Abstract
Purpose
To examine how tele-ICU nurse characteristics and organizational characteristics influence tele-ICU nurses’ trust and satisfaction of monitored bedside ICU nurses, and whether these influences are mediated by communication.
Materials and Methods
Data of tele-ICU characteristics and characteristics of the ICUs they monitored were collected at 5 tele-ICUs located throughout the country. 110 tele-ICU nurses at those tele-ICUs completed a questionnaire containing items related to their characteristics and their trust, satisfaction, and perceived communication with monitored bedside nurses. We analyzed the data using a hierarchical path model, with communication variables entered as mediators.
Results
Many of the tele-ICU nurse characteristics (age, currently or previously worked at the monitored ICU, hours worked per week, and years as a ICU nurse) had statistically significant direct effects on perception of communication timeliness, accuracy, and openness, as well as trust and satisfaction with monitored bedside ICU nurses. Communication openness mediated the relationships of both working at a monitored ICU and being older (≥55) on satisfaction. Communication accuracy mediated the relationships of both a specialized monitored ICU and working at a monitored ICU on trust.
Conclusions
Tele-ICUs and monitored ICUs should work to optimize communication so that trust can be established among the nurses.
Keywords: Telemedicine, tele-ICU, communication, intensive care units, satisfaction and trust
Introduction
The tele-intensive care unit (tele-ICU) allows critical care nurses and intensivists to monitor ICU patients from remote locations, using technology that allows them to assess the patient via video, keep track of the patient’s vital signs, communicate with doctors and nurses in the ICUs, and access the patient’s electronic medical records. One key characteristic of the tele-ICU is that the relationship between healthcare practitioners in the tele-ICUs and monitored ICUs is a form of virtual collaboration: “the process of two or more geographically separated health care providers collaborating via information technology to provide value-added health care delivery” [1]. The literature shows that virtual collaboration can be a double-edged sword: on the one hand it can improve resource utilization, lower costs, and increase flexibility, responsiveness, and timeliness, but on the other hand it can decrease individual commitment and autonomy; increase role overload, role ambiguity and workload; create communication problems and conflicts; and decrease trust [2–5].
Trust plays an important role as a foundation for effective collaboration[6–8]. In face-to-face interactions, trust is assumed to build gradually between people and within teams over time based on personal interaction and communication [9]. However, the literature has shown that in the absence of face-to-face contact it is difficult to build trust in virtual collaboration[6, 10, 11]. The technology (the EHR, e-care manager, video and audio) that replaces the face-to-face communication can undermine the emotional relationship aspects of trust[6, 10–12]. Familiarity between members of the tele-ICU team and monitored ICU team also needs to be considered. Results of a study by Mullen-Fortino et al. [13] show that 79% of ICU nurses agree with the statement that it is important (to them) that they are familiar with the tele-ICU physician, and 61% agree with the statement that ICU nurses are more likely to communicate with the tele-ICU if they personally know the physician. In fact, communication and interaction between the teams is infrequent. Results of this study showed further that only half of the nurses in their study reported being called three or more times in the preceding six months by the tele-ICU; nearly half (46%) reported never having contacted the tele-ICU themselves; and 44% reported regularly incorporating interventions suggested by tele-ICU staff. The lack of a shared social context and limitations on personal interaction and communication among members in virtual teams decrease the potential for trust [11, 12, 14].
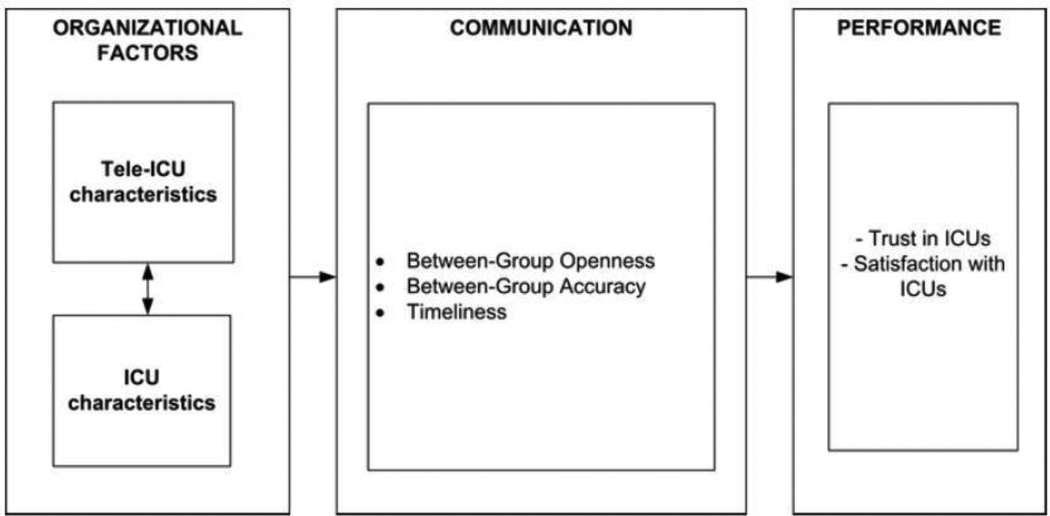
Shortell et al. [15, 16] developed and tested a model (see Figure 1) to describe the relation between managerial practices and organizational processes that are related to effective performance, defined in terms of quality and efficiency of care provided to patients. They hypothesized that “a team-oriented, achievement oriented culture and leaders who set high standards and provide necessary support provide more open, accurate, and timely communication, effective coordination with other units, and more open collaborative problems solving approaches. These, aspects, in turn, produce greater cohesiveness among team members resulting in the delivery of more effective patient care” [15]. In addition, results of a study by Jarvenpaa & Leidner [11] on communication and trust in virtual teams suggest that (1) (social) communication facilitates trust, (2) unequitable, irregular and unpredictable communication hinders trust, and (3) that communication timeliness and immediate feedback enhances trust.
Figure 1.
Factors affecting ICU performance (adapted from Shortell et al, 1991)
We know very little about communication between the tele-ICUs and the ICUs. It is unknown whether organizational factors at the tele-ICU and monitored ICU level can facilitate or hinder tele-ICU nurses’ perception of such communication. In addition, we do not know if quality communication between groups leads to a higher level of trust and satisfaction in the monitored ICUs. In this paper, we describe how we use a multiple case study research design approach to examine how tele-ICU nurse characteristics and monitored ICU characteristics influence tele-ICU nurses’ trust and satisfaction of monitored bedside ICU nurses, and whether these influences are mediated by communication.
Methods
Setting and sample
We collected data at 5 large tele-ICUs (two on the East coast, two in the Midwest and one on the West coast). Tele-ICUs needed to meet the following criteria to be included in the study:
-
-
Tele-ICU has existed for at least 1 year
-
-
Tele-ICU is connected to a minimum of two ICUs and one or more healthcare system(s)
-
-
One tele-ICU in the sample is an independent ICU that is not part of a healthcare system
-
-
On average, the tele-ICU employs a minimum of 25–30 nurses.
The last criterion was based on results of a power-analysis. We used the PASS 2008 (Power Analysis and Sample Size) software in order to determine the sample size. A power of .80 and an alpha value of .05 were used in the analyses. In order to detect a correlation of .30 we needed a sample size of 84 participants. Given an expected response rate of 60%, we needed to recruit at least 140 nurses. Therefore, we needed to ensure that each tele-ICU had a minimum of 25–30 nurses in order to achieve an overall target of 140 nurses.
Procedure
Data were collected during tele-ICU site visits. Before each site visit, the operations manager of the tele-ICU was sent a short questionnaire about characteristics of the tele-ICU and the ICUs that they monitored (see http://cqpi.wisc.edu/documents/Tele-ICU_Characteristic_Survey.pdf and table 1 for a summary of the characteristics). During the site visits, all nurses in the 5 tele-ICUs were asked to fill out a paper questionnaire and return the questionnaire in a locked mailbox in the unit. In total, 110 nurses filled out and returned the questionnaire. The overall response rate across all five tele-ICUs was 84%.
Table 1.
Characteristics of tele-ICUs, tele-ICU nurses, and monitored ICUs
| Tele-ICU Characteristics |
Years in existence (mean, min-max) | 6.2, 4–10 |
| Largest number of beds monitored per nurse (mean, min-max) | 44.4, 30–52 | |
| Tele-ICU Nurse Characteristics |
Hours worked per week (mean, min-max) | 26.6, 6–72 |
| Years of experience working as ICU nurse (mean, min-max) | 17.5, 0.3–37.8 | |
| Age, in years (%) | ||
| ≤ 34 | 8 | |
| 35–54 | 73 | |
| ≥ 55 | 19 | |
| Work at a monitored ICU (%) | 17.2 | |
| Monitored ICU Characteristics |
Closed [Intensivist present at all times] (%) | 19.3 |
| Specialized patient population [Cardiac, neuro, etc.] (%) | 27.8 | |
| Number of ICU beds (mean, min-max) | 12, 2–44 | |
| Years working with tele-ICU (mean, min-max) | 4.8, 0.6–11 | |
Questionnaire
We developed a questionnaire specific for nurses in the tele-ICU. The questionnaire included items related to:
Nurses’ characteristics, such as personal information (age, highest level of education) and work-related information (hours worked per week, whether the nurse works or has worked in an ICU that the tele-ICU monitors, and years of experience working as a nurse in an ICU),
Nurses’ trust and satisfaction of the bedside ICU nurses they monitor, rated on a scale of 1–10.
Nurses’ assessment of communication (on a scale from 1–5) with bedside nurses in 3 randomly-chosen ICUs they monitor. This resulted in total 321 assessments of communication between the tele-ICU nurse and nurses in the ICUs.
The measures of communication included 9 items that are grouped into 3 scales: (1) communication openness, (2) communication inaccuracy, and (3) communication timeliness. The communication scale measures were recoded to values between 0 and 100. These measures have been adapted from the Shortell and colleagues [15] questionnaire; extensive item analysis was performed to shorten the original scales of Shortell and colleagues and to produce reliable and valid scales that we have used in a study of ICU nurses [17]. The questionnaire was tested in a pilot study. See http://cqpi.wisc.edu/documents/Tele-ICU_Questionnaire.pdf for the full version of the questionnaire.
Data Analysis
The data from the tele-ICU nurses’ questionnaires were merged with the questionnaires of the tele-ICU’s characteristics and monitored ICUs characteristics, and then uploaded into Mplus for data analysis. The data collected had nested relationships at three levels (the monitored ICUs were nested in the tele-ICU nurses monitoring them, and the tele-ICU nurses were nested in the tele-ICUs employing them). However, the data were analyzed at two levels (monitored ICUs and tele-ICU nurses) for two reasons: 1.) To simplify the model and 2.) The variation at the level of the tele-ICU was minimal. Subsequently, the variables collected at the tele-ICU level that were entered into the model are disaggregated and analyzed at the level of the tele-ICU nurse. The resulting model is a two-level hierarchical path model used to analyze the effects of organizational factors, tele-ICU nurse characteristics, and perception of communication on tele-ICU nurses’ trust and satisfaction of monitored bedside ICUs.
The communication variables (communication openness, inaccuracy, and timeliness) were entered into the model as mediators, to assess the hypothesis that communication mediates performance (in this study, the performance of interest is trust and satisfaction). The indirect effects of the mediating variables were analyzed using a bootstrap distribution. This distribution was created by randomly sampling observations from the data set with replacement data and then multiplying the effect of independent variable on the mediating variable with the effect of the mediating variable on the dependent variable 1000 times [18]. All tests of significance were analyzed with an alpha of 0.05.
Results
Characteristics of the tele-ICUs, tele-ICU nurses, and monitored ICUs are presented in Table 1.
Communication between the tele-ICU and ICUs
Results in table 2 show that the mean scores for the different types of communication (openness, inaccuracy and timeliness) are relatively low (on a scale from 0–100). Results also show that there is considerable variation between the 5 tele-ICUs: the mean scores for communication in tele-ICU #2 are higher than, for example, tele-ICUs #3 and #5.
Table 2.
Communication between the tele-ICU and ICU monitored by tele-ICU on a scale from 0–100, mean scores and [standard deviations]
| Communication: Openness |
Communication: Accuracy* |
Communication: Timeliness |
|
|---|---|---|---|
| Tele-ICU #1 (n=62) | 58.1 [24.8] | 58.3 [18.7] | 52.2 [26.7] |
| Tele-ICU #2 (n=65) | 62.8 [21.5] | 73.1 [19.9] | 46.4 [22.9] |
| Tele-ICU #3 (n=33) | 53.0 [25.8] | 67.7 [23.5] | 45.8 [27.1] |
| Tele-ICU #4 (n=85) | 55.9 [22.9] | 64.3 [18.7] | 44.1 [23.7] |
| Tele-ICU #5 (n=76) | 53.1 [21.0] | 58.0 [15.9] | 51.5 [23.5] |
| Total (n=321) | 56.8 [23.0] | 63.8 [19.6] | 48.1 [24.5] |
Differences in communication between the tele-ICU nurses and ICU bedside nurses are significant at p<0.05
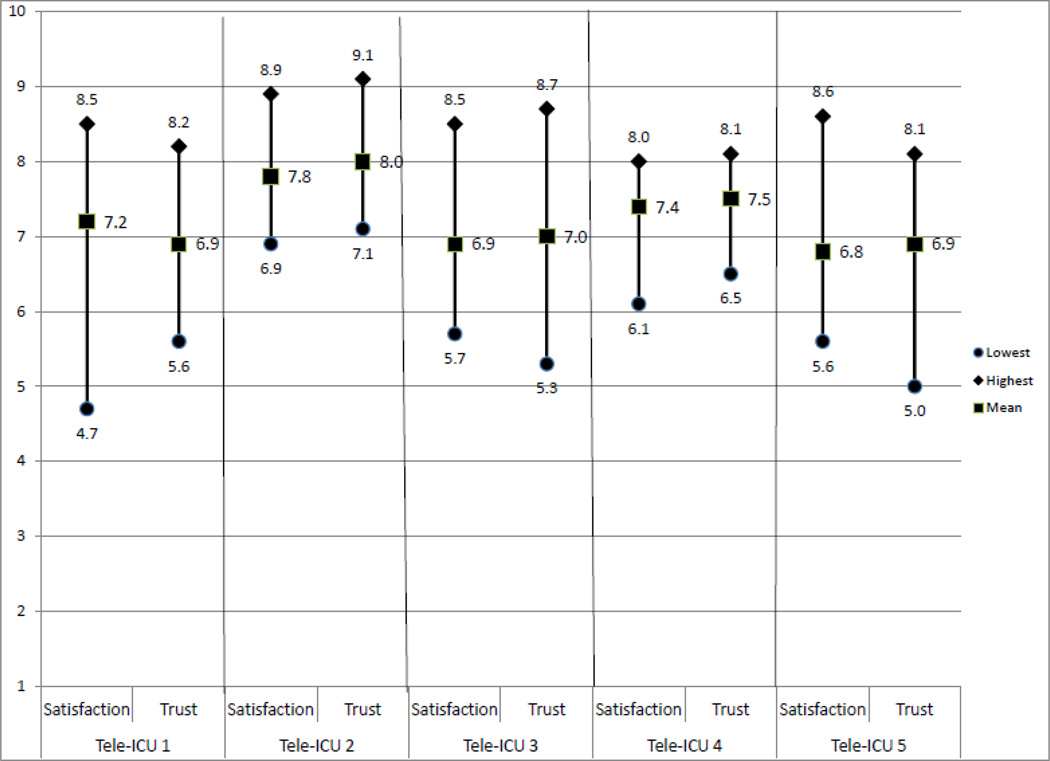
Satisfaction and trust
Figure 2 shows the mean scores for satisfaction and trust for all the ICUs that the tele-ICUs monitor. On average there are no statistically significant differences between the tele-ICUs. However, Figure 2 also shows the considerable variation of satisfaction and trust within the ICUs that are monitored by the tele-ICUs. The scores show that satisfaction with and trust in some ICUs is sometimes very low (e.g. a lowest score of 4.7 on a scale from 1–10 for satisfaction [tele-ICU #1] and a lowest score of 5.0 on a scale from 1–10 for trust [tele-ICU #5]).
Figure 2.
Satisfaction and trust between the tele-ICUs and ICUs by tele-ICU, mean, minimum and maximum scores
Effect of Communication on Trust and Satisfaction
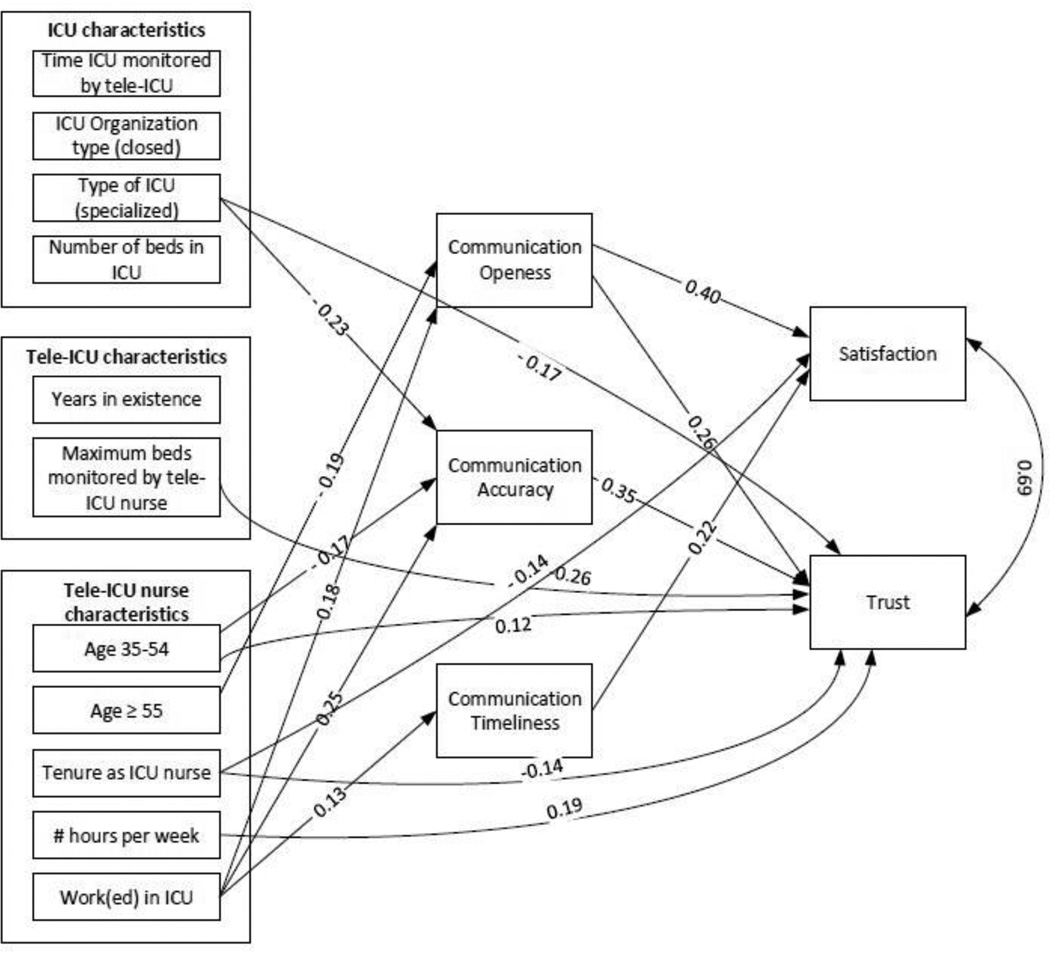
Figure 3 shows the statistically significant standardized paths of the direct effects of organization and nurse characteristics on communication, trust and satisfaction, as well as the direct effects of communication on trust and satisfaction. Tables of all direct and indirect relationships are available in the appendix/as online supplementary materials. All measures of communication—openness, inaccuracy, and timeliness—were associated with tele-ICU nurses’ trust or satisfaction on the ICUs they monitored. Communication openness was significantly associated with both trust (p<0.01) and satisfaction (p<0.001). Communication inaccuracy was significantly associated with less trust of the monitored ICUs (p<0.001). Lastly, communication timeliness was significantly associated with satisfaction of the monitored ICUs (p<0.05).
Figure 3.
Direct effects (standardized betas) of organizational and nurse characteristics on communication, satisfaction and trust
Organizational Factors
Tele-ICU nurses who needed to monitor more ICU beds had less trust in the monitored ICUs (p<0.05). The type of ICU being monitored also had an effect on tele-ICU nurses’ trust. Tele-ICU nurses had less trust in ICUs that were specialized to care for a specific patient population (such as cardiac or neurology patients) than general medical/surgical ICUs (p<0.01). In addition, ICUs with specialized patient populations had a negative effect on tele-ICU nurse’s perception of the accuracy of the communication received from the ICUs (p<0.01). The relationship between a specialized patient population and low levels of tele-ICU nurses’ trust is partially explained by their perception of inaccurate communication (p<0.05).
Nurse Characteristics
Many of the significant relationships involved characteristics at the tele-ICU nurse level. The longer the tele-ICU nurse had been working as an ICU nurse, the more negatively the nurse perceived trust (p<0.05) and satisfaction (p<0.05) with the monitored ICUs. Tele-ICU nurses who worked more hours each week had more trust in the monitored ICUs (p<0.05).
The age of the tele-ICU nurse was also associated with the perception of the communication received from the monitored ICU. Compared to younger tele-ICU nurses, older tele-ICU nurses (≥55 years old) were less likely to report experiencing open communication with the monitored ICUs (p<0.05) and this perception of communication openness mediates their low satisfaction in the monitored ICUs (p<0.05). Middle-aged tele-ICU nurses (35–54 years old) were more likely to assess communication as inaccurate (p<0.05), yet were more likely to trust the monitored ICUs (p<0.05) than younger tele-ICU nurses.
Tele-ICU nurses who have either previously worked or continue to work at a ICU that they also monitor in the tele-ICU showed significant associations with perception of communication, trust and satisfaction. Work in a monitored ICU was associated with higher perception of open communication (p<0.01), lower perception of inaccurate communication (p<0.001), and higher perception of communication timeliness (p<0.01). Communication inaccuracy mediated the relationship between tele-ICU nurses’ work history in a monitored ICU and increased trust (p<0.01) and communication openness mediated the relationship between tele-ICU nurses’ work history in a monitored ICU and increased satisfaction (p<0.05).
Discussion
Relatively little is known about communication between nurses in the tele-ICU and nurses in the ICUs that they monitor, and how this has an impact on satisfaction and trust between the tele-ICUs and ICUs. The literature shows that communication facilitates trust, and that trust is essential for collaboration. In face-to-face interactions, trust is assumed to build over time; but how is trust established in a virtual collaboration in which the different team members often have never met? In this study, we examined the relationship between organizational characteristics of the tele-ICU and the ICU and the characteristics of the tele-ICU nurses on communication, satisfaction and trust. Results show that – although the tele-ICU nurses’ perceptions of satisfaction and trust in the ICUs that they monitor are moderately high—there is considerable variation in these perceptions (see Figure 2). Results also show that there are differences in communication between nurses in the tele-ICU and the ICU that they monitor (see Table 2).
Results of our multi-level analysis show that there are moderately strong relationships between communication openness, inaccuracy and timeliness and satisfaction and trust in the ICUs. Several tele-ICU studies have stressed the importance of communication for effective team interaction [13, 19–21], but as far as we know this is the first study to demonstrate the impact of communication on satisfaction and trust. Results show that nearly all of the relationships between the organizational factors and satisfaction are mediated by communication but that there are some direct effects of organizational characteristics on, notably, trust. Most of these direct effects are related to tele-ICU nurse characteristics, such as age, tenure and number of hours per week that the nurses work in the tele-ICU. In general, older nurses (≥55 year old) and/or nurses with more years of tenure are less satisfied and express less trust with regard to the ICUs that they monitor. Results of a study designed to predict ICU nurses’ intention to use tele-ICU technology by Kowitlawakul [22] showed that nurses who had worked longer had more negative attitudes towards tele-ICU technology than younger nurses, which suggest that older nurses may have less trust in technology-mediated communication.
Results show further that few of the ICU characteristics in this study play a role in the relationship between communication and satisfaction and trust. Only the type of ICU (specialized) plays a minor role, and has a negative impact on communication accuracy and trust. One other study suggests that virtual collaboration with highly specialized ICUs may be more challenging than collaboration with general ICUs [23] Nurses and physicians in specialized ICUs have highly specific knowledge and skill sets and may be less willing to accept advice from outsiders, than nurses and physicians in general ICUs. The number of beds monitored by a tele-ICU nurse does have a negative impact on communication accuracy and on trust, which seems to indicate that a high workload can be detrimental to communication and trust. Interestingly, the history between the tele-ICU and the ICUs that they monitor does not play a role. The literature shows that in virtual collaboration in general levels of satisfaction and trust increase over time [11, 24, 25].
Finally, whether the tele-ICU nurse has worked or currently works in the ICU that is monitored is positively related to communication openness and timeliness and negatively related to communication inaccuracy. Results of other studies support the finding that knowing the virtual team members can increase communication and trust [26–28]. Tele-ICU #2 in our sample had actually set up a program to encourage ICU nurses to meet tele-ICU nurses [27]. Tele-ICU #2 scores highest on communication openness and timeliness and lowest on communication inaccuracy, and also has the highest satisfaction and trust scores of all tele-ICUs in our sample.
Study limitations
A limitation of this study was that we only examined the perceptions of tele-ICU nurses and not the perceptions of the nurses in the ICUs, or the experiences of physicians in the tele-ICU or ICUs. Another limitation was that, although the response rate in this study was high (84%) which increases generalizability of the study, in the survey nurses were randomly assigned only three of the ICUs that they monitored, and were asked questions about communication with regard to these three ICUs. In reality, tele-ICU nurses can monitor patients in more than 3 ICUs. However, we did not think that we could require tele-ICU nurses to answer more than three times the same questions about communication. This was a cross-sectional study; therefore the relationships between organizational characteristics, communication, and satisfaction and trust are not causal. In addition, we measured satisfaction and trust using a single item on a 1–10 scale. Further research on satisfaction and trust between nurses should explore satisfaction and trust as a more complicated constructs using more sophisticated tools.
Conclusions
The findings of this study demonstrate the importance of communication on tele-ICU nurses’ trust and satisfaction of monitored ICUs. As health care systems consider utilizing a tele-ICU for support of their bedside ICU nurses, it will be important to build relationships between the nurses who will be working together. ICUs and tele-ICUs should work to optimize communication so that trust can be established among the nurses. Future research should also explore the implications of low trust and satisfaction in virtual collaborations.
Supplementary Material
Acknowledgments
Funding: This study work was supported by the National Science Foundation [NSF Grant #: OCI-0838513]. The study was made possible with the cooperation from the 5 tele-ICUs, their managers and the nurses who work there.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Paul DL, Pearlson KE, McDaniel RRJ. Telemedicine: a virtual collaboration persepctive. Int J Healthcare Technology and Management. 2000;2(1/2/3/4):37–55. [Google Scholar]
- 2.Mowshowitz A. Virtual organization. Communications of the ACM. 1997;40(9):30–37. [Google Scholar]
- 3.Houghton GB, Marshall Scott P, Thomas LR. Interpersonal Traits, Complementarity, and Trust in Virtual Collaboration. J Manage Inf Syst. 2004;20(4):115–138. [Google Scholar]
- 4.Jarvenpaa SL, Knoll K, Leidner DE. Is anybody out there? Antecedents of trust in global virtual teams. Journal of Management Information Systems. 1998;14(4):29–64. [Google Scholar]
- 5.Caya O, Mortensen M, Pinsonneault A. Virtual Teams Demystified: An Integrative Framework for Understanding Virtual Teams. Int J e-Collab. 2013;9(2):1–33. [Google Scholar]
- 6.Paul DL, McDaniel RR. A field study of the effect of interpersonal trust on virtual collaborative relationship performance. Mis Quarterly. 2004;28(2):183–227. [Google Scholar]
- 7.Kramer RM. Trust and distrust in organizations: Emerging perspectives, enduring questions. Annu Rev Psychol. 1999;50:569–598. doi: 10.1146/annurev.psych.50.1.569. [DOI] [PubMed] [Google Scholar]
- 8.Rousseau DM, Sitkin SB, Burt RS, Camerer C. Not so different after all: A cross-discipline view of trust. The Academy of Management Review. 1998;23(3):393–404. [Google Scholar]
- 9.Mayer RC, Davis JH, Schoorman FD. An Integrative Model of Organizational Trust. The Academy of Management Review. 1995;20(3):709–734. [Google Scholar]
- 10.Paul DL. Collaborative activities in virtual settings: A knowledge management perspective of telemedicine. Journal of Management Information Systems. 2006;22(4):143–176. [Google Scholar]
- 11.Jarvenpaa SL, Leidner DE. Communication and trust in global virtual teams. Organization Science. 1999;10(6):791–815. [Google Scholar]
- 12.Nohria N, Eccles R. Face-to-face: Making network organizations work. In: Eccles NNR, editor. Networks and organizations: Structure, form, and action. Boston, MA: Harvard Business School Press; 1992. pp. 288–308. [Google Scholar]
- 13.Mullen-Fortino M, DiMartino J, Entrikin L, Mulliner S, Hanson CW, Kahn JM. Bedside Nurses’ Perceptions of Intensive Care Unit Telemedicine. American Journal of Critical Care. 2012;21(1):24–32. doi: 10.4037/ajcc2012801. [DOI] [PubMed] [Google Scholar]
- 14.O'Hara-Devereaux M, Johansen R. Global work: Bridging distance, culture, and time. San Francisco , CA: Jossey-Bass Publishers; 1994. [Google Scholar]
- 15.Shortell SM, Rousseau DM, Gillies RR, Devers KJ, Simons TL. Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse-physician questionnaire. Medical Care. 1991;29(8):709–726. doi: 10.1097/00005650-199108000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Shortell SM, Zimmerman JE, Rousseau DM, Gillies RR, Wagner DP, Draper EA, et al. The performance of intensive care units - does good management make a difference Medical Care. 1994;32(5):508–525. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Hoonakker PLT, Carayon P, Douglas S, Schulz K, Walker J, Wetterneck TB. Communication in intensive care units. In: Snelwar LL, Mascia FL, Meontedo UB, editors. Organizational Design And Management-IX. Santa Monica, CA: IEA Press; 2008. pp. 715–721. [Google Scholar]
- 18.Shrout PE, Bolger N. Mediation in Experimental and Nonexperimental Studies: New Procedures and Recommendations. Psychological Methods. 2002;7(4):422–445. [PubMed] [Google Scholar]
- 19.Stafford TB, Myers MA, Young A, Foster JG, Huber JT. Working in an eICU unit: life in the box. Crit Care Nurs Clin North Am. 2008;20(4):441–450. doi: 10.1016/j.ccell.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Young LB, Chan PS, Cram P. Staff acceptance of tele-icu coverage: A systematic review. Chest. 2011;139(2):279–288. doi: 10.1378/chest.10-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoonakker PLT, Carayon P, McGuire K, Khunlertkit A, Wiegmann D, Alyousef B, et al. Motivation and Job Satisfaction of Tele-ICU Nurses. Journal of Critical Care. 2013;28(3):315, e13–e21. doi: 10.1016/j.jcrc.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Kowitlawakul Y. The Technology Acceptance Model: Predicting Nurses' Intention to Use Telemedicine Technology (eICU) CIN: Computers, Informatics, Nursing. 2011;29(7):411–418. doi: 10.1097/NCN.0b013e3181f9dd4a. [DOI] [PubMed] [Google Scholar]
- 23.Siek T, Cox R, Schmidt J. American Telemedicine Association Thirtheenth Annual Meeting and Exposition. Seattle, WA: 2008. eICU impact in a rural community hospital. [Google Scholar]
- 24.Wilson JM, Straus SG, McEvily B. All in due time: The development of trust in computer-mediated and face-to-face teams. Organizational Behavior and Human Decision Processes. 2006;99(1):16–33. [Google Scholar]
- 25.Hill NS, Bartol KM, Tesluk PE, Langa GA. Organizational context and face-to-face interaction: Influences on the development of trust and collaborative behaviors in computer-mediated groups. Organizational Behavior and Human Decision Processes. 2009;108(2):187–201. [Google Scholar]
- 26.Roberts G, Dewoody S. Lights, camera, collaboration: implementation of an eICU orientation program. Critical Care Nurse. 2008;28(2):e12. [Google Scholar]
- 27.Goran SF. A second set of eyes: An introduction to tele-ICU. Critical Care Nurse. 2010;30(4):46–55. doi: 10.4037/ccn2010283. [DOI] [PubMed] [Google Scholar]
- 28.Mullen-Fortino M, DiMartino J, Entrikin L, Mulliner S, Hanson CW, Kahn JM. Bedside nurses' perceptions of intensive care unit telemedicine. American journal of critical care : an official publication, American Association of Critical-Care Nurses. 2012;21(1):24–31. doi: 10.4037/ajcc2012801. quiz 2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.