Abstract
Tracheal intubation (TI) is a routine procedure in the Intensive Care Unit (ICU) and is often life-saving. In contrast to the controlled conditions in the operating room, critically ill patients with respiratory failure and shock are physiologically unstable. These factors, along with a suboptimal evaluation of the airway and limited oxygen reserves despite adequate pre-oxygenation, are responsible for a high incidence of life-threatening complications such as severe hypoxaemia and cardiovascular collapse during TI in the ICU. The All India Difficult Airway Association (AIDAA) proposes a stepwise plan for safe management of the airway in critically ill patients. These guidelines have been developed based on available evidence; wherever robust evidence was lacking, recommendations were arrived at by consensus opinion of airway experts, incorporating the responses to a questionnaire sent to members of the AIDAA and the Indian Society of Anaesthesiologists. Non-invasive positive pressure ventilation during pre-oxygenation improves oxygen stores in patients with respiratory pathology. Nasal insufflation of oxygen at 15 L/min can increase the duration of apnoea before the occurrence of hypoxaemia. High-flow nasal cannula oxygenation at 60–70 L/min may also increase safety during TI in critically ill patients. Stable haemodynamics and gas exchange must be maintained during rapid sequence induction. It is necessary to implement an intubation protocol during routine airway management in the ICU. Adherence to a plan for difficult airway management incorporating the use of intubation aids and airway rescue devices and strategies is useful.
Keywords: Complications, emergency department, intensive care, intubation bundle, ketamine, non-invasive positive pressure ventilation, tracheal intubation
INTRODUCTION
Difficult intubations are common in the Intensive Care Unit (ICU), emergency department (ED) and pre-hospital settings, with the incidence ranging between 8% and 13%.[1,2,3,4,5]
Compromised cardiorespiratory physiology, risk of aspiration and the presence of specific factors related to the environment and inadequately trained operators render tracheal intubation (TI) in the ICU more likely to be associated with complications compared to that in the operating room (OR). Unlike in the OR, postponing airway management is not an option in critically ill patients who need a definite airway to be secured at the earliest.[6] The Fourth National Audit Project (NAP4) report of the Royal College of Anaesthesiologist and the Difficult Airway Society[7] found that more than 60% of airway complications in the ICU lead to death or brain damage, compared with 14% in anaesthesia. Several evidence-based strategies have been proposed to improve the safety and outcome of TI in the ICU. The All India Difficult Airway Association (AIDAA), therefore, developed guidelines to provide a stepwise approach to TI in the ICU with the goal of improving safety and outcomes in ICU patients. These guidelines neither represent the minimum standard of practice nor are they a substitute for good clinical judgement. These guidelines should be used in conjunction with ‘The AIDAA 2016 Guidelines for the Management of the Unanticipated Difficult Intubation in Adults’.[8]
METHODS
The methodology adopted for the development of AIDAA guidelines including anticipated difficult extubation guidelines has been described previously.[8] A thorough literature search was done using databases/search engines (Medline, PubMed, Google Scholar, websites of National Societies for airway guidelines) till September 2016. The articles were manually searched from cross-referencing. All manuscripts and abstracts published in English were searched. The keywords used included ‘intubation, intensive care, critical care, critically ill, complications, cardiovascular, pre-oxygenation, high-flow nasal cannula’. For areas that did not have robust evidence, opinions of experts and members of the societies were taken regarding issues related to TI in the ICU.
CHALLENGES AND COMPLICATIONS DURING TRACHEAL INTUBATION IN THE INTENSIVE CARE UNIT
There are several factors that make TI more challenging in ICU as compared to that in the OR [Table 1].
Table 1.
Challenges during tracheal intubation in the Intensive Care Unit

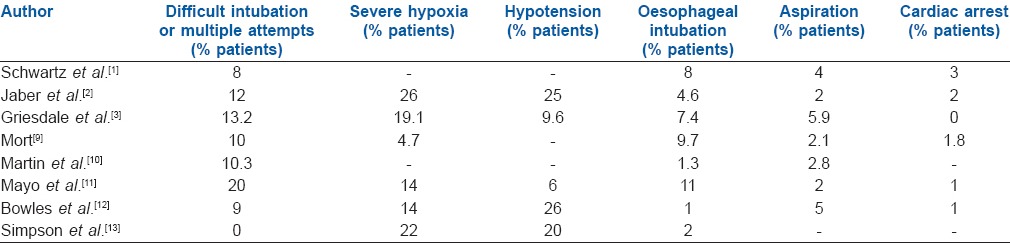
The incidence of complications during intubation in critically ill patients in the ICU and ED ranges from 22% to 54%, making emergency intubation a very high-risk procedure. Table 2 summarises the incidence of serious complications observed in some studies.[1,2,3,9,10,11,12,13] Two or more attempts at TI significantly increase the risk of complications.[3,14] In one study, complication rates in patients in whom two or more attempts were required, compared to those in whom intubation was successful at the first attempt, were aspiration (22% vs. 2%), hypoxaemia (70% vs. 12%) and cardiac arrest (11% vs. 1%).[9] These findings highlight the importance of improving first attempt success in critically ill patients.[14] The occurrence of aspiration and hypoxaemia during emergency intubations increased the risk of developing a cardiac arrest by 22 and four times, respectively. Oesophageal intubation was the most common cause of cardiac arrest and was associated with a seven-fold increase in the risk of death.[15]
Table 2.
Incidence of complications during tracheal intubation in critically ill patients
PREDICTING DIFFICULT INTUBATION IN THE INTENSIVE CARE UNIT
Most conventional tests used at predicting difficult airway[16,17] focus on anatomical features that make glottis visualisation difficult and are difficult to perform in patients requiring emergency intubation.[18] The MACOCHA score (Mallampati score III or IV, Apnoea syndrome (obstructive), Cervical spine limitation, Opening mouth 3 cm, Coma, Hypoxia and Anesthesiologist non-trained) has been recently developed to identify patients with potentially difficult airway in the ICU.[19] This score considers not only patient-related anatomical difficulty but also physiological factors and operator experience. The components of the score are the presence of a modified Mallampati Class III or IV scoring five points, obstructive sleep apnoea scoring two points and cervical immobility, limited mouth opening, coma, severe hypoxaemia and a non-anaesthesiologist operator scoring one point each. The score thus has a maximum of 12 points, with zero predicting an easy intubation and 12 points predicting a very difficult one. This test has a sensitivity of 73% and has not been validated for video laryngoscopy.[19]
SPECIAL CONSIDERATIONS DURING TRACHEAL INTUBATION IN THE INTENSIVE CARE UNIT
Presence of two operators (one experienced in airway management)
Studies suggest that the presence of an experienced operator during airway management and supervision of junior doctors performing intubation by a senior consultant can help reduce complications during TI in ICU.[2,20] Based on the available data, we recommend the presence of two operators during ICU intubations, with one being experienced in airway management.
Calling for help
In addition to the two operators present during intubation, we recommend calling for additional help at the earliest when the first difficulty in airway management is encountered. We also recommend calling for additional help when the final attempt at rescue mask ventilation fails and emergency cricothyroidotomy is planned. An additional person, who has not been part of the process until then, may be able to think more rationally and perform better in this situation, in addition to being an extra helping hand.
Pre-oxygenation and peri-intubation oxygenation in the Intensive Care Unit
Oxygen desaturation is the most common complication occurring during intubation in the ICU and is the most common reason for aborting intubation attempts. Therefore, proper pre-oxygenation is important to prolong the time to desaturation during intubation and increase the chance of first attempt success at intubation.[21]
Three minutes of pre-oxygenation using non-invasive positive pressure ventilation (NIPPV) delivered by an ICU ventilator using a face mask is more effective at reducing desaturation than by face mask with bag and reservoir.[22]
High-flow nasal cannula (HFNC) oxygen delivered at 70 L/min through a device capable of providing heated, humidified oxygen has been compared with standard methods of pre-oxygenation with mixed results.[23,24] HFNC oxygen administered at a flow rate of 60 L/min for pre-oxygenation that was continued during the intubation reduced the incidence of desaturation from 14% to 2% compared with non-rebreathing face mask preoxygenation. After pre-oxygenation with NIPPV, the addition of HFNC oxygen during attempts at TI significantly reduces the severity of desaturation.[25]
Apnoeic oxygenation provided through an HFNC during laryngoscopy may decrease desaturation during intubation and may lead to a higher first attempt success without hypoxaemia.[26,27,28] The use of an apnoeic oxygenation by simple nasal cannula at 15 L/min to prolong the duration of safe apnoea after the administration of neuromuscular blockade has been advocated in the ED.[28] However, a recent randomised trial did not show the benefit of apnoeic oxygenation during TI in critically ill patients,[29] possibly because the effectiveness of apnoeic oxygenation in the critically ill patient may be limited by the presence of illness causing a physiologic shunt. Recently, the addition of supplemental oxygen through a nasal cannula in the presence of mask leaks has been shown to improve the end-tidal oxygen during pre-oxygenation.[30]
Haemodynamic stabilisation
Hypotension after intubation is reported in nearly half of the intubated patients in ICU, with cardiovascular collapse occurring in 30% patients.[31,32,33] Haemodynamic instability is an independent predictor of death following intubation.[33] Peri-intubation haemodynamic instability has been shown to increase ICU stay and hospital mortality.[31,33,34,35,36] These studies highlight the importance of fluid resuscitation in critically ill patients along with pre-oxygenation to improve the safety of emergency intubations. In addition, preparedness and prompt treatment of post-intubation hypotension with vasopressors and further fluid therapy are important. Although adequate fluid resuscitation can help prevent post-intubation hypotension, proper selection of drugs for intubation is equally important.
Selection of pharmacological agents for tracheal intubation
Drugs such as benzodiazepines, propofol and thiopental may be used in reduced doses; however, they decrease the systemic vascular resistance, produce myocardial depression and may cause precipitous fall in blood pressure, especially in the American Society of Anesthesiologists III–IV patients and those with hypotension.[37,38,39] Drugs such as etomidate and ketamine are preferred in comparison in ICU. Although there are concerns about transient adrenal insufficiency with etomidate, especially in septic patients, there is no convincing evidence of harm.[40] Ketamine, due to its sympathomimetic effects, helps maintain blood pressure during intubation. When compared with etomidate, there was no difference in the rate of complications.[41] Ketamine may cause hypertension, tachycardia, increased airway secretions, raised intracranial and intraocular pressure. Unless contraindicated, it should be the preferred induction agent for endotracheal intubation. Other agents such as opiates, dexmedetomidine and lignocaine can be used as adjuncts to blunt the sympathetic response to laryngoscopy.
The use of neuromuscular blocking agents improves not only the laryngoscopic grade of view but also the overall intubating conditions. Use of neuromuscular blocking agents has been shown to improve the first-attempt intubation success with both rapid and delayed sequence intubation, irrespective of the choice of induction agent (ketamine or etomidate) or route of administration used.[42,43] Suxamethonium has been the conventionally used neuromuscular blocking agent of choice, unless contraindicated, due to its fast action facilitating early intubation without the need for ventilation. However, rocuronium at a dose of 1.2 mg/kg has comparable speed of action and intubating conditions to suxamethonium.[44]
Device selection
Although used more widely in the OR, video laryngoscopy has been shown to increase the first-attempt success and improve glottis visualisation during intubation in the ICU, ED and in the pre-hospital setting, even in patients with a predicted difficult airway.[45,46,47] The meta-analysis by De Jong et al., comparing direct laryngoscopy with video laryngoscopy for TI in ICU, showed that the first-attempt success was twice as much when a video laryngoscope was used.[45]
The NAP4 report of the intensive care and ED[7] patients identified the non-availability of appropriate equipment such as the flexible fibre-optic bronchoscope, lack of training to use the equipment and failure to consider using the right equipment to be the most common issues with use of airway management devices in ICU. This highlights the importance of adequate training regarding airway equipment for ICU doctors and availability of appropriate devices for airway management in the ICU, just as is in the OR.
Rapid sequence induction
Most of ICU patients are considered to have a full stomach, and securing the airway with a rapid sequence intubation seems logical. Either suxamethonium (if not contraindicated) or rocuronium may be used for neuromuscular blockade. Application of cricoid pressure may make the laryngoscopic view unfavourable. In such situations, cricoid pressure should be partially or completely released to improve the laryngoscopic view and later reapplied. Gentle mask ventilation while applying cricoid pressure before TI can prolong the time to desaturation and may be useful in patients with poor respiratory reserve and sepsis. A second-generation supraglottic airway device (SAD) offers greater protection against aspiration as compared to the first-generation devices[48] and should be inserted if TI fails during a rapid sequence induction. SAD insertion may become difficult if cricoid pressure is applied and this should be released during insertion.
Confirmation of tracheal Intubation
The NAP4 report[7] showed that failure to use capnography contributed to 17 deaths or brain damage in ICU. Oesophageal intubations and accidental tube displacements accounted for 82% of events leading to death or brain damage. This report strongly recommends the use of capnography for confirmation of TI in all critically ill patients, irrespective of location.
Human factors and training
Intubation in ICU is required at any time in the day or night and may often be performed by the less experienced practitioner. In addition, considering the altered physiology of the critically ill patients, lesser time to desaturation and higher risk of complications, these intubations may lead to very stressful situations,[6] which may compromise the performance of the operator. Thus, airway management training should be an integral part of the training of any speciality which deals with critically ill patients. Use of simulation-based training will help enhance both technical and non-technical skills and improve preparedness for this highly stressful situation. Use of an algorithmic approach and an intubation bundle may further improve performance.
The intubation bundle
Bundles are a structured way of improving processes of patient care and outcomes using a small, straightforward set of evidence-based practices, which when performed collectively and reliably, have proved to improve patient outcomes. Based on the available evidence, Jaber et al.[49] proposed an intubation management protocol. Adherence to the protocol resulted in significantly fewer life-threatening complications such as severe hypoxaemia, severe hypotension or cardiac arrest (21% vs. 34%) and also mild to moderate complications (9% vs. 21%), compared to a conventional strategy. This bundle has ten components[49] which include presence of two operators, fluid loading with 500 ml saline, preparation of long-term sedation and pre-oxygenation for 3 min with non-invasive ventilation (100% oxygen, pressure support ventilation level between 5 and 15 cmH2O to obtain an expiratory tidal volume between 6 and 8 ml/kg and positive end-expiratory pressure [PEEP] of 5 cmH2O) in case of acute respiratory failure in the pre-intubation period. Rapid sequence induction is performed using cricoid pressure with either ketamine or etomidate for induction and suxamethonium or rocuronium for neuromuscular blockade. Post-intubation components include immediate confirmation of tube placement using capnography, using norepinephrine if the diastolic blood pressure remains low, initiation of long-term sedation and use of protective lung ventilation. While this bundle has not been validated, we believe it is a reasonable protocol for safe TI in the ICU.
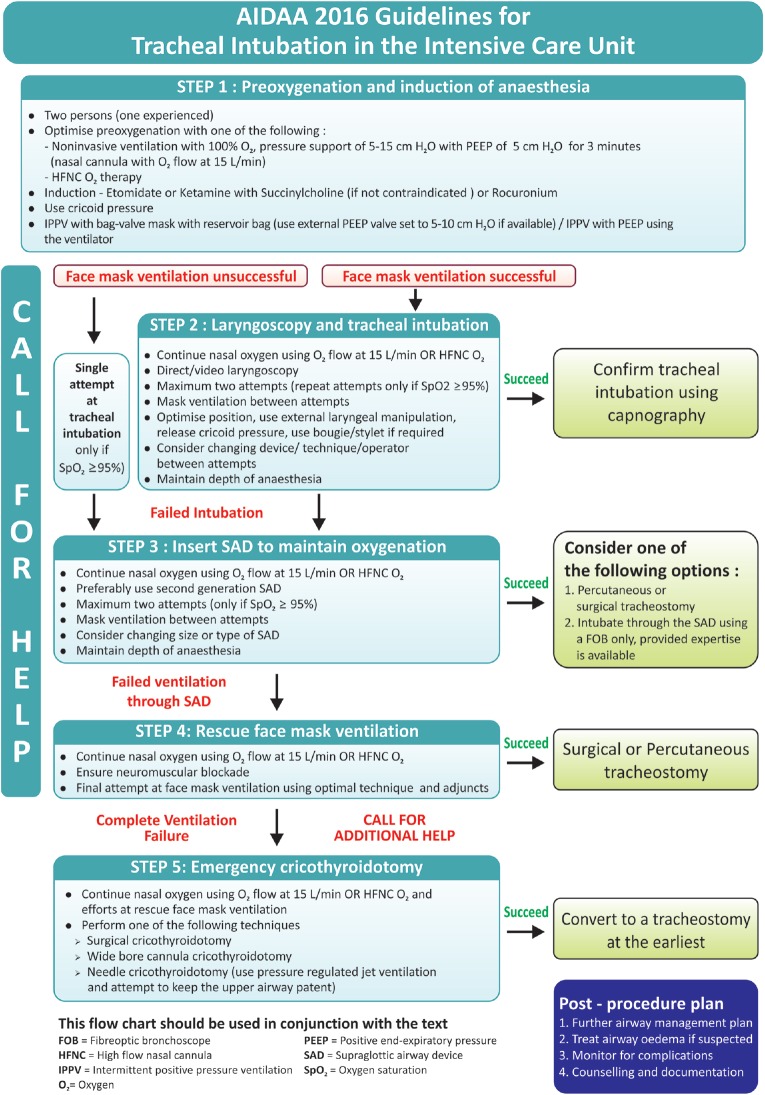
A STEPWISE APPROACH FOR THE MANAGEMENT TRACHEAL INTUBATION IN THE INTENSIVE CARE UNIT
The AIDAA proposes a stepwise approach for management of TI in ICU [Figure 1]. It is important to remember that while following any step in the algorithm, if the oxygen saturation is not maintained or starts rapidly falling or bradycardia develops, one can bypass one or more steps and proceed to rescue ventilation and even emergency cricothyrotomy.
Figure 1.
All India Difficult Airway Association 2016 algorithm for the management of tracheal intubation in the Intensive Care Unit
Step 1: Pre-oxygenation and induction of anaesthesia
During intubation, the presence of minimum two persons is required, of which one should be experienced in airway management. Pre-oxygenation should be done, in the head-elevated position, if possible, using non-invasive ventilation with a pressure support ventilation level between 5 and 15 cmH2O to obtain an expiratory tidal volume between 6 and 8 mL/kg and PEEP of 5 cm H2O (nasal cannula with an oxygen flow of 15 L/min may be used in addition when there is a mask leak) or HFNC with 70 L/min of oxygen flow should be used. Pre-intubation fluid loading with 500 mL of saline should be given in the absence of cardiogenic pulmonary oedema. The patient should be anaesthetised using ketamine or etomidate and neuromuscular blockade provided with succinylcholine or rocuronium. Intermittent positive pressure ventilation (IPPV) may be performed using bag-valve mask with reservoir bag using external PEEP valve set to 5–10 cmH2O PEEP if available or IPPV using the ventilator maintaining a cricoid pressure throughout. Cricoid pressure should be given but may be partially or completely released if ventilation is inadequate.
Step 2: Laryngoscopy and tracheal intubation
If mask ventilation is successful, proceed with TI using direct or video laryngoscopy. Nasal oxygen using oxygen flow of 15 L/min or HFNC oxygen should be continued. Do not exceed more than two attempts at intubation and repeat an attempt only if the oxygen saturation (SpO2) is ≥95%. Mask ventilation should be performed between attempts. Optimise position, use external laryngeal manipulations, partially or completely release the cricoid pressure to optimise the laryngoscopic view if required and use a bougie or stylet if required. Between attempts at intubation, consider changing the device or technique, rather than repeating the same technique. Maintain depth of anaesthesia throughout the intubation attempts. If mask ventilation is not possible, a single attempt at intubation could be made, provided the SpO2 is ≥95%. After intubation, confirm proper endotracheal tube (ET) tube position using capnography along with clinical methods.
Step 3: Insert supraglottic airway device to maintain oxygenation
If two attempts at intubation fail, or after a single attempt at intubation following unsuccessful mask ventilation fails, insert a SAD (preferably a second generation device) and ventilate to maintain oxygenation. Not more than two attempts should be made to insert an SAD and only if the SpO2 is ≥95%. Nasal oxygen using oxygen flow of 15 L/min or HFNC oxygen should be continued during SAD insertion. Perform mask ventilation between the attempts. Consider using a different type or size of SAD during the second attempt. Maintain depth of anaesthesia throughout the insertion attempts. Once SAD insertion is successful and oxygenation is maintained, consider performing a percutaneous or surgical tracheostomy for further airway management. Intubation through the SAD may be considered, but only under vision using a flexible fibre-optic bronchoscope. Intubation should not be attempted blindly through the SAD if a bronchoscope and the expertise to use it are unavailable.
Step 4: Rescue face mask ventilation
If ventilation through the SAD fails, continue nasal oxygenation using oxygen flow of 15 L/min or HFNC oxygen. Ensure complete neuromuscular blockade, repeat a muscle relaxant if required. Give one final attempt at face mask ventilation using optimal technique and adjuncts. If rescue face mask ventilation is successful, proceed with a percutaneous or surgical tracheostomy. However, if rescue face mask ventilation is unsuccessful, there is ‘complete ventilation failure’. Continue nasal oxygenation using oxygen flow at 15 L/min or HFNC oxygen and call for additional help. Immediately, start performing emergency cricothyroidotomy before the patient desaturates further.
Step 5: Emergency cricothyroidotomy
Perform emergency cricothyroidotomy using needle or surgical cricothyroidotomy, based on familiarity and availability of equipment. If needle cricothyroidotomy is performed, maintain oxygenation using pressure-regulated jet ventilation, until a tracheostomy is performed. If a wide bore cannula cricothyroidotomy set has been used or an ET tube has been passed through the front of the neck, continue ventilation manually or using a ventilator circuit.
SUMMARY
TI in the ICU is a potentially hazardous procedure, most commonly due to failing oxygenation and unstable haemodynamics during emergency intubations. The AIDAA stepwise approach emphasises the importance of adequate supervision, good pre-oxygenation with non-invasive ventilation or HFNC oxygen at 60 L/min, maintenance of haemodynamic stability, use of IPPV with PEEP before intubation and insufflation of oxygen at 15 L/min or HNFC oxygen throughout the period of apnoea. SADs have an important role in difficult airway management, and cricothyroidotomy is the procedure of choice when there is complete ventilation failure. We believe that the AIDAA guidelines will help increase the safety of TI in the ICU.
Financial support and sponsorship
All expenses related to the development of the guidelines were entirely funded by the All India Difficult Airway Association.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–76. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the Intensive Care Unit: A prospective, multiple-center study. Crit Care Med. 2006;34:2355–61. doi: 10.1097/01.CCM.0000233879.58720.87. [DOI] [PubMed] [Google Scholar]
- 3.Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008;34:1835–42. doi: 10.1007/s00134-008-1205-6. [DOI] [PubMed] [Google Scholar]
- 4.Jabre P, Avenel A, Combes X, Kulstad E, Mazariegos I, Bertrand L, et al. Morbidity related to emergency endotracheal intubation - A substudy of the KETAmine SEDation trial. Resuscitation. 2011;82:517–22. doi: 10.1016/j.resuscitation.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Breckwoldt J, Klemstein S, Brunne B, Schnitzer L, Mochmann HC, Arntz HR. Difficult prehospital endotracheal intubation - Predisposing factors in a physician based EMS. Resuscitation. 2011;82:1519–24. doi: 10.1016/j.resuscitation.2011.06.028. [DOI] [PubMed] [Google Scholar]
- 6.Divatia JV, Khan PU, Myatra SN. Tracheal intubation in the ICU: Life saving or life threatening? Indian J Anaesth. 2011;55:470–5. doi: 10.4103/0019-5049.89872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook TM, Woodall N, Harper J, Benger J Fourth National Audit Project. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. Br J Anaesth. 2011;106:632–42. doi: 10.1093/bja/aer059. [DOI] [PubMed] [Google Scholar]
- 8.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India Difficult Airway Association 2016 for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;12:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mort TC. Emergency tracheal intubation: Complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–13. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 10.Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: Airway outcomes and complications. Anesthesiology. 2011;114:42–8. doi: 10.1097/ALN.0b013e318201c415. [DOI] [PubMed] [Google Scholar]
- 11.Mayo PH, Hegde A, Eisen LA, Kory P, Doelken P. A program to improve the quality of emergency endotracheal intubation. J Intensive Care Med. 2011;26:50–6. doi: 10.1177/0885066610384070. [DOI] [PubMed] [Google Scholar]
- 12.Bowles TM, Freshwater-Turner DA, Janssen DJ, Peden CJ RTIC Severn Group. Out-of-theatre tracheal intubation: Prospective multicentre study of clinical practice and adverse events. Br J Anaesth. 2011;107:687–92. doi: 10.1093/bja/aer251. [DOI] [PubMed] [Google Scholar]
- 13.Simpson GD, Ross MJ, McKeown DW, Ray DC. Tracheal intubation in the critically ill: A multi-centre national study of practice and complications. Br J Anaesth. 2012;108:792–9. doi: 10.1093/bja/aer504. [DOI] [PubMed] [Google Scholar]
- 14.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–8. doi: 10.1111/acem.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: A justification for incorporating the ASA Guidelines in the remote location. J Clin Anesth. 2004;16:508–16. doi: 10.1016/j.jclinane.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict difficult tracheal intubation: A prospective study. Can Anaesth Soc J. 1985;32:429–34. doi: 10.1007/BF03011357. [DOI] [PubMed] [Google Scholar]
- 17.Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–6. doi: 10.1093/bja/61.2.211. [DOI] [PubMed] [Google Scholar]
- 18.Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med. 2004;44:307–13. doi: 10.1016/j.annemergmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 19.De Jong A, Molinari N, Terzi N, Mongardon N, Arnal JM, Guitton C, et al. Early identification of patients at risk for difficult intubation in the Intensive Care Unit: Development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med. 2013;187:832–9. doi: 10.1164/rccm.201210-1851OC. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt UH, Kumwilaisak K, Bittner E, George E, Hess D. Effects of supervision by attending anesthesiologists on complications of emergency tracheal intubation. Anesthesiology. 2008;109:973–7. doi: 10.1097/ALN.0b013e31818ddb90. [DOI] [PubMed] [Google Scholar]
- 21.Mosier JM, Hypes CD, Sakles JC. Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med. 2016 Jun 24; doi: 10.1007/s00134-016-4426-0. [Epub ahead of print]. DOI 10.1007/s00134-016-4426-0. [DOI] [PubMed] [Google Scholar]
- 22.Baillard C, Fosse JP, Sebbane M, Chanques G, Vincent F, Courouble P, et al. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am J Respir Crit Care Med. 2006;174:171–7. doi: 10.1164/rccm.200509-1507OC. [DOI] [PubMed] [Google Scholar]
- 23.Vourc’h M, Asfar P, Volteau C, Bachoumas K, Clavieras N, Egreteau PY, et al. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: A randomized controlled clinical trial. Intensive Care Med. 2015;41:1538–48. doi: 10.1007/s00134-015-3796-z. [DOI] [PubMed] [Google Scholar]
- 24.Miguel-Montanes R, Hajage D, Messika J, Bertrand F, Gaudry S, Rafat C, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med. 2015;43:574–83. doi: 10.1097/CCM.0000000000000743. [DOI] [PubMed] [Google Scholar]
- 25.Jaber S, Monnin M, Girard M, Conseil M, Cisse M, Carr J, et al. Apnoeic oxygenation via high-flow nasal cannula oxygen combined with non-invasive ventilation preoxygenation for intubation in hypoxaemic patients in the Intensive Care Unit: The single-centre, blinded, randomised controlled OPTINIV trial. Intensive Care Med. 2016;42:1877–87. doi: 10.1007/s00134-016-4588-9. [DOI] [PubMed] [Google Scholar]
- 26.Sakles JC, Mosier JM, Patanwala AE, Arcaris B, Dicken JM. First pass success without hypoxemia is increased with the use of apneic oxygenation during rapid sequence intubation in the emergency department. Acad Emerg Med. 2016;23:703–10. doi: 10.1111/acem.12931. [DOI] [PubMed] [Google Scholar]
- 27.Wimalasena Y, Burns B, Reid C, Ware S, Habig K. Apneic oxygenation was associated with decreased desaturation rates during rapid sequence intubation by an Australian helicopter emergency medicine service. Ann Emerg Med. 2015;65:371–6. doi: 10.1016/j.annemergmed.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–75-e1. doi: 10.1016/j.annemergmed.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Semler MW, Janz DR, Lentz RJ, Matthews DT, Norman BC, Assad TR, et al. Randomized trial of apneic oxygenation during endotracheal intubation of the critically Ill. Am J Respir Crit Care Med. 2016;193:273–80. doi: 10.1164/rccm.201507-1294OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hayes-Bradley C, Lewis A, Burns B, Miller M. Efficacy of nasal cannula oxygen as a preoxygenation adjunct in emergency airway management. Ann Emerg Med. 2016;68:174–80. doi: 10.1016/j.annemergmed.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 31.Heffner AC, Swords D, Kline JA, Jones AE. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care. 2012;27:417-e9–13. doi: 10.1016/j.jcrc.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Perbet S, De Jong A, Delmas J, Futier E, Pereira B, Jaber S, et al. Incidence of and risk factors for severe cardiovascular collapse after endotracheal intubation in the ICU: A multicenter observational study. Crit Care. 2015;19:257. doi: 10.1186/s13054-015-0975-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green RS, Turgeon AF, McIntyre LA, Fox-Robichaud AE, Fergusson DA, Doucette S, et al. Postintubation hypotension in Intensive Care Unit patients: A multicenter cohort study. J Crit Care. 2015;30:1055–60. doi: 10.1016/j.jcrc.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 34.Green RS, Edwards J, Sabri E, Fergusson D. Evaluation of the incidence, risk factors, and impact on patient outcomes of postintubation hemodynamic instability. CJEM. 2012;14:74–82. doi: 10.2310/8000.2012.110548. [DOI] [PubMed] [Google Scholar]
- 35.Kim WY, Kwak MK, Ko BS, Yoon JC, Sohn CH, Lim KS, et al. Factors associated with the occurrence of cardiac arrest after emergency tracheal intubation in the emergency department. PLoS One. 2014;9:e112779. doi: 10.1371/journal.pone.0112779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smischney NJ, Demirci O, Ricter BD, Hoeft CC, Johnson LM, Ansar S, et al. Vasopressor use as a surrogate for post-intubation hemodynamic instability is associated with in-hospital and 90-day mortality: A retrospective cohort study. BMC Res Notes. 2015;8:445. doi: 10.1186/s13104-015-1410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shah SB, Chowdhury I, Bhargava AK, Sabbharwal B. Comparison of hemodynamic effects of intravenous etomidate versus propofol during induction and intubation using entropy guided hypnosis levels. J Anaesthesiol Clin Pharmacol. 2015;31:180–5. doi: 10.4103/0970-9185.155145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaushal RP, Vatal A, Pathak R. Effect of etomidate and propofol induction on hemodynamic and endocrine response in patients undergoing coronary artery bypass grafting/mitral valve and aortic valve replacement surgery on cardiopulmonary bypass. Ann Card Anaesth. 2015;18:172–8. doi: 10.4103/0971-9784.154470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A, et al. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005;101:622–8. doi: 10.1213/01.ANE.0000175214.38450.91. [DOI] [PubMed] [Google Scholar]
- 40.Gu WJ, Wang F, Tang L, Liu JC. Single-dose etomidate does not increase mortality in patients with sepsis: A systematic review and meta-analysis of randomized controlled trials and observational studies. Chest. 2015;147:335–46. doi: 10.1378/chest.14-1012. [DOI] [PubMed] [Google Scholar]
- 41.Jabre P, Combes X, Lapostolle F, Dhaouadi M, Ricard-Hibon A, Vivien B, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: A multicentre randomised controlled trial. Lancet. 2009;374:293–300. doi: 10.1016/S0140-6736(09)60949-1. [DOI] [PubMed] [Google Scholar]
- 42.Mosier JM, Sakles JC, Stolz U, Hypes CD, Chopra H, Malo J, et al. Neuromuscular blockade improves first-attempt success for intubation in the Intensive Care Unit. A propensity matched analysis. Ann Am Thorac Soc. 2015;12:734–41. doi: 10.1513/AnnalsATS.201411-517OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lyon RM, Perkins ZB, Chatterjee D, Lockey DJ, Russell MQ Kent, Surrey and Sussex Air Ambulance Trust. Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia. Crit Care. 2015;19:134. doi: 10.1186/s13054-015-0872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marsch SC, Steiner L, Bucher E, Pargger H, Schumann M, Aebi T, et al. Succinylcholine versus rocuronium for rapid sequence intubation in intensive care: A prospective, randomized controlled trial. Crit Care. 2011;15:R199. doi: 10.1186/cc10367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Jong A, Molinari N, Conseil M, Coisel Y, Pouzeratte Y, Belafia F, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the Intensive Care Unit: A systematic review and meta-analysis. Intensive Care Med. 2014;40:629–39. doi: 10.1007/s00134-014-3236-5. [DOI] [PubMed] [Google Scholar]
- 46.Sakles JC, Patanwala AE, Mosier JM, Dicken JM. Comparison of video laryngoscopy to direct laryngoscopy for intubation of patients with difficult airway characteristics in the emergency department. Intern Emerg Med. 2014;9:93–8. doi: 10.1007/s11739-013-0995-x. [DOI] [PubMed] [Google Scholar]
- 47.Silverberg MJ, Li N, Acquah SO, Kory PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: A randomized controlled trial. Crit Care Med. 2015;43:636–41. doi: 10.1097/CCM.0000000000000751. [DOI] [PubMed] [Google Scholar]
- 48.Cook TM, Kelly FE. Time to abandon the ‘vintage’ laryngeal mask airway and adopt second-generation supraglottic airway devices as first choice. Br J Anaesth. 2015;115:497–9. doi: 10.1093/bja/aev156. [DOI] [PubMed] [Google Scholar]
- 49.Jaber S, Jung B, Corne P, Sebbane M, Muller L, Chanques G, et al. An intervention to decrease complications related to endotracheal intubation in the Intensive Care Unit: A prospective, multiple-center study. Intensive Care Med. 2010;36:248–55. doi: 10.1007/s00134-009-1717-8. [DOI] [PubMed] [Google Scholar]