1016/j.diabres.2004.07.011. [DOI] [PubMed] [Google Scholar]