Abstract
A 74-year-old man with a left-ventricular assist device (LVAD) as destination therapy for end-stage ischemic cardiomyopathy presented with acute upper gastrointestinal bleeding. Other symptoms included chronic early satiety, intermittent nausea, and non-specific abdominal discomfort since LVAD implantation 3 years ago. An actively bleeding duodenal arteriovenous malformation was successfully treated with endoscopic coagulation. There was also evidence of moderate external compression of the anterior gastric wall from the LVAD pump with luminal narrowing in the antrum. While bleeding may be the most commonly encountered gastrointestinal manifestation in LVAD patients, other potential complications, including luminal compression by the device, should be recognized.
Introduction
Left-ventricular assist device (LVAD) implantation is an increasingly prevalent form of mechanical circulatory support as a bridge to heart transplant and as destination therapy.1 Several studies have demonstrated improved clinical outcomes in patients with LVAD at the time of transplant compared to those without such devices.2,3 The most commonly reported adverse events include gastrointestinal (GI) bleeding (GIB), device malfunction, and infections. GIB can result in significant morbidity, and its incidence has been estimated to range between 18–40%.4,5 While GIB remains the most recognized adverse GI event, other complications from LVAD implantation have also been previously described, such as the mechanical compression of the LVAD on the anterior gastric wall, which can lead to catastrophic complications such as bleeding and perforation.6,7
Case Report
A 74-year-old man with end-stage ischemic cardiomyopathy and LVAD implantation with a Heartmate II™ (Thoratec, Pleasanton, CA) as destination therapy was admitted to the hospital after 4 days of melena. Esophagogastroduodenoscopy (EGD) and colonoscopy prior to LVAD showed no abnormalities. On presentation, the patient was hemodynamically stable and not in distress. The patient denied having any prior GIB events. His main symptoms included chronic early satiety, intermittent nausea, and non-specific abdominal discomfort since LVAD implantation 3 years before. Laboratories revealed a significant decrease in his baseline hemoglobin from 12 g/dL to 8.5 g/dL and an international normalized ratio 2.2. Other laboratories were significant for a chronically elevated lactate dehydrogenase 370 U/L and undetectable haptoglobin levels, both of which were unchanged from his prior routine outpatient tests. In the setting of his GIB, the patient’s warfarin was withheld and he was transitioned to an intravenous heparin drip.
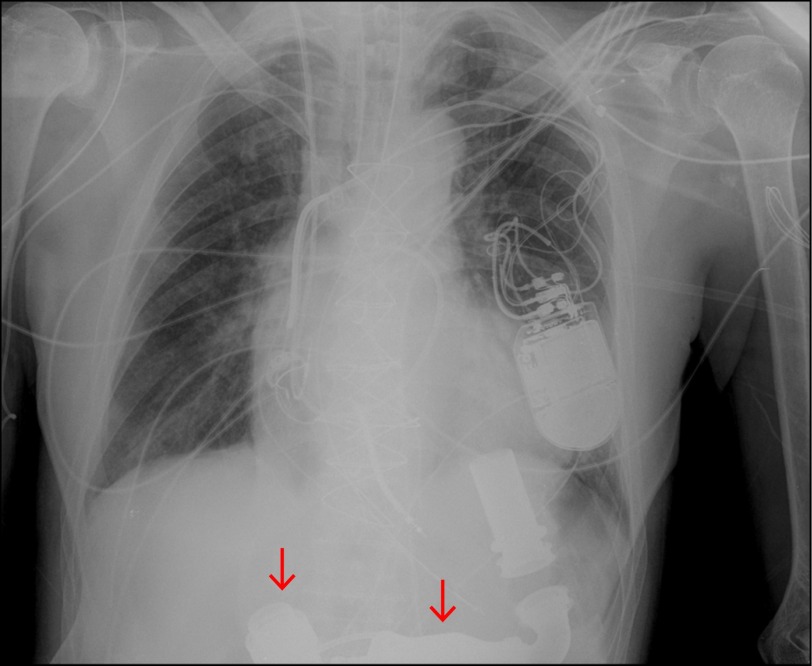
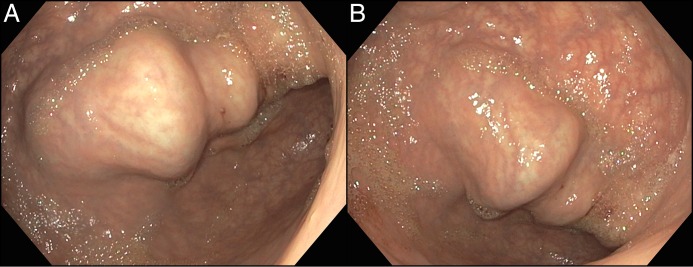
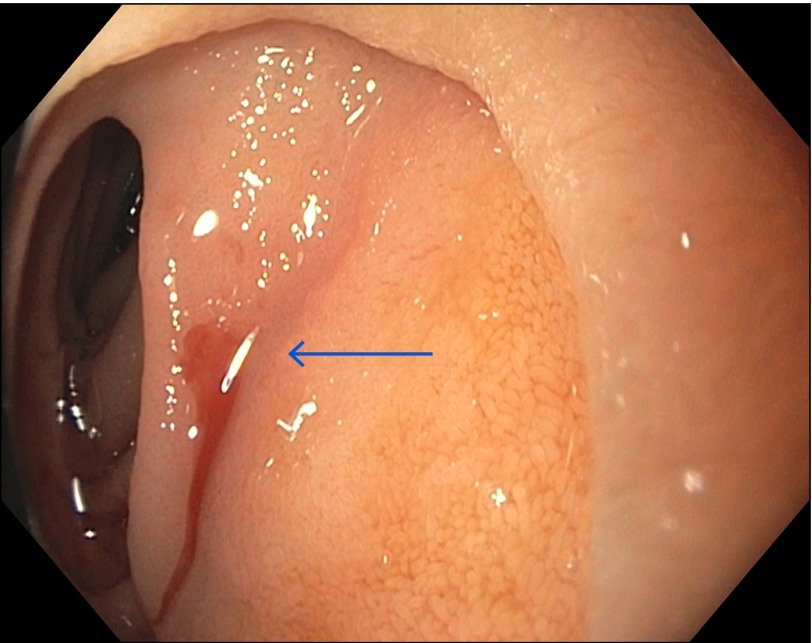
Post-operative chest radiograph showed the LVAD pump and outflow cannula in relation to the stomach (Figure 1). EGD showed that the stomach lumen was dilated but without any food contents as the patient had nothing by mouth for at least 48 hours prior to endoscopic evaluation. There was moderate external compression of the anterior gastric wall from the LVAD pump and outflow tract with luminal narrowing in the antrum (Figure 2). This was associated with some mild resistance to the maneuvering of the endoscope across the pylorus and into the duodenum. A bleeding arteriovenous malformation (AVM) was found in the second portion of the duodenum (Figure 3). Hemostasis was achieved with submucosal injection of 1 mL epinephrine (1:10,000 dilution) followed by thermal therapy (10-French Gold Probe™, Boston Scientific Corporation, Marlborough, MA) and placement of a hemoclip (Instinct™, Cook Medical, Winston-Salem, NC) (Figure 4). The patient recovered without further episodes of GIB and was discharged with outpatient follow-up.
Figure 1.
Chest radiograph showing the location of the LVAD pump and outflow cannula (arrows) in relationship to the stomach.
Figure 2.
(A) External compression of the anterior gastric wall in the body and antrum from the LVAD pump and outflow cannula. (B) Moderate luminal distortion in the prepyloric region from the pressure exerted by the LVAD.
Figure 3.
A bleeding AVM (arrow) is visualized endoscopically in the second portion of the duodenum.
Figure 4.
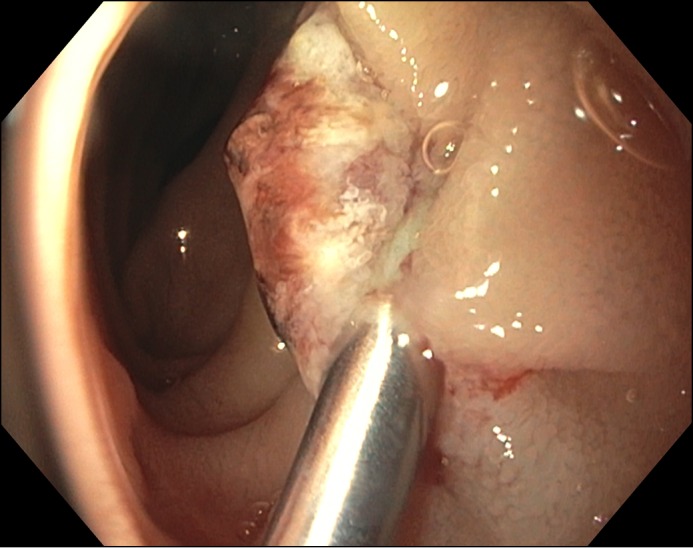
AVM following endoscopic therapy, epinephrine, thermal therapy, and hemoclips.
Discussion
LVADs are increasingly utilized for the management of patients with medically refractory heart failure as a bridge to cardiac transplantation or as a destination therapy for those who are not candidates for heart transplant. GIB is one of the most common adverse events associated with this type of device. A meta-analysis showed that the prevalence of GIB in LVAD patients was 23%, with 48% of these cases being from an upper GI source and 15% from a small bowel source.8 The underlying etiology of GIB in LVAD patients is likely multifactorial. For one, these patients are on antiplatelet and anticoagulation agents due to the concern for thrombosis. Furthermore, unlike the physiologic pulsatility associated with cardiac contraction, the continuous flow through the LVAD pump results in a narrowed arterial pulse pressure.9 This phenomenon predisposes to excessive cleavage of the large von Willebrand factor, which in turn has been associated with the development of AVMs and pathological bleeding.9-12 In a retrospective study of 172 patients with LVAD, AVMs were identified as the source of bleeding in 10 (32%) of the 32 patients presenting with GIB.13 All of these patients were successfully treated with endoscopic therapy without the need for surgery. Similarly, our patient with LVAD and duodenal bleeding AVM was successfully managed with endoscopic coagulation and clip placement without complications.
LVAD implantation can also exert other potential GI effects given its close anatomical proximity to the upper GI system, particularly the anterior gastric wall. One study reported early satiety and nausea in 70% of patients (n = 27) who had undergone LVAD placement.14 In this case series, gastric emptying rate (normal < 90 min) was prolonged in all of the patients (mean 283 min, range 106–506 min), and there was a single fatality due to aspiration pneumonia secondary to small bowel obstruction from LVAD compression.
Our patient reported similar symptoms of early satiety and intermittent nausea since the placement of the LVAD. We recognize that these symptoms are non-specific and could be due to chronic illness. It is less likely, however, that his complaints were due to his cardiac function, as this had actually improved following LVAD insertion and had remained stable for the past several years. We speculate that the patient’s symptoms of early satiety and nausea coincided with LVAD implantation in the setting of endoscopic evidence of gastric luminal compression and distortion from the device. The possibility of symptomatic gastric compression from LVAD is supported by two other case reports of patients who developed gastric ulceration and subsequent perforation at the site of LVAD compression, presumably secondary to local ischemia from pressure exerted by the device on the gastric wall.6,7
Disclosures
Author contributions: Both authors contributed equally to manuscript creation and approved the final version. D. Yang is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1. Ontario HQ. Left ventricular assist devices for destination therapy: A health technology assessment. Ont Health Technol Assess Ser. 2016; 16:1–60. [PMC free article] [PubMed] [Google Scholar]
- 2. Islam S, Cevik C, Madonna R, et al. Left ventricular assist devices and gastrointestinal bleeding: A narrative review of case reports and case series. Clin Cardiol. 2013; 36;36:190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Harvey L, Holley CT, John R. Gastrointestinal bleed after left ventricular assist device implantation: Incidence, management, and prevention. Ann Cardiothorac Surg. 2015; 3(5):475–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guha A, Eshelbrenner CL, Richards DM, Monsour HP. Gastrointestinal bleeding after continuous-flow left ventricular device implantation: Review of pathophysiology and management. Houston Methodist Debakey Cardiovasc J. 2015; 11:24–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cassell B, Kushnir VM. Gastrointestinal bleeding following left ventricular assist device (LVAD) implantation: Taking the pulse of the problem. Dig Dis Sci. 2015; 60:3507–9. [DOI] [PubMed] [Google Scholar]
- 6. Hou JK, Hampel H, Lukens FJ. Gastric ulceration and perforation as a complication of a left ventricular assist device. Gastrointest Endosc. 2005; 61:629–31. [DOI] [PubMed] [Google Scholar]
- 7. Yannopoulos D. Subacute gastric perforation caused by a left ventricular assist device. World J Gastroenterol. 2007; 13:3253–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: A systematic review and meta-analysis. Gastrointestinal Endoscopy. 2014; 80(3):435–46. [DOI] [PubMed] [Google Scholar]
- 9. Cushing K, Kushnir V. Gastrointestinal bleeding following LVAD placement from top to bottom. Dig Dis Sci. 2016; 61:1440–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morgan JA, Paone G, Nemeh HW, et al. Gastrointestinal bleeding with the HeartMate II left ventricular assist device. J Heart Lung Transplant. 2012; 31:715–8. [DOI] [PubMed] [Google Scholar]
- 11. Stern DR, Kazam J, Edwards P, et al. Increased incidence of gastrointestinal bleeding following implantation of the HeartMate II LVAD. J Card Surg. 2010; 25:352–6. [DOI] [PubMed] [Google Scholar]
- 12. Aggarwal A, Pant R, Kumar S, et al. Incidence and management of gastrointestinal bleeding with continuous flow assist devices. Ann Thorac Surg. 2012; 93:1534–40. [DOI] [PubMed] [Google Scholar]
- 13. Demirozu ZT, Radovancevic R, Hochman LF, et al. Arteriovenous malformation and gastrointestinal bleeding in patients with the HeartMate II left ventricular assist device. J Heart Lung Transplant. 2011; 30(8):849–53. [DOI] [PubMed] [Google Scholar]
- 14. el-Amir NG, Gardocki M, Levin HR, et al. Gastrointestinal consequences of left ventricular assist device placement. ASAIO J. 1996; 42:150–3. [PubMed] [Google Scholar]