Summary
Objectives
This paper is a systematic literature review intended to gain an understanding of the most original, excellent, state-of-the-art research in the application of eHealth (including mHealth) in the management of chronic diseases with a focus on cancer over the past two years.
Method
This review looks at peer-reviewed papers published between 2013 and 2015 and examines the background and trends in this area. It systematically searched peer-reviewed journals in databases PubMed, Proquest, Cochrane Library, Elsevier, Sage and the Institute of Electrical and Electronic Engineers (IEEE Digital Library) using a set of pre-defined keywords. It then employed an iterative process to filter out less relevant publications.
Results
From an initial search return of 1,519,682 results returned, twenty nine of the most relevant peer reviewed articles were identified as most relevant.
Conclusions
Based on the results we conclude that innovative eHealth and its subset mHealth initiatives are rapidly emerging as an important means of managing cancer and other chronic diseases. The adoption is following different paths in the developed and developing worlds. Besides governance and regulatory issues, barriers still exist around information management, interoperability and integration. These include medical records available online information for clinicians and consumers on cancer and other chronic diseases, mobile app bundles that can help manage co-morbidities and the capacity of supporting communication technologies.
Keywords: eHealth, mHealth, chronic diseases, cancer, management, self-management, self- care
1 Introduction
This survey article focuses on significant developments in the use of eHealth and mHealth to manage chronic diseases with a special emphasis on cancer. The management of chronic diseases across the developed world and now, in the developing world, is becoming an increasing burden. The worldwide burden of non-communicable diseases is expected to increase from 46% in 2001 to 57% in 2020 [1]. The Global Burden of Disease Study [2] indicates that the world’s ageing population is leading to a substantial increase in the number of individuals with chronic diseases.
Cancer is no exception. In Australia, thanks to increased earlier detection and improvements in treatment, medical science is steadily improving survival rates. Recent estimates of cancer prevalence show that in 2012 there were approximately 775,000 people living in Australia who had been diagnosed with cancer in the previous 26 years, including 339,000 in the previous five years [3].
As a result health authorities are seeking to lessen the burden by using technology to support a move towards self-care and outpatient long-term monitoring [4].
“eHealth” has many definitions. The term can cover a wide range of technologies including computers, telephony and wireless communications to provide access to health care providers, consumers, care management and education. The World Health Organisation [5] sees eHealth as a generic term, which includes four distinct but related components.
Mobile Health (mHealth): Provision of health services and information via mobile and wireless technologies;
Health Information Systems (HIS): Including electronic patient records and administrative systems;
Telemedicine: Provision of health care services at a distance; can be used for inter-professional communication, patient communication and remote consultation; and
Distance Learning (eLearning): Education and training in electronic form for health professionals.
For the purposes of this paper, mHealth is defined as a subset of eHealth that delivers such services via mobile and wireless technologies [6]. The paper has focused on the first three components, which in the view of the authors have the most potential to lessen the burden of chronic diseases by supporting a move towards self-care and outpatient long-term monitoring.
2 Objective
The objective of this article is to undertake a systematic review of the most original, state-of-the-art research in the application of eHealth (including mHealth) in the management of chronic diseases with a focus on cancer over the past two years. The review will examine how they provide solutions to new and emerging problems.
The questions to be answered were:
What are the most relevant technical advances made in the last two years to advance the use of eHealth (including mHealth) to manage cancer and other chronic diseases?
What are differences between developed and developing countries in how eHealth and mHealth solutions are being applied?
What are the implications for management and self-management of cancer and other chronic diseases?
What Sociotechnical Factors are affecting usability and take-up?
3 Methodology
A structured literature review [7] was adapted. The process developed for the literature review included:
The first step to identify the relevant resources was to establish the relevant keywords. This was carried out following the experimental method given by Dieste et al. 2009. We conducted a broad search using the terms Chronic Diseases, Cancer, eHealth and Developing Countries.
Once we determined the keywords, we searched the databases listed in Point 5 below to find relevant studies in the field. For the initial screening, only titles, abstracts and keywords were considered.
The following search phrases were used while querying each database – e.g. the second search indicated that the article should contain the word ‘eHealth’ along with any of ‘management’ or ‘self-management or self-care’ in its title, keywords or abstract.
Three iterations were then conducted and peer reviewed articles were selected on the criteria of relevance and publication date between 2013 an 2015. The iterations are illustrated in Diagram 1 below.
The systematic review used Endnote Version 7 to document search results of peer-reviewed journals in databases PubMed, Proquest, Cochrane Library, Elsevier, Sage and the Institute of Electrical and Electronic Engineers (IEEE Digital Library).
3.1 Queries
We organised queries around three broad categories adapted from an existing methodology [8]:
Context: Cancer, Chronic Disease Management, Self-Management, Self-Care, eHealth, mHealth, Biomedical Technology drawn from peer-reviewed articles in Journals published after December 2013.
Mechanisms: Methods to apply eHealth, including mHealth solutions to improve the management, self-management and self-care of cancer and other chronic diseases in developed and developing countries.
Impacts/outcomes: Measurable health and efficiency outcomes based on repor ted findings. Acceptance and Take-Up of eHealth.
The other search terms such as telemedicine, medical informatics, telehealth, electronic medical records may also return “eHealth” initiatives. Using only eHealth presents a risk that any search may be restrictive in scope and misses some papers written in this domain. However the authors took the view that the term “eHealth” has become widely recognized as the dominant term, especially in the last two to three years. Given this chapter is intended to give an overview of developments in eHealth for that period, it was considered that use of this term would be sufficient and the risk would be acceptable.
While there is considerable “grey” literature published on this topic, which can often be more current, the authors have restricted their search to peer reviewed journals in an effort to maintain academic rigour.
Advanced searches were conducted and are listed below:
3.2 Selection of Studies
The process for selecting studies is shown in Figure 1.
Fig. 1.
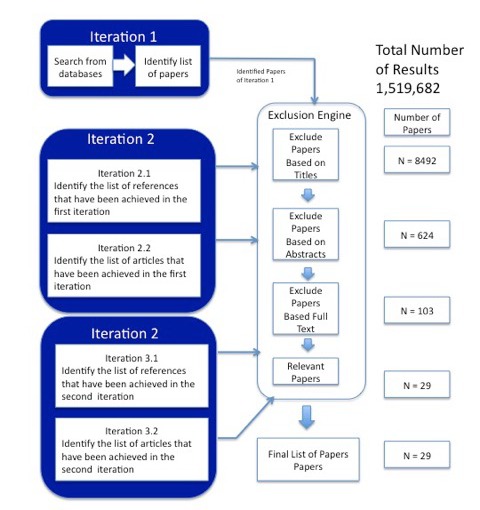
Selection of Studies. Source: Adapted from (Bakshi, Talaei-Khoei et al. 2013) [7]
Selecting studies involves filtering relevant papers from the initial list. The first iteration involved searching for the selected keywords over the seven databases and excluding papers based on titles, keywords, abstracts and full text. This removed articles that did not address our exclusion criteria:
Did not focus on eHealth or mHealth;
Did not focus on cancer and other chronic diseases;
Were not peer reviewed;
Were written in languages other than English;
Were not available online;
Were not in the relevant fields or could not be applied to the relevant fields; and
Were published no earlier than 2013.
The last requirement was a major factor in the large reduction from over 1.5 million results to 8,492. The other factor was a manual review of titles returned that restricted the relevance of application to medicine and health related activities.
The second iteration had two sub-iterations (I) searching the references of the papers found in the first iteration and (II) searching the papers, which cited the found papers in Iteration 1. This was done using the University of NSW Library search facility. In each of these two sub-iterations, we applied the exclusion criteria and excluded papers not based on the above criteria. Iteration 2 found 21 papers.
In Iteration 3 we repeated the above process on the papers found in Iteration 2. This added eight papers giving a total of 29 of which all seven came from cited papers.
Once papers were excluded based on titles and abstracts, the papers were read and the results summarized in a Summary Table. An extract from the summary table is shown below (Figure 2). The entire completed table is in Appendix A.
Fig. 2.
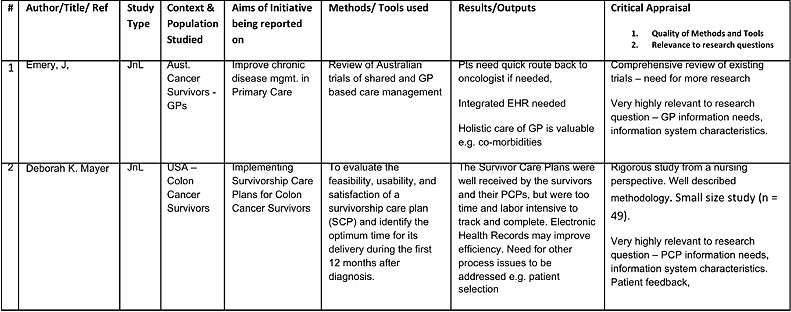
Summary Table
3.3 Data Extraction and Synthesis
In the data extraction and synthesis phase the key details from the selected papers were obtained. In this review the information extracted was divided into the four themes listed below. Table 2 shows how each of the articles contributed to each theme. A small number of referenced articles were not included in table 2 as they were only relevant either for the Introduction or the Methodology.
Table 2.
Themes and Articles
| Theme | Article |
|---|---|
| Technical Advances | National Health Service. Biotechnology; New Findings in Biomedical Informatics Described from NHS Foundation Trust (Exploring medical device design and use through layers of Distributed Cognition: How a glucometer is coupled with its context). Biotech Week; 2015:891 |
| Castelnuovo G, Mauri G, Simpson S, Colantonio A, Goss S. New Technologies for the Management and Rehabilitation of Chronic Diseases and Conditions. Biomed Res Int 2015;2015:180436. | |
| Conway A, Inglis SC, Clark RA. Effective Technologies for Noninvasive Remote Monitoring in Heart Failure. Telemed J E Health 2014 Jun;20(6):531-8. Jameson JL, Longo DL. Precision Medicine — Personalized, Problematic, and Promising. N Engl J Med 2015 Jun 4;372(23):2229-34. | |
| Jansen F, van Uden-Kraan CF, van Zwieten V, Witte BI, Verdonck-de Leeuw IM. Cancer survivors’ perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer 2015 Jun;23(6):1679-88. | |
| Kerr C, Murray E, Stevenson F, Gore C, Nazareth I. Interactive health communication applications for chronic disease: patient and carer perspectives. J Telemed Telecare 2005;11 Suppl 1:32-4. | |
| Mendoza G, Levine R, Kibuka, T, Okoko L. mHealth Compendium, Volume Four. Arlington, VA: African Strategies for Health, Management Sciences for Health; October 2014. | |
| Moja L, Kwag KH, Lytras T, Bertizzolo L, Brandt L, Pecoraro V, et al. Effectiveness of Computerized Decision Support Systems Linked to Electronic Health Records: A Systematic Review and Meta-Analysis. Am J Public Health 2014 Dec;104(12):e12-22. | |
| Differences between developed and developed countries | Ahmed T, Lucas H, Khan AS, Islam R, Bhuiya A, Iqbal M. eHealth and mHealth initiatives in Bangladesh: A scoping study. BMC Health Serv Res 2014 Jun 16;14:260. |
| Khatun F, Heywood AE, Ray PK, Hanifi SM, Bhuiya A, Liaw ST. Determinants of readiness to adopt mHealth in a rural community of Bangladesh. Int J Med Inform 2015 Oct;84(10):847-56. | |
| Meier CA, Fitzgerald MC, Smith JM. eHealth: Extending, Enhancing, and Evolving Health Care. Annu Rev Biomed Eng 2013;15:359-82. | |
| Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I et al; Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743-800. | |
| Implications for Management | Emery J. Cancer survivorship - the role of the GP. Aust Fam Physician 2014 Aug;43(8):521-5. |
| Erfani SS, Abedin B. Effects of Web based cancer support resourcesuse on cancer affected people: A systematic literature review. The International Technology Management Review 2014;4(4):201-11. | |
| Forczek E, Makra P, Lanyi CS, Bari F. The Internet as a New Tool in the Rehabilitation Process of Patients-Education in Focus. Int J Environ Res Public Health 2015 Feb 23;12(3):2373-91. | |
| Jansen F, van Uden-Kraan CF, van Zwieten V, Witte BI, Verdonck-de Leeuw IM. Cancer survivors’ perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer 2015 Jun;23(6):1679-88. | |
| Khan NF, Evans J, Rose PW. A qualitative study of unmet needs and interactions with primary care among cancer survivors.” Br J Cancer 2011 Nov 8;105 Suppl 1:S46-51. | |
| Mayer D, Gerstel A, Walton AL, Triglianos T, Sadiq TE, Hawkins NA, Davies JM. Implementing Survivorship Care Plans for Colon Cancer Survivors.” Oncol Nurs Forum 2014;41(3):266-73. | |
| Roorda C, Berendsen AJ, Haverkamp M, van der Meer K, de Bock GH. Discharge of breast cancer patients to primary care at the end of hospital follow-up: A cross-sectional survey. Eur J Cancer 2013;49(8):1836-44. | |
| Zulman D, Jenchura EC, Cohen DM, Lewis ET, Houston TK, Asch SM. How Can eHealth Technology Address Challenges Related to Multimorbidity? Perspectives from Patients with Multiple Chronic Conditions. J Gen Intern Med 2015;30(8):1063-70. | |
| Sociotechnical Factors | Atun R. Transitioning health systems for multimorbidity. Lancet 2015; 386(9995):721-72. |
| Chen Z, Koh PW, Ritter PL, Lorig K, Bantum EO, Saria S. Dissecting an Online Intervention for Cancer Survivors: Four Exploratory Analyses of Internet Engagement and Its Effects on Health Status and Health Behaviors. Health Educ Behav 2015;42(1):32-45. | |
| El-Gayar O, Sarnikar S, Abdullah Wahbeh A. On the Design of IT-Enabled Self-Care Systems: A Socio-technical Perspective. System Sciences (HICSS), 2013 46th Hawaii International Conference on; 2013. | |
| El-Gayar OF, Deokar AV, Wills MJ. Evaluating task-technology fit and user performance for an electronic health record system. International Journal of Healthcare Technology and Management 2010;11(1-2):50-65. | |
| Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health Care Provider Adoption of eHealth: Systematic Literature Review. Interact J Med Res 2013 Apr 16;2(1):e7 Ruland CM, Maffei RM, Børøsund E, Krahn A, Andersen T, Grimsbø GH. Evaluation of different features of an eHealth application for personalized illness management support: Cancer patients’ use and appraisal of usefulness. Int J Med Inform 2013;82(7):593-603. |
4 Findings
Advances in the use of eHealth in the management of cancer and other chronic diseases continue to accelerate in areas like targeted treatment; community based monitoring and consumer self-management. The application of data analytics to management of chronic diseases is also starting to have a significant impact, but much has already been published in that area. For this reason the review only briefly covers data analytics within the context of the broad themes outlined below:
The findings are divided into four broad themes:
-
Technical Advances
The widespread adoption of eHealth and mHealth technologies are enabling earlier diagnosis and better monitoring, early risk detection, more targeted treatment and rehabilitation plus provision of feedback and alerts [4].
-
Differences between Developed and Developing Countries
According to the Global Burden of Disease Study, chronic diseases are rapidly increasing in developing countries with non-fatal outcomes rapidly becoming the dominant source of burden of disease outside of sub-Saharan Africa [2]. However many developing countries are applying innovative eHealth solutions to address this.
-
Implications for Management and Self-Management
Self-care and self-management are becoming more important in the management of cancer and other chronic diseases. Self-care can be supported by an increasing range of Internet based applications which enable new forms of healthcare and can make doctor-doctor, doctor-patient, patient-patient relationships independent of geographical location [9].
-
Socio-technical Factors affecting Usability and Take-Up
One key finding of much of the literature reviewed is that eHealth applications need to be easy to use and easily accessible, taking account of human-computer interaction issues and socio-technical factors. Such pervasive IT-enabled systems for self-care and self-management applications should address the holistic needs of consumers and be built following socio-technical principles and components (El-Gayar, Deokar et al. 2010). eHealth implementation is frequently a disruptive change in the health care workplace. It is likely to require changes in individual job design and clinical pathways to efficiently incorporate technology [10].
These are further discussed below.
4.1 Technical Developments
New technologies enable many more treatments and chronic disease management options for both clinicians and patients. Such solutions extend across the entire spectrum of care and include “diagnostic and monitoring, early risk detection, treatment and rehabilitation, provision of feedback and alerts, and motivational strategies that facilitate changes in dysfunctional behaviors or maintenance of healthy lifestyle” [4].
Bio-medical Devices
Biomedical devices such as glucometers, used to measure blood sugar levels, now need to be interconnected with other medical devices and electronic medical record systems. The information produced by such devices is more useful if it is considered within the overall context of patient care along with other vital signs, for example blood pressure, temperature and weight. The UK NHS Foundation Trust has applied Distributed Cognition Theory, to provide a level of artificial intelligence to explore how an inpatient blood glucose meter is coupled with the context in which it is used. The analysis is based on a study of clinicians using a newly introduced glucometers on an oncology ward. It enabled researchers to improve the basic mechanics of the system, incremental design considerations, and larger design considerations (NHS Foundation (2015). Developing “smart” contextual medical devices will support more accurate diagnosis and monitoring, support self-management and self-care once a patient returns to the community.
Another biomedical innovation is a stethoscope that can be attached to a mobile phone, enabling patients to monitor their own lung health. This study was designed to address a 40% post-diagnosis death rate, due to cardiac arrest, of patients with tuberculosis-related pericarditis [11].
Other biomedical devices now emerging which support improved management of chronic diseases include a rehabilitation system for stroke patients using vibrotactile feedback, a new system of facial movement analysis for facial paresis, an exploration of the effects of exercise for dialysis and cancer patients, and the influence of environment on those with dementia and coronary artery disease [4].
Non-Invasive Remote Monitoring
Smart phones and other mobile devices now have the capacity of a personal computer and when coupled with even a basic Internet connection, can enable greater self-care and self-management of cancer and other chronic diseases. This factor, together with the increased burden of chronic diseases and the high cost of acute care has generated greater interest in remote monitoring models for delivering care. Such models depend upon rapidly developing eHealth and especially mHealth technology such as “tele-monitoring (transfer of physiological data such as blood pressure, weight, electrocardiographic details, and oxygen saturation through telephone or digital cable from home to healthcare provider)”[12].
A recent Cochrane Review [12] has confirmed the value of non-invasive tele-monitoring for people with heart failure can reduce mortality by 20%, reduce or shorten heart failure related hospitalisations by 29%. Combined with structured telephone support, it reduced all-cause mortality by 13% and in the process delivered an acceptable experience for patients. Remote monitoring will be especially relevant to patients who face issues of distance or lack of mobility.
This is but one example of how eHealth and mHealth “can improve health outcomes, quality of life, and well-being and facilitate functional patient empowerment and engagement” [4]. mHealth, used with such devices as implants and biomedical sensors has the potential to be a disruptive technology which could overcome many of the limitations associated with the traditional, restricted, and highly expensive in-patient treatment of many chronic pathologies. The model would enable chronic disease management to be tailored to the specific needs of the individual [4].
Precision Medicine
Precision medicine is another example of a disruptive technology, where an innovation will change how health services are delivered by altering existing clinical guidelines and the relationships between providers, payers and consumers. Precision medicine is “treatments targeted to the needs of individual patients on the basis of genetic, biomarker, phenotypic, or psychosocial characteristics that distinguish a given patient from other patients with similar clinical presentations” [13].
It is now apparent that cancer is not one, but many diseases which can effect outcomes differently for individuals according to their genetic make-up and lifestyle. It is the same for many other chronic diseases and this is what makes precision medicine so attractive. It promises personalized treatment. For example, in cancer chemotherapy it is often not possible to see whether an anti-cancer drug is going to be effective unless it is tried. With better diagnostic tests based on individual genomics, it will be possible to predict a drug’s effectiveness in advance, so avoiding unnecessary side effects for the patient and unnecessary cost for the health system. Such advances in individual genomics together with better imaging and bioinformatics will enable smaller and faster trials. All such trials would involve an initial screening step to identify any mutations responsible for an individual’s cancer. It is then possible to perform genomic sequencing to determine if that particular cancer will respond to targeted therapy [14]. The implications for eHealth will be that genetic information will become an essential part of any Electronic Health Record, with all the privacy, data ownership and security obligations that go with it.
eHealth capability is supported by sound information management and health informatics standards – such as the SNOMED nomenclature and ICD10 classification. To support precision medicine eHealth systems will need to manage greater complexity of progressively more detailed classifications of diseases, with more precise definitions. Jameson states that advances in genetics and biomarkers will increase the pressure for more precise definitions and classifications, which eHealth systems will need to handle [13].
4.2 Differences in eHealth between Developed and Developing Countries
Chronic diseases, including cancer are emerging as major burdens in developing countries. According to the World Health Organisation in five out of the six WHO regions, deaths caused by chronic diseases now dominate the mortality statistics. The trend is accelerating and the shift is occurring at a faster rate in developing countries than it did in developed countries half a century ago. The WHO warns that this rapid rate of change, together with the increasing burden of disease, is creating a major public health threat, which demands immediate and effective action (http://www.who.int/nutrition/topics/2_background/en/). This prompts the need for a radical rethink of health systems especially in developing countries [1].
In developed countries eHealth is about applying information technology to improve the efficiency and effectiveness of health-care delivery, while in emerging and developing countries it is about providing access to basic health-care for people, usually experiencing poverty or disadvantage who do not have any access using lower cost technology such as mobile phones.
One example of a developing country that is moving decisively to adopt eHealth and mHealth to initiate innovative ways to manage chronic diseases is Bangladesh. Bangladesh is acknowledged as a leading developing country in the innovative use of eHealth, especially mHealth. A recent review [15] of developing countries health systems concluded that “Bangladesh has made enormous health advances and now has the longest life expectancy, the lowest total fertility rate, and the lowest infant and under-5 mortality rates in south Asia, despite spending less on health care than several neighbouring countries. ”Much of this can be attributed to the contribution of a web based electronic health record and mHealth [16]. There are over 113 million mobile phone subscribers in Bangladesh with the penetration of mobile phones increasing rapidly, from 6% in 2005 to 74% in 2013 [17] Such high and rapidly increasing penetration presents many opportunities to provide accessible and economical health services, especially to rural and disadvantaged populations.
There are already over 20 mHealth initiatives, mostly from private businesses and NGOs including primary healthcare, disease surveillance and data collection, health promotion and disease prevention, and health information systems and support tools. Examples include “Telemedicine link” and ‘Health Line 789’, a GSM infrastructure based call center for Grameen Phone, which provides real time medical consultations, emergency services, medical information facilities, emergency services, and SMS based laboratory services over mobile phones to 49 million subscribers [17] The use of such technology has enabled developing countries like Bangladesh to develop new more accessible models for health care delivery, many of which can be applied in developed countries, often being able to disruptively “leapfrog” health service provision.
Much progress has also been made in sub-Saharan African countries. These initiatives have already been well doccumented in the 2014 mHealth Compendium [5]. For this reason we have focused on Bangladesh as an example of what can be achieved. While developing countries like Bangladesh have rapidly adopted new eHealth technologies there remains much work to be done on governance, standards and regulatory frameworks if such initiatives are to provide quality, affordable health care. Bangladesh already has a set of supportive policies towards eHealth. The objectives of the Bangladesh National ICT Policy (2009) are social equity, productivity, integrity, education and research, employment generation, strengthening exports, healthcare, universal access, environment, climate & disaster management, and support to ICT initiatives [17].
Bangladesh is now implementing a framework for eHealth, which will improve countrywide information management in the areas of a central register for providers, levels of usage, privacy and security standards. Once this occurs it will overcome the difficulties of assessing comparative gains in health outcomes. In a paper, which examined eHealth initiatives in Bangladesh Ahmed, Lucas et al. suggested that policy and regulatory issues are the most urgent issues for the Government of Bangladesh to work on [6].
The experience of Bangladesh can be generalized to other developing countries and presents opportunities to extend eHealth and mHealth services to many disadvantaged people to achieve improved chronic disease outcomes from innovative health ser vice applications. In a recent study of applying eHealth solutions to managing multi-morbidity associated with chronic diseases [1] Atun concluded that the opportunity now exists to “transition to person-centred health systems underpinned by technology-enabled primary, community and social care that sustain and improve health and do not merely react to disease”.
4.3 Consumer Self-Management
Consumer self-management refers to behaviours that individuals engage in to promote health or manage chronic health conditions [9]. Besides offering opportunities for cost reduction, Forczek states that “it also gives rise to new forms of healthcare and makes doctor-doctor, doctor-patient, patient-patient relationships independent of geographical location, thus laying the foundations of telemedicine” [9].
Access to Oncology Knowledge
One of the most significant barriers to self-management is lack of oncology knowledge amongst both GPs and cancer survivors. The average GP is likely to encounter only four new patients each year with a life threatening cancer and on average, have only sixteen cancer patients on their books at any one time [18]. While this was a relatively old study, the issues raised are still relevant e.g. GPs getting a sufficient volume of cancer survivors to develop and maintain their skills.
While cancer survivor concerns about GPs’ oncology knowledge are well documented, the literature also identifies that many GPs also have similar concerns [19]. While this was a Dutch study focusing on breast cancer survivors, its findings apply to other cancer patients. The need for rapid access to cancer specialists (for both Cancer Survivors and GPs) was identified by this and other studies [20]. While the holistic care available from GPs was seen as valuable for example, to manage, side effects and co-morbidities, patients wanted a quick route back to the oncologist if needed. The same studies also highlighted the need for an integrated EHR to facilitate this communication [3].
Training of GPs and developing administrative tools was seen as potentially useful for them to organize other services for cancer survivors [19]. This study is relevant in that it highlighted attitudes of GPs and patients towards GP follow up. One such administrative tool identified is a Survivorship Care Plan (SCP) to facilitate communication across the primary/secondary interface and with patients. The SCP documents surveillance, health maintenance, and health-promotion recommendations for individual cancer survivors to decrease the risk of recurrence and to facilitate early detection [21]. The Survivor Care Plans were viewed positively by survivors and their GPs, but were often seen as “too time and labor intensive to track and complete”. Electronic Health Records were seen as having the potential to improve efficiency [21].
Holistic Self-Management for Chronic Diseases
Although patients with multiple health issues use eHealth technology to support self-care for specific conditions, they also desire more holistic capability through tools that transcend disease boundaries. By addressing the holistic needs of patients with multiple co-morbidities, eHealth technology can advance health care from a disease-centered to a patient-centered model [22].
Most studies reviewed indicated that cancer survivors had a positive attitude towards self-management and eHealth. Positive attitudes towards eHealth applications were associated with male gender, lower age, treatment with chemotherapy or (chemo) radiation (versus surgery alone), hematological cancer (versus skin cancer, breast cancer, and other types of cancer), and lower quality of life [23]. However a holistic approach requires a level of integration that many eHealth systems are not yet capable of. One example is in glucose self monitoring. El-Gayer [24] describes a situation where self-monitoring needs to be conducted in combination with dietary schedules and renewing prescriptions and supplies. The technology dimension for glucose self-monitoring involves a level of complexity and includes use of glucometers at the work system level, exchange of data between glucometer and the home computer at the building.
Despite these difficulties, among eHealth technology users, patients with more chronic conditions tend to derive greater knowledge and increased motivation to improve their health [25].
One example is where a joint Norwegian/American study examined cancer patient’s experiences with an application called WebChoice. WebChoice is an interactive eHealth application that is personalized and interactively tailored to patients’ specific needs, and that patients can share knowledge and experience to better manage their own care [26]. The authors describe it as enabling patients to self-monitor their symptoms and health problems, providing them with individually tailored information and support to manage their symptoms and illness-related problems between treatments and during rehabilitation, offer personal mail communication with expert nurses in cancer care who answer questions and concerns, and it includes a forum for group discussion with other cancer patients [25].
The study found that the messaging function which enabled close interaction with cancer care nurses and the interactive forum which allowed peer support with other patients were heavily used and very much valued. This suggests that eHealth self-care applications are more likely to succeed when they include a component of human interaction in addition to supplying information.
Social Media
The growing importance of social media in supporting cancer survivor’s self-help efforts and in supporting clinician’s communities of practice and knowledge transfer has not yet been reflected in the literature. A study of social media posts by cancer survivors [27] identified an association between writing posts and positive outcomes. Also from reviewing colon cancer survivor posts on websites like Beating Bowel Cancer http://community.beatingbowelcancer.org/forum/ [28] it appears that thousands of cancer survivors get a great deal of information and support from such sites but more research is clearly needed in this area.
One typical recent study [29] which, examined web based cancer support services such as websites, online forums, email listservs, bulletin boards and blogs showed that using web based support resources by cancer affected people enabled them to achieve health and psychological related benefits. Benefits identified included improved confidence, enhanced satisfaction and self-esteem. It also identified improvement in feelings of wellbeing and quality of life, increased optimism, reduction in depression, feeling empowered, become more active in their treatment and experiencing better health status. However such studies did not find direct links to positive health outcomes such as improved mortality.
The relevance of social media in helping support care of cancer survivors in GP led integrated primary care networks is that they can support personal relationships and knowledge sharing. Social media can also involve and empower patients. This is important as one Australian study by Harris and Pascoe [30] found that “GPs take notice of patient input when making referral decisions which means that information systems need to include patient input and perspectives”. That study also found that the key-determining factor for which specialist a GP refers patients to be the quality of personal relationship the GP has with the specialist. For this reason Harris concluded, “Information systems must support personal relationships based on a shared knowledge base”.
Communities of Practice
Similarly many online communities of practice exist which support the exchange of clinical knowledge and experience. According to Moja et al. [22] communities of practice have great potential for facilitating clinician led practice change. The involvement of those who can effectively implement change is a key element in quality improvement and research in general practice. This approach may be particularly relevant to rural and remote areas where practitioners are geographically dispersed and often isolated.
4.4 Socio-technical Factors Affecting Usability and Take-up
There is no point in developing eHealth applications, which are not easy for consumers and clinicians to use. They must also meet an immediate need. This is why human computer interaction and other socio-technical factors are so critical to their success. It is also important to recognize that eHealth implementation represents a disruptive change in the health care workplace. One review that is typical of the literature searched, suggests, “that change does not occur simply from the introduction of ICT infrastructure but may also require remodelling of the job design of interconnected health professionals to effectively and efficiently incorporate technology” [10].
There is considerable literature describing how a socio-technical approach to developing and implementing information systems in health care (and specifically cancer care) can improve usability and acceptability by clinicians. The approach broadly identifies a mismatch between the information systems development approach where processes are defined, then codified and enforced by instantiating a rigid process into an information system and the clinical process which is flexible and dynamic. Almost invariably, the clinical process needs to be modified to meet the needs of the information system resulting in usability issues and increasing the risk of non-acceptance.
Considerable evidence exists in the literature, including a Cochrane Review, which indicated that eHealth applications for people with chronic diseases had a significant effect on knowledge, perceived social support, health behaviors, clinical outcomes, and very likely also a positive effect on self-efficacy [31]. There is also wide agreement in the literature that eHealth applications that provide targeted support are more likely to be successful because information that is relevant to specific groups is more likely to be used [25].
One key finding of much of the literature reviewed is that eHealth applications need to be easy to use and easily accessible, taking account of human-computer interaction issues and socio-technical factors. Such pervasive IT-enabled systems for self-care and self-management applications should address the holistic needs of consumers and be built upon socio-technical principles and components [26]. eHealth implementation is frequently a disruptive change in the health care workplace. It is likely to require changes in individual job design and clinical pathways to efficiently incorporate technology [10].
4.5 eHealth Policy and Management Implications
Much still needs to be done so that eHealth policy and regulation can keep pace with rapidly changing eHealth and mHealth developments. Some key priorities are listed below.
Privacy
It will necessary to update privacy measures previously developed for institutional contexts to be relevant in the home setting where eHealth is now being introduced. Meier argues that currently ownership and/or control of clinical information lie predominantly in the hands of health-care providers, and patient access to information about them is at providers’ discretion and may be selective. With the globalization of telemedicine and eHealth, this may become problematic. This is especially the case when diagnostic tests are moved offshore [11].
One emerging privacy concern is the developing ability of some medical devices like pacemakers, insulin pumps, defibrillators and other monitoring devices to transmit vital patient health information to clinicians and external parties via the Internet. When such a device is remotely controlled the risk of privacy and security breaches emerges [32].
Liability
Because health care professionals are now mostly responsible for data entry and management, data-related mistakes or misadventures, therefore, are purely a matter of professional care, diligence, and competence. Meier argues that with eHealth, patients may readily become participants in the data generation process when data gathering and transmission is not entirely automated (through indwelling telemetry, etc.). This introduces the possibility of patient error either in measuring or in reporting values. Even when the process is automatic, patients may accidentally interfere with measurement or with the transmission process, resulting in misadventure [11].
Payment Models
eHealth implementation will disrupt existing payment models where consumers may be faced with a confusing range of such models. For example will an email consultation with a health professional be charged on a fee for service basis, via subscription or will it be free? How will performance be measured? – According to outcomes or by activity?
5 Conclusions and Future Work
This systematic review of the literature from 2013 to 2015 inclusive reveals that innovative eHealth and its subset mHealth initiatives are rapidly emerging as an important means of managing cancer and other chronic diseases. The adoption is following different paths in the developed and developing worlds. Besides the governance and regulatory issues described above, barriers still exist around information management, interoperability and integration. These barriers are discussed below.
-
Medical Records
As health care services are managed across settings, it becomes essential for electronic medical records to be standardized, to be portable across settings and easily discoverable regardless of how or where they are stored.
Available Online Information for Patients If greater self-management is to benefit patients and contribute to containing health costs, information needs to be accurate, easy to find and consolidate. Patients suffering chronic diseases need to have access to eHealth applications, which consolidate and synthesize information about multiple co-morbidities, such as applications that help identify potential medication-medication or condition-medication interactions [11].
-
Mobile App Bundles
The literature reveals that consumers of eHealth technology would prefer high-quality mobile app bundles that address their specific conditions as well as apps that provide assistance with common self-management challenges for example, complicated medication regimens and integrate information from different health care systems such as appointment reminders. mHealth could also be more extensively used to support smaller, smarter and timelier clinical trials. More research is needed in this area [14].
-
Communications Technology
Secure messaging, rapid response time and the ability to seamlessly communicate were also a key theme of the literature reviewed. As demand increases broadband capacity will need to expand, otherwise it will be a major barrier to adoption
-
Questions Answered
The questions posed in Section 2 can now be answered.
-
The most relevant technical advances include:
“Smart” bio-medical devices, which operate within the context of other patient information e.g. blood pressure, blood sugars that can produce a more holistic view of the patient’s state of health. Such medical devices will support more accurate diagnosis and monitoring, support self-management and self-care once a patient returns to the community.
Non-Invasive remote monitoring: non-invasive tele monitoring can reduce mortality, reduce or shorten hospitalisations. Combined with structured telephone support, it can reduce all-cause mortality and in the process deliver an acceptable experience for patients. Improved low cost remote monitoring will greatly improve access to health services, especially in developing countries and is especially relevant to patients who face issues of distance or lack of mobility.
Precision medicine makes it possible to perform genomic sequencing to determine if a particular cancer will respond to targeted therapy. The implications for eHealth will be that genetic information will become an essential part of any Electronic Health Record as it will save patients unnecessary trauma and the health system unnecessary costs as well as greatly increasing the efficacy of chemotherapy,
-
Significant differences have been identified between developed and developing countries in how eHealth and mHealth solutions are being applied. –
In developed countries eHealth is about applying information technology to improve the efficiency and effectiveness of health-care delivery, while in emerging and developing countries it is about providing access to basic health-care for people, usually experiencing poverty.
The use of such technology has enabled developing countries like Bangladesh to develop new more accessible models for health care delivery, many of which can be applied in developed countries, often being able to disruptively “leapfrog” current health service provision in developed countries.
-
The implications for more holistic management and self-management of cancer and other chronic diseases of eHealth centre on the disruptive nature of new technology implementation on job roles and responsibilities, privacy models. These include:
A holistic approach requires a level of integration that many eHealth systems are not yet capable of. While devices are becoming more context-aware they still depend on human (medical) expertise to interpret them.
eHealth self-care applications are more likely to succeed when they include a component of human interaction in addition to supplying information. This introduces the possibility of patient error either in measuring or in reporting values. Even when the process is automatic, patients may accidentally interfere with measurement or with the transmission process, resulting in misadventure. Protocols will need to be developed on how patients and clinicians can safely share responsibility in these situations.
Self-monitoring devices may well automatically report to external entities e.g. pharmaceutical companies patient data that patients may not have given consent for, or are even aware is being reported. Privacy laws will need to be reviewed to address these emerging situations.
-
Sociotechnical Factors are affecting usability and take-up
eHealth applications need to be easy to use and easily accessible, taking into account human-computer interaction issues and socio-technical factors. Pervasive IT-enabled systems for self-care and self-management applications should address the holistic needs of consumers and be built upon socio-technical principles and components.
eHealth applications for people with chronic diseases have a significant effect on knowledge, perceived social support, health behaviors, clinical outcomes. However implementing such systems will require attention to be given to job and clinical process redesign.
applications that provide targeted support are more likely to be successful because information that is relevant to specific groups is more likely to be used.
-
This review examined at a high level new developments in eHealth and its subset mHealth to improve the management of cancer and other chronic diseases. It did this from the perspectives of new technical advances, differences between Developed and Developing Countries, the implications for management and self-Management, usability and take-up, eHealth policy and management implications. Much progress has been made in implementing eHealth and mHealth technologies in both the developed and developing world. eHealth is now realizing its potential to be a disruptive technology, which could overcome many of the limitations associated with the traditional, restricted, and highly expensive in-patient treatment of many chronic pathologies.
Table 1.
Queries
| Query | Results |
|---|---|
| Chronic Diseases or eHealth and Developing Countries | 892,441 |
| eHealth and Cancer or Chronic Diseases | 326,767 |
| Cancer Survivor and Self Management and Self Care | 224,670 |
| Cancer Survivor and Self Management and Self Care | 50,033 |
| Sociotechnical Factors, eHealth or mHealth | 9718 |
| Sociotechnical Factors, eHealth or mHealth | 6485 |
| Chronic Disease Management and eHealth or mHealth | 6,475 |
| eHealth and Management | 2,711 |
| Biomedical Technology, New | 334 |
| eHealth, Cancer or Chronic Diseases | 41 |
| Developing Countries and eHealth and Chronic Diseases | 7 |
| Total Results | 1,519,682 |
Acknowledgements
This research was partly supported by the WHO Collaborating Centre on eHealth in UNSW-Australia, as part of its contribution to the Asia pacific Ubiquitous Health research Consortium (APUHC), the research arm of Asia eHealth Information Network (www.aehin.org), the organisation sponsored by WHO, ADB and other agencies to coordinate eHealth activities in Asia Pacific countries.
Appendix
Appendix 1.
Summary Table of Articles Reviewed
| # | Author/Title/ Ref | Study Type | Context & Population Studied | Aims of Initiative being reported on | Methods/ Tools used | Results/Outputs | Critical Appraisal
|
|---|---|---|---|---|---|---|---|
| 1 | National Health Service. (2015) | Review | Worldwide | Provides overview of new developments in biomedical devices | Systematic Review of Literature | Provides a succinct overview of new biomedical device development | High quality systematic review |
| Biotechnology; New Findings in Biomedical Informatics [34] | Relevant because it discusses the disruptive nature of some new biomedical devices and the effect on clinical work processes of their implementation. | ||||||
| 2 | Atun R. (2015).Tronsitioning health systems for multimorbidity [1] | Review | Worldwide | To increase understanding of the impact of chronic disease | Summary of the 2013 WHO Report on the Impact of chronic disease | Discusses the impact on health systems in both developing and developed countries of chronic diseases | Succinct commentary in Lancet |
| Relevant because it summarises the impact of chronic diseases on the health system | |||||||
| 3 | Bakshi A, et al. (2013) Adaptive policy framework: A systematic review [7] | Review | Australia | Used to provide a robust methodology | Systematic Review of Literature | Robust methodology | Robust methodology |
| 4 | Costelnuovo G, etol. (2015) New Technologies for the Management and Rehabilitation of Chronic Diseases and Conditions. [4] | Article | Worldwide | Provide an overview of new technologies | Survey new biomedical technologies | Potential for the development of a new and innovative model of healthcare as represented by such technologies as telemedicine, e-heolth applications, biomedical sensors and devices, integrated platforms and technologies for remote monitoring and management, web and Internet based clinical protocols, and m-heolth solutions. | Summary article |
| Relevant in that it gave a concise summary of new technologies for the management of chronic diseases | |||||||
| 5 | Chen Z, et al. (2015) Dissecting an Online Intervention for Cancer Survivors. [27] | Article | USA | To understand how cancer survivors use social media to support self-management | Qualitative methods-semi structured interviews and analysis of text from posts | Four Exploratory Analyses of Internet Engagement and Its Effects on Health Status and Health Behaviors.” | Rigourous analysis of cancer survivor posts on social media. |
| Relevant in that it showed how cancer survivors can receive emotional and social support using social media | |||||||
| 6 | Conway A, et al. (2014) Effective Technologies for Noninvasive Remote Monitoring in Heart Failure. [12] | Article | UK | Explanation of self monitoring technology for heart patients | A sub analysis of a large systematic review and meta-analysis was conducted. Studies were stratified according to the specific type of technology used, and separate meta-analyses were performed. | This sub analysis identified that only two of the four specific technologies used for noninvasive remote monitoring in heart failure improved outcomes. | Rigourous analysis |
| Relevant in that it provived recent examples of self managed bio-meicol technologies and critiqued their effectiveness | |||||||
| 7 | EI-Goyor O, etol. (2013) Onthe Design of IT-Enobled Self-Care Systems: A Socio-technical Perspective. [24] | Article | USA | Discussion of user acceptance issues of IT enabled health care systems | Analysis of design issues | Identified key socio-technical principles for IT enabled self care systems | In-depth review of sociotechnicol issues associated with design and use of IT enabled self care systems |
| Relevant in that it presented a set of sociotechnicol based principles for system design and effectiveness | |||||||
| 8 | El-Gayar OF, et al. (2010) Evaluating task-technology fit and user performance for an electronic health record system. [26] | Article | USA | Discussion of task technology fit for an EHR | Analysis of design issues | Identified key design principles to enable health IT systems to align with clinical processes | Identifies eight dimensions for measuring and evaluating health information system performance. |
| Strong methodology used to obtain perceptions of task-technology fit by surveying 100 nurses. | |||||||
| 9 | Emery J. (2014) Cancer survivorship - the role of the GP. [3] | Review | Aust. Cancer Survivors-GPs | Improve chronic disease mgmt. in Primary Care | Literature review of Australian trials of shared and GP based care management | Pts need quick route back to oncologist if needed, Integrated EHR needed Holistic care of GP is valuable e.g. co-morbidities | Comprehensive review of existing trials - need for more research |
| GP Role | Very highly relevant to research question - GP information needs, information system characteristics. | ||||||
| 10 | Erfani SS, e† al. (2014) Effects of Web based cancer support resources use on cancer affected people: A systematic literature review. [29] | Review | Australia and world wide | Understanding the impact of web based support resources use on cancer affected people | Science Direct, Springer Link, IEEE Explore, Google Scholar, and expert consultation to select articles, thirty five (35) of which met the selection criteria. | Results showed the use of web based support recourses by cancer affected people enabled them to archive health and psychological related benefits. | Comprehensive review of existing resources - need for more research |
| Very highly relevant to research question- EHealth & Management of Chronic diseases | |||||||
| 11 | Forczek E, et al. (2015) The Internet as a New Tool in the Rehabilitation Process of Patients-Education in Focus. [9] | Article | Hungary | Understanding the rehabilitation of patients using information technology, especially Internet support | Examination of experience in Hungarian health system | In the development of rehabilitation programmes, the knowledge of the IT professional and the therapist, in the IT support of web guidance, medical expertise plays the primary role. | Limited in scope and coverage. Hungary seems well behind in e Health development |
| Relevant in that examined tHe IT specialist/clinician communication issues needing to be addressed to develop effective IT support for rehab programs | |||||||
| 12 | Harris, M. (2012) Patients with Colorectal cancer: A qualitative study of referral pathways and continuing care. [30] | Article | Australia | Understanding Referral Pathways | Qualitative Interviews with Clinicians | Relationships are paramount in determining referral pathways | Rigorous |
| Relevant in that it is important eHealth systems to take into account clinician relationships | |||||||
| 13 | Jameson JL (2015) Precision Medicine - Personalized, Problematic, and Promising. [13] | Article | USA | Understanding trends in Precision Medicine | Review | Precision Medicine will enable personalized treatment and will be a disruptive force | Very comprehensive overview of precision medicine. |
| Relevant in that it is a major trend that eHealth will need to deal with | |||||||
| 14 | Jonsen F, et al. (2015) Cancer survivors’ perceived need for supportive care and their attitude towards self- management and eHealth. [23] | Study | Cancer Survivors in Germany | To explore the perceived need for supportive care including healthy lifestyle programs among cancer survivors, their attitude towards self-management and eHealth | A questionnaire on the perceived need for supportive care and attitude towards self-management and eHealth was completed by 212 cancer survivors from an online panel. | The perceived need for supportive care includ- ing healthy lifestyle programs was high, and in general, cancer survivors had a positive attitude towards self-management and eHealth. | Highly relevant in that the article examines Cancer survivors’ perceived need for supportive care and their attitude towards self-management and eHealth.” |
| 15 | Kerr C, et al. (2005). Interactive health communication applications for chronic disease: patient and carer perspectives. [31] | Study | UK Cancer survivors | Analysis of patient acceptance of INTERACTIVE eHealth applications | Qualitative – 4 focus groups | Showed broad acceptance of eHealth applications – with Web 2.0 interactivity – emphasis on good HC interaction | Limited in scope but highly relevant and generalizable. |
| Relevant for patient acceptance. | |||||||
| 16 | Khan NF, et al. (2011) A qualitative study of unmet needs and interactions with primary care among cancer survivors. [20] | Qual. Research | UK Cancer Survivors in 2 NE England Counties N=40 | To explore the experiences of individuals who have survived at least 5 years following a cancer diagnosis, and to describe perceived unmet needs and interactions with primary care. | Grounded Theory Approach — semi-structured interviews - coded themoticolly using NVivo 7 qualitative analysis software (Doncaster, Australia) by one researcher (NK). | Cancer survivors cited three main reasons for not using GP services in relation to their cancer diagnosis. GPs were seen as non-experts in cancer; they were perceived as too busy; and a lack of continuity within primary care made it difficult to talk about long-term issues. | Rigorous qualitative study. |
| Patient Perspective | Relevant in that it described areas of GP capability that were perceived as lacking — specialised cancer knowledge and lack of integrated, continuity of care. | ||||||
| 17 | Khatun F, et al. (2015). Determinants of readiness to adopt mHealth in a rural community of Bangladesh. [17] | Study | To understand factors required for the take-up of eHealth in developing countries | Survey | A conceptual framework for mHeolth readiness was developed, which included three categories: technological, motivational and resource readiness. This guided the questionnaire development for the survey conducted in the Chokorio sub-district of Bangladesh | A total of 4915 randomly selected household members aged 18 years and over completed the survey. The data explained the sub-categories of the readiness dimensions. In terms of access, 45% of respondents owned a mobile phone with ownership higher among males, younger participants and those in the highest socioeconomic quintiles. Results related to technological readiness showed that among mobile phone owners, 50% were aware of SMS but only sending and receiving SMS. | Very rigorous methodology |
| Highly relevant in that it detailed the conditions need to enable take-up of eHealth in developing countries | |||||||
| 18 | Li J, et al. (2014). Health Care Provider Adoption of eHealth: Systematic Literature Review. [10] | Review | To identify and synthesize influential factors to health care providers’acceptance of various eHealth systems. | Identified factors were analyzed and grouped in accordance with the Unified Theory of Acceptance and Use of Technology (UTAUT). | Systematic Literature Review | There would be potential to extend theories on information technology adoption, which is of great benefit to readers interested in learning more on the topic. Practically, these findings may help health care decision makers proactively introduce interventions to encourage acceptance of eHealth and may also assist health policy makers refine relevant policies to promote the eHealth innovation. | Comprehensive literature review highly relevant to research question |
| 19 | Liaw ST, et al. (2013). Towards an ontology for data quality in integrated chronic disease management: A realist review of the literature. [8] | Review | To improve understanding of an ontological approach to DQ as a potential solution and address existing research in this area which is limited and fragmented. | Screened 245 papers, excluded 26 duplicates, 135 on abstract review and 31 on full-text review; leaving 61 papers for critical appraisal. Of the 33 papers that examined ontologies in chronic disease management, 13 defined data quality and 15 used ontologies for DQ. | Systematic Literature Review | Most saw DQ as a multidimensional construct, the most used dimensions being completeness, accuracy, correctness, consistency and timeliness. | Focused on data quality Effective use of routine data to support integrated chronic disease management (CDM) and population health is dependent on underlying data quality (DQ) and, for cross system use of data, semantic interoperability. |
| Highly relevant because of its rigorous and re-usable methodology | |||||||
| 20 | Deborah K. Mayer (22/06/2015) | Quality Research | USA-Colon Cancer Survivors | Implementing Survivorship Care Plans for Colon Cancer Survivors | Study to evaluate the feasibility, usability, and satisfaction of a survivorship care plan (SCP) and idenifify the optimum time for its delivery during the first 12 months after diagnosis. | The Survivor Care Plans were well received by the survivors and their PCPs, but were too time and labor intensive to track and complete. Electronic Health Records may improve efficiency. Need for other process issues to be addressed e.g. patient selection | Rigorous study from a nursing perspective. Well-described methodology. Small size study (n = 49). Very highly relevant to research question – PCP information needs, information system characteristics. Patient feedback |
| Implementing Survivorship Core Plans for Colon Cancer Survivors | GP & Nursing Role | ||||||
| 21 | McAvoy BR (2007). General practitioners and cancer control. [18] | Personal Experience | Australian GPs and Cancer Survivors | Aims to describe the role of GPs in managing cancer survivors | Aims to describe the role of GPs in managing cancer survivors | GPs cover the full spectrum of cancer care from prevention to palliation, including providing psychosocial support to patients and their families and carers. GPs have a key role in early diagnosis and referral, follow-up and detection of recurrence, and survivorship. There is a developing role for GPs in cancer policy and research. | Older study but issues still relevant |
| P- GPs and Cancer survivors in Australia | |||||||
| 1 - GPs have a key role in early detection, managing side effects of treatment and follow up monitoring and survivorship | |||||||
| C-Not relevant | |||||||
| O - GPs are in the best position to provide coordinated and continuity of care especially in dealing with co morbidities, which two thirds of cancer patients have. | |||||||
| 22 | Meier CA, et al (2013). eHealth: Extending, Enhancing, and Evolving Health Care. [11] | Review | Focus on worldwide uptake of eHealth solutions — majority of examples from USA | Wide-ranging review of past, present and predicted future of eHeolth. Examines eHealth definition, benefits and adoption challenges | Systematic Review of Literature | Predicts eHealth will have an increasingly vital role in improving the efficiency of the health system. | Comprehensive, well referenced review of literature but somewhat high level. A good overview but it kept to a high level. |
| 23 | Lorenzo Moja (04/07/2015) Effectiveness of Computerized Decision Support Systems Linked to Electronic Health Records: A Systematic Review and Meta-Analysis | Lit Review | Sixteen RCTs contributed to this analysis.--A total of 37 395 individuals participated in these trials: 18 848 in the intervention groups and 18 547 in the control groups. | Conducted a systematic review to rigorously evaluate the impact of CDSSs linked to EHRs on critical outcomes-mortality, morbidity, and costs | Searched MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials and Cochrane Database of Abstracts of Reviews of Effects. Information on system design, capabilities, acquisition, implementation context, and effects on mortality, morbidity, and economic outcomes were extracted. | This systematic review of 28 RCTs revealed little evidence for a difference in mortality when pooling results from comparisons of adoption of a CDSS integrated with an EHR versus health care settings without a CDS. We found weak evidence that an active CDSS is associated with a lower risk for morbidity. | Extensive literature search. Rigorous analysis of the literature. Study did not consider the following outcomes: patient satisfaction, measures of process, and health care professional activity or performance (e.g., adherence to guidelines, rates of screening and other preventive measures, provision of counseling, rates of appropriate drug administration, and identification of at-risk behaviors). |
| The beneficial effects of CDSSs might still be greater than that suggested by the current analysis given the limited number of actual studies providing results on hard outcomes. | Relevant to the research question – study casts doubt on the effectiveness of CDSSs to reduce mortality. | ||||||
| 24 | Roorda C, et al. Discharge of breast cancer patients to primary care at the end of hospital follow-up: A cross-sectional survey. Europ J Cancer 2013;49(8):1836-44. | Survey of GPs | Dutch GPs N=527 | Discharge of breast cancer patients to primary care at the end of hospital follow-up: A cross-sectional survey | Survey to 976 GPs resulting in a 53% return rate. Then regression analysis of results | Perceived barriers in current and future primary care-based follow-up included: communication with breastcancer specialists, patients’ preference for specialist follow-up, GPs’ oncology knowledge and skills and the organisation of follow-up in general practice. | Large sample size enabled sophisticated statistical analysis. Survey had limitations - inconsistent response rate, self- reporting, cross- sectional (not longitudinal) |
| Relevant in that it highlighted attitudes of GPs and patients towards GP follow up. GPs need a threshold number of patients to be able to build up their expertise. | |||||||
| Survivorship care plans are needed to facilitate communication across the primary/secondary interface and with patients. Training of GPs and developing administrative tools may be helpful in arranging follow-up care and using guidelines in general practice. | |||||||
| 25 | Rulond CM, et al. (2013). Evaluation of differentfeotures of an eHeolth application for personalized illness management support: Cancer patients’ use and appraisal of usefulness. [25] | Study | Norway Cancer Survivors | To describe patients’ use of a multi-component eHeolth application, WebChoice, designed to support cancer patients in illness management. | Analyzed user logs of breast and prostate cancer patients who participated in the experimental arm of an RCT to test effects of WebChoice on clinical outcomes. Patients could freely use the system for one year. | The Forum and asking questions to the nurse were used the most, yet there were large individual variations in use patterns. Also, patients used different WebChoice components for different reasons. The e-mail communication with nurses was valued highest. | Rigorous |
| Relevant because it was one of few studies which looked at how cancer survivors actually used an eHeolth support system. It highlighted the functions and features most valued by patients | |||||||
| 26 | Vos T et al. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. [2] | Review | Worldwide | To quantify the impact of chronic diseases on health systems in both developed and developing countries | Analyzed statistics provided from WHO member countries | The worldwide burden of non-communicable diseases is expected to increase from 46% in 2001 to 57% in 2020 | Classic study on worldwide burden of chronic diseases. Rigorous methodology. Useful background material on how rapidly increasing burden of chronic diseases will challenge health systems to become more efficient. |
| 27 | Zulmon D, et al. (2015). How Can eHeolth Technology Address Challenges Related to Multimorbidity? [33] | Review | USA | To understand how eHeolth systems should be designed to address multiple chronic conditions | Qualitative study giving perspectives from Patients with Multiple Chronic Conditions | Patients suffering chronic diseases need to have access to eHeolth applications, which consolidate and synthesize information about multiple co-morbidities, such as applications that help identify potential medication-medication or condition-medication interactions | Rigorous |
| Makes the point that many people with chronic diseases have multimorbidities, which need to be addressed holisticolly, and e Health systems need to support this. | |||||||
| 28 | Mendoza G, et al. (October 2014). mHeolth Compendium, Volume Four. [5] | Review | USA | To give an overview of recent developments in mHealth in sub-Sohoron Africa | Meta analysis of published studies | There are many successful mHeolth projects mostly funded by USAID that are enabling greater access to health care | Comprehensive overview of mHeolth projects up to 2014 |
| 29 | Balabanova D, et al. (2013). Good health at low cost 25 years on: lessons for the future of health system strengthening. [15] | Review | UK | To give an overview of recent developments in developing countries | Meta analysis of published studies | Discusses progress made in eHeolth and lessons learned | Rigorous review |
Footnotes
Conflict of Interest Statement The authors declare they have no conflicts of interest.
References
- 1.Atun R. Transitioning health systems for multi-morbidity. Lancet 2015; 386(9995):721-72. [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. ; Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emery J. Cancer survivorship - the role of the GP. Aust Fam Physician 2014;43:521-5. [PubMed] [Google Scholar]
- 4.Castelnuovo G, Mauri G, Simpson S, Colantonio A, Goss S. New Technologies for the Management and Rehabilitation of Chronic Diseases and Conditions. Biomed Res Int 2015:2015:180436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendoza G, Levine R, Kibuka T, Okoko L. mHealth Compendium, Volume Four. Arlington, VA: African Strategies for Health, Management Sciences for Health; October 2014. [Google Scholar]
- 6.Ahmed T, Lucas H, Khan AS, Islam R, Bhuiya A, Iqbal M. eHealth and mHealth initiatives in Bangladesh: A scoping study. BMC Health Serv Res 2014;14(1):260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bakshi A, Talaei-Khoei A, Ray P. Adaptive policy framework: A systematic review. Journal of Network and Computer Applications 2013;36(4):1261-71. [Google Scholar]
- 8.Liaw ST, Rahimi A, Ray P, Taggart J, Dennis S, de Lusignan S, et al. Towards an ontology for data quality in integrated chronic disease management: A realist review of the literature. Int J Med Inform 2013;82(1):10-24. [DOI] [PubMed] [Google Scholar]
- 9.Forczek E, Makra P, Lanyi CS, Bari F. The Internet as a New Tool in the Rehabilitation Process of Patients-Education in Focus. Int J Environ Res Public Health 2015;12(3):2373-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health Care Provider Adoption of eHealth: Systematic Literature Review. Interact J Med Res 2013. Apr 16;2(1):e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meier CA, Fitzgerald MC, Smith JM. eHealth: Extending, Enhancing, and Evolving Health Care. Annu Rev Biomed Eng 2013;15(1):359-82. [DOI] [PubMed] [Google Scholar]
- 12.Conway A, Inglis SC, Clark RA. Effective Technologies for Noninvasive Remote Monitoring in Heart Failure. Telemed J E Health 2014;20(6):531-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jameson JL, Longo DL. Precision Medicine — Personalized, Problematic, and Promising. N Engl J Med 2015;372(23):2229-34. [DOI] [PubMed] [Google Scholar]
- 14.National Cancer Institute Website. http://www.cancer.gov/news-events/cancer-currents-blog/2015/precision-medicine-trials.
- 15.Balabanova D, Mills A, Conteh L, Akkazieva B, Banteyerga H, Dash U, et al. Good health at low cost 25 years on: lessons for the future of health system strengthening. Lancet 2013;381:2118-33. [DOI] [PubMed] [Google Scholar]
- 16.Adams AM, Ahmed T, El Arifeen S, Evans TG, Huda T, Reichenbach LLancet Bangladesh Team. Innovation for universal health coverage in Bangladesh: a call to action. Lancet 2013. Dec 21;382(9910):2104-11. [DOI] [PubMed] [Google Scholar]
- 17.Khatun F, Heywood AE, Ray PK, Hanifi SM, Bhuiya A, Liaw ST. Determinants of readiness to adopt mHealth in a rural community of Bangladesh. Int J Med Inform 2015;84(10):847-56. [DOI] [PubMed] [Google Scholar]
- 18.McAvoy BR. General practitioners and cancer control. Med J Aust 2007;187(2):115-7. [DOI] [PubMed] [Google Scholar]
- 19.Roorda C, Berendsen AJ, Haverkamp M, van der Meer K, de Bock GH. Discharge of breast cancer patients to primary care at the end of hospital follow-up: A cross-sectional survey. Eur J Cancer 2013;49(8):1836-44. [DOI] [PubMed] [Google Scholar]
- 20.Khan NF, Evans J, Rose PW. A qualitative study of unmet needs and interactions with primary care among cancer survivors. Br J Cancer 2011;105(S1):S46-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer D, Gerstel A, Walton AL, Triglianos T, Sadiq TE, Hawkins NA, Davies JM. Implementing Survivorship Care Plans for Colon Cancer Survivors.” Oncol Nurs Forum 2014;41(3):266-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moja L, Kwag KH, Lytras T, Bertizzolo L, Brandt L, Pecoraro V, et al. (2014). Effectiveness of Computerized Decision Support Systems Linked to Electronic Health Records: A Systematic Review and Meta-Analysis. Am J Public Health 2014;104(12):e12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansen F, van Uden-Kraan CF, van Zwieten V, Witte BI, Verdonck-de Leeuw IM. Cancer survivors’ perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer 2015;23(6):1679-88. [DOI] [PubMed] [Google Scholar]
- 24.El-Gayar O, Sarnikar S, Abdullah Wahbeh A. On the Design of IT-Enabled Self-Care Systems: A Socio-technical Perspective. System Sciences (HICSS), 2013 46th Hawaii International Conference on; 2013. [Google Scholar]
- 25.Ruland CM, Maffei RM, Børøsund E, Krahn A, Andersen T, Grimsbø GH. Evaluation of different features of an eHealth application for personalized illness management support: Cancer patients’ use and appraisal of usefulness. Int J Med Inform 2013;82(7):593-603. [DOI] [PubMed] [Google Scholar]
- 26.El-Gayar OF, Deokar AV, Wills MJ. Evaluating task-technology fit and user performance for an electronic health record system. International Journal of Healthcare Technology and Management 2010;11(1-2):50-65. [Google Scholar]
- 27.Chen Z, Koh PW, Ritter PL, Lorig K, Bantum EO, Saria S. Dissecting an Online Intervention for Cancer Survivors: Four Exploratory Analyses of Internet Engagement and Its Effects on Health Status and Health Behaviors. Health Educ Behav 2015;42(1):32-45. [DOI] [PubMed] [Google Scholar]
- 28.Beating Bowel Cancer Website: http://community.beatingbowelcancer.org/forum/
- 29.Erfani SS, Abedin B. Effects of Web based cancer support resources use on cancer affected people: A systematic literature review. The International Technology Management Review 2014;4(4):201-11. [Google Scholar]
- 30.Harris MF, Pascoe S, Crosland L, Beilby J, Veitch C, Spigelman A, et al. Patients with colorectal cancer: A qualitative study of referral pathways and continuing care. Aust Fam Physician 2012;41(11):899-902. [PubMed] [Google Scholar]
- 31.Kerr C, Murray E, Stevenson F, Gore C, Nazareth I. Interactive health communication applications for chronic disease: patient and carer perspectives. J Telemed Telecare 2005;11:32-4. [DOI] [PubMed] [Google Scholar]
- 32.Wikipedia Website: https://en.wikipedia.org/wiki/Medical_device.
- 33.Zulman D, Jenchura EC, Cohen DM, Lewis ET, Houston TK, Asch SM. How Can eHealth Technology Address Challenges Related to Multimorbidity? Perspectives from Patients with Multiple Chronic Conditions. J Gen Intern Med 2015;30(8):1063-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Health Service. Biotechnology; New Findings in Biomedical Informatics Described from NHS Foundation Trust (Exploring medical device design and use through layers of Distributed Cognition: How a glucometer is coupled with its context). Biotech Week; 2015:891. [DOI] [PubMed] [Google Scholar]


