Abstract
Limited data are available on epidemiology and drug use in Chinese hypertensive patients with chronic kidney disease (CKD). We determined the prevalence; awareness, treatment, and control rates of hypertension; anti-hypertensive use, expenditure pattern; and factors associated with hypertension prevalence and control in Chinese patients with CKD. This was one of the largest cross-sectional surveys that enrolled 6079 CKD participants (mean age, 51.0 ± 16.37 years) with or without hypertension from 22 centres across China. The prevalence, awareness, and treatment rates were 71.2%, 95.4%, and 93.7%, respectively. Control rates 1 and 2 (Blood pressure, BP <140/90 and <130/80 mmHg) were 41.1% and 15.0%, respectively. Patients were treated mostly with monotherapy (37.7%) or 2-drug anti-hypertensive combination (38.7%). Factors associated with prevalence of hypertension included age; smoking; body mass index; physical exercise; family history of hypertension; hyperuricaemia; and CKD. Control rate was associated with CKD stage, BP monitoring at home, and use of drug combinations. Despite high rates of awareness and treatment, the control rates are low. CKD stages 4 and 5 adversely affect the control rate. The results suggest the immediate need of comprehensive controlling measures to improve the control of hypertension in Chinese patients with CKD.
Hypertension and chronic kidney disease (CKD) are interrelated and increasingly recognised as a serious global public health concern1. The estimated worldwide prevalence of CKD is 8% to16%2. Its prevalence is not only high in developed countries3,4,5 but is also on the rise in developing countries6,7. In China, an estimated 10.8% of the population has CKD, and the prevalence has been observed to increase with increasing age7,8.
Hypertension is also highly prevalent in China (≈26.6%) and predominantly in men9. Hypertension became one of the most prominent risk factors and a comorbidity of CKD over a period of time (from 1990s to 2009–2010), and 24.2% elderly patients develop CKD as a result of hypertension10. In China, 2 studies reported the prevalence of hypertension in patients with CKD at 82.0% and 67.3%, respectively. However, despite high awareness and treatment rates reported in these studies, the control rates for hypertension were relatively very low11,12. Moreover, the control rate of hypertension is inversely associated with the CKD stage13. Uncontrolled hypertension is associated with poor prognosis of CKD, its progression to end-stage renal disease (ESRD), renal failure, and mortality. Patients with high-grade hypertension are at a higher risk of CKD progression14 and other complications such as stroke, cardiovascular disease, and target organ damage (TOD)15. Although awareness and treatment of hypertension in patients with CKD are showing an improving trend, treatment and control of blood pressure (BP) at all the CKD stages remain suboptimal16.
Despite the recognition of hypertension and CKD as a major public health concern, epidemiologic research to provide insights into public health approaches on prevention and treatment of hypertension in patients with CKD is limited and very few studies have been conducted in China to determine the prevalence and control rate of hypertension in patients with CKD. Therefore, we determined the prevalence, awareness, control, and rate of reaching the target BP in hypertensive Chinese patients with CKD using a nationwide survey across China. We study also evaluated the anti-hypertensive drug use situation, pattern of expenditure on drugs and factors associated with hypertension prevalence and control.
Results
Patient Characteristics
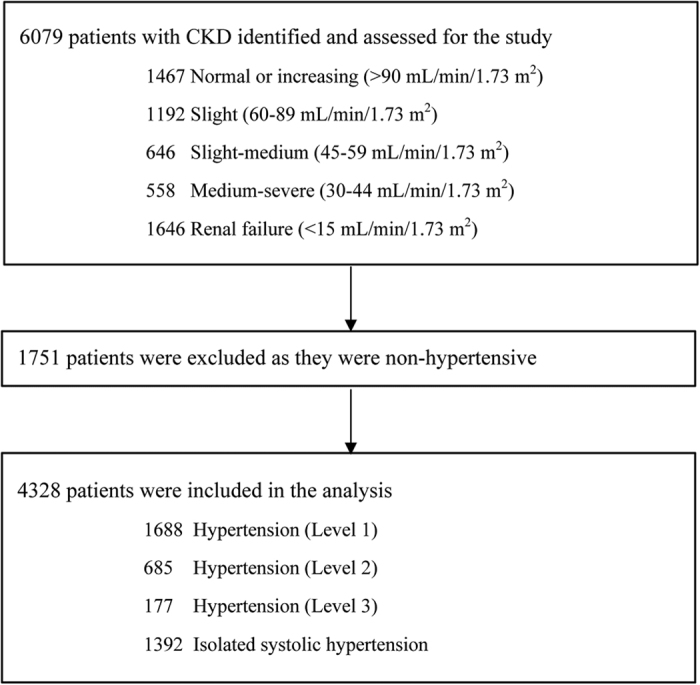
The study enrolled 6079 patients with CKD (mean age, 51.0 ± 16.37 years; mean BMI, 23.49 ± 3.483 kg/m2), with more than 50% (51.9%) males. The study population had 27.1% patients with CKD stage 5. The main aetiologies of CKD included diabetic nephropathy (n = 695, 11.4%); hypertensive and ischaemic renal damage (n = 875, 14.4%); primary chronic glomerulonephritis (n = 3710, 61.0%); secondary glomerulonephritis (n = 403, 6.6%); interstitial disease of renal tubules (n = 116, 1.9%); cystic kidney disease (n = 94, 1.5%); obstructive nephropathy (n = 56, 0.9%); hereditary and congenital nephropathy (n = 32, 0.5%); and tumour-related renal damage (n = 9, 0.1%). CKD was of unknown origin in 209 patients (3.4%). Of the total participants, 4328 were found to be hypertensive (71.2%). Other demographic characteristics and medical history of the patients are presented in Table 1. Mean BP at baseline was 136.6/81.3 mmHg (±19.55/11.27) for the whole study population (n = 6078). Other than hypertension, the major co-morbid indications were dyslipidaemia (34.6%), hyperuricaemia (32.6%), diabetes (21.6%), coronary heart disease (6.8%), other endocrine disorders (18.6%), and stroke (6%).
Table 1. Demographic Characteristics.
| Demographic Characteristics | Value, n (%) |
|---|---|
| Total number of patients | 6079 (100) |
| Age, years (±SD) | 51.0 (±16.37) |
| Men | 3154 (51.9) |
| Ethnic group/nationality | |
| Han | 5964 (98.1) |
| Others | 115 (1.9) |
| Educational level | |
| Primary school and below | 1218 (20.0) |
| Junior middle school | 1671 (27.5) |
| Senior high school | 1227 (20.2) |
| Technical secondary school | 440 (7.2) |
| Junior college | 635 (10.4) |
| Undergraduate college or above | 879 (14.5) |
| Smoking history | |
| No | 4719 (77.6) |
| Yes | 1360 (22.4) |
| Has quit smoking | 724 (11.9) |
| Still smoking | 635 (10.4) |
| Physical exercise | |
| No | 4508 (74.2) |
| Yes | 1571 (25.8) |
| Mean serum creatinine (mg/dL) | 3.5 (4.15) |
| Mean urine protein positive | 4606 (75.8) |
| Mean urine ACR (mg/mmol) (n = 4154) | 165.6 (382.65) |
| Proteinuria level | |
| A1 (<30 mg/24 h) | 501 (8.2) |
| A2 (30–300 mg/24 h) | 1475 (24.3) |
| A3 (>300 mg/24 h) | 2475 (40.7) |
| Mean eGFR (MDRD), mL/min | 54.8 (43.64) |
| Mean eGFR (CKD-EPI), mL/min | 53.1 (40.62) |
| GFR staging (mL/min/1.73 m2) | |
| Stage 1: Normal or increasing (>90) | 1467 (24.1) |
| Stage 2: Slight (60–89) | 1192 (19.6) |
| Stage 3a: Slight-medium (45–59) | 646 (10.6) |
| Stage 3b: Medium-severe (30–44) | 558 (9.2) |
| Stage 4: Severe (15–29) | 569 (9.4) |
| Stage 5: Renal failure (<15) | 1646 (27.1) |
| Albuminuria (mg/g) | |
| <30 | 941 (15.5) |
| 30–300 | 1736 (28.6) |
| >300 | 2636 (43.4) |
ACR = albumin and albumin/creatinine ratio, CKD-EPI = chronic kidney disease - epidemiology collaboration, eGFR = estimated glomerular filtration rate, MDRD = modification of diet in renal disease.
Prevalence, Awareness, Treatment, and Control Rates of Hypertension
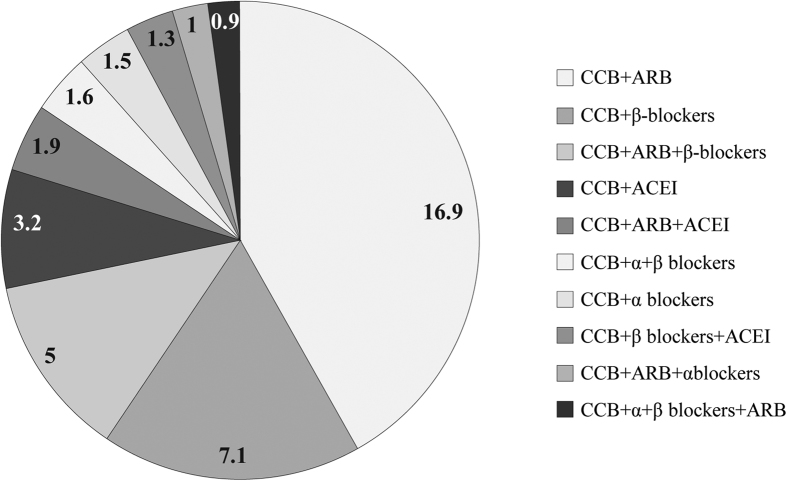
Overall, 4328 of the 6079 (71.2%) patients had hypertension. Prevalence of grade 1, 2, 3, and isolated systolic hypertension were 27.8%, 11.3%, 2.9%, and 22.9%. The overall prevalence, awareness, treatment and control rates are presented in Fig. 1. A total of 93 (2.3%) patients were diagnosed with hypertension after use of cortical hormone (n = 55, 1.3%), Chinese medicines (n = 17 0.4%), or other medicines (n = 25, 0.6%). Hypertension in these patients was possibly due to administration of previously administered therapy. Low prevalence of grade 3 in patients with CKD and high prevalence of patients with CKD stage 5 may indicate that small number of patients with CKD stage 5 have grade 3 hypertension. Among patients with hypertension, 4129 (95.4%) had been diagnosed and were aware of the disease before the study. The rate of treatment was 93.7%. Control rate 1 and control rate 2 were achieved by 41.1% and 15.0% patients, respectively with anti-hypertensive medications. Figure 2 shows reduction of BP post treatment from baseline. Among patients who were taking anti-hypertensive medications, BP was controlled in 1666 patients and lowered to a mean of 127.2/77.1 mmHg (±8.74/7.36). The decrease in BP in the controlled group was significant compared with baseline (difference from baseline: −9.4/4.2 mmHg, P = .0178). A total of 1778 patients had uncontrolled hypertension (did not achieve control rate 1 or 2). In these patients, BP at end of study was higher compared with the baseline mean BP, 154.1/88.2 mmHg (±14.44/11.28), difference: +17.5/6.9 mmHg]).
Figure 1. Prevalence, Awareness, and Control Rates of Hypertension.
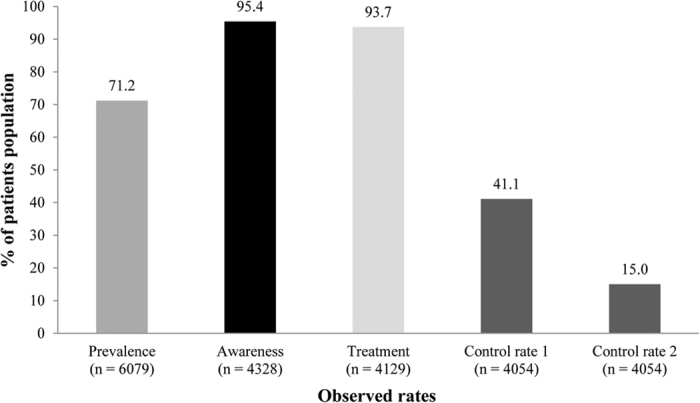
Figure 2. SBP, DBP, and Mean Arterial Pressure at Baseline and Post Treatment.
Patients who were aware of the disease also used non-drug treatments such as restricting salt intake (73.7%), controlling body weight (58.7%), cessation of smoking (17.7%) and alcohol consumption (24.3%), and starting physical activity (31.4%). Most of the patients (97.0%) started with anti-hypertensive therapy after diagnosis, and majority of the patients (85.3%) took the medications regularly.
Pattern of Anti-hypertensive Administration and Drug Expenditure
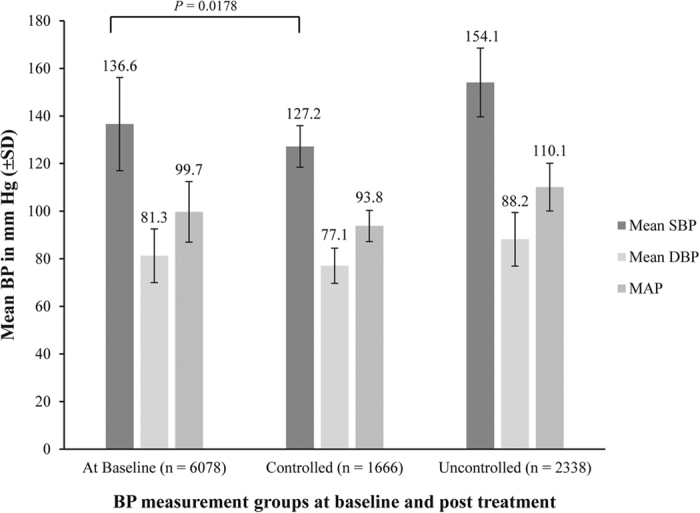
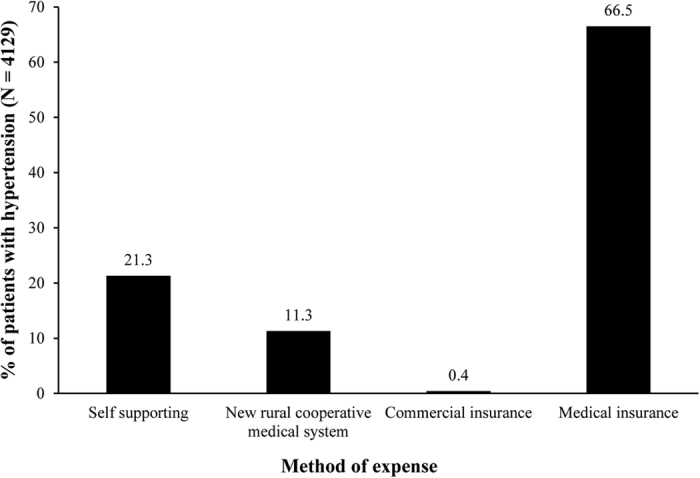
Monotherapy (37.7%) and 2 drug combination (38.7%) were the preferred anti-hypertensive treatment regimen. Three-, 4-, 5-, and 6-drug combinations were received by 15.8%, 3.9%, 0.7%, and 0.1% patients, respectively. Patients were administered angiotensin receptor blockers (ARB), α- and β-adrenergic blockers, calcium channel blocker (CCB), diuretics, angiotensin converting enzyme inhibitors (ACEI), centrally acting medicines, or compound preparations. Overall, CCB was the most preferred drug class in China (77.6%), followed by drugs affecting renin angiotensin system inhibitors (RASI; ARB [52.9%] and ACEI [24.0%] and β-receptor inhibitors [24.0%]). Combination therapy was administered in 2406 patients. CCBs were the major component of the drug combinations. A summary of CCB use in combinations is presented in Fig. 3. Anti-hypertensive drug expenditure patterns of patients are presented in Fig. 4. Patients spending on drugs through public medical insurance had employment (20.8%), retirement (38.8%), or small town insurance (6.9%).
Figure 3. Percentage Usage of CCBs in Combination Therapy.
Figure 4. Anti-Hypertensive Drug Expenditure Patterns.
Factors Associated With Prevalence, Awareness, Treatment, and Control Rates
All the independent factors were evaluated for association with prevalence, awareness, treatment, and control rates of hypertension using logistic regression. The analysis revealed that age, region or geography, smoking, BMI, lack of physical exercise, history of hypertension, hyperuricaemia; and stages of CKD had a significant positive association with prevalence of hypertension. In addition, awareness and treatment rates of hypertension were associated with age, region/geography, and glomerular filtration rate (GFR) staging. Apparently, level of education did not show any association with disease awareness and treatment. Control rates 1 and 2 for hypertension had association with age, gender, region, smoking, BMI, GFR staging, and self-monitoring of BP at home.
Multivariate analysis of the associated factors (Table 2) confirmed that patients 45 to 65 and 65 to 80 years of age had a significantly higher prevalence compared with patients 18 to 45 years of age (P < 0.001, for both comparisons). Prevalence of hypertension was higher in middle and northern China compared with southern China (P < 0.0001, for both comparisons). The prevalence of hypertension was significantly associated with 18–23 kg/m2, 23–28 kg/m2 and 28–32 kg/m2 higher BMI groups compared with the <18 kg/m2 BMI group (P = 0.0059, <0.0001, and <0.0001, respectively), with higher BMI showing greater association with hypertension prevalence. Compared with stage 1 CKD (reference stage), all the other stages of CKD had higher probability of being hypertensive (stage 2 OR: 1.387, P = 0.0004; stage 3a OR: 2.608, P < 0.0001; stage 3b OR: 2.705, P < 0.0001; stage 4 OR: 6.139, P < 0.0001; and stage 5 OR: 10.205, P < 0.0001). Lack of physical exercise, family history of hypertension and co-morbid indications increased the likelihood of hypertension in patients with CKD. Older age groups had a significant greater awareness of disease than the 18- to 45-year group (P < 0.001). Awareness rate was significantly associated with family history of hypertension (odds ratio (OR), 2.576; confidence interval [CI], 1.779–3.731; P < 0.0001). All the age groups and regions had a significant association with rate of treatment. Control rate 1 was significantly dependent on the region (for mid China vs. south China: OR, 3.028; CI, 2.207–4.153; P < .0001; for north China vs. south China: OR, 1.609; CI, 1.121–2.309; P = 0.0099) and smoking (OR, 0.754; CI, 0.522–1.778; P = 0.0077). Likelihood of achieving control rate 1 (≤140/90 mmHg) was significantly lower in patients with stage 5 CKD (OR, 0.559; CI, 0.404–0.774; P = 0.0005) and stage 4 CKD (OR, 0.605; CI, 0.404–0.905; P = 0.0145) compared with stage 1 CKD, which interpreted that the patients with uncontrolled hypertension belonged to stage 4 and 5 CKD. In stages 2, 3a and 3b, probability of achieving control rate 1 was similar to the CKD stage 1. Patients who applied home BP measurement (OR, 1.649; CI, 1.3–2.091; P < 0.0001) and used drug combination (OR, 0.597; CI, 0.483–0.74; P < 0.0001) were more likely to achieve a BP of <140/90 mmHg. Achievement of control rate 2 was dependent on gender (OR, 1.466; CI, 1.098–1.957; P = 0.0095), BP monitoring at home (OR, 1.879; CI, 1.333–2.648; P = 0.0003), and use of drug combination (OR, 0.548; CI, 0.415–0.722; P < 0.0001).
Table 2. Result of Multi-factor Regression Analysis.
| Characteristic | Prevalence | Awareness | Treatment | Control Rate 1 | Control Rate 2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age ([18, 45] -[65, 80]) | 3.659 (2.96–4.522) | <0.0001 | 2.381 (1.573–3.604) | <0.0001 | 3.393 (1.962–5.869) | <0.0001 | — | — | — | — |
| Age ([18, 45]-[45, 65]) | 1.868 (1.606–2.172) | <0.0001 | 1.613 (1.162–2.239) | 0.0042 | 2.27 (1.498–3.442) | <0.0001 | — | — | — | — |
| Gender, male-female | — | — | — | — | — | — | — | — | 1.466 (1.098–1.957) | 0.0095 |
| Region: South-middle | 1.598 (1.359–1.879) | <0.0001 | 0.878 (0.588–1.31) | 0.5229 | 0.54 (0.31–0.941) | 0.0295 | 3.028 (2.207–4.153) | <0.0001 | 3.69 (2.273–5.99) | <0.0001 |
| Region: South-north | 1.982 (1.601–2.454) | <0.0001 | 0.316 (0.213–0.468) | <0.0001 | 0.259 (0.146–0.46) | <0.0001 | 1.609 (1.121–2.309) | 0.0099 | 0.963 (0.522–1.778) | 0.9053 |
| Smoke (no-yes) | 1.499 (1.253–1.794) | <0.0001 | — | — | — | — | 0.754 (0.613–0.928) | 0.0077 | ||
| BMI ([0, 18]-[28, 32]) | 3.707 (2.557–5.374) | <0.0001 | — | — | — | — | — | — | — | — |
| BMI ([0, 18]-[23, 28]) | 2.415 (1.786–3.267) | <0.0001 | — | — | - | — | — | — | — | — |
| BMI ([0, 18]-[18, 23]) | 1.513 (1.126–2.032) | 0.0059 | — | — | — | — | — | — | — | — |
| Patients have physical exercise or not (no-yes) | 1.522 (1.292–1.793) | <0.0001 | — | — | — | — | — | — | — | — |
| Have family history of hypertension or not (no-yes) | 2.594 (2.201–3.057) | <0.0001 | 2.576 (1.779–3.731) | <0.0001 | — | — | — | — | ||
| Have other endocrine diseases or not (no-yes) | 1.248 (1.029–1.515) | 0.0247 | — | — | — | — | — | — | — | — |
| Have coronary heart disease or not (no-yes) | 1.994 (1.26–3.157) | 0.0032 | — | — | — | — | — | — | — | — |
| Have heart failure or not (no-yes) | 2.912 (1.387–6.113) | 0.0047 | — | — | — | — | — | — | — | — |
| Have hyperuricaemia or not (no-yes) | 1.566 (1.322–1.854) | <0.0001 | — | — | — | — | — | — | — | — |
| Have stroke or not (no-yes) | 4.215 (2.348–7.567) | <0.0001 | — | — | — | — | — | — | — | — |
| GFR staging 1: normal or increased (>90) −5: renal failure (<15) | 10.205 (8.2–12.701) | <0.0001 | — | — | — | — | 0.559 (0.404–0.774) | 0.0005 | — | — |
| GFR staging 1: normal or increased (>90) −4: severe (15–29) | 6.139 (4.546–8.291) | <0.0001 | — | — | — | — | 0.605 (0.404–0.905) | 0.0145 | — | — |
| GFR staging 1: normal or increased (>90) −3b: middle-severe (30–44) | 2.705 (2.075–3.526) | <0.0001 | — | — | — | — | 0.957 (0.631–1.452) | 0.8358 | — | — |
| GFR staging 1: normal or increased (>90) −3a: mild-middle (45–59) | 2.608 (2.054–3.311) | <0.0001 | — | — | — | — | 0.903 (0.611–1.335) | 0.6089 | — | — |
| GFR staging 1: normal or increased (>90) −2: mild (60–89) | 1.387 (1.157–1.662) | 0.0004 | — | — | — | — | 1.05 (0.735–1.501) | 0.7875 | — | — |
| Test BP in house or not | — | — | — | — | — | — | 1.649 (1.3–2.091) | <0.0001 | 1.879 (1.333–2.648) | .0003 |
| Drug combination administered (no-yes) | — | — | — | — | — | — | 0.597 (0.483–0.74) | <0.0001 | 0.548 (0.415–0.722) | <0.0001 |
BMI = body mass index, GFR = Glomerular filtration rate, OR = odds ratio.
Discussion
The prevalence of hypertension and CKD is constantly increasing in China and has seen multiple fold increase over the past 3 decades17,18,19. Since there are only a few studies that have determined the epidemiology and control of hypertension in Chinese patients with CKD; reliable information is necessary for the development of health policies in China, to prevent and control hypertension in patients with CKD. As per our knowledge, this is one of the largest nationwide survey that analysed the prevalence of hypertension, awareness of the disease, rates of treatment, control of hypertension; anti-hypertensive drug use and drug expenditure pattern; and factors associated with prevalence, awareness, treatment, and control rates of hypertension in patients with CKD in China.
Nationwide surveys such as the Chronic Renal Insufficiency Cohort (CRIC) study, Chronic REnal Disease In Turkey (CREDIT) study, and study in Columbia revealed that the prevalence, awareness, and treatment rates for hypertension were high and the control rates were sub-optimal20,21,22. Data from the CRIC study showed prevalence of 85.7%, awareness rate of 98.9%, treatment rate of 98.3% and control rate of 67.1% (<140/90 mmHg) and 46.1% < 130/80 130/80 mmHg20. The CREDIT study also reported a prevalence rate of 56.3%, awareness and treatment rates of 56.3%, 61.9% and 44.2%. The control rate was sub-optimal at 28.8% after treatment21. Sarafidis et al. reported a control rate of 13.2% despite high prevalence (86.2%), awareness (80.2%) and treatment rates (70.0%)22. Studies determining the control of hypertension in the United Kingdom and Japan also reported high prevalence (88.0% and 58.0%) and low control rates of hypertension (34.2% and 34.6%) in patients with CKD23,24,25. Similarly, a multinational survey was conducted in 2009 to 2010 across China that reported hypertension prevalence, awareness, and treatment rates of 82.0%, 90.7%, and 87.3%, respectively, in adult Chinese patients with CKD. The control rates were however very low at 29.6% for target BP of <140/90 mmHg and 12.1% for target BP of <130/80 mmHg. Another study by Zheng et al. showed that the rates of prevalence of hypertension in patients with CKD, awareness, and treatment were 67.3%, 85.8%, and 81.0%, respectively. The control rates of hypertension were 33.1% for BP <140/90 mmHg and 14.1% for BP <130/80 mmHg12. On similar lines, our study also reported high rates of prevalence of hypertension, awareness, and treatment. The control rate for target BP of <140/90 mmHg was observed to be slightly higher in this study than the previous studies (41.1% vs 29.6% and 33.1%). Proportion of patients achieving target BP of <130/80 mmHg was similar in our study and earlier studies (15.0% vs 12.1% and 14%). Low control rates in all the studies showed that hypertension in China is not optimally controlled in patients with CKD. This is an alarming situation considering the continuously increasing trend of hypertension in Chinese patients with CKD. The study also highlights relatively very low control rates of hypertension despite increased awareness and treatment. The control rate among different countries might vary due to ethnicity, economic or educational level differences, as reported by Sarafidis et al. Within the same country, improvement in economy and setting of the study (study conducted in rural or urban setting) may also improve the treatment and control rates.
The Chinese guidelines for the treatment of hypertension suggest the use of CCB, ACEI, ARB, diuretics, and β-blockers as monotherapy or combination therapy for hypertension management15. The JNC8 guidelines recommend the use of ACEI or ARB for CKD patients with hypertension26, whereas the European Society of Hypertension (ESH) guidelines recommend the use of all anti-hypertensive drugs except diuretics (in the haemodialysis patients) after dose determination based on hemodynamic instability and the ability of the drug to be dialysed27. In the present study, CCB, ARB, and β-blockers were the most prescribed medications in China.
Anti-hypertensive drug expenditure patterns also support the association of prevalence, awareness, and treatment of hypertension with older age, as approximately 39% patients were retired from work.
The factors associated with prevalence, control, awareness, and treatments were determined. The risk of hypertension was more in older patients (42–65 and 65–80 years of age) than in relatively younger patients (18–45 years of age). Hypertension prevalence was associated more with patients from middle and southern China than those from north China. Smokers, patients with BMI >18 kg/m2, lack of physical exercise, CV and metabolic co-morbidities, and CKD stages 2 to 5 were associated with a high prevalence of hypertension. In a study by Stevens et al., the prevalence of hypertension in participants with CKD aged 65 and older in KEEP and NHANES 1999 to 2006 were 94.5% and 91.6%, respectively28. Findings from this study were consistent with previous literature that showed older age, higher BMI, smoking, CV, and metabolic disease as the factors associated with a high prevalence of hypertension11,22. Awareness of hypertension was found to be higher in older patients and those with a family history of hypertension. Older age and geography were associated with a higher rate of treatment. Control rate 1 was determined primarily by CKD stage, BP monitoring at home, and use of drug combinations for treatment. Patients with CKD stage 4 and stage 5 were not able to achieve control rate 1. Anti-hypertensive therapy with ARBs as mono- or combination therapy improved the rate of hypertension control in Chinese patients with hypertension and CKD. Measurement of BP at home was responsible for increasing the awareness of patients toward the disease and medication, subsequently improving the BP control rate. Achievement of control rate 2 was positively associated with female gender, regular BP monitoring at home, and use of combination drug therapy. Overall, the control rate was low for patients taking anti-hypertensive medications. The findings highlight that high prevalence and control of hypertension were associated with renal function in adult patients with CKD.
The present study has the following strengths: (i) stringent use of a standard data collection protocol; (ii) inclusion of extensive data on demography, medical-related history, drug treatments, expenditure behaviour of patients, and factors associated with hypertension in patients with CKD; and (iii) analyses of data from a large sample size.
This study has certain limitations because of which the findings must be interpreted with caution. Most notably, the cross-sectional study design does not allow for causal associations to be established with certainty. Second, sampling was not done randomly. Number of patients was limited and out of those, ESRD patients accounted for a relatively large number. Third, potential limitation is that there might be some variation in evaluating laboratory parameters or BP measurement despite following the standardised protocol. Selection of hospitals from 3 developed cities of China limited the extrapolation of the results to the whole Chinese CKD population. Another potential limitation of our study is that we correlated the control of hypertension with GFR only, while the correlation between hypertension and albuminuria was not evaluated. Furthermore, well-designed, large sample cohort studies and randomised clinical trials are warranted to draw effective conclusions.
The prevalence, awareness, and treatment rates of hypertension in Chinese patients with CKD were high. However, the low control rates reflect the sub-optimal control of hypertension in patients with CKD. Association of monitoring BP indicated toward the need of greater awareness of the disease, whereas association of drug combinations with control rates suggested toward the need of developing effective interventions for managing hypertension in patients with CKD in China. Therefore, strategies to improve awareness and treatment of hypertension in patients with CKD are needed in China for better healthcare management.
Methods
Study Design and Population
The ‘Research on hypertensive nephropathy and ischemic kidney diseases National key technology R&D program (12-5) (Study No. 2011BAI10B00 (2011BAI10B06)’ study was one of the largest multicentre, cross-sectional survey in China. A total of 22 hospitals (Supplementary Table S1) were selected from mid-China (n = 11), northern (n = 6), and southern China (n = 5).
Patients with CKD (aged >15 years) were invited to participate in this survey. The inclusion criteria were: (i) age 16 to 85 years; (ii) CKD (stage 1–5) with or without hypertension. Patients were excluded if they had malignant tumour, BMI >32 kg/m2; coagulation disorder, drug abuse history or addicted to alcohol, severe CV or cerebrovascular disease, psychological disorder or were pregnant or lactating. The study was approved by the ethics committee (Ref no: 2012–54) of all the 22 hospitals in China (Rui Jin Hospital Shanghai Jiao Tong University School of Medicine, Shanghai; Huashan Hospital Fudan University, Shanghai; Shanghai General Hospital, Shanghai; Jiangsu Province Hospital, Jiangsu; Sichuan Provincial People’s Hospital, Sichuan; Union Hospital Tongji Medical College, Hubei; Tongji Hospital Tongji Medical College, Hubei; Jiangsu Taizhou People’s Hospital, Jiangsu; Yangpu Hospital, Shanghai; Shanghai Construction Group Hospital, Shanghai; Tongren Hospital Shanghai Jiao Tong University School Of Medicine, Shanghai; Guangdong General Hospital, Guangdong; Fujian Provincial Hospital, Fujian; The First Affiliated Hospital of Nanchang University, Jiangxi; The First Affiliated Hospital of Wenzhou Medical University, Zhejiang; The First Affiliated Hospital of Xiamen University, Fujian; Beijing Anzhen Hospital Capital Medical University, Beijing; PLA Navy General Hospital, Beijing; The First Affiliated Hospital of Zhengzhou University, Henan; The First Affiliated Hospital of Xinjiang Medical University, Xinjiang; Inner Mongolia People’s Hospital, Neimenggu; The 2nd Affiliated Hospital of Harbin Medical University, Heilongjiang) and conducted in accordance with International Conference on Harmonisation Good Clinical Practice (GCP, E6), Declaration of Helsinki (1964) and its subsequent revisions. All participants provided their informed consent before initiation of the study.
Data Collection
The data were collected from 30 June 2012 to 30 December 2013 (18 months) using a standardised questionnaire. Before commencing the study, all investigators were trained on the study protocol. Trained investigators collected the demographic, clinical, laboratory, drug treatment (use of monotherapy or combination), drug expense, and BP data. In addition, the investigators completed case report form using a standardised protocol. The study flow diagram is presented in Fig. 5.
Figure 5. Study Flow Chart.
BP was measured by trained healthcare professionals (HCPs) in the morning (8 am to 11 am) as per standard protocol. Literature suggests taking a minimum 2 measurements for ensuring the accuracy of BP measurement. Therefore, before recording the BP, participants rested for approximately 5 minutes following which BP was measured twice using a mercury sphygmomanometer with at least a 1-minute interval between measurements in an ambulatory setting. Mean of the 2 measurements was considered for the analysis. If the difference between the 2 BP measurements was >5 mmHg, one more measurement was taken, and mean of the 3 BP measurements was used29,30.
Definitions of Hypertension, Awareness, Treatment, and Control Rates
Hypertension is defined as a systolic BP (SBP) of ≥140 mmHg or a diastolic BP (DBP) of ≥90 mmHg or undergoing treatment for hypertension. Grades 1, 2, and 3 of hypertension are defined as BP of 140–159/90–99, 160–179/100–109, and ≥180/≥110 mmHg. Participants with SBP of 130 to 139 mmHg or DBP of 85 to 89 mmHg were considered to be having critical or borderline hypertension, as it is not suitable to define these patients as normotensives. Isolated systolic hypertension was defined as BP ≥140/<90 mmHg27. The ESH and the European Society of Cardiology (ESC) suggest maintaining a BP of <140/90 mmHg in patients with CKD, whereas the Chinese 2010 Hypertension guidelines suggest maintaining BP of <130/80 mmHg in such patients15,27. It is not possible to recommend specific BP targets in elderly adults with CKD due to lack of evidence and difference in target BP range of various guidelines11. Therefore, in this study target BP levels were chosen as <140/90 (control rate 1; as per ESH/ESC, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High BP [JNC-8] Guidelines)26,27 and <130/80 mmHg (control rate 2; Chinese 2010 Hypertension guidelines)15 with anti-hypertensive drug treatment. Awareness rate was defined as the proportion of patients with hypertension who were diagnosed with hypertension by a physician or HCP before enrolment into this study. Treatment rate was defined as the proportion of patients with hypertension receiving anti-hypertensive medications before enrolment in the study.
Definition of CKD
In accordance with the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, CKD was defined as GFR of <60 mL/min/1.73 m2 for ≥3 months. Patients were classified into different CKD stages based on their GFR. Definition of different stages of CKD is presented in Table 131.
Statistical Analysis
Statistical analysis was performed using Statistical Analysis System (SAS) Ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Descriptive statistics was used to evaluate demographic characteristics, medical history, and parameters for laboratory inspection, drug treatment, and expenditure patterns. Logistic regression was used to find the association between demographic and clinical factors with prevalence, awareness, and control rates. A P value of <0.05 was considered as statistically significant.
Additional Information
How to cite this article: Zhang, W. et al. A nationwide cross-sectional survey on prevalence, management and pharmacoepidemiology patterns on hypertension in Chinese patients with chronic kidney disease. Sci. Rep. 6, 38768; doi: 10.1038/srep38768 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
We thank and acknowledge R&D Pharma Studies Co., Ltd for their contribution in study monitoring and data analysis. We also thank Karan Sharma and Dr. Amit Bhat from Indegene Pvt Ltd, Bangalore, India, for providing medical writing support and technical assistance in the preparation of this manuscript, with funding from Bayer Healthcare Company Ltd (China). All authors contributed in the conceptualising the study design, data collection, analysis, and interpretation. All the authors were involved in drafting of the manuscript or revising it critically for important intellectual content, and have approved the final version of the manuscript. The main funding for this study was provided by the Bayer HealthCare Pharmaceuticals, Research on hypertensive nephropathy and ischaemic kidney diseases National key technology R&D programme (12-5) (Study No. 2011BAI10B00 (2011BAI10B06). The study was partially funded by Beijing Novartis Pharma.
Footnotes
Author Contributions W.Z. and W.S. contributed equally to this manuscript. W.Z., W.S., Z.S., Y.G., Q.C., W.Y., Y.Z., L.G., R.Z., M.L., H.C., J.L., J.C., C.H., Y.R., P.M., C.X., F.H., D.J., L.W., G.X., J.L, N.C. contributed in the conceptualising the study design, data collection, analysis, and interpretation. All the authors were involved in drafting of the manuscript or revising it critically for important intellectual content, and have approved the final version of the manuscript.
References
- Tedla F. M., Brar A., Browne R. & Brown C. Hypertension in chronic kidney disease: navigating the evidence. Int J Hypertens 2011, 132405 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha V. et al. Chronic kidney disease: global dimension and perspectives. Lancet 382, 260–272 (2013). [DOI] [PubMed] [Google Scholar]
- Xue L. et al. Prevalence of chronic kidney disease and associated factors among the Chinese population in Taiwan, China. BMC Nephrol 15, 205 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assogba G. F. et al. Prevalence, screening and treatment of chronic kidney disease in people with type 2 diabetes in France: the ENTRED surveys (2001 and 2007). Diabetes Metab 38, 558–566 (2012). [DOI] [PubMed] [Google Scholar]
- Stack A. G. et al. Prevalence and variation of chronic kidney disease in the Irish health system: initial findings from the national kidney disease surveillance programme. BMC Nephrol 15, 185 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham G. et al. Chronic kidney disease hotspots in developing countries in South Asia. Clin Kidney J 9, 135–141 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L. et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 379, 815–822 (2012). [DOI] [PubMed] [Google Scholar]
- Liu Z. et al. Prevalence and related factors of chronic kidney disease (CKD) among long lived individuals (LLI) over 95 years of age. Arch Gerontol Geriatr 60, 354–358 (2015). [DOI] [PubMed] [Google Scholar]
- Gao Y. et al. Prevalence of hypertension in China: a cross-sectional study. PLoS One 8, e65938 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Y. et al. Diabetes and hypertension have become leading causes of CKD in Chinese elderly patients: a comparison between 1990–1991 and 2009–2010. Int Urol Nephrol 44, 1269–1276 (2012). [DOI] [PubMed] [Google Scholar]
- Cai G., Zheng Y., Sun X. & Chen X. Prevalence, awareness, treatment, and control of hypertension in elderly adults with chronic kidney disease: results from the survey of prevalence, awareness, and treatment rates in chronic kidney disease patients with hypertension in China. J Am Geriatr Soc 61, 2160–2167 (2013). [DOI] [PubMed] [Google Scholar]
- Zheng Y. et al. Prevalence, awareness, treatment, and control of hypertension in the non-dialysis chronic kidney disease patients. Chin Med J 126, 2276–2280 (2013). [PubMed] [Google Scholar]
- Cheng L. T. et al. Stepwise increase in the prevalence of isolated systolic hypertension with the stages of chronic kidney disease. Nephrol Dial Transplant 23, 3895–3900 (2008). [DOI] [PubMed] [Google Scholar]
- Staples A. & Wong C. Risk factors for progression of chronic kidney disease. Curr Opin Pediatr 22, 161–169 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. S. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. [in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi 39, 579–615 (2011). [PubMed] [Google Scholar]
- Horowitz B., Miskulin D. & Zager P. Epidemiology of hypertension in CKD. Adv Chronic Kidney Dis 22, 88–95 (2015). [DOI] [PubMed] [Google Scholar]
- The Renal Association. CKD stages http://www.renal.org/information-resources/the-uk-eckd-guide/ckd-stages#sthash.eqquPsIN.dpbs/2016/01/04 (2013).
- Chen X. et al. Trends in the prevalence of hypertension in island and coastal areas of China: a systematic review with meta-analysis. Am J Hypertens 27, 1503–1510 (2014). [DOI] [PubMed] [Google Scholar]
- Wang J. et al. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 27, 1355–1361 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntner P., Anderson A. & Charleston J. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis 55, 441–451 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altun B. et al. Prevalence, awareness, treatment and control of hypertension in adults with chronic kidney disease in Turkey: results from the CREDIT study. Kidney Blood Press Res 36, 36–46 (2012). [DOI] [PubMed] [Google Scholar]
- Sarafidis P. A. et al. Hypertension awareness, treatment, and control in chronic kidney disease. Am J Med 121, 332–340 (2008). [DOI] [PubMed] [Google Scholar]
- Fraser S. D. et al. Suboptimal blood pressure control in chronic kidney disease stage 3: baseline data from a cohort study in primary care. BMC Fam Pract 14, 88 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konta T. et al. Blood pressure control in a Japanese population with chronic kidney disease: a baseline survey of a nationwide cohort. Am J Hypertens 25, 342–327 (2012). [DOI] [PubMed] [Google Scholar]
- Tylicki L. et al. Treatment of hypertension in chronic kidney disease patients under specialized care: one center cross-sectional analyses. Blood Press 24, 79–85 (2015). [DOI] [PubMed] [Google Scholar]
- Armstrong C. Joint National Committee. JNC 8 Guidelines for the management of hypertension in adults. Am Fam Physician 90, 503–504 (2014). [PubMed] [Google Scholar]
- Mancia G. et al. Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology. 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hyperten 31, 1281–1357 (2013). [DOI] [PubMed] [Google Scholar]
- Stevens L. A. et al. Prevalence of CKD and comorbid illness in elderly patients in the United States: Results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 55, S23–S33 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frese E. M., Fick A. & Sadowsky H. S. Blood Pressure Measurement Guidelines for Physical Therapists. Cardiopulm Phys Ther J. 22, 5–12 (2011). [PMC free article] [PubMed] [Google Scholar]
- Pickering T. G. et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 45, 142–161 (2005). [DOI] [PubMed] [Google Scholar]
- Update of the KDOQI™ Clinical Practice Guideline for Hemodialysis Adequacy https://www.kidney.org/sites/default/files/KDOQI-Clinical-Practice-Guideline-Hemodialysis-Update_Public-Review-Draft-FINAL_20150204.pdf/2016/01/04 (2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.