Abstract
Background and Aims:
Hypotensive anaesthesia reduces intra-articular bleed and promotes visualisation during arthroscopy. The haemodynamic effects of inhalational agents isoflurane and sevoflurane were studied extensively, and both were found to reduce mean arterial pressures (MBP) to an equivalent magnitude. We investigated the relative ability of isoflurane vis-a-vis sevoflurane to maintain the target systolic blood pressure (SBP) in patients undergoing shoulder arthroscopic procedures.
Methods:
In a prospective randomised study, 59 patients in two groups of 30 and 29 patients each received concomitant general anaesthesia (1.2–1.5 MAC of isoflurane and sevoflurane) and interscalene brachial plexus block. Nitrous oxide was used in both groups. Intraoperatively, serial blood pressure recordings of SBP, diastolic blood pressure (DBP), MBP and heart rates were done at every 3rd min intervals. The manipulations needed to achieve target SBP (T = 90 mmHg) for optimal arthroscopic visualisation and treat unacceptable hypotensive episodes were noted. Conventional statistical tests and process capability index (PCI) evaluation were both deployed for data analysis.
Results:
Lower mean SBP and DBPs were recorded for isoflurane patients as compared to sevoflurane (P < 0.05, for mean, maximum and minimum recordings). Higher mean heart rates were recorded for isoflurane (P < 0.05). PCIs indicated that isoflurane was superior to sevoflurane in the ease of achieving target SBP of 90 mmHg as well as maintaining blood pressures in the range of 80–100 mmHg.
Conclusion:
Isoflurane provides better intraoperative haemodynamic status vis-a-vis sevoflurane in patients undergoing shoulder arthroscopic surgery with preliminary interscalene blockade. The PCI can be a useful additional medical data analysis tool.
Keywords: Isoflurane, process capability index, sevoflurane, shoulder arthroscopy, volatile anaesthetic
INTRODUCTION
Controlled hypotension[1] has an established role in reducing intra-articular bleed and thereby improving visualisation during shoulder arthroscopy.[2] The haemodynamic effects of isoflurane and sevoflurane have been extensively studied earlier. Both these agents reduce mean arterial blood pressures (MBP) to an equivalent magnitude.[3] The haemodynamic parameter which is directly linked to pump pressures, intra-articular bleed and clarity of vision is the systolic blood pressure (SBP).[4] SBP is, therefore, preferentially targeted during controlled hypotension. An agent which achieves low SBP with concomitant preservation of autoregulation of vital organ blood flow would be the anaesthetic of choice.[5] While hunt continues for the ideal anaesthetic maintenance agent for shoulder surgery, MEDLINE search (NCBI database literature; key words: volatile anaesthetic, isoflurane, sevoflurane, shoulder arthroscopy, controlled hypotension) revealed no study on shoulder arthroscopic surgeries till date comparing isoflurane and sevoflurane inhalational techniques employed with concomitant interscalene brachial plexus block. This study aims to compare the capability (to achieve and maintain the desired haemodynamic status, target, TSBP = 90 mmHg, SBP) and convenience (of manipulations performed by the anaesthesiologist for maintaining such a status) of these two inhalational agents in this subset of patients. Considering the comparability of isoflurane at 1.2–1.5 MAC to sevoflurane at equal MAC, we investigated the hypothesis that both agents are similar to each other in their capability to achieve the desired haemodynamic status. We used the ‘process capability indices’ (PCIs) as an additional statistical tool in analysing our data, which we believe lends to more accurate conclusions.
METHODS
This prospective study was approved by the Institute Ethical Committee. Fifty-nine (among 64) randomly assigned (Random number generator, Random # generator, Jess Tucker, version 1.1.3, © 2013 Webberface, LLC, iOS application, Category: Utilities, info@webberface.com) patients belonging to the American Society of Anesthesiologists (ASA) status 1 and 2, who underwent shoulder arthroscopic surgery over a 23-month period (January 2014 to November 2015) were included in the study. Since an effective preliminary interscalene block formed an essential part of the anaesthetic procedure, patients, in whom the regional block was not performed (n = 4; 1 in isoflurane and 3 in sevoflurane group) or less than optimally effective before inhalational anaesthesia was instituted, were excluded from the study. Likewise, patients with severe pain at the operative site immediately after termination of inhalational anaesthesia indicating ineffectiveness of the block were also excluded from the study (n = 1, sevoflurane, [Consort Chart 1]). Of the 59 patients, 29 underwent sevoflurane anaesthesia and 30 received isoflurane. All patients were anaesthetised by the same anaesthesiologist, the first author and operated by the same surgeon. After preoperative assessment and recording of baseline vitals, these hospital inpatients were premedicated with tablet ranitidine 150 mg, having fasted overnight before the surgical procedure. No sedatives or opioids were used for premedication.
Consort Chart 1.
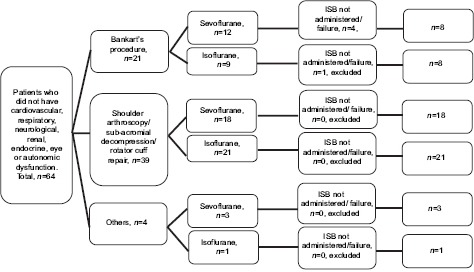
The distribution of patients in both groups. ISB=Interscalene block
In the operating room, patients were administered intravenous (i.v.) injection fentanyl 2 μg/kg. Ultrasound-guided (SonoSite™, high frequency, linear probe, 13-6 MHz) interscalene, in-plane block was performed in the supine position with a mixture of 6 ml lignocaine 2% and 25 ml levobupivacaine 0.25%. The effectiveness of the block was confirmed by the abolition of sensations (pinprick) over C4–C7 dermatomes and/or free and painless (passive) abduction in patients with painful shoulders. Induction was performed with i.v. bolus dose of injection propofol 2 mg/kg. Tracheal intubation was facilitated using i.v. injection vecuronium or rocuronium in 2 ED95 doses and ventilation was instituted to achieve normocarbia. Three-lead electrocardiogram, SpO2, non-invasive blood pressure (NIBP), end-tidal carbon dioxide and inhalational agent monitoring were done during the entire procedure. NIBP recording was done in 3 min intervals in the non-operative upper arm.
With the patient in the lateral decubitus position, anaesthesia was maintained using either sevoflurane (Abbott laboratories Ltd., DatumVaporizer, MediTec England, Queenborough, Kent MEII, 5EL) or isoflurane (Abbott loan vaporizer, Abbott Australasia Pty. Ltd, 32-34 Lord street, Botany NSW 2019, Australia) at 1.2–1.5 MAC dosages. Oxygen 33% and N2O 66% mixture were used in both the groups. Age-related iso-MAC inhalational concentrations (ChronoMAC, Application Timeline, Version 1.0: iOS application, 2011)[6] were used to achieve the desired end-tidal concentrations (0.3%, 1.0% - minimum and 2%, 3.0% - maximum for isoflurane and sevoflurane, respectively) for maintenance of anaesthesia. Muscle paralysis was achieved with bolus doses of injection vecuronium or rocuronium to obtain train-of-four counts 1–2 and controlled ventilation was carried out. SBP, diastolic blood pressure (DBP), MBP and heart rate were recorded every 3rd min. The study period was considered from the time of insertion of the arthroscope to its removal. Before inserting the arthroscope and during the maintenance of anaesthesia, efforts were made to attain the target (T) SBP of 90 mmHg using the following methods: Method A- increasing the depth of anaesthesia by administering additional doses of fentanyl (1 μg/kg) with propofol (1 mg/kg) and Method B- pharmacological intervention using a α/β-blocker (Labetalol, minimum 20 mg and maximum 40 mg). Method B was followed only after failure of Method A. Any adverse events such as persistent hypotension (3 consecutive readings of SBPs lower than target or MBP <60 mmHg) or severe bradycardia (heart rate <40 beats/min) were treated (saline bolus, i.v. ephedrine and i.v. atropine). The arthroscopic pump (Continuous Wave III Arthroscopy Pump, Arthrex, Arthrex Med. Inst. GmbH, Germany) pressure was 30–40 mmHg and irrigant flow at 40%–50% were maintained throughout the procedure for adequate visualisation. Necessary efforts were made to avoid hypothermia, urinary bladder distension and position-related complications.
The data was checked for its distribution by Anderson–Darling (AD) test. Statistical analysis was performed using Minitab® 17.1.0, © 2013 Minitab Inc. statistical software. A minimum of 16 patients was required in each group to detect a mean blood pressure (BP) difference of 10 mmHg, and these differences and sample sizes were based on earlier similar studies on arthroscopy haemodynamics (power 80%, α = 0.05, β = 0.20, with standard deviation [SD] of 10mmHg) in each group. A P-value of <0.05 was considered as statistically significant. The study included a higher number of subjects than necessary owing to the methodology of evaluation employed (PCI analysis).
Data was categorised and analysed by two methods [Flow Chart 1].
Flow Chart 1.
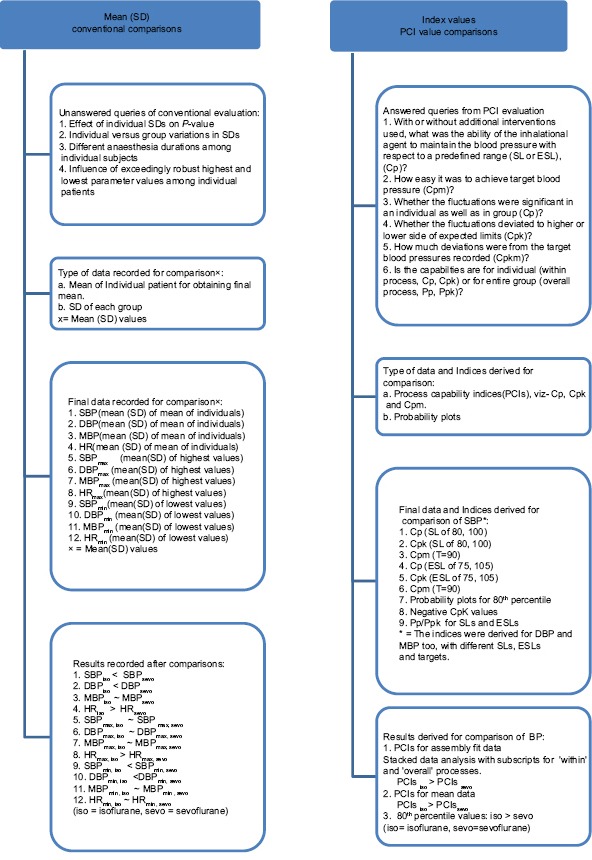
Describing the data evaluation methods, merits and demerits. HR- heart rate. For other abbreviations, please see text
First, as mean with SD and 95% confidence intervals for vital recordings were derived. Mean (SD) of mean of BPs (SBP, MBP, DBP) and heart rate for both groups, mean (SD) of each patient's maximum (max) and minimum (min) readings for both groups were noted separately. The independent sample t-test was used for comparison of haemodynamic data.
The second method included derivation through PCIs. Each patient's recordings were analysed (stacked data) for obtaining assembly fit data and separately for means (with SDs). Assembly fit data of SBP were re-derived for PCIs after Box-Cox data transformation with lambda, λ = 0.5 as AD test showed its distribution as non-normal. Setting the desired systolic pressure target (T) during the procedure (TSBP = 90 mmHg, SBP) for each patient, we derived PCIs for the desired range of maintained SBP i.e., between 100 and 80 mmHg. These formed the upper specification limit and lower specification limit (USL and LSL) of SBP(100,80). Further, the capability of the inhalational agents was analysed using a wider range of SBPs simply by extension of the upper and lower limits to 105 and 75 mmHg, respectively (extended SLs [ESLs, SBP(105,75)]).
Similar to SBPs, PCIs for DBPs (TDBP = 60 mmHg) and MBPs (TMBP = 70 mmHg) too were derived for SLs and for ESLs, separately (SLs for DBP(70,50), MBP(80,60) and the ESLs for DBP(75,45) and MBP(85,55)). For these co-variables, hypothetical targets were considered for PCI analysis.
To determine the ability of the inhalational agent to maintain the blood pressure with respect to a predefined range (SL or ESL), the PCI, Cp was considered. Cpm was useful in evaluating the convenience of the inhalational agent in achieving target blood pressure. To analyse whether the fluctuations deviated to higher or lower side of expected limits, the PCI, Cpk was considered. These three PCIs were derived for assembly fit and for means data in each group. Corresponding ‘overall process’ indices, Pp and Ppk values too were derived for ‘group performance’ analysis. These overall process indicators were derived for each group with respect to SBP alone. The probability plots of blood pressures were analysed for 80th percentile values and distribution in each group.
RESULTS
The demographic characteristics, duration of surgery and the variety of surgical procedures are detailed in Table 1 and Consort Chart 1.
Table 1.
Characteristics of patients, surgical procedures and haemodynamic parameter comparisons between the groups
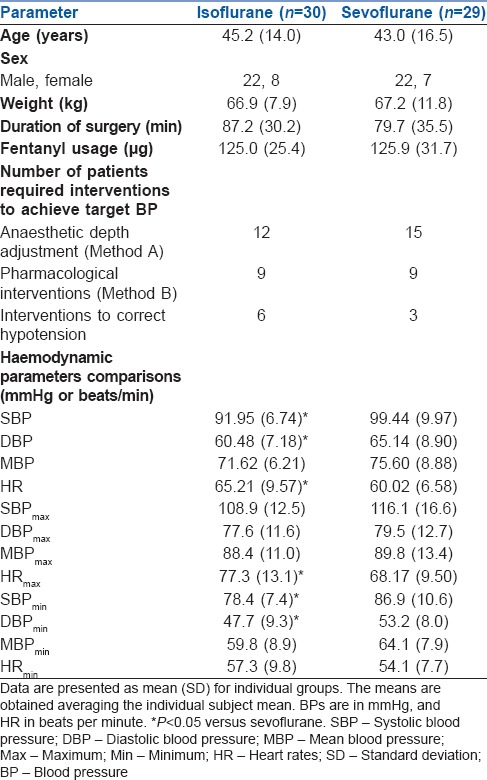
The primary targeted independent variable was the SBP, and co-variables were DBP and MBP. Significantly lower mean of mean SBP and DBP was recorded for isoflurane (independent sample t-test, P = 0.001, 0.032, respectively), but not for MBP (P > 0.05). The mean of mean heart rates achieved was significantly higher in the isoflurane group (P = 0.019 [Table 1]). The comprehensive list of maximum and minimum blood pressure and heart rate averages is included in Table 1.
The derived PCIs show higher values of Cp, Cpk and Cpm for all blood pressures (SBP, DBP and MBP) at predefined USLs and LSLs for isoflurane patients compared to sevoflurane [Table 2 and Figures 1, 2] suggesting superior capability of maintaining blood pressures and in achieving target defined. A higher number of patients in the sevoflurane group had ‘negative’ values for Cpk derived for all BP recordings [Tables 2 and 3] suggesting that the achieved BP parameters crossed the USLs more frequently in this subset.
Table 2.
Process capability report for systolic blood pressures of both groups, for overall and within processes and for two different specification limits (specification limits and extended specification limits)
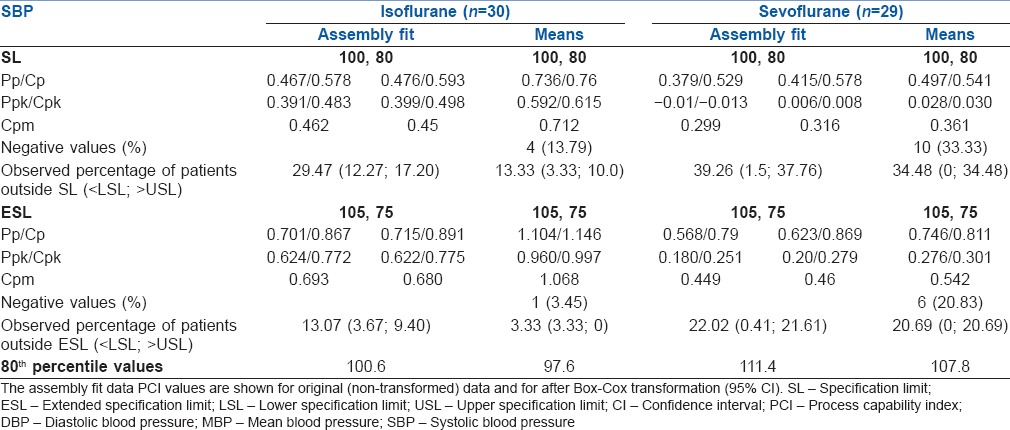
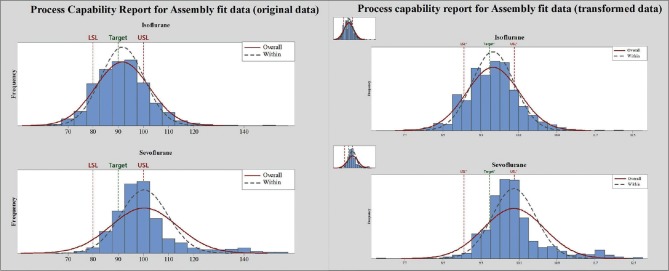
Figure 1.
The process capability reports of systolic blood pressures for assembly fit data. The graphs represent both for original (non-transformed) data and after Box-Cox transformation. The overall and within processes are shown. Data are in mmHg (original data). The LSL and USL lines represent SLs. The right corner minor images represent original data before transformation
Figure 2.
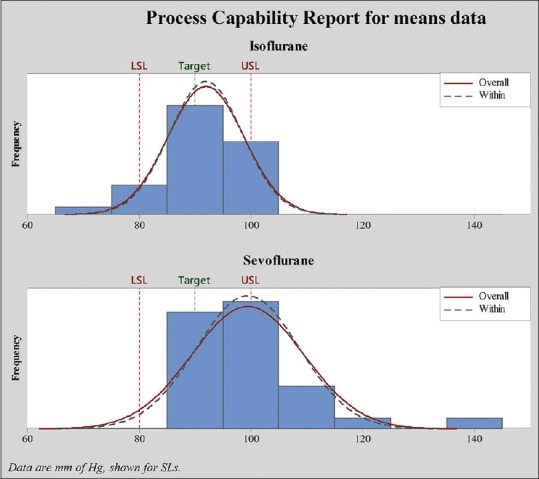
The process capability report of systolic blood pressures for means data. The overall and within processes are shown. Data are in mmHg. The LSL and USL lines represent SLs
Table 3.
Process capability report for diastolic blood pressures and mean arterial blood pressures of both groups and for two different specification limits (specification limit and extended specification limits)
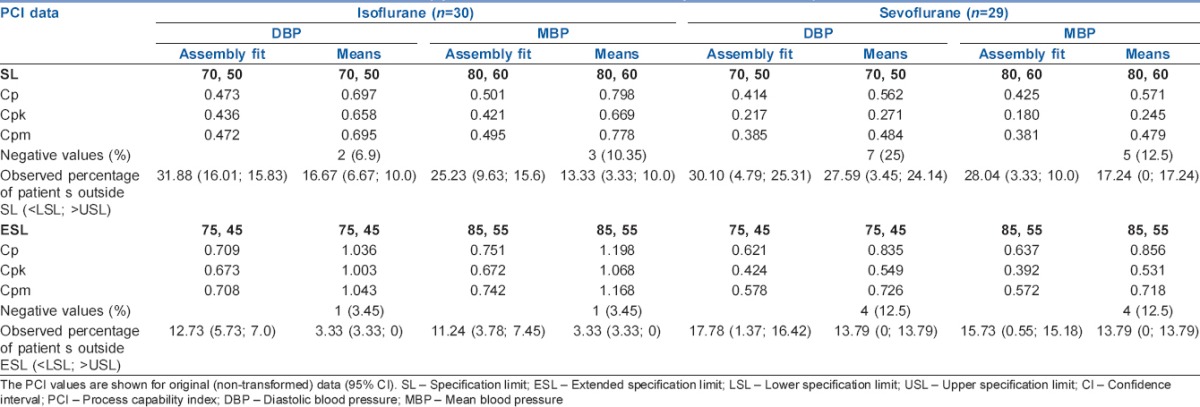
Probability plots distribution analysis revealed a higher percentage of patients outside the SLs and ESLs for all blood pressure readings (SBP, DBP and MBP) for sevoflurane vis-a-vis isoflurane and higher 80th percentile values of blood pressures for sevoflurane [Tables 2 and 3].
A comparable number of patients in both groups required either anaesthetic intervention, pharmacological manipulation or both to achieve the desired blood pressures [Table 1]. The episodes of hypotension requiring corrective interventions were higher in isoflurane patients. No perioperative surgical or anaesthetic complications were noted.
DISCUSSION
While comparison of the efficacy of isoflurane vis-a-vis sevoflurane in hypotensive anaesthesia for shoulder arthroscopy formed the primary objective of our study, a new analytical approach, process capability indices (PCIs), different from conventional statistical methodologies deriving significance from P values[7,8,9,10] was additionally deployed to derive more practical and meaningful conclusions. For various reasons (refer Flow chart), we felt that comparisons using conventional P values could highlight some but not all significant variations, and this could ultimately result in a divergence between ‘statistical’ significance and ‘clinical’ significance. For example, when the means (and SDs) of the SBPs in two groups (isoflurane and sevoflurane) were compared, lower mean SBP and minimum SBPs were achieved with isoflurane indicating its enhanced hypotensive action. Surprisingly, the mean MBP, DBPmax, SBPmax and MBPmax, min were not significantly different between the groups. Searching for a more inclusive analytical technique to overcome the possible inaccuracies of these comparisons, we found computing of PCIs[11,12] very useful and advantageous. As an indicator of how closely a process is able to match the output to its overall specifications and to predefined targets, it is widely employed as a statistical tool to assess production, quality and process improvement efforts in engineering design. PCIs measure patient volumes against predetermined parameter limits rather than vice-versa in conventional statistical analysis. Uniquely, this methodology, therefore, takes into account a multitude of influencing factors, both known and unknown, to provide us a ‘capability’ measure. In short, it evaluates ‘performance’ regardless of conventional P values.
The flow chart attempts to explain the role of each capability index. Cp indicates a limit distribution. A high value of Cp (close to 1) was observed in the isoflurane group considering SBP within 80 and 100 mmHg. This translated into 87% of patients in the isoflurane group maintaining SBPs between predefined limits vis-a-vis 65% of sevoflurane suggest superior ‘tolerance’ of isoflurane. Cpk is a trust index that reinforces Cp. The Cp and Cpk for blood pressures moved in consonance for isoflurane while following an off-process-centralisation with high variability for sevoflurane. We observed isoflurane group patients had higher Cpk values of 0.6 (for the range of 80–100 mmHg, sevoflurane 0.03) along with a greater percentage of negative Cpk value in the sevoflurane group of all blood pressure data. Both these findings confirm that the process mean has fallen out of USLs (blood pressure readings over 100 mmHg systolic, 3% isoflurane patients vs. 32% sevoflurane) thereby lending support to the superiority of isoflurane. Cpm herein specifically relates to a target blood pressure. Higher Cpm for isoflurane suggests that irrespective of the predefined range considered, the ease of achieving target blood pressure (90 mmHg SBP) was higher with this agent. Higher heart rates were recorded in the isoflurane group, but PCIs were not computed for this non-targeted parameter. However, but for the additional pharmacological interventions necessitated by isoflurane, heart rates recorded would possibly have been higher.
Cardiovascular effects specific to isoflurane have been detailed in several studies on animals,[9] human volunteers,[3] ASA1 patients[13] and in patients with coronary artery disease.[14] The circulatory effects of isoflurane are distinctly self-specific while sevoflurane resembles both isoflurane and halothane.[3,15] A study of isoflurane and sevoflurane in healthy volunteers by Philip Malan and colleagues demonstrated that dose-dependent decrease of MBP could be blunted by concomitant use of N2O.[3] Our study groups were comparable to these patients since N2O was used in all and the complete interscalene block created a pain-free status before inhalational agents were administered. However, if not for N2O usage, the hypotensive effect of isoflurane demonstrated in our patients could have been more profound. In horses, isoflurane-induced decrease in mean, systolic and diastolic BPs has been shown to be maximum at 80–100 min of anaesthesia.[9] Interscalene block has a potentiating effect on the hypotensive response of general anaesthesia.[16] A dose-dependent hypotensive effect for both the inhalational agents at 1–2 MAC has been established; each, however, having a different attributed mechanism of action.[17]
The variance in the magnitude of hypotension (isoflurane versus sevoflurane) is difficult to explain. Multiple animal as well as human volunteer studies have shown the myocardial depressant effects of regional anaesthetic drugs. Isoflurane acts synergistically with bupivacaine to decrease myocardial contractility in rats[18] clearly demonstrating the additive myocardial suppressive activity induced by regional anaesthetic used concomitantly with general anaesthesia. Bupivacaine at a plasma concentration of 3 × 10−5 mol/L, a level normally achieved during regional anaesthesia shows negative ionotropic effects (lower dP/dtmax) when administered with isoflurane. This has been attributed to decreased calcium release from sarcoplasmic reticulum. Levobupivacaine has a higher negative effect on isotonic relaxation (maxVr) than bupivacaine at equipotent plasma concentrations,[19] thus causing more diastolic dysfunction. Moreover, plasma concentrations are doubled under additional inhalational anaesthesia as compared to awake patients under local anaesthetic alone, and hence the effects too could be simply binary.[20,21] Lidocaine too has additive depressive effects on the myocardium.[18] We have used a mixture of both levobupivacaine and lidocaine but have not measured plasma concentrations. Animal studies have shown that the cumulative dose of bupivacaine required for inducing cardiac depression and arrhythmia is higher (though not statistically significant) with concomitant 1MAC sevoflurane vis-a-vis isoflurane.[22] It has been suggested that enhanced myocardial depression could result from a ‘fast in - slow out’ mechanism[23] of the local anaesthetic drug during repolarisation, in tandem with the heart rate. Our isoflurane patients did show higher heart rates than the sevoflurane group, but a simple extrapolation of our observations to explain the enhanced hypotensive effect may be an oversimplification.
This study has its pitfalls. The application of engineering indices for analysis of haemodynamic parameters in medicine may be questionable. Ninety-five percent confidence was used for power in contrast to true formulae of engineering indices where 99.99% confidence is routinely used.[11] The desired target blood pressure and SLs for blood pressures would be more meaningful if set for each individual patient rather than for a group. Individual variability of MAC, autonomic tone, etc., may have influenced the more sensitive haemodynamic parameters and therefore the study. For PCI analysis, the data should preferentially be normally distributed; if not, a Box-Cox or Johnson's data transformation should be attempted. Further, a 3-parameter distribution analysis with lowest AD statistic value too would best analyse non-normal data, but all these data transformations have their limitations. No follow-up data for delayed postoperative problems is evaluated.
CONCLUSION
This study confirms the superiority of isoflurane over sevoflurane in achieving target SBPs, a parameter that has been directly linked to intra-articular bleeding during arthroscopic procedures. We used PCIs as an additional practical tool that we believe, analyses better, the observed overall and within performances, with more valid outputs of ‘spec's which are independent of capability index values. Isoflurane can provide better intraoperative haemodynamic status as compared to sevoflurane in patients undergoing shoulder arthroscopic surgery with preliminary interscalene blockade. We also recommend that PCIs be more frequently used for analysing haemodynamic and other similar data (e.g., pain scores) in medical research to establish their true place among current statistical methodologies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We sincerely acknowledge Dr. Rajani Kadri, M.S., Associate Professor, Department of Ophthalmology, AJIMS, Mangalore, for her excellent support, contribution and cooperation during the preparation of manuscript. We also thank Mr. Naveen Mishra, for the kind help during manuscript preparation.
REFERENCES
- 1.Salem MR, Baraka AS. In: Control of circulation, part I. Wylie and Churchill. Davidson's A Practice of Anesthesia. Ch. II. Healy TE, Knight PR, editors. London: Arnold; 2003. pp. 203–19. [Google Scholar]
- 2.Duralde XA, editor. Rosemont: American Academy of Orthopaedic Surgeons; 2009. Bleeding problems during shoulder arthroscopy. In: Complications in Orthopaedics; Shoulder Arthroscopy. First Indian Pharmaceutical Edition, (AAOS monograph). Ch. 1; pp. 1–7. [Google Scholar]
- 3.Malan TP, Jr, DiNardo JA, Isner RJ, Frink EJ, Jr, Goldberg M, Fenster PE, et al. Cardiovascular effects of sevoflurane compared with those of isoflurane in volunteers. Anesthesiology. 1995;83:918–28. doi: 10.1097/00000542-199511000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Morrison DS, Schaefer RK, Friedman RL. The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy. 1995;11:557–60. doi: 10.1016/0749-8063(95)90131-0. [DOI] [PubMed] [Google Scholar]
- 5.Moppett IK, Mahajan RP. Transcranial Doppler ultrasonography in anaesthesia and intensive care. Br J Anaesth. 2004;93:710–24. doi: 10.1093/bja/aeh205. [DOI] [PubMed] [Google Scholar]
- 6.Nickalls RW, Mapleson WW. Age-related iso-MAC charts for isoflurane, sevoflurane and desflurane in man. Br J Anaesth. 2003;91:170–4. doi: 10.1093/bja/aeg132. [DOI] [PubMed] [Google Scholar]
- 7.Tantry TP, Muralishankar B, Adappa KK, Bhandary S, Shetty P, Shenoy SP. Target-controlled infusion (Propofol) versus inhaled anaesthetic (Sevoflurane) in patients undergoing shoulder arthroscopic surgery. Indian J Anaesth. 2013;57:35–40. doi: 10.4103/0019-5049.108559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryu JH, Sohn IS, Do SH. Controlled hypotension for middle ear surgery: A comparison between remifentanil and magnesium sulphate. Br J Anaesth. 2009;103:490–5. doi: 10.1093/bja/aep229. [DOI] [PubMed] [Google Scholar]
- 9.Raisis AL, Blissitt KJ, Henley W, Rogers K, Adams V, Young LE. The effects of halothane and isoflurane on cardiovascular function in laterally recumbent horses. Br J Anaesth. 2005;95:317–25. doi: 10.1093/bja/aei180. [DOI] [PubMed] [Google Scholar]
- 10.Watson KR, Shah MV. Clinical comparison of ‘single agent’ anaesthesia with sevoflurane versus target controlled infusion of propofol. Br J Anaesth. 2000;85:541–6. doi: 10.1093/bja/85.4.541. [DOI] [PubMed] [Google Scholar]
- 11.ªenvar O, Tozan H. Marmara University, Turkish Naval Academy Turkey, Process Capability and Six Sigma Methodology Including Fuzzy and Lean Approaches. 2010. [Last accessed on 2015 June 30]. pp. 153–78. Available from: http://www.cdn.intechopen.com/pdfs-wm/12326.pdf .
- 12.Lee S. Why do we read many articles with bad statistics.: What does the new American Statistical Association's statement on P-values mean? Korean J Anesthesiol. 2016;69:109–10. doi: 10.4097/kjae.2016.69.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frink EJ, Jr, Malan TP, Atlas M, Dominguez LM, DiNardo JA, Brown BR., Jr Clinical comparison of sevoflurane and isoflurane in healthy patients. Anesth Analg. 1992;74:241–5. doi: 10.1213/00000539-199202000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Rooke GA, Ebert T, Muzi M, Kharasch ED. The hemodynamic and renal effects of sevoflurane and isoflurane in patients with coronary artery disease and chronic hypertension. Sevoflurane Ischemia Study Group. Anesth Analg. 1996;82:1159–65. doi: 10.1097/00000539-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Eger EI, 2nd, Liu J, Koblin DD, Laster MJ, Taheri S, Halsey MJ, et al. Molecular properties of the “ideal” inhaled anesthetic: Studies of fluorinated methanes, ethanes, propanes, and butanes. Anesth Analg. 1994;79:245–51. doi: 10.1213/00000539-199408000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Janssen H, Stosch RV, Pöschl R, Büttner B, Bauer M, Hinz JM, et al. Blood pressure response to combined general anaesthesia/interscalene brachial plexus block for outpatient shoulder arthroscopy. BMC Anesthesiol. 2014;14:50. doi: 10.1186/1471-2253-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eger EI. In: Inhaled anesthetics: Uptake and distribution. Miller's Anaesthesia. Miller RD, editor. Philadelphia: Churchill Livingstone; 2010. pp. 531–59. [Google Scholar]
- 18.Takamura T, Sakamoto A, Ogawa R. Bupivacaine combined with isoflurane synergistically depressed myocardial contractility in rat working heart preparation. Nihon Ika Daigaku Zasshi. 1997;64:292–7. doi: 10.1272/jnms1923.64.292. [DOI] [PubMed] [Google Scholar]
- 19.David JS, Ferreti C, Amour J, Vivien B, Eve O, Petit P, et al. Effects of bupivacaine, levobupivacaine and ropivacaine on myocardial relaxation. Can J Anaesth. 2007;54:208–17. doi: 10.1007/BF03022642. [DOI] [PubMed] [Google Scholar]
- 20.Copeland SE, Ladd LA, Gu XQ, Mather LE. The effects of general anesthesia on whole body and regional pharmacokinetics of local anesthetics at toxic doses. Anesth Analg. 2008;106:1440–9. doi: 10.1213/ane.0b013e31816ba541. [DOI] [PubMed] [Google Scholar]
- 21.Feary DJ, Mama KR, Wagner AE, Thomasy S. Influence of general anesthesia on pharmacokinetics of intravenous lidocaine infusion in horses. Am J Vet Res. 2005;66:574–80. doi: 10.2460/ajvr.2005.66.574. [DOI] [PubMed] [Google Scholar]
- 22.Fukuda H, Hirabayashi Y, Shimizu R, Saitoh K, Mitsuhata H. Sevoflurane is equivalent to isoflurane for attenuating bupivacaine-induced arrhythmias and seizures in rats. Anesth Analg. 1996;83:570–3. doi: 10.1097/00000539-199609000-00023. [DOI] [PubMed] [Google Scholar]
- 23.Cox B, Durieux ME, Marcus MA. Toxicity of local anaesthetics. Best Pract Res Clin Anaesthesiol. 2003;17:111–36. doi: 10.1053/bean.2003.0275. [DOI] [PubMed] [Google Scholar]