Abstract
Objective
This paper aims to assess the socioeconomic determinants of a high 10 year cardiovascular risk in Tunisia.
Setting
We used a national population based cross sectional survey conducted in 2005 in Tunisia comprising 7780 subjects. We applied the non-laboratory version of the Framingham equation to estimate the 10 year cardiovascular risk.
Participants
8007 participants, aged 35–74 years, were included in the sample but effective exclusion of individuals with cardiovascular diseases and cancer resulted in 7780 subjects (3326 men and 4454 women) included in the analysis.
Results
Mean age was 48.7 years. Women accounted for 50.5% of participants. According to the Framingham equation, 18.1% (17.25–18.9%) of the study population had a high risk (≥20% within 10 years). The gender difference was striking and statistically significant: 27.2% (25.7–28.7%) of men had a high risk, threefold higher than women (9.7%; 8.8–10.5%). A higher 10 year global cardiovascular risk was associated with social disadvantage in men and women; thus illiterate and divorced individuals, and adults without a professional activity had a significantly higher risk of developing a cardiovascular event in 10 years. Illiterate men were at higher risk than those with secondary and higher education (OR=7.01; 5.49 to 9.14). The risk in illiterate women was more elevated (OR=13.57; 7.58 to 24.31). Those living in an urban area had a higher risk (OR=1.45 (1.19 to 1.76) in men and OR=1.71 (1.35 to 2.18) in women).
Conclusions
The 10 year global cardiovascular risk in the Tunisian population is already substantially high, affecting almost a third of men and 1 in 10 women, and concentrated in those more socially disadvantaged.
Keywords: CARDIOLOGY, EPIDEMIOLOGY, 10-year global cardiovascular risk, non–laboratory Framingham model, socio-economic determinants
Strengths and limitations of this study.
This study is one of the few existing population-based, representative and large studies address in the association between socioeconomic status and cardiovascular disease in the Mediterranean region, and particularly in North Africa.
The study was conducted using standardized methodology and showed a very high response rate.
The high response rate registered in this study.
The study is based on a cross-sectional survey that limits the causal interpretation of observed associations and also the dynamic and/or life course perspective of risk factors.
The selection bias was unavoidable as the investigation takes place in households which leads to greater involuntary recruitment of women and older persons.
The use of the non-laboratory version of the Framingham risk score might result in misclassification of CVD risk. However, as in most large-scale studies in countries with low resources, laboratory blood test remains difficult such as glucose measurement was made by a capillary blood glucose reader and absence of total cholesterol and HDL measurement: This score used the same risk factors that “laboratory” Framingham except the lipid tests (total cholesterol and HDL) were replaced by the body mass index (BMI). This method was originally designed to be used in settings with limited resources.30 Ankur Pandya et al. showed excellent agreement between the Framingham risk characterization using the “laboratory” model and “non-laboratory”.31 Although this score has not been calibrated to the Tunisian population yet, our estimates were critically appraised by Tunisian experts in risk estimation.
Introduction
Like the countries in the Eastern Mediterranean Region, Tunisia is entering a new phase of its epidemiological transition, characterised by population ageing1 and a significant increase in non-communicable diseases (NCDs), particularly cardiovascular diseases (CVDs) and type 2 diabetes.2 The burden of NCDs, including diabetes and CVDs, is already a challenge for the Tunisian health system, with CVDs now being the main burden of disease, accounting for 30% of registered deaths in 2009.2 3
A recent modelling study conducted at the national level showed that 98% of deaths from coronary heart disease between 1997 and 2009 in Tunisia were explained by a marked increase in risk factor levels.4 Trends for CVD risk factors are well known in Tunisia, with increasing levels particularly in the coastal zone.2 5 6 This might be attributable to changes in diet, lifestyle habits, increasing urbanisation and changing working conditions.2
In the context of the increasing burden of NCDs in developing, and particularly Southern and Eastern Mediterranean, countries, socioeconomic inequalities are significant and persistent, and linked to sociocultural issues.7–9
Describing social differences and the mechanisms underlying them is therefore of enormous importance, and examining the association of CVD risk with social characteristics might help in tackling the unequal burden of CVD in the region.10 11
Therefore, the aim of our study was to assess overall cardiovascular risk in Tunisia by 2015 to understand the distribution of global cardiovascular risk in Tunisian territories, and to assess its socioeconomic determinants.
Methods
Sampling
For our analyses, we used a nationwide representative survey of the Tunisian population. This survey was integrated in a collaborative project funded by the European Commission to study epidemiological transition and health impact in North Africa (TAHINA). The cross sectional survey was conducted from April 2004 to September 2005.
A national representative, stratified, three tier cluster sample of households was selected according to the seven administrative regions of Tunisia (d1: selection of 47 districts by major regions; d2: selection of 25 households among those comprising people aged 35–74 years; d3: selection randomly one person per household from all eligible household members) who responded to a questionnaire on previous morbidity, lifestyle and access to healthcare, and had received anthropometric and biological measures. It was a stratified sampling of the seven regions of Tunisia (Tunis District, North East, North West, Central East, Central West, South East and South West); these regions are characterised by a marked disparity in socioeconomic development.12 Sampling was conducted by the National Institute of Statistics. The sampling frame used was the 2004 national census. Sample size was 8225. A total of 8007 participants, aged 35–74 years, were included in the sample (response rate 97%).
Individuals with CVDs and cancer were excluded: hence 7780 subjects (3326 men and 4454 women) were included in the analysis.
Factors measured in our study were systolic blood pressure (SBP), diastolic blood pressure, weight, height, fasting capillary glucose and total cholesterol. Type 2 diabetes was defined according to WHO criteria (WHO 1999): either fasting capillary glucose ≥6.1 mmol/L, confirmed medication usage from the medication inventory or self-reported use of antidiabetic medications within the past 2 weeks of the examination. Smoking status was defined as ‘current smoker’ and blood pressure measurement was the average of three measurements.
Estimating cardiovascular risk
The Framingham model was used to calculate the overall 10 year cardiovascular risk of subjects without CVD and cancer, from 2005 to 2015. The risk factors included in the score were: age, sex, SBP treated (medication and lifestyle changes) and untreated, body mass index (BMI), smoking and diabetes. This calculation was based on the study of cardiovascular risk profile for use in primary prevention, detailed in the online supplementary appendix 1.13 The estimated risk is expressed as a percentage; it corresponds to a probability of cardiovascular event onset in the next 10 years.14 Details calculations are presented in online supplementary appendix 1.
bmjopen-2015-009195supp_appendix.pdf (218.8KB, pdf)
For univariate analysis, the score was coded into three classes: <10%=low risk; 10–20%=moderate risk; and >20%=high risk. For logistic regression analysis, the two first classes were combined.
Measurement of socioeconomic characteristics
Data on age, gender, marital status, level of education and professional occupation of the subjects were collected by interview. Professional occupation categories were obtained from the National Institute of Statistics.15
To assess living standards at the household level, an asset based proxy index for economic level of the household was derived from multivariate analysis of relevant items in the Tunisian context. The proxy was built from information on habitat characteristics as well as household goods via multiple components analysis and a hierarchical classification whose goal was determination of certain classes of homogeneous individuals. Individuals were then classified in three groups: low, moderate and high standard of living.
Data management and statistical analysis
Epidata software, V.3.1, was used for data entry and validation by double entry and standard procedures for checking quality. Management and data analysis in this study were done by the R software 2.15.2.
The sampling design—stratification, clustering and sampling weights (accounting for differential probabilities of selection)—was taken into account in all estimates and analyses.
Continuous variables are represented as mean±SD. Comparison of means was performed using ANOVA analysis. Binary variables were described and compared according to the χ2 test. Logistic regression results were used to determinate the association between socioeconomic determinants and 10 year global cardiovascular risk as binary variables in men and women separately. Crude associations were first assessed using univariate models, and then associations where adjusted for socioeconomic factors (area, education, household economic level proxy, professional activity and marital status). Results are presented as ORs (crude and adjusted) and 95% CI.
A linear model was used to determinate the association between socioeconomic determinants and 10 year global cardiovascular risk as continuous variables and testing the interaction between the level of education and the living standard of the household.
Missing values for biological data represented 5–10% and 3–5% for socioeconomic data. The Multiple Imputation by Chained Equations (MICE) method, an algorithm based on Markov Chain Monte Carlo, applicable in the case of random missing data, was used.16 17
Ethics
The study protocol was carried out according to the Declaration of Helsinki and was approved by the Tunisian Ministry of Health and the Tunisian National Council of Statistics (visa No 5/2005). Due to a high illiteracy rate, we used verbal consent; consent was written and read to participants. All participants gave their free informed verbal consent, after being thoroughly informed about the purpose, procedures and requirement of the survey. The ethics committees approved this consent procedure.
Results
In total, 7780 subjects (42.8% men and 57.2% women) were included who were free from CVDs and cancer.
Socioeconomic and demographic characteristics of the study population
Table 1 shows the socioeconomic and demographic characteristics of the study population by gender. Mean age was 48.7±9.4 years. Women accounted for 57.2% of participants; 67.6% lived in an urban area with 1 in 4 people residing in Greater Tunis; and 34.7% were illiterate (education level differed significantly by gender (49.2% for women vs 19.8% for men)).
Table 1.
Socioeconomic and demographic characteristics of the population study by gender
| Men (n=3326) | Women (n=4454) | Total (n=7780) | Significance | |
|---|---|---|---|---|
| Age (years) | 0.000 | |||
| 35–44 | 1367 (43.2) | 1739 (43.9) | 3106 (43.6) | |
| 45–54 | 1055 (31.7) | 1505 (33.8) | 2560 (31.2) | |
| 55–64 | 552 (16.8) | 777 (17.1) | 1329(16.9) | |
| 65–74 | 352 (8.3) | 433 (8.2) | 785 (8.3) | |
| Mean (±SD) age | 49.4±9.7 | 49.3±9.5 | 49.3±9.6 | |
| Area | 0.000 | |||
| Urban | 1965 (68.8) | 2518 (66.4) | 4483 (67.6) | |
| Rural | 1361 (31.2) | 1936 (33.6) | 3297 (32.4) | |
| Region | 0.000 | |||
| Great Tunis | 410 (26.0) | 580 (24.6) | 990 (25.3) | |
| North East | 540 (14.8) | 551 (14.1) | 1091 (14.4) | |
| North West | 483 (12.6) | 678 (13.3) | 1161 (12.9) | |
| Central East | 510 (21.8) | 605 (21.9) | 1115 (21.8) | |
| Central West | 512 (11.4) | 664 (12.2) | 1176 (11.8) | |
| South East | 433 (8.2) | 675 (8.5) | 1108 (8.4) | |
| South West | 438 (5.3) | 701 (5.4) | 1139 (5.4) | |
| Education | 0.000 | |||
| Illiterate | 811 (19.8) | 2527 (49.2) | 3338 (34.7) | |
| Primary | 1340 (39.1) | 1335 (31.5) | 2675 (35.2) | |
| Secondary | 820 (26.7) | 458 (14.2) | 1278 (20.4) | |
| High | 355 (14.3) | 134 (5.2) | 489 (9.7) | |
| Household economic level proxy | 0.000 | |||
| Low | 1197 (29.8) | 1795 (33.8) | 2992 (31.8) | |
| Moderate | 1150 (33.4) | 1616 (33.8) | 2766 (33.6) | |
| High | 979 (36.8) | 1043 (32.4) | 2022 (34.6) | |
| Professional activity | 0.000 | |||
| Not working/retired | 233 (7.1) | 3725 (78.4) | 3958(43.1) | |
| Employee | 1919 (55.7) | 414 (12.0) | 2333 (33.6) | |
| Intermediate | 357 (11.5) | 126 (3.8) | 483 (7.6) | |
| Senior | 817 (25.7) | 189 (5.8) | 1006 (15.6) | |
| Marital status | 0.000 | |||
| Single | 102 (3.0) | 130 (2.9) | 232 (2.9) | |
| Married | 3140 (94.0) | 3700 (83.2) | 6840 (88.5) | |
| Divorced/widowed | 84 (3.0) | 624 (13.9) | 708 (8.5) | |
| Social security | 0.000 | |||
| Yes | 2277 (71.5) | 2783 (65.7) | 5060 (68.5) |
Values are n (%) unless otherwise specified.
A statistically significant difference in occupation by gender was also evident: 78.4% of women were unemployed compared with only 7.1% of men (p<0.0001). The majority of the population was married (88.5%) and 34.6% of the surveyed population had a high standard of living. Only 68.5% of those surveyed were receiving social security.
Prevalence of cardiovascular risk factors by socioeconomic characteristics
Tables 2 and 3 show the prevalence of cardiovascular risk factors.
Table 2.
Prevalence of cardiovascular risk factors by socioeconomic characteristics among men
| Diabetes (%) | SBP (mean±SD) | Treated hypertension (%) | BMI (mean±SD) | Smoking (%) | |
|---|---|---|---|---|---|
| Age (years) | 0.000* | 0.000* | 0.006* | 0.000* | 0.001* |
| 35–44 | 10.6 | 122.0±13.7 | 49.7 | 25.6±4.4 | 58.7 |
| 45–54 | 17.1 | 126.1±17.2 | 79.7 | 25.6±4.4 | 53.2 |
| 55–64 | 22.7 | 133.0±19.26 | 85.6 | 25.3±4.4 | 54.0 |
| 65–74 | 22.8 | 137.0±22.91 | 91.3 | 24.3±4.04 | 49.1 |
| Area | 0.000* | NS** | 0.015* | 0.000* | NS** |
| Rural | 10.0 | 125.4±18.4 | 67.6 | 24.4±4.2 | 57.1 |
| Urban | 18.3 | 126.8±17.0 | 84.8 | 25.9±4.4 | 54.6 |
| Region | 0.000* | 0.000* | NS** | 0.000* | 0.004* |
| District of Tunis | 18.7 | 127.8±16.8 | 86.9 | 26.2±4.7 | 54.8 |
| North East | 13.3 | 122.8±16.1 | 76.0 | 25.1±4.1 | 56.1 |
| North West | 7.1 | 125.0±18.0 | 68.4 | 24.1±4.0 | 60.3 |
| Centre East | 21.5 | 128.8±18.4 | 78.1 | 25.9±4.3 | 56.1 |
| Centre West | 12.6 | 125.2±19.2 | 68.2 | 24.8±4.3 | 55.8 |
| South East | 15.1 | 128.0±15.2 | 83.9 | 25.3±3.8 | 49.2 |
| South West | 12.7 | 123.3±15.7 | 88.0 | 25.3±4.2 | 49.5 |
| Education | NS** | 0.000* | NS** | 0.000* | 0.000* |
| Illiterate | 15.0 | 129.6±20.9 | 78.5 | 23.9±3.8 | 55.4 |
| Primary | 14.2 | 125.4±16.8 | 69.1 | 25.3±4.6 | 60.4 |
| Secondary | 17.8 | 125.7±16.3 | 90.5 | 26.0±4.3 | 54.3 |
| High | 17.0 | 126.0±15.4 | 80.0 | 27.0±3.8 | 43.5 |
| Household economic level proxy | 0.000* | NS** | 0.016* | 0.000* | 0.000* |
| Low | 11.2 | 126.3±18.8 | 62.8 | 23.7±3.8 | 60.7 |
| Moderate | 14.9 | 126.5±17.7 | 79.9 | 25.3±4.2 | 57.7 |
| High | 20.1 | 126.4±16.1 | 87.3 | 26.9±4.4 | 48.9 |
| Professional activity | 0.013* | 0.000* | NS** | 0.000* | 0.000* |
| Not working/retired | 16.4 | 131.0±21.0 | 83.4 | 24.8±4.8 | 50.7 |
| Employee | 15.0 | 125.4±17.0 | 80.0 | 25.0±4.3 | 59.8 |
| Intermediate | 20.2 | 128.2±18.9 | 93.1 | 26.3±3.9 | 51.1 |
| Senior | 15.3 | 126.4±16.4 | 70.1 | 26.1±4.4 | 48.9 |
| Marital status | NS** | 0.007* | NS** | 0.006* | NS** |
| Single | 6.1 | 119.6±11.4 | 72.3 | 23.7±3.3 | 58.9 |
| Married | 16.0 | 126.4±17.5 | 80.5 | 25.5±4.3 | 55.2 |
| Divorced/widowed | 17.1 | 131.5±18.9 | 78.6 | 26.6±5.3 | 56.6 |
*p=0.05;
**p>0.05.
BMI, body mass index; SBP, systolic blood pressure.
Table 3.
Prevalence of cardiovascular risk factors by socioeconomic characteristics among women
| Diabetes (%) | SBP (mean±SD) | Treated hypertension (%) | BMI (mean±SD) | Smoking (%) | |
|---|---|---|---|---|---|
| Age (years) | 0.000* | 0.000* | 0.005* | 0.000* | 0.000* |
| 35–44 | 8.0 | 119.3±14.6 | 70.7 | 28.1±5.3 | 3.1 |
| 45–54 | 14.4 | 129.0±19.6 | 83.0 | 29.0±5.6 | 3.4 |
| 55–64 | 22.7 | 138.9±22.6 | 83.5 | 28.9±5.5 | 5.2 |
| 65–74 | 25.6 | 142.8±22.5 | 91.4 | 27.9±5.7 | 9.0 |
| Area | 0.000* | 0.014* | 0.007* | 0.000* | 0.011* |
| Rural | 9.7 | 126.9±20.6 | 77.6 | 26.7±5.3 | 4.3 |
| Urban | 16.0 | 127.9±20.2 | 85.7 | 29.4±5.3 | 3.9 |
| Region | 0.000* | 0.000* | NS** | 0.000* | 0.000* |
| District of Tunis | 16.8 | 128.3±19.4 | 87.3 | 29.9±5.3 | 7.2 |
| North East | 10.5 | 122.9±18.8 | 86.9 | 28.2±5.3 | 3.9 |
| North West | 9.9 | 129.0±20.7 | 80.7 | 27.1±5.4 | 3.8 |
| Centre East | 16.8 | 128.5±19.9 | 74.6 | 28.8±5.1 | 1.2 |
| Centre West | 8.2 | 125.7±22.8 | 81.1 | 26.6±5.5 | 6.1 |
| South East | 17.9 | 132.5±20.2 | 92.0 | 29.0±5.8 | 0.5 |
| South West | 14.9 | 125.4±20.6 | 89.3 | 28.2±5.5 | 3.0 |
| Education | NS** | 0.000* | NS** | 0.000* | 0.000* |
| Illiterate | 14.2 | 131.6±22.2 | 82.8 | 27.7±5.4 | 4.4 |
| Primary | 15.6 | 124.8±18.2 | 87.0 | 29.6±5.5 | 2.0 |
| Secondary | 11.9 | 122.6±16.8 | 81.3 | 29.1±5.0 | 6.2 |
| High | 6.7 | 119.7±14.0 | 78.8 | 27.9±5.1 | 7.5 |
| Household economic level proxy | 0.000* | 0.008* | 0.056* | 0.000* | 0.002* |
| Low | 11.4 | 126.8±20.4 | 80.4 | 26.5±5.3 | 4.5 |
| Moderate | 14.5 | 129.2±20.9 | 81.3 | 29.3±5.4 | 3.4 |
| High | 16.0 | 126.7±19.5 | 88.4 | 29.8±5.1 | 4.3 |
| Professional activity | NS** | 0.000* | NS** | 0.000* | NS** |
| Not working/retired | 14.3 | 128.9±20.6 | 83.7 | 28.5±5.6 | 3.5 |
| Employee | 12.2 | 122.8±17.6 | 74.9 | 28.3±4.9 | 6.2 |
| Intermediate | 12.2 | 121.7±19.8 | 91.5 | 29.2±5.5 | 4.3 |
| Senior | 13.1 | 123.5±18.9 | 95.3 | 28.4±5.0 | 6.9 |
| Marital status | 0.000* | 0.000* | NS** | 0.006* | 0.000* |
| Single | 15.0 | 129.2±21.5 | 52.4 | 26.7±5.1 | 12.2 |
| Married | 12.9 | 126.7±20.0 | 84.0 | 28.5±5.4 | 3.0 |
| Divorced/widowed | 19.6 | 132.5±21.5 | 84.9 | 28.7±5.6 | 8.7 |
*p=0.05; **p>0.05.
BMI, body mass index; SBP, systolic blood pressure.
Diabetes
There were no significant differences in terms of level of education for both sexes, of marital status in men or in terms of professional activity among women.
In contrast, the prevalence of diabetes increased with age in both men and women: from 10.6% (9.0–12.3%) to 22.8% (18.5–27.3%) in men and from 8.0% (6.7–9.3%) to 25.6% (21.6–29.9%) for women aged 35–44 years compared with those aged 65 years and over.
The highest prevalence of diabetes was observed in the high household economic group: 20.1% (17.6–22.7%) of men and 16.0% (13.8–18.3%) of women with a high standard of living were diabetic.
The prevalence of diabetes was higher in urban than in rural areas. The difference according to region of residence was statistically significant in both men and women, reaching 21.5% (18.1–25.3%) in men living in East Central and 17.9% (15.1–20.9%) in women residing in South East.
Hypertension
Mean SBP increased with age in both sexes. The rise was more pronounced in women. SBP increased from 122.0±13.7 for men in the age group 35–44 years to 137.0±22.91 for the age group 65–74 years. For the same age groups, SBP increased in women from 119.35±14.7 to 142.8±22.6.
SBP was higher in urban than in rural areas, with no statistically significant differences among men. Comparing mean SBP by region showed a statistically significant difference.
A higher mean SBP was recorded among illiterate people without a professional activity and in married participants for both genders.
Among those who were aware that they had hypertension, 80.4% (75.0–85.4%) of men and 83.5% (80.3–86.5%) of women reported being treated. For both genders, the prevalence of treated hypertension increased with age: from 49.7% (31.3–68.7%) in the age group 35–44 years to 91.3% (81.7–95.6%) in the age group 65 years and older for men, and from 70.7% (57.2–81.3%) to 91.4% (85.6–95.2%) for women.
SBP was also higher in urban compared with rural areas in men (67.6% (56.5–76.4%) vs 84.8% (77.8–89.9%)) and in women (77.6% (71.7–83.0%) vs 85.7% (81.6–88.9%)). There was no statistically significant difference in the prevalence of treated hypertension according to residence area, educational level or professional activity in men and women.
The prevalence of treated hypertension was higher among those who had a high standard of living for men (87.3% (79.0–93.1%)) and for women (88.4% (82.5–92.7%)).
Single women were less likely to treat their hypertension: 52.4% (40.2–59.7%) versus 84.0% (80.2–87.1%) for married women. However, marital status was not associated with access to treatment in men.
Body mass index
Mean BMI was 25.4±4.4 kg/m² for men and 28.5±5.5 kg/m² for women. Older participants had the lowest mean BMI for both men and women.
Mean BMI was higher in urban than in rural areas in men (25.9±4.4 vs 24.4±4.2) and in women (29.4±5.3 vs 26.7±5.3). The Greater Tunis area recorded the highest mean BMI in men (26.2±4.7) and in women (29.9±5.3).
There was a significant difference in mean BMI according to the standard of living in both men and women: mean BMI increased with the standard of living of households, from 23.7±3.8 for low level to 26.9±4.4 for high level in men and from 26.5±5.3 to 29.8±5.1 in women. Senior and intermediate managers among men and women had a higher mean BMI than employees and workers and those without a professional activity.
The lowest BMI mean was recorded among illiterate men and women. It increased significantly depending on the educational level for men, from 23.9±3.8 for illiterate men to 27.0±3.8 for those who had a higher level. However, comparing mean BMI according to educational level among women showed no difference: 27.7±5.4 for no school level versus 27.9±5.1 for higher educational level.
Single men and women had the lowest BMI mean: 23.7±3.3 versus 25.5±4.3 for married men and 26.7±5.1 versus 28.5±5.4 for married women.
Smoking prevalence
Smoking prevalence was 29.4% (28.3–30.4%) with an uneven gender distribution: 55.4% (53.7–57.0%) of men and 4.0% (3.4–4.6%) of women reported smoking. Younger and older men showed a higher prevalence of smoking.
Regional inequalities were observed in men and women. Smoking prevalence was higher in the district of Tunis for women (7.2%; 5.2–9.5%) and in the North West for men (60.3%; 56.6–63.9%), and it was higher in rural than in urban areas.
Men who were more educated were less likely to smoke. Conversely, women were more likely to smoke when they reached a high level of education. Smoking prevalence was 4.4% (3.6–5.2%) for women and 55.4% (51.9–58.7%) for men who had not attended school and 7.5% (3.8–12.9%) and 43.5% (38.2–48.5%), respectively, for those who attended university.
Smoking prevalence by occupation was not significantly different in women, whereas employed men smoked more. Both single men and women had a higher prevalence of smoking (men 58.9% (49.0–68.0%) vs women 12.2% (7.5–18.8%)) as well as those with low living standards.
Global 10 year cardiovascular risk
Distribution of 10 year global cardiovascular risk
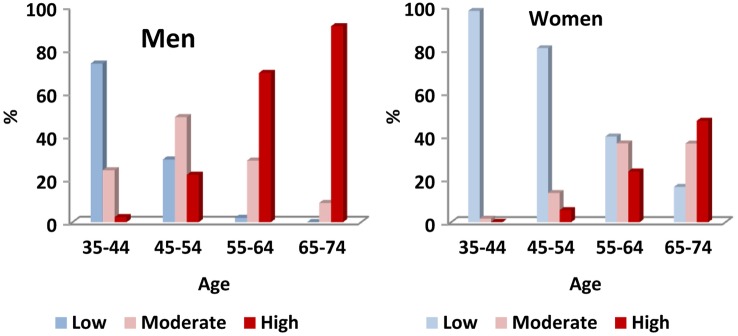
According to the Framingham equation, 18.1% (17.25–18.9%) of the study population had a high risk for a cardiovascular event in 10 years. The gender difference was marked, with 27.2% (25.7–28.7%) of men having a high risk compared with only 9.7% (8.8–10.5%) of women. As expected, the frequency of high risk was significantly increased with age in both men and women: from 2.3% (1.4–3.0%) of men aged 35–44 years to 91.1% (87.5% to 93.5%) of men aged 65 years and over. In women, the risk increased by 0.3% (0.1–0.6%) to 47.1 (42.4–51.8%) for the same age groups (figure 1).
Figure 1.
Distribution of 10 year global cardiovascular risk by age in men and women.
Spatial distribution of 10 year global cardiovascular risk
The 10 year global cardiovascular risk mean is 12% (11.8–12.4%): the national mean for men is twice that of women, 17.0 (16.5–17.5%) versus 8.48 (8.18–8.8%).
The spatial distribution of the 10 year global cardiovascular risk in Tunisian territories, divided into 24 governorates, revealed regional differences in both men and women (figure 2). In men, the mean 10 year global cardiovascular risk ranged from 15% (13.3–17.3%) in Tozeur in southern Tunisia to 21% (17.9–24.5%) in Ben Arous in the Greater Tunis area.
Figure 2.
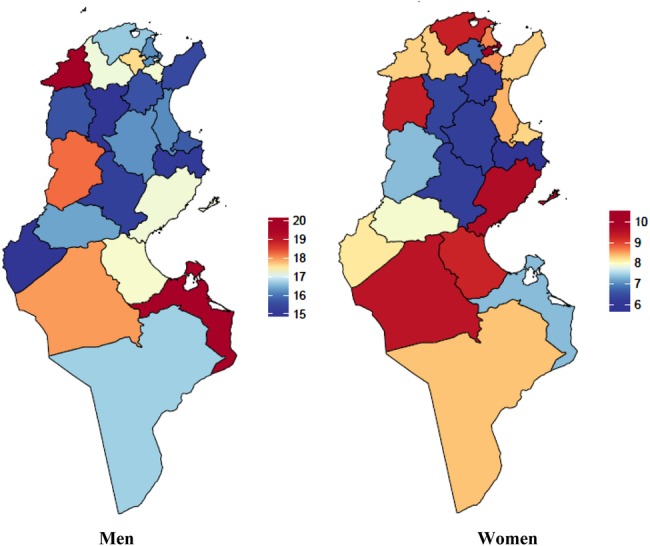
Spatial distribution of 10 year global cardiovascular risk in men and women.
In women, intra-regional variability was marked. For example, in the first region, the governorate of Manouba had a lower risk than the capital, Tunis (7.9% (6.5–9.3%) vs 11.8% (10.02–13.4)), and in the second region, Sidi Bouzid had a lower risk than Kasserine (6.0% (5.2–6.8%) vs 9.5% (7.9–10.9%)).
Socioeconomic determinants of 10-year global cardiovascular risk
Table 4 presents the results of a logistic regression of the high 10 year global cardiovascular risk depending on socioeconomic determinants of cardiovascular risk.
Table 4.
Socioeconomic determinants of 10 year global cardiovascular risk in men and women
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| OR unadjusted* | OR adjusted† | p (Wald's) | OR unadjusted* | OR adjusted† | p (Wald's) | |
| Area | <0.001 | <0.001 | ||||
| Rural | 1 | 1 | ||||
| Urban | 0.98 (0.84 to 1.14) | 1.45 (1.19 to 1.76) | <0.001 | 1.46 (1.20 to 1.79) | 1.71 (1.35 to 2.18) | <0.00 |
| Education | <0.001 | <0.00 | ||||
| Secondary or more | 1 | 1 | ||||
| Primary | 1.03 (0.84 to 1.25) | 1.27 (1.02 to 1.58) | 0.033 | 1.72 (0.96 to 3.06) | 2.34 (1.28 to 4.29) | 0.006 |
| Illiterate | 4.77 (3.91 to 5.83) | 7.09 (5.49 to 9.14) | <0.001 | 6.96 (4.12 to 11.75) | 13.57 (7.58 to 24.31) | <0.00 |
| Household economic level proxy | 0.003 | <0.001 | ||||
| Low | 1 | 1 | ||||
| Moderate | 0.93 (0.78 to 1.11) | 1.37 (1.11 to 1.70) | 0.004 | 1.19 (0.95 to 1.49) | 1.4 (1.09 to 1.79) | 0.009 |
| High | 0.73 (0.60 to 0.89) | 1.54 (1.49 to 2.14) | 0.002 | 1.25 (0.98 to 1.61) | 3.1 (2.24 to 4.27) | <0.00 |
| Professional activity | <0.001 | 0.001 | ||||
| Employee/intermediate | 1 | 1 | ||||
| Senior | 1.05 (0.88 to 1.26) | 1.19 (0.98 to 1.45) | 0.074 | 1.29 (0.64 to 2.6) | 2.1 (1.4 to 39) | 0.049 |
| Not working /Retired | 2.53 (1.92 to 3.33) | 2.05 (1.52 to 2.76) | <0.001 | 2.41 (1.62 to 3.6) | 2.15 (1.4 to 3.3) | <0.000 |
| Marital status | 0.013 | 0.001 | ||||
| Single | 1 | 1 | ||||
| Married | 1.99 (1.17 to 3.36) | 2.06 (1.18 to 3.61) | 0.011 | 1.12 (0.58 to 2.15) | 1.12 (0.57 to 2.19) | 0.745 |
| Divorced /Widowed | 2.37 (1.18 to 4.74) | 2.74 (1.31 to 5.75) | 0.008 | 3.28 (1.67 to 6.43) | 3.1 (1.55 to 6.2) | 0.001 |
OR, OR of the category relative to the reference category.
CI (p=0.95).
*Model 1: unadjusted model.
†Model 2: adjusted associations for socioeconomic factors (area of residence, educational level, economic proxy household level, professional activity and marital status).
In men, no crude association was demonstrated between high 10 year global cardiovascular risk and area of residence but by adjusting for other socioeconomic determinants (education, household economic level proxy, professional activity and marital status), the association was found (urban vs rural: OR=1.45 (1.19 to 1.76) in men and OR=1.71 (1.35 to 2.18) in women).
The association between high 10 year global cardiovascular risk and professional activity persisted after adjustment for all other variables in the model for men and women. Unemployed subjects had twice the risk of workers and intermediate managers for both sexes (OR=2.05 (1.52 to 2.76) in men and OR=2.15 (1.4 to 3.3) in women).
A high 10 year global cardiovascular risk was independently associated with marital status. Divorced and widowed women and men recorded a risk three times higher than single people (OR=2.74 (1.31 to 5.75) in men and OR=3.10 (1.55 to 6.2) in women).
Educational level was significantly associated with a high 10 year global cardiovascular risk in men and especially women. Illiterate men were at higher risk than those with secondary and higher education (OR=7.01 (5.49 to 9.14 risk)). The risk in illiterate women was more elevated (OR=13.57 (7.58 to 24.31)).
The association between 10 year global cardiovascular risk and living standards of the household showed a gradient from disadvantaged life to the most favoured level. Women with high living standards had a three times higher risk of developing a cardiovascular event in 10 years than those with low living standards (OR=3.10 (2.24 to 4.27)). In men, the OR corresponding to high standard of living was 1.54 (1.18 to 2.02) relative to the reference category (level of disadvantaged life).
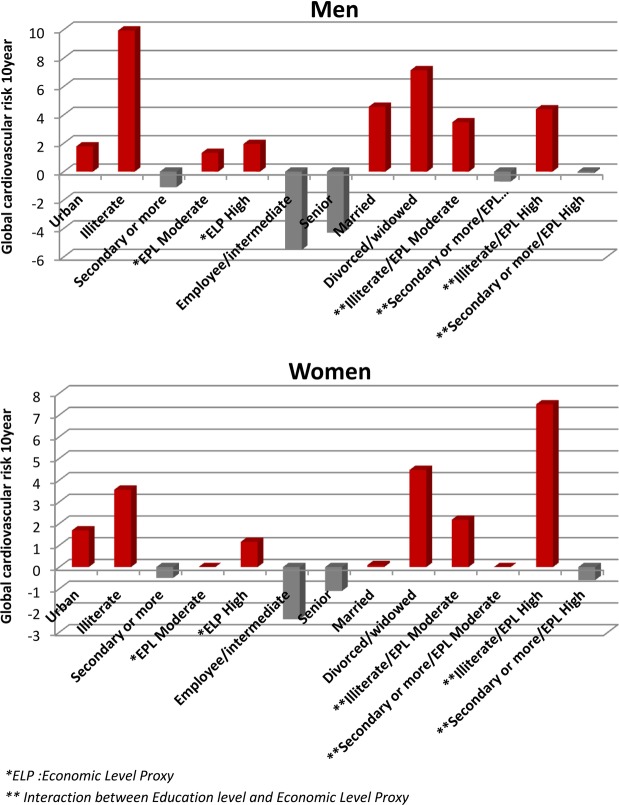
We tested the interaction between level of education and living standards of the household. The risk increased with better living standards but decreased with level of education (figure 3).
Figure 3.
Linear regression model for estimate of 10 year global cardiovascular risk by socioeconomic determinants.
Discussion
This paper reports the association between socioeconomic determinants and 10 year global cardiovascular risk in Tunisia. Our results showed that a spatial distribution of 10 year global cardiovascular risk in Tunisian territories, divided into 24 governorates, revealed regional differences in both men and women, with a higher risk in urban areas compared with rural areas. A high 10 year global cardiovascular risk was associated with social disadvantage in men and women; illiterate and divorced participants, and those without professional activity were more at risk of developing a cardiovascular event in 10 years. However, those living in a household with high living standards and in urban areas had the higher risk.
A gender inequality was very striking in our study (27.2% of men and 9.7% of women), perhaps explained by the appearance of CVD later in life for women, about 10–15 years later in women than in men,18 but still reflecting a general younger population.
This estimated percentage is close to that found in an Algerian study done in Tlemcen with 1088 subjects aged 25 years in 2008; 21.7% had a very high level risk,19 similar to some Arab Gulf countries, such as Saudi Arabia, where the prevalence of a high risk was 28.4%.20
However, this is substantially higher than the prevalence observed in European countries (8.4%).21 It is interesting to note that studies using selected populations in the region tend to show a lower risk, comparable with European levels.22 23 This is likely to reflect healthier populations or risk estimation approaches, highlighting the need for population based studies to guide policy.
Spatial distribution of 10 year global cardiovascular risk
Inter-regional differences in 10 year global cardiovascular risk in the Tunisian territories most likely reflect the role played by urbanisation, changes in lifestyles and unbalanced socioeconomic development between different regions of Tunisia. Similar to countries in the Eastern Mediterranean Region, Tunisia is facing a crucial epidemiological transition.2 However, the transition is complex, and contrasts between the regions in Tunisia are reflected through urbanisation, and demographic and socioeconomic indicators.8 24
The association between 10 year global cardiovascular risk and residence area appeared after adjusting for other socioeconomic determinants, and was more marked in men than in women.
Socioeconomic determinants of 10 year global cardiovascular risk
Substantial evidence exists for an association between poor socioeconomic conditions, such as poor housing, inadequate services, an unfavourable environment, unemployment or family breakdown, and health problems, especially CVDs.25
Our study showed an increase in 10 year global cardiovascular risk associated with social disadvantage: illiterate, unemployed and divorced men and women. These results are consistent with those reported in the literature.7 10 11
The association between education and risk of CVD has been well documented.6 26 In this study, we found that a low level of education was significantly associated with 10 year global cardiovascular risk, even after adjusting for area, occupation, marital status and living standards.
In our study, education seemed to be the most discriminating variable. The illiterate and less educated had a high risk of develop a cardiovascular event in 10 years, and this perhaps suggests a major future role for health and overall education to improve health outcomes.
However, this also might be linked to overall living standards, a key social determinant of health. It affects the habits and behaviours related to health, such as quality of food, level of physical activity, smoking and excessive alcohol consumption.27 Contrary to some studies,25 26 our study showed that high living standards were associated with a high level of 10 year global cardiovascular risk, consistent with Boutahiri,22 suggesting that obesity is a key risk factor in the Tunisian population.
Unemployment and family stability might have an important role in determining health behaviours in our population, by contributing to the living standards of the household but also increasing stress levels.25 28 Our results are consistent with these observations.
Strengths and limitations of the study
This study is one of the few population based, representative and large studies addressing the association between socioeconomic status and CVD in the Mediterranean region, and particularly in North Africa.
The study was conducted using standardised methodology and showed a very high response rate.
However, our study has some limitations. Our study was based on a cross sectional survey which limits the causal interpretation of observed associations and also the dynamic and/or life course perspective of risk factors.
Despite the high response rate, selection bias was unavoidable as the investigation takes place in households which leads to greater involuntary recruitment of women and older persons.
Our decision to use the non-laboratory version of the Framingham risk score might have resulted in misclassification of CVD risk. However, as in most large scale studies in countries with low resources, laboratory blood tests are difficult—glucose measurements were made by a capillary blood glucose reader and there were no total cholesterol or high density lipoprotein measurements.
This score used the same risk factors as the ‘laboratory’ Framingham except for the lipid tests (total cholesterol and high density lipoprotein) which were replaced by BMI. This method was originally designed to be used in settings with limited resources.29 Pandya et al30 showed excellent agreement between the Framingham risk characterisation using the ‘laboratory’ and ‘non-laboratory’ models. Although this score has not been calibrated in the Tunisian population, our estimates were critically appraised by Tunisian experts in risk estimation.
Finally, it is possible that there were misclassification of standards of living as households generally do not want to declare possession of certain goods and services.
Public health implications
In Tunisia, the importance of NCDs and their impact were well recognised early in the 1990s. National programmes for hypertension and diabetes were developed, and an NCD Management Unit was established within the Department of Primary Healthcare. The first strategic document on CVD was produced in 1999; a strategy on obesity and tobacco prevention and control has developed within this context.31 32 These came together in a 2010–2014 Action Plan on NCD Prevention and Control.33
However, the health system which theoretically recognises the challenge of CVD, in reality faces several problems in meeting these challenges.
Our study assessed 10 year global cardiovascular risk in the Tunisian population using population based data, and thus provides insights on what would be the future burden of these diseases in the next decade. It also highlighted the powerful socioeconomic determinants of the 10 year global cardiovascular risk.
The high level of global cardiovascular risk in the next 10 years in the Tunisian population requires a comprehensive approach, including the development of a strategy for high risk individuals supported by a collective, population wide strategy. Such strategies include smoke free legislation and healthier food, reinforced by education, information and awareness through campaigns against certain behaviours and habits that threaten health, such as alcohol consumption, smoking and physical inactivity, and campaigns on dietary lifestyle.34 All of these actions would be aimed at primary prevention, especially among young people, and secondary prevention in patients with clinical disease.
The individual and collective preventive strategies are complementary and necessary. However, this comprehensive prevention approach can only be undertaken with the assistance and support of health and political authorities. Particular attention should be given to socially disadvantaged populations, and regional development should be improved in order to reduce future health inequalities.
Conclusions
The Tunisian population has a high proportion of individuals with a high 10 year global cardiovascular risk, particularly concentrated in the most disadvantage members of society. Both structural and targeted interventions, particularly to disadvantaged groups, will be needed to reduce the growing burden of CVD and its social inequalities.
Acknowledgments
We thank Professor Simon Capwell for his comments on this work. We also thank Professor Pascal Astagneau and all of the professors of the Master of Public Health at the University of Pierre and Marie Curie, Paris, for their encouragement.
Footnotes
Contributors: OS, DM and HBR conceived the idea of the study. HAS, LB, OS, NBM and HBR assembled the datasets. OS, DM, NBM, HBR, HAS, LB and MO wrote the first draft of the paper, and finalised the manuscript. All authors contributed to the analysis, intellectual content and critical revisions of the drafts of the paper, and approved the final version. HBR is the guarantor.
Funding: The study was funded by the European Community's Framework Programme under grant agreement ICA3-CT-2002-1001. The study was also supported by the Tunisian Ministry High Education and Research and Ministry of Health. The research was funded by the European Union (INCO: Med Projects 1998–2002, TAHINA: Epidemiological Transition And Health Impact in North Africa—contract No: ICA3-CT-2002-10011) and supported by the Cardiovascular Epidemiology and Prevention Research Laboratory, Faculty of Medicine of Tunis, University of Tunis El Manar.
Competing interests: None declared.
Ethics approval: The study protocol was carried out according to the Declaration of Helsinki and was approved by the Tunisian Ministry of Health and the Tunisian National Council of Statistics (visa No 5/2005).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.National Institute of Statistics. Yearly Statistics Report No 55. National Institute of Statistics: Tunisia, 2012. [Google Scholar]
- 2.Ben Romdhane H, Khaldi R, Oueslati A et al. . Transition épidémiologique et transition alimentaire et nutritionnelle en Tunisie. Options Méditerranéennes 2002;41:278. [Google Scholar]
- 3.National Public Health Institute. Deaths registry. Tunisia, 2013. http://www.insp.rns.tn/index.php?option=com_content&view=section&id=26&Itemid=224 [Google Scholar]
- 4.Saidi O, Ben Mansour N, O'Flaherty M et al. . Analyzing recent coronary heart disease mortality trends in Tunisia between 1997 and 2009. PLoS ONE 2013;8:e63202 10.1371/journal.pone.0063202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ben Romdhane H. Coronary heart diseases: the epidemic and its determinants. In: vol I: the risk factors Tunis: National Public Health Institute Press, 2001. [Google Scholar]
- 6.Elasmi M, Feki M, SenHoji H et al. . Prévalence des facteurs de risque cardiovasculaires conventionnels dans la population du grand Tunis. Rev Epidemiol Sante Publique 2009;57:92–87. [DOI] [PubMed] [Google Scholar]
- 7.Ezzati M, Hoorn SV, Lawes CM et al. . Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med 2005;2:e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ben Romdhane H, Grenier FR. Social determinants of health in Tunisia: the case-analysis of Ariana. Int J Equity Health 2009;8:9 10.1186/1475-9276-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boutayeb A, Helmert U. Social inequalities, regional disparities and health inequity in North African countries. Int J Equity Health 2011;10:23 10.1186/1475-9276-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ben Alaya N, Ben Romdhane H, Delpeuch F. Modèle causal des cardiopathies ischémiques en Tunisie. Options Méditerranéennes Série B: Etudes et Recherches 2002;41. [Google Scholar]
- 11.Kreatsoulas C, Anand S. The impact of social determinants on cardiovascular disease. Can J Cardiol 2010;26(Suppl C):8C–13C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute of Statistics. Main indicators of Census (2014). National Institute of Statistics: Tunisia, 2015. [Google Scholar]
- 13.The Framingham Heart Study. General cardiovascular disease (10 year risk). http://www.framinghamheartstudy.org/risk/gencardio.html#
- 14.Blacher J, Agnoletti D. Echelle de risque cardiovasculaire. Médecine des maladies métaboliques 2011;5:287–93. [Google Scholar]
- 15.Institut National de la Statistique. Enquête nationale sur l'emploi 2005.
- 16.Buuren SV, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R. J Stat Software 2011;45 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 17.Cicognani M, Berchtold A. Imputation des données manquantes: Comparaison de différentes approches. 42èmes Journées de Statistique 2010.
- 18.Stangl V, Baumann G, Stangl K. Coronary atherogenic risk factors in women. Eur Heart J 2002;23:1738–52. [DOI] [PubMed] [Google Scholar]
- 19.Y Berrouiguet A, Benyoucef M, Meguenni K et al. . Enquête sur la prévalence des facteurs de risque de maladies cardiovasculaires à Tlemcen (Algérie). Médecine des maladies métaboliques 2009;3:313–19. [Google Scholar]
- 20.Baynouna LM, Revel AD, Nagelkerke NJ et al. . High prevalence of the cardiovascular risk factors in Al Ain, United Arab Emirates. Saudi Med J 2008;29:1173–8. [PubMed] [Google Scholar]
- 21.Maiques Galán A, Antón García F, FranchTaix M et al. . Cardiovascular risk of SCORE compared to Framingham: consequences of the change proposed by the European Societies. Med Clin (Barc) 2004;123:681–5. 10.1016/S0025-7753(04)75330-0 [DOI] [PubMed] [Google Scholar]
- 22.Boutahiri N.2011. Estimation du risque cardiovasculaire chez le personnel de l'hôpital régional Mohammed V de Meknes (à propos de 512 cas) http://scolarite.fmp-usmba.ac.ma/cdim/mediatheque/e_theses/32-11.pdf.
- 23.Elasmi M, Mebazaa A, Zidi W et al. . Framingham risk score for coronary heart disease is elevated in Tunisian psoriatic patients. Arch Cardiovasc Dis Suppl 2012;4:100–3. [Google Scholar]
- 24.Ben Romdhane H, Haouala H, Belhani A et al. . Epidemiological transition in Tunisia: its determinants and health impact. Tunis Med 2005;83:1–7. [PubMed] [Google Scholar]
- 25.Wilkinson R, Marmot M. Les déterminants sociaux de la santé: les faits. OMS 2004, Deuxième édition.
- 26.Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health 2011;32:39–69. 10.1146/annurev-publhealth-031210-101234 [DOI] [PubMed] [Google Scholar]
- 27.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 1993;88:1973–98. [DOI] [PubMed] [Google Scholar]
- 28.David Locker: Social determinants of health and disease. (http://www.elsevierhealth.com/media/us/samplechapters/9780702029011/9780702029011.pdf)
- 29.Bitton A, Gaziano TA. The Framingham heart study's impact on global risk. Prog Cardiovasc Dis 2010;53:68–78. 10.1016/j.pcad.2010.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandya A, Weinstein MC, Gaziano TA. A comparative assessment of non-laboratory-based versus commonly used laboratory-based cardiovascular disease risk scores in the NHANES III population. PLoS ONE 2011;6:e20416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Direction Des Soins De Santé De Base. Le programme national de lutte anti tabagique: Réalités et perspectives. Direction Des Soins De Santé De Base: Tunis, 2009. [Google Scholar]
- 32.Institut National de Nutrition et de Technologie Alimentaire. Stratégie Nationale de Prévention et de Lutte contre l'Obésité. Institut National de Nutrition et de Technologie Alimentaire: Tunis, 2010. [Google Scholar]
- 33.World Health Organization. Country Cooperation Strategy for WHO and Tunisia 2010–2014 2010. http://www.who.int/countryfocus/cooperation_strategy/ccs_tun_en.pdf
- 34.Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med 2010;7:e1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2015-009195supp_appendix.pdf (218.8KB, pdf)