Abstract
Background
To examine the trends in activities of daily living (ADL) disability in older Chinese adults in Hong Kong between 2001 and 2012.
Methods
Using data from the Elderly Health Centres (EHCs) of the Department of Health comprising a total of 54 808 community-dwelling Chinese adults aged ≥65 years in 1 early cohort (1904–1917) and 10 3-year birth cohorts (1918–1920, 1921–1923, 1924–1926, 1927–1929, 1930–1932, 1933–1935, 1936–1938, 1939–1941, 1942–1944, 1945–1947), we examined trends in ADL disability by using age-period-cohort (APC) models. ADL disability was defined as being unable to perform at least 1 of 7 ADL activities (bathing, dressing, toileting, transferring, feeding, grooming, walking) independently. Cross-classified random-effects logistic regressions were performed for each of the APC trends with adjustment for age, period, cohort, sociodemographic, lifestyle, comorbidity and self-rated health.
Results
The mean age of the cohort was 70.9±4.7 (range 65–99) years. The prevalence rate of ADL disability was 1.6%. ADL disability increased with age (p<0.001) and the gradient of the increase was steeper in the older age groups. At the same age, women (1.7%) were more likely to report ADL disability than men (1.4%, p=0.001). For both genders, there was an increase in ADL disability between 2003 and 2012; adjustment for age, cohort and other covariates has diminished the trends observed among men. There was no cohort effect in ADL disability.
Conclusions
ADL disability in older adults has increased over the last decade. Further study is required to identify possible causes behind the disability trends.
Keywords: Ageing, Activities of Daily Living Disability, Age-Period-Cohort Analysis, Chinese
Strengths and limitations of this study.
The surveys were population-based, which provide an updated examination of disability trends among Chinese adults in Hong Kong aged 65 years and older.
This study includes the adjustment for multiple potential cofounders, including sociodemographic characteristics, lifestyle factors, comorbidities as well as self-rated health, which are known to influence functional status.
The surveys ended in the birth cohort 1947. Therefore, we were unable to examine the cohort differences on disability between prewar generations and postwar baby boomers, whose early-life and mid-life experiences were remarkably different from each other.
Information on birth place or risk factors in early-life and mid-life that may affect disability at older ages was not available, limiting the ability to identify causes of the increased disability burden in late life.
Finally, our results only apply to the community-dwelling elderly. Disability prevalence in institutions tends to be higher than that in the community.
Introduction
Life expectancy at birth of Hong Kong has taken one of the world's leading positions and reached 81.2 years in men and 86.9 years in women in 2014.1 The lengthening of life, however, does not mean that Hong Kong people have years of life with better health and independency. Therefore, concern has emerged about whether the increase in life expectancy will be associated with more disability and higher demand for medical and long-term care services.
The examination of the trends in late-life disability is important, both in the context of the ageing population and because disability has a wide-ranging impact on health and social care systems. Substantial epidemiological studies have shown that the proportion of age-specific disability has been decreasing in recent years;2–4 however, other studies have reported a flat5–8 or a contrary pattern indicating that late-life disability has been increasing.9–11 Aside from the period-based trend studies, very few studies examining the disability prevalence have adjusted for cohort effects. Cohort effects reflect changes applicable to individuals born at a specific time, which is an important dimension for understanding the change of population health over time.
Not until recently, an increasing number of studies have now investigated the existence of cohort differences in the trends in late-life disability. An analysis of data from the National Health and Nutrition Examination Survey (NHANES) demonstrated a significantly higher activities of daily living (ADL) limitation, instrumental ADL limitation and impaired mobility among those aged 60–69 years interviewed in 1999–2004 than their counterparts interviewed in the 1988–1994 survey.12 Another US study showed that newer cohorts of older adults became more disabled, controlling for ageing and period effects.13 A recent analysis of older adults provided further evidence about the cohort effects on disability in older adults across different countries.14 For example, in the USA, the levels of ADL disability steadily increased in the cohorts born between 1916 and 1935, and fell thereafter until measured in people born in 1952, and increased again in the cohorts born between 1952 and 1954.15 In England, the levels of ADL disability remained constant in the cohorts born in the 1920s and rose in the cohorts born between 1944 and 1946.16 A smaller study in Brazil suggested recent cohorts born between 1927 and 1937 had better physical functioning compared with their older counterparts born between 1916 and 1926.17
As far as we are aware, no such study examining the trends in ADL disability in older Chinese people has been undertaken in Hong Kong; therefore, it is necessary to explicate these trends as shown in other health studies. Using data from a large population-based sample of older population of Hong Kong (born between 1904 and 1947) collected between 2001 and 2012, this study examines the trends in ADL disability among older Chinese adults aged 65 years and above using age-period-cohort (APC) models.
Methods
Data source and study population
We used data from the Elderly Health Centres (EHCs) of the Department of Health, which started to collect longitudinal health data from a large population-based cohort in Hong Kong since 1998. Eighteen EHCs have been established to deliver health examinations and primary care services for older adults. All residents of Hong Kong aged 65 years and older can voluntarily enrol. Enrolees in the cohort received standard medical examinations at baseline and were encouraged to have the reassessment every subsequent year. Enrolees found to have health problems would be referred to appropriate specialists for further management. As of 2014, the cohort consisted of ∼140 000 older adults. The details of this cohort have been described elsewhere.18 In this study, we retrieved all baseline data from the EHCs of individuals who were first enrolled between 2001 and 2012, and excluded those who were institutionalised (n=589) and those with missing data on living arrangement (n=2) and ADL disability (n=293). The final sample consisted of 54 808 individuals (19 923 men (36.4%) and 34 885 women (63.6%) with a mean age of 70.9 years (range 65–99 years). The EHCs cohort had higher proportions of young–old (aged 65–74 years) than that in the general population; otherwise, it closely matched the general elderly population of Hong Kong, as there was no significant difference in terms of sociodemographic characteristics (eg, gender, marital status, educational level, employment status, type of housing), lifestyle (eg, smoking) and self-rated health between individuals attending assessments in EHCs and the population as a whole as described in the 2006 and 2011 Hong Kong censuses (table 1).19–24
Table 1.
Comparison of the characteristics between the Elderly Health Centre cohort and the age-matched general populations
| Elderly Health Centre cohort (2001–2012) |
Age-matched Hong Kong general population (2006) |
Age-matched Hong Kong general population (2011) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Total | Men | Women | Total | Men | Women | Total | |
| Persons (number) | 19 923 | 34 885 | 54 808 | 393 412 | 459 384 | 852 796 | 438 257 | 503 055 | 941 312 |
| Age group (years) | |||||||||
| 65–69 | 40.7 | 53.0 | 48.5 | 31.7 | 25.2 | 28.2 | 27.7 | 22.4 | 24.9 |
| 70–74 | 35.6 | 29.3 | 31.6 | 28.6 | 25.4 | 26.9 | 26.6 | 22.6 | 24.5 |
| 75–79 | 16.5 | 12.4 | 13.9 | 21.0 | 20.9 | 21.0 | 22.1 | 21.5 | 21.8 |
| 80–84 | 5.7 | 4.1 | 4.7 | 11.4 | 14.8 | 13.2 | 14.2 | 16.6 | 15.5 |
| ≥85 | 1.5 | 1.3 | 1.4 | 7.3 | 13.6 | 10.7 | 9.3 | 16.8 | 13.3 |
| Cohen effect size* | 0.36 | 0.73 | 0.56 | 0.47 | 0.84 | 0.67 | |||
| Gender | |||||||||
| Men | .. | .. | 36.4 | .. | .. | 47.7 | .. | .. | 46.7 |
| Women | .. | .. | 63.6 | .. | .. | 52.3 | .. | .. | 53.3 |
| Cohen effect size* | 0.23 | 0.21 | |||||||
| Marital status | |||||||||
| Never married | 2.7 | 2.5 | 2.6 | 4.8 | 2.9 | 3.7 | 4.1 | 2.6 | 3.3 |
| Married | 88.7 | 56.9 | 68.4 | 79.8 | 46.4 | 61.8 | 81.5 | 45.7 | 62.4 |
| Widowed/separated/divorced/others | 8.6 | 40.6 | 29.0 | 15.4 | 50.7 | 34.6 | 14.4 | 51.7 | 34.3 |
| Cohen effect size* | 0.22 | 0.21 | 0.14 | 0.19 | 0.23 | 0.12 | |||
| Educational level | |||||||||
| Primary or below | 53.9 | 76.0 | 68.0 | 64.8 | 83.8 | 75.0 | 58.3 | 78.3 | 69.0 |
| Secondary and above | 46.1 | 24.0 | 32.0 | 35.2 | 16.2 | 25.0 | 41.7 | 21.7 | 31.0 |
| Cohen effect size* | 0.23 | 0.21 | 0.16 | 0.09 | 0.06 | 0.02 | |||
| Employment status | |||||||||
| Unemployed/retired/home-makers/others | 90.6 | 97.2 | 94.8 | NA | NA | 93.0 | NA | NA | 93.2 |
| Working (full-time or part-time) | 9.4 | 2.8 | 5.2 | NA | NA | 7.0 | NA | NA | 6.8 |
| Cohen effect size* | 0.07 | 0.06 | |||||||
| Type of housing | |||||||||
| Public and subsidised housing | 45.3 | 47.4 | 46.6 | NA | NA | 57.7 | NA | NA | 56.2 |
| Private housing (rented or self-owned) | 53.4 | 51.2 | 52.0 | NA | NA | 41.3 | NA | NA | 42.8 |
| Others (excluding institutions) | 1.2 | 1.4 | 1.4 | NA | NA | 1.0 | NA | NA | 1.1 |
| Cohen effect size* | 0.23 | 0.19 | |||||||
| Smoking† | |||||||||
| Non-smoker | 42.8 | 93.6 | 75.1 | ||||||
| Ex-smoker | 42.3 | 4.6 | 18.3 | {75.8} | {97.0} | {86.8} | {82.9} | {98.2} | {90.8} |
| Current smoker | 14.9 | 1.9 | 6.6 | 24.2 | 3.0 | 13.2 | 17.1 | 1.8 | 9.2 |
| Cohen effect size* | 0.22 | 0.06 | 0.19 | 0.06 | 0.01 | 0.09 | |||
| Self-rated health‡ | |||||||||
| Better | 6.7 | 7.0 | 6.9 | NA | NA | 5.5 | NA | NA | 2.8 |
| More or less the same | 62.5 | 56.6 | 58.7 | NA | NA | 61.4 | NA | NA | 65.8 |
| Worse | 30.7 | 36.4 | 34.3 | NA | NA | 33.1 | NA | NA | 31.4 |
| Cohen effect size* | 0.07 | 0.27 | |||||||
Unless otherwise indicated, figures reported in columns refer to the percentage of population.
Percentages may not total 100 due to rounding of figures.
*Cohen effect sizes have three levels: 0.1 for small, 0.3 for medium and 0.5 for large.36
†Figures were collected from two thematic household surveys in 2005 and 2010, respectively, which covered those aged 60 years and above. Current smokers refer to daily cigarette smokers in the Thematic Household Surveys; non-current smoker are represented in figures following the curly brackets.
‡Figures were collected from two thematic household surveys in 2005/2006 and 2009/2010, respectively.
.., not applicable; NA, not available.
Variables
ADL disability
A modified version of the Katz Index of Independence in ADL was used to measure ADL disability.25 Respondents reported whether they needed (1) no help, (2) partial help or (3) were unable to do five of the six activities in the Katz ADL including bathing, dressing, toileting, transferring from a bed to a chair and feeding. Incontinence was not included because it may be present in individuals who otherwise display no disability.26–28 Two additional activities, used by Branch et al,29 were also assessed: grooming and ability to walk across a small room. The number of activities that respondents reported as needing help or being unable to perform was calculated for each evaluation. Total possible scores of the ADL scale range from 7 to 21. ADL disability was defined as being unable to perform at least one of seven ADL independently (ie, a score >7 indicates ADL disability).
Independent variables
The main independent variables in this study were age, period and cohort. Age was treated as a continuous variable. The top-coded age for 2001–2012 was 99 years. Period indicates the year in which the respondent was interviewed. It ranges from 2001 to 2012. Birth cohort was estimated by subtracting age from period and we subsequently grouped these cohorts into 3-year cohort bands to break the linear dependence among the APC dimensions, known in demographic research as the identification problem. Individuals born between 1904 and 1917 were merged into the birth cohort of those born in 1917, taking into account the gender-specific distribution of birth year for the total number of men and women in the study. We also adjusted for respondents' sociodemographic characteristics including marital status (never married, married, widowed/separated/divorced/others), educational level (primary or below, secondary and above), employment status (working full-time/part-time, unemployed/retired/home-makers/others) and type of housing (public and subsidised housing, private housing, others), lifestyle factors including physical exercise (no exercise at all, exercise at least once per week), smoking (non-smoker, ex-smoker, current smoker) and alcohol intake (non-regular drinker and regular drinker (current drinkers who were drinking 4 days or more per week)), comorbidities including body mass index (BMI, kg/m2) and the number of prescribed medications (none, 1–4 items, ≥5 items) as well as self-rated heath (compared with 1 year ago; better, more or less the same, worse).
Analysis
Consistency check and data standardisation were performed prior to data analysis. Data were presented in 1 early cohort (1904–1917) and 10 3-year birth cohorts (ie, 1918–1920, 1921–1923, 1924–1926, 1927–1929, 1930–1932, 1933–1935, 1936–1938, 1939–1941, 1942–1944, 1945–1947). To calculate the prevalence rates for ADL disability, we used a numerator consisting of the number of individuals who reported a limitation at a given time point and a denominator as the total population at that time. To examine the trends by APC, cross-classified random-effects logistic regression models for ADL disability were fitted separately for men and women. ADL disability was dichotomised into a categorical variable for ADL disability (ADL score >7). We used validated BMI values by examining the range of values for BMI and excluded non-physiological values: BMI<10 or >60 kg/m2. Prior to model fitting, age and BMI were standardised to have a mean of 0 and a SD of 1. Furthermore, BMI with non-physiological values identified earlier were replaced with the value 0, and missing values for the other categorical covariates were imputed using the most common category. In each regression model, the ADL disability was regressed on age in linear and squared terms and covariates including sociodemographic (ie, marital status, educational level, employment status, type of housing), lifestyle (ie, physical exercise, smoking, alcohol intake), comorbidity (BMI, number of prescribed medications) and self-rated health in the fixed-effect portion of the model. We also specified the random intercept for each period (3-year band) and cohort (3-year band) with the exception of the initial oldest cohort (1904–1917), which covered a broader range of years to ensure a sufficient number of participants. In addition, the predicted probabilities of ADL disability for our models were calculated separately and plotted for each APC dimension and for both genders. The estimated probability of ADL disability for a particular age, birth cohort and period was obtained by substituting the age, birth cohort and period of interest into the fitted logistics regression model and applying the inverse logistic transformation. For example, for the unadjusted APC model with combined gender, the black lines for age (figure 1A), period (figure 1B) and cohort (figure 1C) are, respectively, created by the following formulas:
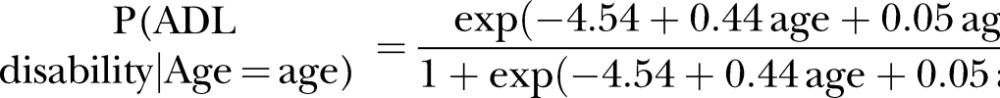 |
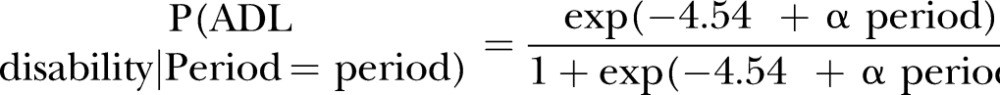 |
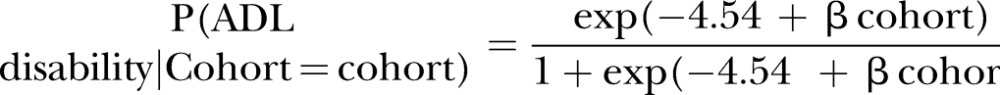 |
Here, −4.54 is the estimated intercept term, 0.44 is the estimated coefficient for the age term, 0.05 is the estimated coefficient for the squared age term, α period is the estimated coefficient for the particular period effect and β cohort is the estimated coefficient for the particular cohort effect. All analyses were carried out using the Window-based SPSS Statistical Package (V.21.0; SPSS, Chicago, Illinois, USA) and p values <0.05 were considered statistically significant.
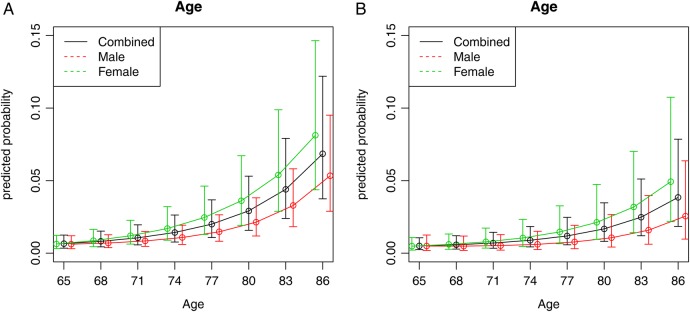
Figure 1.
(A) Unadjusted age trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. (B) Adjusted age trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. The model was adjusted for period, cohort, marital status, educational level, employment status, type of housing, physical exercise, smoking, alcohol intake, BMI, number of prescribed medications and self-rated health. ADL, activities of daily living; BMI, body mass index.
Results
Table 2 shows the characteristics of the study population by gender. The mean age of cohort at the time of study was 70.9±4.7 years (range 65–99 years). The prevalence rate of ADL disability was 1.6% (data not shown). Women (1.7%) were more likely to report ADL disability than men (1.4%, p=0.001).
Table 2.
Characteristics of study population by gender (n=54 808)
| Mean±SD/n (%) |
|||
|---|---|---|---|
| Men (n=19 923) | Women (n=34 885) | p Value | |
| Age (years) | 71.6±4.7 | 70.5±4.6 | <0.001 |
| Age group (years) | |||
| 65–69 | 8112 (40.7) | 18 476 (53.0) | <0.001 |
| 70–74 | 7086 (35.6) | 10 208 (29.3) | |
| 75–79 | 3278 (16.5) | 4338 (12.4) | |
| 80–84 | 1145 (5.7) | 1419 (4.1) | |
| ≥85 | 302 (1.5) | 444 (1.3) | |
| Marital status | |||
| Never married | 531 (2.7) | 869 (2.5) | <0.001 |
| Married | 17 677 (88.7) | 19 838 (56.9) | |
| Widowed/separated/divorced/others | 1715 (8.6) | 14 178 (40.6) | |
| Educational level* | |||
| Primary or below | 10 736 (53.9) | 26 505 (76.0) | <0.001 |
| Secondary and above | 9183 (46.1) | 8371 (24.0) | |
| Employment status | |||
| Unemployed/retired/home-makers/others | 18 055 (90.6) | 33 909 (97.2) | <0.001 |
| Working (full-time and part-time) | 1868 (9.4) | 976 (2.8) | |
| Type of housing | |||
| Public and subsidised housing | 9035 (45.3) | 16 522 (47.4) | <0.001 |
| Private housing (rented or self-owned) | 10 647 (53.4) | 17 864 (51.2) | |
| Others (excluding institutions) | 241 (1.2) | 499 (1.4) | |
| Physical exercise* | |||
| No exercise | 2015 (10.1) | 3505 (10.0) | 0.817 |
| Regular exercise | 17 907 (89.9) | 31 375 (90.0) | |
| Smoking* | |||
| Non-smoker | 8530 (42.8) | 32 629 (93.5) | <0.001 |
| Ex-smoker | 8421 (42.3) | 1588 (4.6) | |
| Current smoker | 2967 (14.9) | 657 (1.9) | |
| Alcohol intake | |||
| Non-regular drinker | 18 407 (92.4) | 34 595 (99.2) | <0.001 |
| Regular drinker | 1516 (7.6) | 290 (0.8) | |
| BMI, kg/m2* | 23.8±3.2 | 24.1±3.5 | <0.001 |
| Number of prescribed medications* | |||
| No use of drug | 8874 (44.6) | 15 546 (44.6) | <0.001 |
| 1–4 items | 9524 (47.8) | 17 218 (49.3) | |
| ≥5 items | 1523 (7.6) | 2 120 (6.1) | |
| Self-rated health* | |||
| Better | 1342 (6.7) | 2453 (7.0) | <0.001 |
| More or less the same | 12 447 (62.5) | 19 718 (56.6) | |
| Worse | 6122 (30.7) | 12 680 (36.4) | |
| ADL disability | 270 (1.4) | 609 (1.7) | 0.001 |
Percentages may not total 100 due to rounding of figures.
P values were obtained by χ2 test for categorical variables/independent sample t-test for continuous variables.
*Missing data in education (n=13), physical exercise (n=6), smoking (n=16), BMI (n=38), number of prescribed medications (n=3) and self-rated health (n=46).
ADL, activities of daily living; BMI, body mass index.
Figure 1A shows the unadjusted age trends of predicted probabilities for ADL disability. CIs for the trend are also shown. The unadjusted predicted probability of ADL disability increased continually with age. The increase was more prominent among the older age group as shown by the steeper slope of the lines. Women had higher predicted probability of having ADL disability than men. The disability gap between women and men have widened overtime. With adjustment for sociodemographic characteristics, lifestyle factors, comorbidities and self-rated health, the trends were becoming less disabled but remained significant (figure 1B).
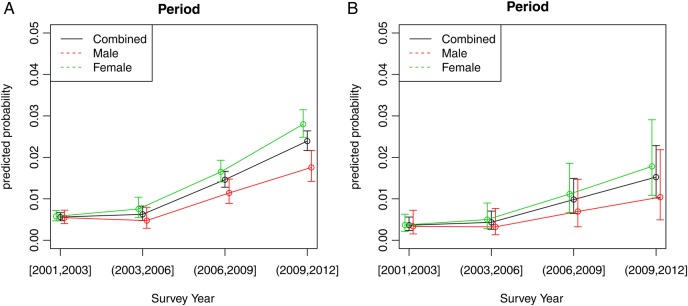
Figure 2A shows the unadjusted period-based trends for ADL disability. A relatively flat trend was observed between 2001 and 2003, followed by an increasing trend from 2003 to 2012. The increase in ADL disability was more pronounced among women than among men. After adjustment for sociodemographic characteristics, lifestyle factors, comorbidities and self-rated health, the upward trends from 2003 to 2012 appeared to have diminished but remained significant, but not among men (figure 2B).
Figure 2.
(A) Unadjusted period trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. (B) Adjusted period trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. The model was adjusted for age, cohort, marital status, educational level, employment status, type of housing, physical exercise, smoking, alcohol intake, BMI, number of prescribed medications and self-rated health. ADL, activities of daily living; BMI, body mass index.
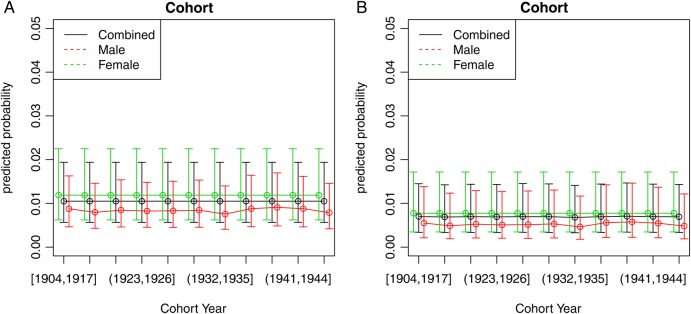
In contrast, the unadjusted and adjusted cohort-based trends of ADL disability were essentially flat and the trends were similar for men and women (figure 3A, B).
Figure 3.
(A) Unadjusted cohort trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. (B) Adjusted cohort trends of ADL disability among Chinese adults aged 65–99 years, with 95% CIs, Elderly Health Centres 2001–2012. The model was adjusted for age, period, marital status, educational level, employment status, type of housing, physical exercise, smoking, alcohol intake, BMI, number of prescribed medications and self-rated health. ADL, activities of daily living; BMI, body mass index.
Discussion
This is the first analysis using data collected from the EHCs to examine the APC effects on ADL disability among community-dwelling older Chinese adults in Hong Kong. Our findings show that disability increased with age and the increase was more prominent among the older age group. Furthermore, women have a higher predicted probability of having ADL disability compared with men, reflecting that they live more years of life with more disability. For both genders, there was an increasing trend in ADL disability between 2003 and 2012. However, there was no cohort effect in ADL disability.
In comparison to the National Health Interview Survey (NHIS) among older adults aged 70 years and older,13 we did not find a stable trend in ADL disability between 2001 and 2009 as the trend that we observed have remained more or less constant between 2001 and 2003, and appeared to have increased between 2003 and 2012. The increased disability we observed between 2003 and 2012 may reflect better survival in very frail individuals with multiple conditions and comorbidities across successive survey years during the study period. According to the Census and Statistics Department of Hong Kong, while the age-specific and gender-specific mortality rates for both genders and all age groups were decreasing continuously from 2003 to 2012,30 there was an increasing trend in chronic diseases from 2007 to 2013.31 Similarly, among the EHCs cohort, the proportion of older adults reporting four or more chronic diseases increased from 4.9% in 2003 to 8.9% in 2012 (data not shown). The increasing trend between 2003 and 2012 may also reflect the growing long-term care demand. This is supported by the increasing trends in waiting time for admission to subsidised residential care homes for the elderly.32 Thus, it may be that individuals with disability who would have lived in institutions a decade or two ago now lived in the community, and were captured in the EHC cohort.
Unlike the period-based disability trends, for both genders, the cohort-based trends were essentially flat. In comparison to the NHANES among older Americans aged 60–69 years,12 we did not find an increase in ADL disability in recent cohorts between 1930 and 1944 as the ADL disability trends remained more or less constant among the entire elderly cohorts born between 1904 and 1947. However, that study only compared disability rates among older adults between two aggregated NHANES periods (1988–1994 vs 1999–2004). Our results were also inconsistent when compared with NHIS, another US study among a much broader spectrum of elderly cohorts, which demonstrated a moderately increased trend in ADL over successive birth cohorts born between 1885 and 1935;13 or a series of analyses of data from the Health and Retirement Study (HRS) of people aged 50 years and older, which have reported increases in ADL disability across consecutive cohorts born between 1916 and 1935.15 The US obesity epidemic has been suggested to explain the increase in disability rate across successive cohorts.13 However, the author of NHIS reported that BMI did not account for the cohort-based increase and concluded that the upward cohort trends in ADL disability remained unexplained.12 Alternatively, selective survival effect may help explain the healthy cohort effects in disability in older cohorts because the older cohorts, who have survived a variety of hardships or historical contexts yet who were still able to walk in for the assessments have to be more fit, with better capacity to undertake the physically demanding tasks (eg, agricultural work) and hence better ADL. However, since the majority of our participants were born during/before the Chinese Civil War, the Second Sino-Japanese War or the Cultural Revolution/Pacific War (ie, prewar generations) and moved from China to Hong Kong during their young adulthood; the relatively homogeneous characteristics of this cohort may mask differences in trends in ADL disability.
In contrast, our results are consistent with the findings reported in the Survey of Health, Ageing and Retirement in Europe study (SHARE)16 and the English Longitudinal Study of Ageing (ELSA) in England,33 whereas the levels of ADL disability seem to have remained more or less constant in cohorts born between 1920s and 1940s. Nevertheless, a recent study (UK Family Resource Survey) of ∼97 000 non-institutionalised older adults aged over 65 years and born before 1945 revealed a significant falling trend in functional difficulties (defined by the presence of any long-standing illness, disability or infirmity) among men born between 1924 and 1945 but no evidence of cohort-based trend among women. The author found that the cohort-based trends in functional disabilities were related to socioeconomic status (SES) and that SES inequalities in functional disabilities increased among successive cohorts.34 In the present study, we found an improvement in SES (in terms of educational level) while disability remained quite stable over the successive birth cohorts. Trend in SES may therefore not reflect cohort-based trends in disability in our populations.
Although our findings are not able to determine the underlying causes of the period-based trend in disability, the increase in the period-based trend in disability observed in this study may be accounted for by better survival among people with chronic diseases, resulting in an eventual uptick in the disability burden. Further research will be needed to consider unmeasured factors that correlate with disability, such as early-life and mid-life factors. Interventions should be developed to improve physical functioning in older adults. Continued population-based survey of the elderly will promise to contribute to our understanding of the determinants of disability as well as their onset. Moreover, health policy approaches that help older adults live independently, such as the increase in use of preventive services, and creation of age-friendly environments to optimise independent functioning.
Several limitations of the current study require discussion. The earliest and latest cohorts did not capture a full age distribution (eg, the ≤1917 cohort only covered respondents at older ages of ≥85, the ≥1937 cohorts only covered respondents at younger ages of 65–74 years), thus biasing the estimates for cohort trends. Individuals born between 1904 and 1917 were merged due to their comparatively small size of several age groups, thus limiting the number of birth cohorts being studied. The surveys ended in the birth cohort 1947; therefore, we were unable to examine the cohort differences on disability between prewar generations and postwar baby boomers, whose early-life and mid-life experiences were remarkably different from each other. Information on birth place or risk factors in early-life and mid-life that may affect disability at older ages was not available, limiting the ability to identify causes of the increased disability burden in late life. The EHCs sample was not generated from population random sampling but rather through voluntary participation; those who were frail and home-bound would be under-represented; therefore, the prevalence of ADL disability may have been underestimated. However, the EHCs services are not designed to address a single specific question, but to provide primary healthcare services to the elderly in Hong Kong. Finally, our sample had higher proportions of young–old (aged 65–74 years) than that in the general population; and only captured the community-dwelling elderly; therefore, findings should not be generalised to the oldest-old and those who are institutionalised, as disability prevalence rates in the oldest-old or those living in institutions are much higher than that in the community.35 Despite these limitations, the surveys were population-based, which provide an updated examination of disability trends among Chinese adults aged 65 years and older in Hong Kong. Although the prevalence rate of ADL disability was low in our sample, the number of disability cases was sufficient to evaluate the trends in disability in the community, with similar trends being observed when institutionalised participants were included in a separate analysis (data not shown). Other strengths of this study include the adjustment for multiple potential cofounders, including sociodemographic characteristics, lifestyle factors, comorbidities as well as self-rated health, which are known to influence functional status.
In conclusion, the ageing population combined with the increased survival and risk of disability will have major implications for health and social care systems. Although there is no a priori reason to suggest any increasing trend in disability in the future survey years, the prevalence of disability will be increasing due to the growing number of older people. These patterns might help forecast the future risk of disability of and hence, to inform healthcare planning and the priorities for resource allocation.
Footnotes
Contributors: RY, MW, BC and JW contributed to the conception and design of the work; the acquisition, analysis and interpretation of data for the work; in drafting the work and revising it critically for important intellectual content and in giving final approval of the version to be published. XL, CML, TWA, JL, KT and RL contributed to the acquisition of data for the work; in partially drafting the work, in revising it critically for important intellectual content and in giving final approval of the version to be published. All authors (RY, MW, BC, XL, CML, TWA, JL, KT, RL and JW) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Department of Health of the Government of the Hong Kong Special Administrative Region.
Data sharing statement: No additional data are available.
References
- 1.Centre of Health Protection. Department of Health. Life expectancy at birth (male and female), 1971–2014. 2014. http://www.chp.gov.hk/en/data/4/10/27/111.html (accessed Dec 2015).
- 2.Manton KG. Recent declines in chronic disability in the elderly U.S. population: risk factors and future dynamics. Annu Rev Public Health 2008;29:91–113. 10.1146/annurev.publhealth.29.020907.090812 [DOI] [PubMed] [Google Scholar]
- 3.Feng QS, Zhen ZH, Gu DA et al. . Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998–2008. J Gerontol B Psychol 2013;68:476–85. 10.1093/geronb/gbt012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang Y, Song A, Du S et al. . Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci 2015;70:739–45. 10.1093/gerona/glu204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman VA, Martin LG, Schoeni RF et al. . Declines in late-life disability: the role of early- and mid-life factors. Soc Sci Med 2008;66:1588–602. 10.1016/j.socscimed.2007.11.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarkeala T, Nummi T, Vuorisalmi M et al. . Disability trends among nonagenarians in 2001–2007: vitality 90+ Study. Eur J Ageing 2011;8:87–94. 10.1007/s10433-011-0188-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedman VA, Spillman BC, Andreski PM et al. . Trends in late-life activity limitations in the United States: an update from five National Surveys. Demography 2013;50:661–71. 10.1007/s13524-012-0167-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaye HS. Disability rates for working-age adults and for the elderly have stabilized, but trends for each mean different results for costs. Health Aff (Millwood) 2013;32:127–34. 10.1377/hlthaff.2012.0533 [DOI] [PubMed] [Google Scholar]
- 9.Fuller-Thomson E, Yu B, Nuru-Jeter A et al. . Basic ADL disability and functional limitation rates among older Americans from 2000–2005: the end of the decline? J Gerontol A Biol 2009;64:1333–6. 10.1093/gerona/glp130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker M, Schön P, Lagergren M et al. . Functional ability in the elderly Swedish population from 1980 to 2005. Eur J Ageing 2008;5:299–309. 10.1007/s10433-008-0096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palacios-Cena D, Jiménez-Garcia R, Hernández-Barrera V et al. . Has the prevalence of disability increased over the past decade (2000–2007) in elderly people? A Spanish population-based survey. J Am Med Dir Assoc 2012;13:136–42. 10.1016/j.jamda.2010.05.007 [DOI] [PubMed] [Google Scholar]
- 12.Seeman TE, Merkin SS, Crimmins EM et al. . Disability trends among older Americans: national health and nutrition examination surveys, 1988–1994 and 1999–2004. Am J Public Health 2010;100:100–7. 10.2105/AJPH.2008.157388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin SF, Beck AN, Finch BK et al. . Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health 2012;102:2157–63. 10.2105/AJPH.2011.300602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chatterji S, Byles J, Cutler D et al. . Health, functioning, and disability in older adults-present status and future implications. Lancet 2015;385:563–75. 10.1016/S0140-6736(14)61462-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HRS: Health and Retirement Study. http://hrsonline.isr.umich.edu/ (accessed Dec 2015).
- 16.SHARE: Survey of Health A and Retirement in Europe. http://www.share-project.org/ (accessed Dec 2015).
- 17.de Oliveira CM, Lima-Costa MF. Birth cohort differences in physical functioning levels among elderly Brazilians: findings from the Bambuí Cohort Study of Aging (1997–2008). Cad Saude Publica 2011;27:S444–S53. 10.1590/S0102-311X2011001500015 [DOI] [PubMed] [Google Scholar]
- 18.Schooling CM, Chan WM, Leung SL et al. . Cohort profile: Hong Kong Department of Health Elderly Health Service Cohort. Int J Epidemiol 2016;45:64–72. 10.1093/ije/dyu227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Census and Statistics Department of Hong Kong Special Administrative Region. 2006 Population By-census: Thematic Report: Older Persons http://www.bycensus2006.gov.hk/FileManager/EN/Content_962/06bc_op.pdf (accessed Sep 2016).
- 20.Census and Statistics Department of Hong Kong Special Administrative Region. 2011 Population Census: Thematic Report: Older Persons http://www.census2011.gov.hk/pdf/older-persons.pdf
- 21.Census and Statistics Department of Hong Kong Special Administrative Region. Social Surveys Section. Thematic Household Survey Report No. 26 http://www.statistics.gov.hk/pub/B11302262006XXXXB0100.pdf (accessed Sep 2016).
- 22.Census and Statistics Department of Hong Kong Special Administrative Region. Thematic Household Survey Report No. 30 2007. http://www.statistics.gov.hk/pub/B11302302007XXXXB0100.pdf (accessed Sep 2016).
- 23.Census and Statistics Department of Hong Kong Special Administrative Region. Thematic Household Survey Report No. 45 2010. http://www.statistics.gov.hk/pub/B11302452010XXXXB0100.pdf (accessed Sep 2016).
- 24.Census and Statistics Department of Hong Kong Special Administrative Region. Thematic Household Survey Report No. 48 2011. http://www.statistics.gov.hk/pub/B11302482011XXXXB0100.pdf (accessed Sep 2016).
- 25.Katz S, Ford AB, Moskowitz RW et al. . Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–19. [DOI] [PubMed] [Google Scholar]
- 26.Zedlewski SR. The needs of the elderly in the 21st century. Washington DC: Urban Institute Press; Distributed by University Press of America, 1990. [Google Scholar]
- 27.Fillenbaum GG. Functional ability. In: Ebrahim S, Kalache A, eds. Epidemiology in old age. 1st edn London: BMJ Publishing Group, 1996:228–35. [Google Scholar]
- 28.Jagger C, Arthur AJ, Spiers NA et al. . Patterns of onset of disability in activities of daily living with age. J Am Geriatr Soc 2001;49:404–9. 10.1046/j.1532-5415.2001.49083.x [DOI] [PubMed] [Google Scholar]
- 29.Branch LG, Katz S, Kniepmann K et al. . A prospective study of functional status among community elders. Am J Public Health 1984;74:266–8. 10.2105/AJPH.74.3.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Census and Statistics Department of Hong Kong Special Administrative Region. Hong Kong Annual Digest of Statistics, 1981 to 2013 2014. http://www.statistics.gov.hk/pub/B10100032014AN14B0100.pdf (accessed Dec 2015).
- 31.Census and Statistics Department of Hong Kong Special Administrative Region. Social data collected via the General Household Survey Special Topics Report No. 62 Persons with disabilities and chronic diseases http://www.statistics.gov.hk/pub/B11301622014XXXXB0100.pdf (accessed Sep 2016).
- 32.Audit Commission of the Government of Hong Kong Special Administration Region. Report No. 63 of the Director of Audit (Chapter 1 Provision of long-term care services for the elderly) 2014. http://www.legco.gov.hk/yr14-15/english/counmtg/papers/cm20141120-sp030-e.pdf (accessed Dec 2015).
- 33.ELSA: English Longitudinal Study of Ageing. http://www.elsa-project.ac.uk/ (accessed Dec 2015).
- 34.Morciano M, Hancock RM, Pudney SE. Birth-cohort trends in older-age functional disability and their relationship with socio-economic status: evidence from a pooling of repeated cross-sectional population-based studies for the UK. Soc Sci Med 2015;136–137:1–9. 10.1016/j.socscimed.2015.04.035 [DOI] [PubMed] [Google Scholar]
- 35.Census and Statistics Department of Hong Kong Special Administrative Region. Thematic Household Survey Report No. 40 2010. http://www.statistics.gov.hk/pub/B11302402009XXXXB0100.pdf (accessed Sep 2016).
- 36.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum, 1998. [Google Scholar]