Abstract
Background:
The advent of new neuromodulators and soft-tissue fillers continues to expand the nonsurgical repertoire of the core cosmetic physician.
Methods:
The authors review relevant facial anatomy as it relates to facial aging and the resultant structural changes that occur. These changes are important for the cosmetic physician to identify and understand in order to perform both safe and effective placement of neuromodulators and soft-tissue fillers. In this anatomic review, the authors review key structures that serve as landmarks for successful treatment using both neuromodulators and fillers.
Conclusions:
Knowledge of key facial anatomical structures allows the cosmetic physician to perform injection of neuromodulators and soft-tissue fillers in a reproducible manner to optimizing patient safety and results.
Although physicians learn the fundamentals of human anatomy in medical school, most have not appreciated the relationship between anatomical structures since then. With more than 6.7 million botulinum toxin injections and more than 2.4 million soft-tissue augmentation procedures performed each year, it is essential that physicians revisit important anatomical relationships to improve patient outcomes.1
As patients age, changes occur deep below the skin’s surface. Rigid boney structures and soft tissues recede and atrophy in all 3 dimensions.2,3 A detailed knowledge of facial fat compartments allows physicians to precisely augment areas of facial deflation using fillers.4,5 Similarly, to maximize the benefits of neurotoxins, physicians must also understand the 3-dimensional location of various muscles.
Here, we discuss the 3-dimensional anatomy of the face as it relates to toxins and fillers, affording the reader a better understanding of facial anatomy and techniques to maximize patient safety.
FACIAL NERVES
The muscles of the face fall into 2 categories: those responsible for facial expression and those involving mastication. Muscles involved in facial expression receive innervation via the VII cranial nerve (facial). The muscles of mastication (temporalis and masseter) are innervated by the trigeminal nerve (V). The facial nerve divides into 5 main branches: temporal, zygomatic, buccal, marginal mandibular, and cervical (Fig. 1). Although the muscles of facial expression have significant impact on facial aesthetics, the muscles of mastication have an influence on the shape and proportions of the face. Repeated contraction of the muscles of facial expression results in the formation of dynamic and static rhytids.
Fig. 1.
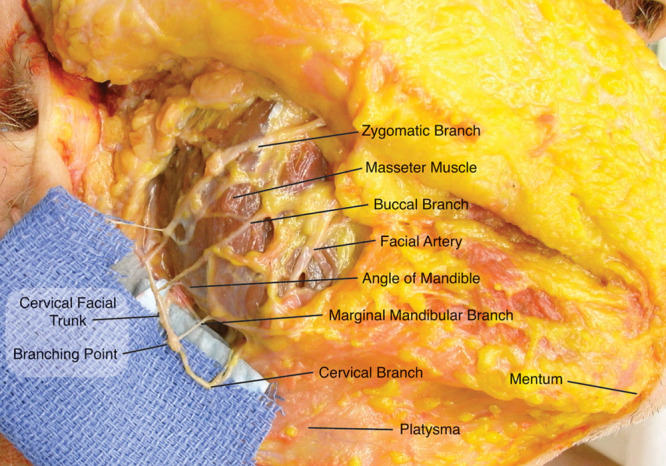
Cadaver dissection demonstrating the branches of the facial nerve in the appropriate anatomical planes. Reprinted with permission from Plast Reconstr Surg 2010;126:875–879.
BROW/GLABELLA NEUROTOXIN
The frontalis is the sole muscle responsible for elevation of the brows. It is a fan-shaped muscle commonly having a midline bifurcation of varying widths and lays in a very superficial plane (Fig. 2). The muscle interdigitates with the brow depressors inferiorly and expands superiorly and laterally to the galea aponeurotica along the temporal fusion line. Care must be taken when placing neurotoxin in the frontalis close to the orbital rim as toxin may migrate into the levator palpabrea superioris, causing temporary upper lid ptosis.
Fig. 2.
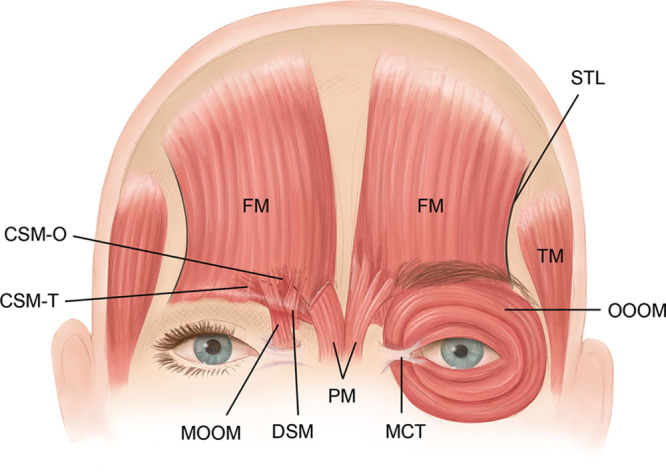
Illustration demonstrating the fan shape of the frontalis muscle with separation between the heads and the muscles involved in the glabellar complex. Muscles of the forehead and glabella: frontalis (FM), oblique head of the corrugator supercilii (CSMO), transverse head of the corrugator supercilii (CSM-T), depressor supercilii (DSM), procerus (PM), medial head of the orbicularis oculi (MOOM), and the orbital portion of the orbicularis oculi (OOOM). Also labeled are the superior temporal fusion line of the skull (STL), the medial canthal tendon (MCT), and the temporalis (TM) muscle. Reprinted with permission from Plast Reconstr Surg. 2009; 124: 2118–2126.
Because the bulk of the muscle lies above the medial two thirds of the brow, facial aging results in the descent of the less supported lateral third containing the tail of the brow. If neurotoxin is placed too far laterally or inferiorly into the frontalis muscle, patients may experience lateral brow descent, causing an aged and unnatural appearance. Lateral brow descent is also partially caused by the downward pull of the orbicularis occuli muscle. Paralysis of the lateral portion of the orbicularis allows for a slight elevation of the tail of the brow because of the remaining pull of the frontalis, elevating the brow. Brow descent can be prevented through a detailed examination, noting the preprocedural brow position. A balance must then be achieved between the pull of the frontalis, orbicularis, and glabellar complex to maintain an aesthetically pleasing brow position and shape.
The glabellar complex comprises the medial brow depressors: procerus, corrugator supercilii, depressor supercilii, and the orbicularis oculi muscles (Fig. 2). Understanding the depth of the glabellar muscles is important so as to only treat those muscles needed for the desired effect while sparing unnecessary paralysis of frontalis segments working to maintain the brow position. The procerus originates at the junction of the nasal bones, running superiorly and inserting into the skin just above the glabella. Contraction of the procerus produces horizontal lines overlying the glabella.
The corrugator supercilii originates medially and deep along the nasofrontal suture, travelling laterally and superiorly above the orbital rim. As the corrugator travels laterally, it becomes more superficial, interdigitating with the frontalis. Neurotoxins injected medially should be placed in a deep plane just above bone, injecting more superficially along the course of the muscle laterally. Knowledge of the depth of muscle and its location is critical to achieving optimal results when injecting botulinum toxins.
The final depressors of the brow are the orbicularis oculi muscle and depressor supercilii muscles. Although some consider the depressor supercilii to be a portion of the ocbicularis oculi, most aesthetic physicians recognize it as a distinct muscle with an origin on the medial orbital rim near the lacrimal bone and an insertion onto the medial portion of the orbit just inferior to the insertion of the corrugator supercilii. This muscle is divided into pretarsal, preseptal, and orbital portions. The pretarsal portion of the muscle lies on the tarsal plate centrally, fusing with the lateral canthal tendon as it travels laterally. The lateral orbital portion of the orbicularis is responsible for the crow’s feet and also contributes to depression of the tail of the brow. A subtle brow lift may be accomplished by placing small amounts of neurotoxin into the orbital portion of the orbicularis, especially into the lateral third in or just below the brow.
Injection technique for the brow may vary by injector, with some placing 4 to 6 depots of toxin in the main body of the frontalis. Others prefer to place smaller doses throughout the muscle. Each of these techniques is partially dependent on the toxin dilution used for injection, but more so is simply injector preference. The frontalis muscle typically requires 10 to 20 units onabotulinum/incobotulinum or 25 to 50 units of abobotulinum.
Careful toxin placement at the correct depth is critical for consistent aesthetic results. Injection of the procerus can include 1 to 2 injection sites above and below the horizontal rhytids in the region of the radix. The injection should be deep onto the bone where the muscle inserts.
The injection of the corrugators is more complex. Treating this muscle close to the origin requires a deeper injection to capture the medial portion and the depressor supercilii muscle. Laterally, the injection of the corrugators should be slightly more superficial as the muscle changes to a more superficial plane. The glabellar complex typical requires 15 to 20 units onabotulinum/incobotulinum or 38 to 50 units of abobotulinum with 1 injection site in the mid body of the procerus and 2 injection sites (on each side) for the corrugators.
Injecting the orbicularis muscle precisely is critical to obtaining an excellent result. When injecting the crow’s feet region, injections should be performed along the midportion of the lateral orbital rim and should be very superficial. If more relaxation of the muscle is required to open up the aperture of the eye or to rectify an asymmetry in the size of the apertures, then these injection sites need to be located closer to the medial border of the lateral orbital rim. Injections performed too medial along the orbital rim could result in diplopia from paralysis of the lateral rectus muscle. It is important to avoid chasing the inferior rhytids of the crow’s feet as this may lead to inadvertent paralysis of the zygomaticus major muscle, resulting in a subtle ptosis of the oral commissure with smiling. Treatment of the crow’s feet typically requires 7 to 10 units onabotulinum/incobotulinum, or 18 to 25 units of abobotulinum (per side) are injected evenly in 3 to 4 sites within the muscle.
BROW/GLABELLA FILLERS
Fillers should be used with caution in the brow/glabella area as there is a robust watershed area, which communicates directly with the central retinal artery and may lead to irreversible blindness. Cases of blindness have resulted from intravascular filler placement into the glabella. When placing a filler here, the needle needs to stay very superficial, almost in an intradermal plane, so as to avoid injection into the supratrochlear or supraorbital vessels. When injecting fine lines in the forehead, a more superficial plane should again be used to avoid vascular insult.
MASSETER NEUROTOXIN
When injecting the masseter muscle, it is best to inject the inferior aspect where the hypertrophy has the greatest effect on the aesthetics of the mandible and facial shape. Three to 4 injections near its insertion on the mandible will usually be sufficient to obtain the desired outcome. Doses of approximately 25 to 40 units of onabotulinum/incobotulinum or 60 to 100 units of abobotulinum are typically utilized for this location.
TEMPORAL FILLERS
There is much debate by injectors as to the proper depth for the correction of temporal hollows. Injection in either a superficial or deep plane has its associated risks. The superficial temporal artery and vein course in a superficial plane, giving off a frontal branch that leads up toward the superior lateral orbital rim, eventually anastomosing with the supraorbital artery. Deeper injections risk injury to the middle temporal vein, which lies just deep to the superficial layer of the deep temporal fascia.6 For these reasons, knowledge of pertinent anatomy is critical to avoid vascular injury.
PERIORAL NEUROTOXIN
The movements of the mouth are controlled through a multitude of synchronized contractions. The zygomaticus major and minor muscles originate on the lateral and medial zygoma, respectively, and insert onto the modiolus to draw the oral commissure superiorly and laterally. The levator anguli oris originates on the deep canine fossa of the maxilla and inserts onto the modiolus to elevate the oral commissure superiorly. The levator labii superioris originates on the maxilla and inserts onto the orbicularis oris medial to the commissure functioning to elevate the more medial lip elements. The levator labii superioris alaeque nasi originates on the frontal process of the maxilla and bifurcates in the region of the superior nasoalar crease, elevating the medial upper lip and ala (Fig. 3).
Fig. 3.

Illustration demonstrating the most common path and orientation of the facial artery as it ascends toward the alar base. Notice the relationship between the DLI and DAO, with the DAO in a more superficial and lateral position. Facial artery branches: inferior alar artery (IA), inferior labial artery (IL), lateral nasal artery (LN), and superior labial artery (SL). Facial muscles: DAO, DLI, levator anguli oris (LAO), levator labii superioris (LLS), levator labii superioris alaeque nasi (LLSAN), orbicularis oculi (OOc), orbicularis oris (OOr), platysma (Pl), risorius (Ri), zygomaticus minor (Zmi), and zygomaticus major (ZMj). Reprinted with permission from Plast Reconstr Surg. 2015;135:437–444.
The orbicularis oris, like the orbicular occuli, functions like a purse string to narrow the aperture of the mouth. The remainder of the upper and lower lip elevators and depressors form a radial pattern around the mouth. The depressor septi muscle originates from the incisive foramen of the maxilla and inserts onto the caudal septum. Its action creates a depression of the nasal tip with smiling. The lip depressors are significant radial retractors of the lower lip. The depressor anguli oris (DAO) originates on the oblique line of the mandible between the first premolar and the first molar and attaches to the modiolus (Fig. 3). Patients with an overactive DAO will have a down turning of the commissures at rest.
The depressor labii inferioris (DLI) lies deep to the DAO originating on the mandible and inserting into the tubercle of the lower lip. Contraction of the DLI exposes the mandibular incisors. The mentalis muscle originates on the mandible centrally and inserts into the skin of the chin. Contraction of the muscle results in elevation and protrusion of the lower lip, causing the “cobble stoning” sometimes seen on the chin. The mentalis muscle sometimes bifurcates, causing a dimple to be present in the center of the chin. The platysma muscle is the primary superficial muscle of the neck. It originates on the deltopectoral fascia and inserts onto the depressors of the lips, margin of the mandible, and mid cheek.5 Its action results in depression of the jaw and lower lip.
Hyperactivity of the levator labii superioris alaeque nasi muscle may result in a “gummy smile,” which oftentimes can be treated with 2 to 5 units of onabotulinum/incobotulinum or 5 to 12 units of abobotulinum (per side). Treating the DAO requires little toxin: typically, injections of 2 to 3 units of onabotulinum/incobotulinum or 5 to 9 units of abobotulinum are sufficient for each side. Since this muscle lies in a very superficial plane care must be taken while injecting so as to not inhibit the action of the deeper DLI, which would result in smile asymmetry. Injections are best performed lateral to the commissure at the level of the mandible where the muscle is the broadest. The mentalis should be injected in its inferior portion toward the midline using 3 to 8 units of onatbotulinum/incobotulinum or 8 to 20 units of abobotulinum. The platysma can be injected using 20 to 40 units of onatbotulinum/incobotulinum or 50 to 100 units of abobotulinum to treat vertical neck bands. Treatment of bands usually requires injection of 4 to 5 units of onatbotulinum/incobotulinm or 10 to 13 units abobotulinum in 2 to 3 spots on each band.
PERIORAL FILLERS
The external carotid artery gives off the facial artery, which is the primary arterial vessel to the face. After the artery crosses the mandibular boarder, it courses in a deeper plane superiorly and medially toward the alar base. Before reaching the nasolabial fold, the facial artery gives off the inferior and superior labial arteries. These branches generally lie deep in the lip between the orbicularis oris and the mucosa. The facial artery lies in a deep plane beneath the modiolus and then transitions to a more intermediate depth as it continues beneath the nasolabial fold.
When injecting the lips, knowledge of the depth and location of the labial arteries is critical to prevent hematoma and necrosis. Because both superior and inferior arteries lie in a deep plane, it is safe to inject the body of the lip, taking care not to inject into the deeper plane between the muscle body and the mucosa where the vessel resides.7 Injection technique may also play a role in preventing vascular injury as some injectors believe that injections using cannulas instead of needles are safer and minimize vascular injury.
NASOLABIAL FILLERS
As the facial artery proceeds superiorly, it is deep at the oral commissure. Running beneath the modiolus, it proceeds in a tortuous course deep to the nasolabial fold, transitioning to a superficial-to-intermediate plane as is approaches the alar base. Placement of fillers near the alar base needs to be either deep along the piriform aperture or very superficial so as to avoid injury to the artery.
NASAL NEUROTOXIN
The nasalis is composed of 2 parts: transverse and alar. The transverse part arises from the maxilla, with fibers travelling superior and medially to join the aponeurosis of the procerus above. Contraction of this portion causes compression of the nares and is responsible for the formation of the “bunny lines.” The alar part also arises from the maxilla and inserts onto ala with contraction causing nasal flaring.
The nasalis may be treated with 2 to 5 units of onabotulinum/incobotulinum or 5 to 12 units of abobotulinum (per side). Injection of the nasalis should be performed by raising a superficial wheal, injecting between the nasofacial groove and the dorsum of the nose. Toxin should be placed in the center of the grouping of rhytids using 1 to 2 injections sites.
NASAL FILLERS
The nose has a robust blood supply, which is predominantly located along the nasal side walls and the lateral portion of the nasal dorsum. The angular artery is a continuation of the facial artery and runs in the nasofacial groove as it originates from the alar base, giving off the lateral nasal artery, which travels up the alar groove to anastomose with the dorsal nasal artery. Knowledge of these arteries is critical because of their communication with the ophthalmic and central retinal arteries via the dorsal nasal artery. Accidental injection of any of these nasal vessels may lead to severe skin necrosis or blindness when injecting the nose. Care must especially be taken in those patients who have had a previous rhinoplasty as the vascular network to the nose has been disrupted.
When injecting the nose stay deep and only in the midline, the dorsal nasal and the lateral nasal arteries are lateral and superficial. The vasculature of the nose is located between the skin and the superficial musculoaponeurotic layer. Staying deep to the nasal superficial musculoaponeurotic layer helps to prevent inadvertent injection into these vessels.
CONCLUSIONS
Nonsurgical facial rejuvenation continues to grow and is important to all of the core aesthetic specialties. A detailed knowledge of the location and depth of each muscle of facial expression is critical for efficacious delivery of neurotoxins. Likewise, a complete understanding of key vascular structures is necessary to avoid vascular injury while injecting fillers. A base knowledge of facial anatomy should still guide aesthetic injectors in their daily practice.
Footnotes
Presented at the The Cosmetic Bootcamp meeting, Aspen, Colo., July 8-11, 2016.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge for this proceeding was paid for by Allergan plc, as part of an unrestricted educational grant to support the entire Cosmetic Boot Camp 2016 Supplement. Allergan plc had no involvement in the production, selection, or review of this proceeding supplement.
Cosmetic Bootcamp: PRS Global Open proudly publishes the proceedings from The Cosmetic Bootcamp July 2016 meeting that was held in the St Regis Resort in Aspen, Colorado on July 8-11th, 2016.
REFERENCES
- 1.ASPS. National Clearinghouse of Plastic Surgery Procedural Statistics. 2015.
- 2.Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36:753–760. doi: 10.1007/s00266-012-9904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121:2107–2112. doi: 10.1097/PRS.0b013e31817123c6. [DOI] [PubMed] [Google Scholar]
- 4.Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–2227. doi: 10.1097/01.prs.0000265403.66886.54. discussion 2228–2231. [DOI] [PubMed] [Google Scholar]
- 5.Ramanadham SR, Rohrich RJ. Newer understanding of specific anatomic targets in the aging face as applied to injectables: superficial and deep facial fat compartments–an evolving target for site-specific facial augmentation. Plast Reconstr Surg. 2015;136(5 Suppl):49S–55S. doi: 10.1097/PRS.0000000000001730. [DOI] [PubMed] [Google Scholar]
- 6.Jiang X, Liu DL, Chen B. Middle temporal vein: a fatal hazard in injection cosmetic surgery for temple augmentation. JAMA Facial Plast Surg. 2014;16:227–229. doi: 10.1001/jamafacial.2013.2565. [DOI] [PubMed] [Google Scholar]
- 7.Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthetic Plast Surg. 2014;38:1083–1089. doi: 10.1007/s00266-014-0401-8. [DOI] [PubMed] [Google Scholar]


