Abstract
Context:
Surgical outcome of retropupillary fixation of iris claw lens.
Aims:
To evaluate the various indications, intra and post-operative complications, and visual outcome of retropupillary fixation of iris claw lens in aphakic eyes.
Settings and Design:
The study design is a retrospective study at a tertiary eye care center.
Methods:
Review of medical records of 61 aphakic eyes of 61 patients, who were rehabilitated with retropupillary fixation of an iris claw lens, with a follow-up duration of at least 1 year.
Statistical Analysis Used:
Data analysis was performed using paired t-test and Chi-square test.
Results:
Mean preoperative uncorrected visual acuity was 1.66 ± 0.3 LogMAR and postoperative acuity at 1 year was 0.53 ± 0.5 LogMAR (P = 0.00001). Preoperative distant best-corrected visual acuity was 0.30 ± 0.48 LogMAR and postoperative acuity at 1 year was 0.27 ± 0.46 LogMAR (P = 0.07). Mean preoperative astigmatism was 1.43 ± 1.94 D and postoperatively was 1.85 ± 2.16 D (P = 0.0127). Mean endothelial cell count was 2353.52 ± 614 cells/mm2 preoperatively which decreased to 2200 ± 728 cells/mm2 at 1 year follow-up (P = 0.006). There was no significant difference in central macular thickness and intraocular pressure pre and post-surgery. Complications included ovalization of pupil in 9.83%, hypotony in 1.63%, toxic anterior segment syndrome in 1.63%, cystoid macular edema in 11.47%, epiretinal membrane in 3.27%, and iris atrophy in 6.55%.
Conclusion:
Iris claw is a safe and an effective method of rehabilitating aphakic eyes.
Keywords: Aphakia, cystoid macular edema, retropupillary iris claw, specular microscopy
In the bag implantation of intraocular lens (IOL) is the basic standard of care in cataract surgeries. The lens is ideally placed in the capsular bag, which, provides a more physiological placement of lens as it is the closest to the nodal point of the eye.[1] This may not be possible in eyes with inadequate posterior capsular support, congenital and secondary weakness of the lens zonules. In such cases, the options available are anterior chamber IOL (ACIOL), retropupillary fixated iris claw lens or scleral fixated IOL (SFIOL). Implantation of ACIOL is debatable these days owing to its associated complications.[2] Iris-claw IOL and SFIOL are the preferred options. SFIOL has been studied extensively and has good visual outcome but for a few complications such as suture-related problems, cystoid macular edema, decentration, and pigment dispersion.[3,4] The knowledge regarding iris claw lens is limited, especially in Indian eyes.[5,6] This study has been conducted at tertiary eye hospital to evaluate the various indications, intra and post-operative complications and the visual outcome of retropupillary fixation of iris claw in aphakic Indian eyes. The study was approved by the Institution Ethical Committee.
Methods
This study is in accordance with the Helsinki declaration of 1975 as revised in 2000. This is a retrospective case series of 61 aphakic eyes of 61 patients. Of 61 patients, 33 were males and 28 were females. The mean age was 65 ± 2.7 years. A review of the medical records of patients who underwent retropupillary fixation of iris claw lens between January 2012 and December 2013 and completed a minimum follow-up of 1 year was done and the data obtained were included in the study. Patients with binocular surgical aphakia, aphakic patients with posterior segment pathologies such as cystoid macular edema, choroidal neovascular membrane, and aphakic eyes with insufficient iris tissue were excluded from the study. Data about distant uncorrected visual acuity (DUCVA), distant best-corrected visual acuity (DBCVA), intraocular pressure (IOP), keratometry, slit-lamp examination, posterior segment optical coherence tomography, and specular microscopy were gathered from medical records. In all the cases, indirect ophthalmoscopy was performed to screen for any peripheral retinal degenerations and barrage laser was done whenever necessary. In all cases, aphakic rehabilitation by iris claw was done 4 weeks after the primary surgery and was performed under peribulbar anesthesia by a single surgeon.
Excel iris claw lens (PIC 5590 model; Excel optics [p] Ltd., Chennai, India) with an optic size of 5.5 mm and total length of 9.00 mm was used for retropupillary fixation. IOL power was calculated using SRK T formula with an A constant of 117.2. Lens power needed for emmetropia was chosen.
All patients were informed about the risks and benefits of the surgery, and a written informed consent was obtained. The study was approved by the Institute Ethical Committee.
After making a superior scleral incision, two side port incisions at 3 and 9 o’clock positions were made. Adequate anterior vitrectomy and a peripheral iridectomy were done with the help of 23-gauge cutter when it was deemed necessary. The claw lens was introduced into the anterior chamber. The lens was stabilized with Shepard's forceps, and one haptic was placed under the iris in line with the side port. Reverse sinskey hook was passed through the side port, and enclavation was done by tucking a sufficient amount of the iris tissue. The end point was the presence of dimple at the enclavation site. Proper enclavation of iris claw lens was ensured at the end by looking for the presence of dimple on the iris. This would prevent the spontaneous de-enclavation of the iris claw lens. Similar procedure was repeated on the other side. Incision was secured with interrupted 10-0 nylon suture, and the conjunctiva was closed with 8-0 Vicryl suture. Patients were prescribed ofloxacin and dexamethasone eye drops which were tapered over 6 weeks.
Patients were called for follow-up on day 1, 1 week, 1, 3, and 6 months, and six monthly thereafter.
Data analysis was performed using paired t-test and Chi-square test and a 0.05 level of significance was considered.
Results
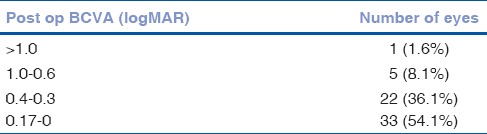
Retropupillary fixation of iris claw was done in 61 aphakic eyes of 61 patients. Preoperative barrage lasers for lattice degeneration were done in three (4.9%) eyes. All patients completed 1-year follow-up. Table 1 shows causes of aphakia in these patients. Mean preoperative DUCVA was 1.66 ± 0.3 LogMAR and mean postoperative DUCVA at 1 year was 0.53 ± 0.5 LogMAR (P = 0.00001) which was statistically significant [Figs. 1 and 2]. Preoperative DBCVA was 0.30 ± 0.48 LogMAR and postoperative mean DBCVA at 1 year was 0.27 ± 0.46 LogMAR. This was not statistically significant (P = 0.07) [Table 2]. Mean preoperative astigmatism was 1.43 ± 1.94 D and postoperatively at the end of 1 year was 1.85 ± 2.16 D. This difference was significant (P = 0.0127). Mean endothelial cell count was 2353.52 ± 614 cells/mm2 preoperatively which decreased to 2200 ± 728 cells/mm2 (11.76% decrease) at 1-year follow-up. The difference was statistically significant (P = 0.006). Mean central macular thickness (CMT) preoperatively was 228.72 ± 45.16 µm and at 1-year follow-up was 229.29 ± 46.38 µm which was not statistically significant (P = 0.44). Mean IOP preoperatively was 14.37 ± 5.44 mmHg and postoperatively was 14.32 ± 5.18 mmHg. Difference was not statistically significant (P = 0.45).
Table 1.
Causes of aphakia. Complicated cataract surgery was the most common cause
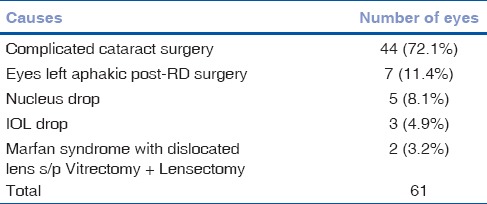
Figure 1.
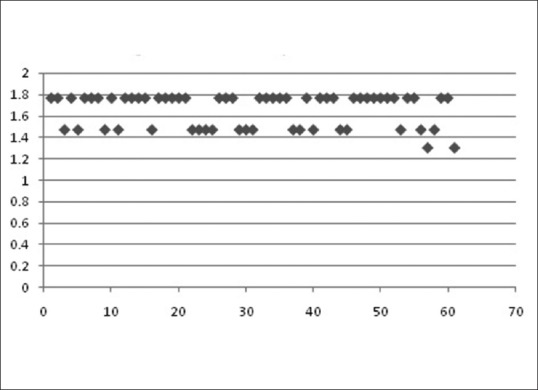
Preoperative uncorrected visual acuity (LogMAR)
Figure 2.
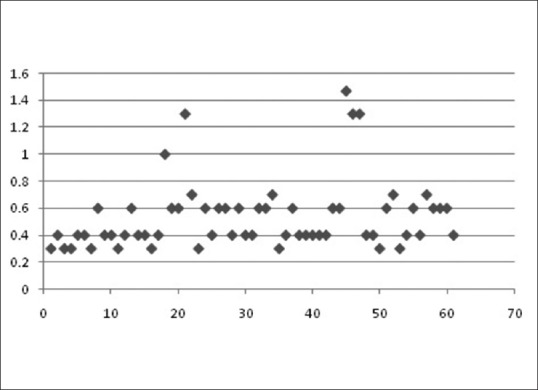
Postoperative uncorrected visual acuity (LogMAR)
Table 2.
Postoperative best-corrected visual acuity
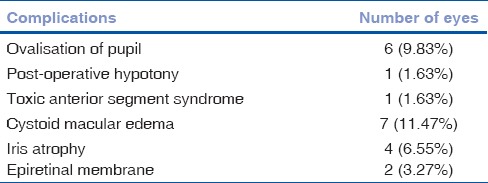
Intraoperative complications included ovalization of pupil in six (9.83%) eyes [Fig. 3b]. Early postoperative complications were hypotony in one (1.63%) eye and toxic anterior segment syndrome (TASS) in one (1.63%) eye. Delayed complications included cystoid macular edema in seven (11.47%) eyes and epiretinal membrane in two (3.27%) eyes. Iris atrophy was seen in four (6.55%) eyesm and none of these eyes had pigment dispersion. None of the eyes needed re-enclavation [Table 3].
Figure 3.
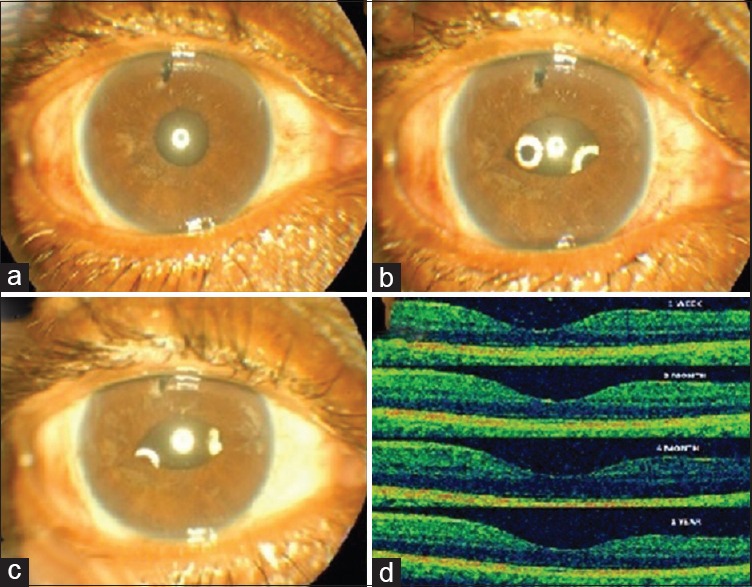
(a) Preoperative. (b) Day 1 postoperative showing ovalization of pupil and iris atrophy. (c) 1-year postoperative showing ovalization of pupil and iris atrophy. (d) Optical coherence tomography serial scan
Table 3.
Postoperative complications of retropupillary iris claw fixation. Cystoid macular edema and ovalization of pupil were the frequently encountered complications postoperatively
Discussion
Aphakia can be corrected by spectacle correction, contact lens, ACIOL, SFIOL, or retropupillary fixation of iris claw lens. Aphakic eyes rehabilitated with ACIOL have been found to have a favorable visual outcome but are associated with complications such as cystoid macular edema, ovalization of the pupil, pigment dispersion, and vitreous herniating anterior to the optic.[2,7] The SFIOL procedure has good visual outcomes but is known to be associated with long-term complications such as cystoid macular edema, retinal detachments, and suture-related complications.[3,8,9] Teng and Zhang compared anterior chamber implantation of iris claw lens with SFIOL and found that iris claw lens implantation can be performed less invasively, within a shorter surgical duration and is associated with faster visual recovery in comparison with SFIOL.[9] The safety and efficacy of aphakic rehabilitation with retropupillary iris claw fixation has been studied and it has been found to be a safe procedure for rehabilitation of aphakic eyes.[5,6,10,11] There are very few studies on this procedure in Indian eyes, and hence this study has been conducted.[5,6]
Postoperatively, the DUCVA improved by 1.12 LogMAR over preoperative DUCVA and DBCVA improved by 0.03 LogMAR over preoperative DBCVA. Other studies on retropupillary implantation of iris claw also reported similar improvement in DBCVA.[11,12] Mean preoperative DBCVA was 0.30 ± 0.48 LogMAR and mean postoperative DBCVA at 1 year was 0.27 ± 0.46 Log MAR. Preoperative DBCVA was achieved in 47 eyes (77.04%) by 1 month and 60 eyes (98.30%) by 3 months. In our series, 52 eyes (85.24%) achieved preoperative DBCVA [Table 4]. Of these 52 eyes, 23 eyes maintained preoperative visual acuity and 29 eyes had improvement in visual acuity. Gonnermann et al. reported that 97.1% of eyes achieved preoperative DBCVA and four eyes lost two or more lines of visual acuity, and the cause of decrease in vision was Cystoid macular edema (CME) in three cases and TASS with chronic glaucoma in one eye.[11]
Table 4.
Comparison of pre- and post-operative best-corrected visual acuity

In our series, nine eyes had postoperative DBCVA less than preoperative DBCVA. Of these nine eyes, six eyes (9.83%) had one line decrease in DBCVA, and three (4.91%) had more than two lines decrease in visual acuity, causes being epiretinal membrane (n = 2) and recurrent CME (n = 1). This difference in percentage of eyes achieving postoperative DBCVA may be because of the difference in the criteria chosen to define decrease in DBCVA. In this study, even one line decrease in DBCVA was considered. Instead, if two lines decrease in DBCVA were to be considered, then our study would have had only three (4.91%) eyes with more than two lines drop in DBCVA. This was comparable with the results of Gonnermann et al. (2.9%). Mean preoperative astigmatism was 1.43 ± 1.94 D and postoperatively was 1.85 ± 2.16 D (P < 0.05) which is consistent with Gonnermann et al.[11]
A subset of eyes which was left aphakic following a complicated cataract surgery had a low mean postoperative endothelial count (2212 cells/mm2) when compared to mean postoperative endothelial count (2269 cells/mm2), and it was not significant. Average endothelial loss in our study was 11.76% at the end of 1 year. Anbari and Lake studied endothelial cell loss in 16 cases of iris claw and reported a similar decrease in endothelial cell count postoperatively.[10]
In this study, CMT was measured in pre- and post-operative periods in all the cases, and there was no significant difference at the end of 1 year. So far in the literature, change in CMT has not been studied in eyes which have undergone iris claw lens implantation. [Fig. 3d] Gonnermann et al. reported CME in 12 out of 137 patients (8.7%). In our study, CME was seen in seven cases (11.47%) with a peak incidence at 6 months [Fig. 4].[11] All were initially treated with topical steroids (n = 4) and the resistant ones with posterior subtenon triamcinolone acetonide (n = 3). CME resolved in all the cases. One patient had recurrence of CME at 1 year follow-up. Other studies on ACIOL,[7] SFIOL,[4] and retropupillary fixation of iris claw[11] reported a similar incidence of CME.
Figure 4.
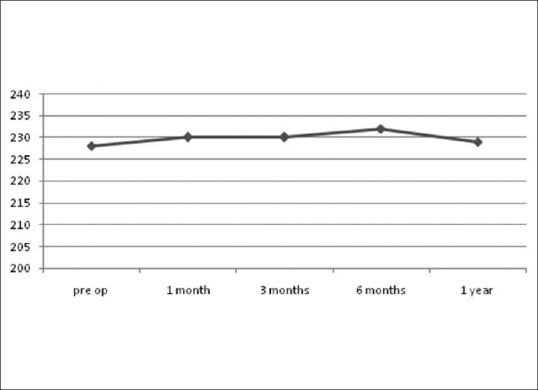
Central macular thickness
Although there was a slight increase in IOP at 1-week postoperative visit (19 ± 1.5 mm of Hg), there was no significant difference at 1 year. Anbari and Lake reported similar results. Initial increase in IOP was managed medically. We did not have any case of chronic secondary glaucoma at 1-year follow-up as reported by Schallenberg et al.[12]
Labeille et al. reported retinal detachment (four out of 32) and choroidal detachment (one out of 32).[13] No such sight-threatening complications have been noted in this study which highlights the importance of preoperative screening and treating peripheral retinal degenerations. Barrage laser was done for lattice degeneration in three cases in our study.
Gonnermann et al. reported disenclavation in 12 out of 137 cases (8.7%) which on an average occurred at 3.3 months postsurgery.[11] In our series, we had only iris atrophy [Fig. 3a–c] at the enclavation site was seen in four cases at the end of 1 year and none of our cases had dislocation unlike other studies.[10,14] Proper surgical technique with adequate iris tissue tuck will prevent disenclavation postoperatively.
Thus, implantation of the iris claw lens is a safe method of rehabilitating aphakic eyes. Meticulous preoperative screening for peripheral retinal degeneration with consequent barrage laser whenever necessary reduces the sight-threatening complications. To the best of our knowledge, this is the largest study of iris claw in Indian eyes. Limitations of this study include smaller sample size, no comparative group, and retrospective.
Conclusion
Iris claw is an effective method of rehabilitating aphakic eyes with very minimal complications that can be managed medically. The technique has an excellent visual outcome and can be performed by the primary cataract surgeon himself at a primary care center with the available equipment and a minimal learning curve.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ozcan AA, Ceran BB. Scleral fixation – Where are we. Int J Ophthalmol Eye Rec. 2014;2:1–2. [Google Scholar]
- 2.Ciccarelli EC. A study of 200 cases of anterior chamber implants. Ophthalmic Surg. 1985;16:425–32. [PubMed] [Google Scholar]
- 3.Luk AS, Young AL, Cheng LL. Long-term outcome of scleral-fixated intraocular lens implantation. Br J Ophthalmol. 2013;97:1308–11. doi: 10.1136/bjophthalmol-2013-303625. [DOI] [PubMed] [Google Scholar]
- 4.Kumar DA, Agarwal A, Prakash G, Jacob S, Saravanan Y, Agarwal A. Glued posterior chamber IOL in eyes with deficient capsular support: A retrospective analysis of 1-year post-operative outcomes. Eye (Lond) 2010;24:1143–8. doi: 10.1038/eye.2010.10. [DOI] [PubMed] [Google Scholar]
- 5.Rao R, Sasidharan A. Iris claw intraocular lens: A viable option in monocular surgical aphakia. Indian J Ophthalmol. 2013;61:74–5. doi: 10.4103/0301-4738.107198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patil KB, Meleth P, Shanker MP. Pars plana vitrectomy with posterior iris claw implantation for posteriorly dislocated nucleus and intraocular lens. Indian J Ophthalmol. 2011;59:497–500. doi: 10.4103/0301-4738.86321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nikica G, Ljerka HP, Jelena P, Metez-Soldo K, Mladen B. Cystoid macular edema in anterior chamber lens implantation following posterior capsule rupture. Doc Ophthalmol. 1992;81:309–15. doi: 10.1007/BF00161769. [DOI] [PubMed] [Google Scholar]
- 8.Yadav NK, Kemmanu V, Bhargava M, Shetty B. A truly knotless technique for scleral fixation of intraocular lenses: Two-year results. Indian J Ophthalmol. 2012;60:147–8. doi: 10.4103/0301-4738.90493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teng H, Zhang H. Comparison of Artisan iris-claw intraocular lens implantation and posterior chamber intraocular lens sulcus fixation for aphakic eyes. Int J Ophthalmol. 2014;7:283–7. doi: 10.3980/j.issn.2222-3959.2014.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anbari A, Lake DB. Posteriorly enclavated iris claw intraocular lens for aphakia: Long-term corneal endothelial safety study. Eur J Ophthalmol. 2015;25:208–13. doi: 10.5301/ejo.5000527. [DOI] [PubMed] [Google Scholar]
- 11.Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139–43. doi: 10.1016/j.jcrs.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 12.Schallenberg M, Dekowski D, Hahn A, Laube T, Steuhl KP, Meller D. Aphakia correction with retropupillary fixated iris-claw lens (Artisan) – Long-term results. Clin Ophthalmol. 2014;8:137–41. doi: 10.2147/OPTH.S55205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labeille E, Burillon C, Cornut PL. Pars plana vitrectomy combined with iris-claw intraocular lens implantation for lens nucleus and intraocular lens dislocation. J Cataract Refract Surg. 2014;40:1488–97. doi: 10.1016/j.jcrs.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 14.Farrahi F, Feghhi M, Haghi F, Kasiri A, Afkari A, Latifi M. Iris Claw versus scleral fixation intraocular lens implantation during pars plana vitrectomy. J Ophthalmic Vis Res. 2012;7:118–24. [PMC free article] [PubMed] [Google Scholar]


